Abstract
Objective
To examine functional mobility and strength loss in the ankle plantarflexors and dorsiflexors and knee extensors and flexors after total knee arthroplasty (TKA).
Design
Prospective, longitudinal cohort study. Maximal voluntary isometric contractions and gait speed assessments were performed before and after TKA.
Results
Twenty patients undergoing primary TKA were followed. Repeated measures ANOVA results indicated an effect of time on muscle strength, with all muscle groups being significantly weaker (knee extensors p<0.001; knee flexors p<0.001, ankle plantarflexors p= 0.004; ankle dorsiflexors p<0.001) one month post-operatively. Knee extensors were 42% weaker than pre-operative levels and knee flexors were 34% weaker while the ankle plantarflexors were 17% weaker and the dorsiflexors were 18% weaker. Three and six months after surgery, strength in all muscle groups was similar to pre-operative levels (p>0.05 for all muscle groups). Patient function followed a similar trend, with patients walking slower one month post-operatively (p<0.001) and recovering to pre-operative levels by three and six months after surgery (p>0.05).
Conclusions
Patients may benefit from early post-operative rehabilitation including strengthening of the plantarflexors and dorsiflexors, although strengthening of the quadriceps and hamstrings muscles should continue to be a priority.
Keywords: Muscle Strength, Knee Arthroplasty, Knee, Ankle
Introduction
Over 650,000 total knee arthroplasties (TKAs) are performed each year in the United States1, and this number is expected to grow to 3.5 million per year by the year 2030.2 This surgery has a profound effect on muscle function and particularly affects quadriceps muscle strength. Deficits in quadriceps strength can persist for years after TKA.3-5 However, muscular changes do not seem to be specific to the quadriceps as strength losses have also been documented in other lower extremity muscles after TKA.6 In particular, the quadriceps muscles have been shown to lose 50-60% of their pre-operative strength 4, while the hamstrings lose nearly 50% of their pre-operative strength.6 Not only do these muscles experience similar magnitudes of strength loss acutely after TKA, they recover at similar rates over the first six months after surgery6 and remain weaker years after surgery compared to healthy adults of similar age.3, 4, 6
The substantial strength loss in the knee extensors and flexors after TKA has been well described. However, whether lower extremity strength loss after TKA is muscle-specific or more widespread due to post-operative limb disuse is less clear. Muscle strength loss has been reported in the hip abductors and adductors as well as the hip flexors and extensors following orthopedic surgeries in the knee, such as anterior cruciate ligament (ACL) reconstruction.7 Moreover, the hip adductors have been shown to have a 44% deficit in strength after ACL reconstruction compared to healthy controls.8 Together, these findings imply that strength loss after knee surgery may not be confined to just the knee extensors and flexors and suggest that more global strength loss after knee surgery may occur. Despite this, investigations have not yet explored acute deficits and longitudinal recovery of the ankle plantarflexors and dorsiflexors after TKA.
Clinically and experimentally, patients after TKA have demonstrated altered gait patterns implicating weakness in the ankle plantarflexors and dorsiflexors.9, 10 Specifically, patients after TKA demonstrate a reduction in ankle plantar flexion angle during terminal stance, suggesting decreased activity of the plantarflexors.10 Furthermore, studies of muscle activity during gait indicate there is less electromyographic (EMG) activity from the plantarflexors on the side of ACL injury8 as well on the surgical side after TKA.10 These findings not only suggest that the plantarflexors may be weak, but further support the potential for generalized patterns of muscle disuse and related weakness after surgery. Additionally, it has been shown that an injury at one joint will influence muscle strength in sites away from the injured joint11 and shared neural projections are purported to exist between the knee extensors and flexors and the ankle plantarflexors and dorsiflexors. 12, 13 This evidence suggests that TKA surgery might have similar effects in the ankle plantarflexors and dorsiflexors as the previously described deficits in the knee extensors and flexors.
The effects of TKA on muscle strength are substantial, as lower extremity weakness affects functional mobility in patients after surgery.4, 14-18 Specifically, quadriceps and hamstrings muscle weakness leads to deficits in rising from a chair, walking speed and stair climbing.4, 14, 19 Furthermore, hip strength after TKA has been shown to play a substantial role in gait quality and functional mobility.15 Although the effect of TKA on ankle plantarflexor and dorsiflexor strength is unknown, it has been shown that weakness in these muscles contributes to decreased gait speed, increased fall risk and decreased functional mobility in older adults.16-18 Therefore, the decline in functional mobility seen after TKA may be not only due to knee extensor and hip abductor weakness, but also due to ankle muscle weakness. Consequently, understanding the degree of strength loss in the ankle plantarflexors and dorsiflexors and the effect on functional mobility after TKA may help target rehabilitation strategies after TKA to optimize recovery.
This study examined strength in the ankle plantarflexors and dorsiflexors in addition to the knee extensors and flexors before and after (1, 3, 6 months) TKA. Secondarily, this study examined gait speed before and after TKA as a measure of functional mobility. We hypothesized that muscle weakness would present in all muscle groups at each post-operative time point compared to pre-operative strength. Further, we hypothesized gait speed would be reduced at all post-operative time points compared to pre-operative values.
Methods
Study Design
This investigation was a prospective, longitudinal cohort study examining muscle strength and gait speed in patients undergoing TKA.
Setting and Participants
Patients undergoing primary, unilateral TKA were recruited from two hospitals in the community between March 2008 and September 2010 as part of an ongoing clinical investigation. Patients were considered eligible if they were between the ages of 50 and 85 and scheduled for a primary, unilateral TKA. Patients were excluded if they had uncontrolled hypertension, uncontrolled diabetes, body mass index >40 kg/m2, additional lower extremity orthopaedic pathology, or neurologic disorders which impaired daily function. Volunteers were recruited by physician referral or advertisement at pre-operative educational sessions. All patients underwent a tricompartmental, cemented TKA with a medial parapatellar surgical approach. Following surgery, all participants participated in post-operative home health and outpatient physical therapy as prescribed by their surgeon. The rehabilitation program was directed by a licensed physical therapist and was a traditional program comprised of global strengthening, range-of-motion and mobility exercises. Consistent with recently published rehabilitation guidelines20, 21, most of these rehabilitation programs prioritized quadriceps strengthening, but also included some exercises for hamstrings and plantarflexors. Few programs included exercises specifically targeting dorsiflexors. Testing sessions took place pre-operatively and at 1, 3, and 6 months post-operatively. Each participant provided written informed consent and the study was approved by the Colorado Multiple Institutional Review Board.
Strength Testing Procedures
Surgical limb ankle plantarflexor and dorsiflexor and knee extensor and flexor strength was measured at each testing session. Maximal voluntary isometric contractions (MVICs) of the ankle plantarflexors and dorsiflexors were performed with the patient laying supine on an electromechanical dynamometer (HUMAC NORM CSMI, Stoughton, MA) with the knee supported at 45° of flexion (Figure 1). Ankle plantarflexor strength measurements were performed with the ankle joint at 0°, while dorsiflexor strength measurements were taken with the ankle joint in 20° of plantar flexion. Knee extensor and flexor strength measurements were performed while the patients were seated and stabilized on the dynamometer. Patients were positioned in 85° of hip flexion and 60° of knee flexion as previously described (Figure 2).6, 22 Data were sampled using a Biopac Data Acquisition System at a sampling frequency of 2000Hz (Biodex Medical Systems, Inc., Shirley, NY) and analyzed using AcqKnowledge software, Version 3.8.2 (Biodex Medical Systems). Strength measurements were expressed in units of torque (Nm), which was calculated by multiplying the force (N) collected by the dynamometer by the lever arm length (m) (ankle: medial malleolous to the metatarsal-phalengeal joint; knee: medial joint line to one inch superior to the medial malleolus). Each MVIC was preceded by two sub-maximal warm-up contractions. All patients were given visual targets and strong verbal encouragement during each MVIC to aid in eliciting maximal effort. All MVICs were performed by allowing the patient to gradually increase force to his/her maximum ability; maximal effort was maintained for three to five seconds. Patients were allowed 20-30 second rest periods between MVICs. MVICs for all muscle groups were performed twice; however, if maximal torque during the first two trials differed by more than 5%, a third trial was performed. The trial with the highest torque was used for analysis. Following each MVIC, patients were asked to report a pain level using a numerical pain rating scale (NPRS) of 0-10.
Figure 1.
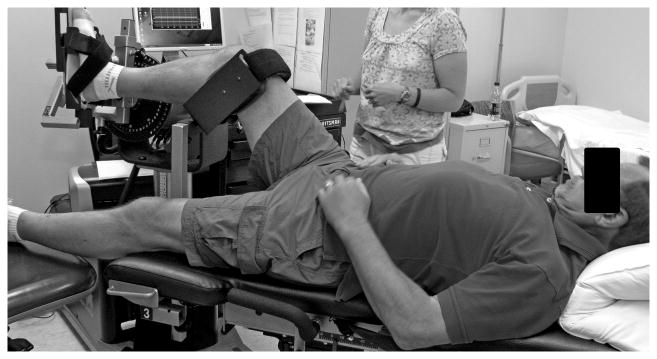
Study participant positioned on the dynamometer for ankle plantarflexor and dorsiflexor testing position.
Figure 2.
Study participant positioned on the dynamometer for knee extensor and extensor testing position.
Gait Speed Testing Procedures
A six-minute walk test was also performed at each testing session. Each patient was given the instructions to walk as quickly but as safely as they were able in a 30.5 meter hallway. Gait speed was measured as the time it took to walk the first 30.5 meters during the six-minute walk test. Patients were permitted to use an assistive device as they deemed necessary to ensure pain reduction and patient safety.
Statistical methods
Sample size estimates were calculated based on plantarflexor muscle strength measurements collected during pilot testing in this population. Using the means and standard deviations for plantarflexor strength measured pre-operatively and at one month after surgery, our effect size was estimated to be 0.78. Assuming two-sided type I error protection of 0.05 and a power of 0.80, we anticipated that 16 patients were required to detect plantarflexor strength loss one month after TKA. Therefore, we conservatively enrolled 20 patients.
For analysis, peak torque (Nm) for each muscle was normalized to body mass (kg). A repeated-measures ANOVA was performed to assess for an effect of time on muscle strength for each muscle group. Post-hoc paired t-tests were performed to detect differences in strength and gait speed from pre-operative testing at each post-operative time point. A significance level of 0.05 was set for all statistical tests. Statistical analyses were performed using Statistical Package for the Social Sciences (SPPS) software (SPSS version 19, Chicago, IL). Furthermore, to compare relative magnitudes of strength loss across muscle groups, estimates of the percent differences between the pre-operative and one month post-operative time points were calculated as follows:
Results
Twenty patients with end-stage osteoarthritis (OA), scheduled for primary TKA were followed (age: 65.1 ± 7.8years; BMI: 29.7 ± 4.3 kg/m2; 13 women, 7 men). Two patients were missing plantarflexor and dorsiflexor strength measurements at the six month time point and one patient was missing knee extensor and flexor measurements at the six month time point. For missing data points, the last recorded value was carried forward. Gait speed data were only available for a subset of our sample (n= 16); therefore, gait speed analysis was performed on this subset of 16 patients.
Results from the repeated measures ANOVA indicated an effect of time for each muscle (p<0.001 for all muscle groups). Post-hoc t-tests indicated that at one month after surgery all muscle groups were significantly weaker compared to pre-operative measures (plantarflexors p= 0.004; dorsiflexors p<0.001; knee extensors p<0.001; knee flexors p<0.001; Figure 3 A-D). One month after TKA, patients exhibited 17% less plantarflexor strength and 18% less dorsiflexor strength than before surgery. In addition, patients demonstrated 42% less knee extensor strength and 34% less knee flexor strength one month after TKA (Figure 3 A-D). By three and six months after surgery, patients' strength in all muscle groups was similar to pre-operative strength levels (p>0.05 for all muscle groups). Average pain levels with the NPRS during each session were 1.6/10 pre-operatively, 1.3/10 one month after surgery, 0.4/10 and 0.1/10 at three and six months, respectively.
Figure 3. (A-D). Muscle strength preoperatively through 6 months after TKA.
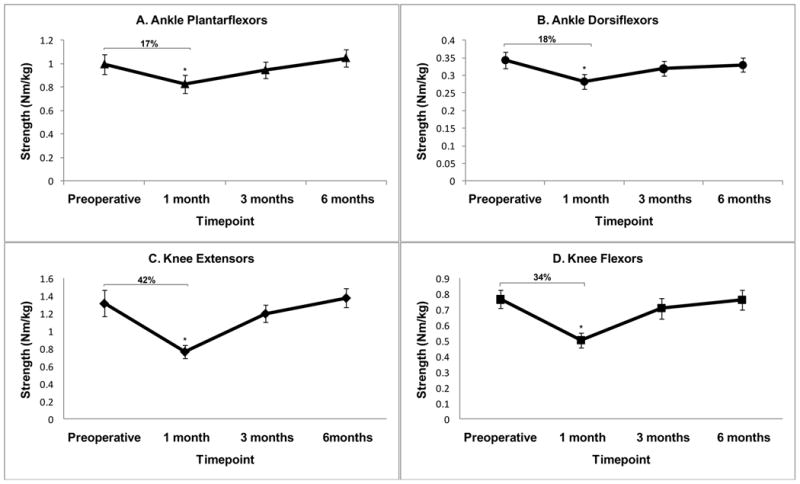
A) Ankle plantarflexors, B) Ankle dorsiflexors, C) Knee extensors, D) Knee flexors.
*indicates significant strength loss after surgery (pre-op to 1month) (p<0.05). Percent difference in muscle strength preoperative to 1 month noted in figure. Strength (N-m) is normalized to body weight (kg) (mean ± SEM).
Gait speed analysis similarly indicated an effect of time on gait speed (p<0.001). Post-hoc t-tests demonstrated that patients walked slower one month after surgery compared to the pre-operative testing session (p<0.001). By three and six months after surgery, gait speed returned to levels similar to pre-operative values (p>0.05).
Discussion
Understanding the impact of TKA surgery on lower extremity muscle strength helps ensure that rehabilitation is correctly targeted to maximize functional recovery. Therefore, this study documented changes in isometric strength in the ankle plantarflexors and dorsiflexors as well as knee extensors and flexors through six months of recovery after TKA. Although recovery of strength and gait speed to pre-operative levels was seen by three months after surgery, recent investigations have indicated that recovery to pre-operative levels may not be adequate as functional mobility in patients after TKA is inferior to healthy, older adults.4 The results from this study indicates that rehabilitation strategies need to be improved to optimize recovery4. Commonly after TKA, physical therapists routinely focus post-operative rehabilitation programs on strengthening the quadriceps and to a lesser extent, the hamstrings, because of the well documented strength loss in these muscles early after surgery. 4, 6, 23 The present investigation provides additional support for targeting muscle weakness in the knee extensors and flexors but also suggests that the ankle plantarflexors and dorsiflexors warrant attention in post-operative rehabilitation programs to improve functional mobility.
We hypothesized that the ankle plantarflexors and dorsiflexors, as well as the knee extensors and flexors would all lose strength after TKA. Our results confirmed part of our initial hypothesis, as there was muscle weakness present in all muscle groups one month after surgery. However, in this population, we saw general recovery to pre-operative levels at three and six months after surgery. Although all muscle groups tested were weaker after surgery, we saw that patients lost twice as much strength in the knee extensors and flexors than in the ankle plantarflexors and dorsiflexors compared to pre-operative values. Due to low patient-reported pain levels during testing, we do not believe pain contributed substantially to these findings. The results from our study support previous findings that some global strength loss occurs in the surgical limb after knee surgery. Jaramillo et al. 7 studied hip muscle strength after knee surgery and found that isometric strength of the hip abductors, adductors, flexors and extensors in the surgical limb was 12-25% weaker than the non-surgical limb after surgery. Additionally, Piva et al. 15 examined the relationship between hip abductor strength and several functional tasks after TKA and indicated that hip abductor strength explained 10-22% of the variance in these measures. Therefore, functional mobility is also affected by muscle weakness in muscles farther from the knee joint after TKA. The present study is the first to provide longitudinal evidence that muscle weakness also occurs in the ankle plantarflexors and dorsiflexors one month after TKA.
Previous studies4, 14-18 have reported the negative effects of surgery on lower extremity muscle strength. It is clear that muscle weakness translates into declines in functional mobility. In particular, Hernandez et al. 16 indicated that older adults, who reported difficulty with stooping, crouching and kneeling, exhibit weakness in their knee extensors and ankle plantarflexors and dorsiflexors. Furthermore, Tiedemann et al. 18 found that the decline in older adults' self-selected walking speed was related to ankle dorsiflexor strength as well as knee extensor and flexor strength. Likewise, gait speed measures available in a subset of our study population (n=16) support this conclusion whereby at one month after TKA, patients demonstrated a slower self-selected walking speed over a 30.5 meter distance compared to their pre-operative walking speed (p<0.001). Finally, a review article by Horlings et al. 17 reported that lower extremity muscle weakness, including the ankle plantarflexors and dorsiflexors, is a risk factor for increased incidence of falls in older adults. Furthermore, these authors suggest that strength training interventions targeting these muscles can be effective in reducing fall risk. Collectively, these data16-18 not only implicate the ankle musculature in mobility deficits and fall risk, but also suggest that these deficits may be ameliorated through an effective strengthening program. Therefore, a comprehensive rehabilitation program after TKA should include strengthening of the ankle muscles in addition to the quadriceps and hamstrings to optimize safety and function.
There are some limitations to acknowledge in this study. First, one potential limitation of this study was the small sample size. Secondly, our statistical analysis indicated that this cohort of patients returned to pre-operative knee extensor and knee flexor strength levels by three months after surgery. Previous investigations suggest that knee extensor and flexor strength typically do not fully recover until 6 months after TKA.4, 6 The variability noted in this sample cohort may have contributed to our current findings. Finally, we acknowledge that additional data from the contralateral limb would have further strengthened our findings, which should be included in future investigations.
Conclusions
The current findings confirm the presence of knee extensor and flexor weakness following TKA and indicate that the ankle plantarflexors and dorsiflexors also lose strength after TKA. Therefore, patients may benefit from early post-operative strengthening programs targeting the plantarflexors and dorsiflexors although strengthening of the knee extensors and flexors should continue to be a priority.
Acknowledgments
This study was supported by the National Institute of Aging (K23AG029978) and a Clinical and Translational Science Award (UL1 RR025780).
The authors thank Jaclyn Balter, MS, for assistance in study design and data collection and Abbey Thomas, PhD, ATC for reviewing this manuscript. The authors also thank the study volunteers for their time and effort.
Footnotes
Disclosures: Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
This research was previously presented as a poster at the American Physical Therapy Association Combined Sections Meeting, February 2011, New Orleans, LA.
References
- 1.Health Care Cost and Utilization Project. HCUP Facts and Figures: Statistics on Hospital-Based Care in the United States. [Accessed 1/18/2011]; http://www.hcup-us.ahrq.gov/reports/factsandfigures/2008/exhibit3_1.jsp.
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Huang CH, Cheng CK, Lee YT, Lee KS. Muscle strength after successful total knee replacement: a 6- to 13-year followup. Clin Orthop Relat Res. 1996 Jul;(328):147–154. doi: 10.1097/00003086-199607000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010 Sep;40(9):559–567. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003 Sep;21(5):775–779. doi: 10.1016/S0736-0266(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 6.Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG. Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res. 2010 Sep;468(9):2460–2468. doi: 10.1007/s11999-009-1219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaramillo J, Worrell TW, Ingersoll CD. Hip isometric strength following knee surgery. J Orthop Sports Phys Ther. 1994 Sep;20(3):160–165. doi: 10.2519/jospt.1994.20.3.160. [DOI] [PubMed] [Google Scholar]
- 8.Hiemstra LA, Gofton WT, Kriellaars DJ. Hip strength following hamstring tendon anterior cruciate ligament reconstruction. Clin J Sport Med. 2005 May;15(3):180–182. doi: 10.1097/01.jsm.0000157795.93004.ea. [DOI] [PubMed] [Google Scholar]
- 9.Limbird TJ, Shiavi R, Frazer M, Borra H. EMG profiles of knee joint musculature during walking: changes induced by anterior cruciate ligament deficiency. J Orthop Res. 1988;6(5):630–638. doi: 10.1002/jor.1100060503. [DOI] [PubMed] [Google Scholar]
- 10.Ouellet D, Moffet H. Locomotor deficits before and two months after knee arthroplasty. Arthritis Rheum. 2002 Oct 15;47(5):484–493. doi: 10.1002/art.10652. [DOI] [PubMed] [Google Scholar]
- 11.Sedory EJ, McVey ED, Cross KM, Ingersoll CD, Hertel J. Arthrogenic muscle response of the quadriceps and hamstrings with chronic ankle instability. J Athl Train. 2007 Jul-Sep;42(3):355–360. [PMC free article] [PubMed] [Google Scholar]
- 12.Meunier S, Mogyoros I, Kiernan MC, Burke D. Effects of femoral nerve stimulation on the electromyogram and reflex excitability of tibialis anterior and soleus. Muscle Nerve. 1996 Sep;19(9):1110–1115. doi: 10.1002/(SICI)1097-4598(199609)19:9<1110::AID-MUS5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins JT, Ingersoll CD, Krause BA, Edwards JE, Cordova ML. Effect of knee joint effusion on quadriceps and soleus motoneuron pool excitability. Med Sci Sports Exerc. 2001 Jan;33(1):123–126. doi: 10.1097/00005768-200101000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Farquhar SJ, Reisman DS, Snyder-Mackler L. Persistence of altered movement patterns during a sit-to-stand task 1 year following unilateral total knee arthroplasty. Phys Ther. 2008 May;88(5):567–579. doi: 10.2522/ptj.20070045. [DOI] [PubMed] [Google Scholar]
- 15.Piva SR, Teixeira PE, Almeida GJ, et al. Contribution of hip abductor strength to physical function in patients with total knee arthroplasty. Phys Ther. 2011 Feb;91(2):225–233. doi: 10.2522/ptj.20100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hernandez ME, Goldberg A, Alexander NB. Decreased muscle strength relates to self-reported stooping, crouching, or kneeling difficulty in older adults. Phys Ther. 2010 Jan;90(1):67–74. doi: 10.2522/ptj.20090035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horlings CG, van Engelen BG, Allum JH, Bloem BR. A weak balance: the contribution of muscle weakness to postural instability and falls. Nat Clin Pract Neurol. 2008 Sep;4(9):504–515. doi: 10.1038/ncpneuro0886. [DOI] [PubMed] [Google Scholar]
- 18.Tiedemann A, Sherrington C, Lord SR. Physiological and psychological predictors of walking speed in older community-dwelling people. Gerontology. 2005 Nov-Dec;51(6):390–395. doi: 10.1159/000088703. [DOI] [PubMed] [Google Scholar]
- 19.Buchner DM, Larson EB, Wagner EH, Koepsell TD, de Lateur BJ. Evidence for a non-linear relationship between leg strength and gait speed. Age Ageing. 1996 Sep;25(5):386–391. doi: 10.1093/ageing/25.5.386. [DOI] [PubMed] [Google Scholar]
- 20.Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009 Feb 15;61(2):174–183. doi: 10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 21.Meier W, Mizner RL, Marcus RL, Dibble LE, Peters C, Lastayo PC. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther. 2008 May;38(5):246–256. doi: 10.2519/jospt.2008.2715. [DOI] [PubMed] [Google Scholar]
- 22.Mintken PE, Carpenter KJ, Eckhoff D, Kohrt WM, Stevens JE. Early neuromuscular electrical stimulation to optimize quadriceps muscle function following total knee arthroplasty: a case report. J Orthop Sports Phys Ther. 2007 Jul;37(7):364–371. doi: 10.2519/jospt.2007.2541. [DOI] [PubMed] [Google Scholar]
- 23.Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am. 2005 May;87(5):1047–1053. doi: 10.2106/JBJS.D.01992. [DOI] [PMC free article] [PubMed] [Google Scholar]



