Abstract
Purpose
To investigate myopia progression in Correction of Myopia Evaluation Trial (COMET) participants who switched to soft contact lenses (CLs) versus remained in spectacles after the clinical trial ended.
Methods
469 ethnically diverse, 6–11 year old myopic children were randomly assigned to wear single vision lenses (SVLs) or progressive addition spectacle lenses (PALs) for 5 years as part of COMET. Afterwards they could choose another lens type, including CLs. Data in this paper are from 286 participants who wore their original spectacle lenses for 6 years (n =199) or wore CLs most or all of the time between the 5- and 6-year visits (n =87). Refractive error and axial length (AL) were measured after cycloplegia with 1% Tropicamide. The primary outcome was myopia progression between the 5- and 6-year visits. Two-year myopia progression was evaluated in a subset of 183 participants who wore the same lens type for an additional year. Myopia progression and AL were compared between the two lens groups using multiple linear regression.
Results
Participants in the two groups were similar with respect to age, ethnicity, myopia at 5-years, accommodation and phoria, but more girls switched to CLs than remained in spectacles (p<0.0001). Mean (± SD) myopia progression was higher (p=0.003) after one year in the CL group (−0.28 ± 0.33D) than the spectacle group (−0.14 ± 0.36D), and remained higher after two years in the 2-year subset (− 0.52 ± 0.46D versus −0.25 ± 0.39D, p<0.0001). Results were similar after adjustment for related factors. No significant differences in AL were found between groups after adjustment. Corneal curvature remained unchanged in both groups.
Conclusions
COMET children switching from glasses to contact lenses experienced a small, statistically significant but clinically inconsequential increase in myopia progression.
Keywords: contact lenses, myopia physiopathology therapy, disease progression, follow-up studies, adolescent
With so many children wearing contact lenses (CLs) at increasingly younger ages,1 consideration has been given to their possible effect on the progression of myopia. Recent studies evaluating myopia progression in children wearing either soft CLs or spectacles have reported differences in progression between the two lens groups ranging from approximately 0.00 to 0.50D per year.2–4 The largest difference (0.49 D, p<0.0001) was reported by Fulk et al. in a study of children either switching from spectacles to CLs or remaining in spectacles.2 In contrast, two randomized studies found smaller differences in myopia progression between children who were assigned to wear either spectacles or CLs.3,4
The current study investigates myopia progression by lens type, including CLs, in children originally enrolled in the Correction of Myopia Evaluation Trial (COMET), which was a multicenter clinical trial to evaluate whether wearing progressive addition lenses (PALs) versus single vision lenses (SVLs) would reduce the progression of myopia in young children.5,6 Eligible children aged 6–11 years were randomized to wear either SVLs or PALs with a +2.0 addition. Results after 3 years of follow-up showed a statistically significant (p=0.004) but clinically inconsequential adjusted difference in myopia progression of 0.20 ± 0.08 D with slower progression in the PAL group.7
The clinical trial ended after 5 years of follow-up, after which parents and children were invited to continue in an observational phase called COSMICC (the Collaborative Observational Study of Myopia in COMET Children). In consultation with their study optometrist, participants could continue wearing the original spectacle lens, switch to the other spectacle lens, or switch to CLs. Approximately half of the COMET children switched to CLs after the clinical trial phase of the study ended, presenting a unique opportunity to evaluate the effect of CLs on the course of myopia progression in this large, ethnically diverse cohort of children. The purpose of the present report is to compare the progression of myopia in COMET children who either switched to CLs or remained in spectacle lenses after 5 years of follow-up.
METHODS
Study Population
469 ethnically diverse, 6–11 year old children enrolled in COMET at one of four clinical centers in schools/colleges of optometry in Birmingham AL, Boston MA, Houston TX, and Philadelphia PA, between September 1997 and September 1998. Children agreed to wear spectacle lenses (randomly assigned SVLs or PALs) and not CLs for at least 3 years, the initial duration of the clinical trial. Inclusion criteria included spherical equivalent myopia between − 1.25 and −4.5 D inclusive, small amounts of astigmatism (≤1.50 D) in each eye, and anisometropia of 1.0 D spherical equivalent or less. Additional details are published elsewhere.5,6
Data Collection/Study Procedures
Outcome data were collected annually by study optometrists who were certified on all procedures.5,6 Myopia was measured by cycloplegic autorefraction using the Nidek ARK 700A taken 30 minutes after the second drop of 1% Tropicamide. Five measurements per eye with reliability ratings of 7 or higher were collected. Axial length was measured by A-Scan ultrasonography (A-2500; Sonomed; Lake Placid, NY). A-scan measurements were taken until 5 measures with standard deviation below 0.1mm were obtained (available in either eye for 97% of the 434 children at 5 years). At least 3 acceptable measures per visit were necessary for inclusion in data analysis. Horizontal and vertical corneal curvatures were measured using the Nidek ARK 700A. Prior to cycloplegia, accommodative response of the right eye was measured using the Canon R1 autorefractor while the child viewed 20/100 backlit letters at 4M and at 33 cm wearing the spherical equivalent subjective refraction in trial frames. Phorias were measured by cover test with prism neutralization.
The COMET study and protocols conformed to the tenets of the Declaration of Helsinki. The institutional review boards of each participating center approved the research protocols. Informed consent (parents) and assent (children) were obtained after verbal and written explanation of the nature and possible consequences of study participation.
Contact Lens Wear
COMET participants and their parents were unmasked about lens assignment after the 5-year visit. The actual duration of the clinical trial exceeded the initial planned duration of 3 years, but most children wore their assigned lenses until the unmasking visit. After unmasking, children could choose any lens type, including CLs, provided that parents and the study optometrist approved. Children choosing CLs were fit by the study optometrists in Birmingham, by non-study academic optometrists in Houston and Philadelphia, and by community eye providers in Boston. Information collected about CLs use included the general type (hydrogel vs. rigid lens), the frequency of wear (CLs worn all or most of the time, glasses and CLs worn equally, glasses worn all or most of the time) and the duration of wear (determined from the parent's report of the date the child started wearing lenses). No data about the CL parameters, e.g., specific type or power of the lenses, were gathered.
Analysis Cohort
Inclusion Criteria
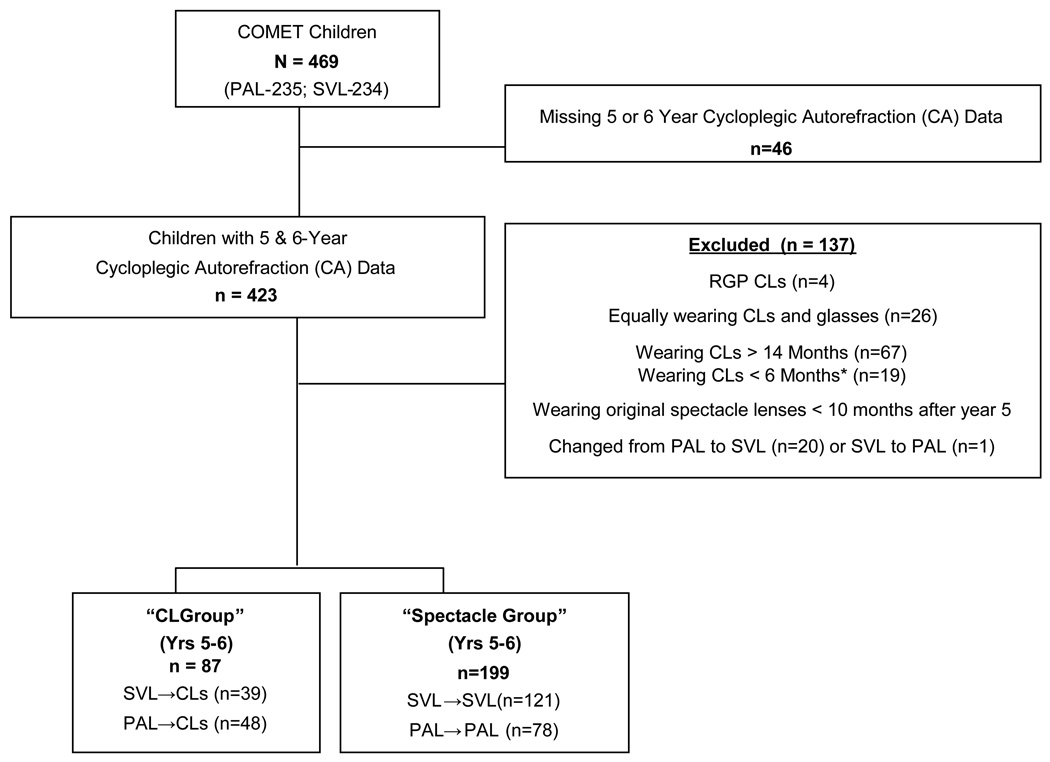
COMET children were considered eligible for the primary analyses (i.e., one year myopia progression) based on the availability of cycloplegic autorefraction data at the 5- and 6- year visits and information about the duration and frequency of glasses/soft CL use at the 6-year visit. Figure 1 shows that, from the original cohort of 469 children, 423 had cycloplegic autorefraction at both the 5- and 6-year visits (200 from the PAL and 223 from the SVL group). Eighty-seven children were eligible for the CL group and 199 were eligible for the spectacle group, while 137 children were excluded for reasons discussed below. Eligibility criteria for the CL group required: switching from spectacles to soft CLs between 6 and 14 months prior to the 6-year examination and reporting wearing CLs "most or all of the time" at that visit. The CL group included 39 children originally assigned to wear SVLs and 48 children originally assigned to wear PALs. Eligibility for the spectacle group required wearing the originally assigned spectacle lenses "most or all of the time" for at least the first 10 months after the 5-year visit. The spectacle group included 121 children originally assigned to wear SVLs and 78 children originally assigned to wear PALs.
Figure 1.
Classification of COMET children for contact lens analyses. *Children who switched to CLs ≤ 2 months before the 6 year visit were eligible for the spectacle group.
Exclusion Criteria
These criteria were developed to exclude children who could not be assigned to one group or the other (used CLs and spectacles equally), to exclude children whose progression might differ from the main group due to brief or prolonged duration of CL wear, and to exclude groups with only a few members (those who switched spectacle lens types). Children were excluded because they: 1) were missing 5- or 6-year cycloplegic autorefraction data (N=46), 2) wore rigid lenses (N=4), 3) used CLs and spectacles equally (N=26), 4) wore CLs more than 14 months before the 6- year visit (N=67) or 5) wore CLs less than 6 months and did not wear original spectacles long enough to be eligible for the spectacle group (the first 10 months after the 5-year visit) (N=19). Children were also excluded if they changed their original spectacle lens type between the 5- and 6-year visits (20 switched from PALs to SVLs and 1 switched from SVLs to PALs).
Two-Year Subset
Children were eligible for the two-year subset if they were members of the analysis cohort described above and continued to wear the same type of lenses (CLs or spectacles) most or all of the time between the 6- and 7- year visits. This two-year subset included 77 children who continued to wear CLs (35 from SVLs and 42 from PALs) and 106 children who remained in spectacles (79 remaining in SVLs and 27 remaining in PALs). Children became ineligible for the two-year subset most frequently because they switched to CLs between the 6- and 7- year visits (N=50). Outcome measures for these subset analyses were evaluated for annual change (between the 5- and 6- year and between the 6- and 7- year visits) and for 2 year change (between the 5- and 7- year visits).
Outcome Measurements
The primary outcome for this report was myopia progression over one year, i.e., the change in spherical equivalent values between the 5- and 6- year visits. Two-year myopia progression (between the 5- and 7- year visits), as well as one- and two-year changes in axial length and corneal curvature were considered as secondary outcomes. Myopia in each eye was represented by the mean spherical equivalent, based on five cycloplegic autorefraction values. Each ocular component and overall axial length for each eye was the average of the A-scan measurements. Corneal radii were analyzed separately as the vertical and horizontal meridian, and the average of the two. All analyses are child-based, i.e., determined by averaging the cycloplegic autorefraction, ultrasound or corneal curvature measurements from right and left eyes. Accommodative response at near was calculated as the mean spherical equivalent of five measurements, and was analyzed as a continuous variable. Phoria was measured with cover test and evaluated as a categorical variable: exophoria (≤ −2 Δ), orthophoria (−1 Δ to +1 Δ), and esophoria (≥ 2 Δ).
Statistical Methods
Characteristics of eligible versus non-eligible children, or children in the CL versus the spectacle groups, were compared using t-tests for continuous variables (age, myopia, and accommodative response at the 5-year visit), and the F test from Analysis of Variance (ANOVA) for categorical variables (gender, ethnicity, and phoria).
One- and two- year changes in myopia, axial length and corneal curvature were compared between the CL and spectacle groups using t-tests without adjusting for other factors. One- and two-year myopia progression and axial elongation were also compared between the two groups using stepwise multiple linear regression (analysis of covariance) to adjust for other factors. For myopia progression, candidate factors were age, gender, ethnicity, myopia at 5 years, progression of myopia between the 4- and 5-year visits, 5-year axial length, 5-year accommodative response, and 5-year phoria. Axial elongation was analyzed using a similar approach to that used for myopia progression. However, for these analyses axial length at 5 years and axial elongation between the 4- and 5-year visits were used as candidate factors instead of myopia at 5 years and myopia progression between the 4- and 5- year visits. Corneal curvature measurements (horizontal, vertical and average) were also included as candidate factors in the evaluation of axial elongation.
RESULTS
No statistically significant differences were found between the eligible and non-eligible children with respect to gender, ethnicity, and 5-year age, phoria, myopia and accommodation (data not shown). Table 1 shows that eligible children in the CL and spectacle groups were similar with respect to age, ethnicity, phoria, myopia, and accommodative response at 5 years, but girls switched to CLs more frequently than boys did (p<0.0001).
Table 1.
5-Year Characteristics of CL and spectacle Groups (N=286).
| CL Group N=87 |
Spectacle Group N=199 |
p- value | |||
|---|---|---|---|---|---|
| Gender | n% | n% | |||
| Male | 26 | 29.9 | 113 | 56.8 | <.0001 |
| Female | 61 | 70.1 | 86 | 43.2 | |
| Ethnicity | |||||
| African-American | 28 | 32.2 | 59 | 29.7 | 0.17 |
| Asian | 5 | 5.8 | 15 | 7.5 | |
| Hispanic | 9 | 10.3 | 37 | 18.6 | |
| Mixed | 7 | 8.1 | 6 | 3.0 | |
| White | 38 | 43.7 | 82 | 41.2 | |
| Phoria (Cover test) | |||||
| Exo(<= −2Δ) | 26 | 29.9 | 58 | 29.2 | 0.54 |
| Ortho(−1 to 1Δ) | 38 | 43.7 | 76 | 38.2 | |
| Eso(>= 2Δ) | 23 | 26.4 | 65 | 32.7 | |
| Mean ± SD | Mean ± SD | ||||
| Myopia (D) | −4.25 ± 1.52 | −4.32 ± 1.40 | 0.71 | ||
| Age (years) | 15.04 ± 1.21 | 14.76 ± 1.39 | 0.10 | ||
| Accommodative response (D) at 33 cm | 2.49 ± 0.54 | 2.48 ± 0.63 | 0.93 | ||
One-Year Myopia Progression
The main finding appears in Table 2; children who switched to CLs had statistically significantly more myopia progression (−0.28 ± 0.33 D) compared to children who remained in spectacle lenses (−0.14 ± 0.36 D; difference of −0.14 D, p=0.003). Table 2 also shows that one year progression in the CL group was similar whether children had originally worn SVLs (−0.29 ± 0.34 D) or PALs (−0.26 ± 0.33 D). Similarly, progression in the spectacle group was comparable whether children remained in SVLs (−0.14 ± 0.34 D) or PALs (−0.15 ± 0.39 D).
Table 2.
One-Year myopia progression (Diopters), change in axial length (mm) and average corneal curvature between years 5 and 6 by lens change group.
| Myopia progression (D) |
Change in Axial Length (mm) |
Change in Average Corneal Curvature (D) |
||
|---|---|---|---|---|
| N | Mean ± SD | Mean ± SD | Mean ± SD | |
| CL Group1 | 87 | −0.28 ± 0.33 | 0.07 ± 0.13 | 0.01 ± 0.19 |
| Spectacle Group2 | 199 | −0.14 ± 0.36 | 0.11 ± 0.14 | 0.00 ± 0.17 |
| Difference (CLs−Spectacles) | ||||
| Unadjusted | −0.14 (p=0.003) |
−0.04 (p=0.04) |
0.01 (p=0.77) |
|
| Adjusted | −0.15 (p=0.001)3 |
0.03 (p=0.11)4 |
NA5 | |
| Lens Change Group | ||||
| SVL-CL | 39 | −0.29 ± 0.34 | 0.05 ± 0.11 | 0.02 ± 0.22 |
| PAL-CL | 48 | −0.26 ± 0.33 | 0.09 ± 0.14 | 0.00 ± 0.17 |
| SVL-SVL | 121 | −0.14 ± 0.34 | 0.09 ± 0.14 | 0.00 ± 0.15 |
| PAL-PAL | 78 | −0.15 ± 0.39 | 0.13 ± 0.15 | 0.00 ± 0.19 |
PAL=progressive addition lenses; SVL=single vision lenses; CL=contact lenses.
CL Group includes ‘PAL-CL’ (children changing from PALs to CLs) and ‘SVL-CL’ (children changing from SVLs to CLs).
Spectacle Group includes ‘PAL-PAL’ (children remaining in PALs) and ‘SVL-SVL (children remaining in SVLs).
Based on regression analysis with age and phoria by cover test at the 5-year visit as covariates.
Based on regression analysis with age at the 5-year visit and axial elongation between the 4-year and 5-year visits as covariates.
Not done due to minimal change in average corneal curvature in both groups.
Age and esophoria at the 5-year visit were associated with more myopia progression between the 5- and 6-year visits (p=0.03 for both factors). After adjusting for these factors, the difference in myopia progression between children in the CL versus spectacle groups was −0.15 D (p=0.001). This adjusted value was similar to the unadjusted difference of −0.14 D (p=0.003) shown in Table 2.
Two-Year Myopia Progression in the Subset of Children
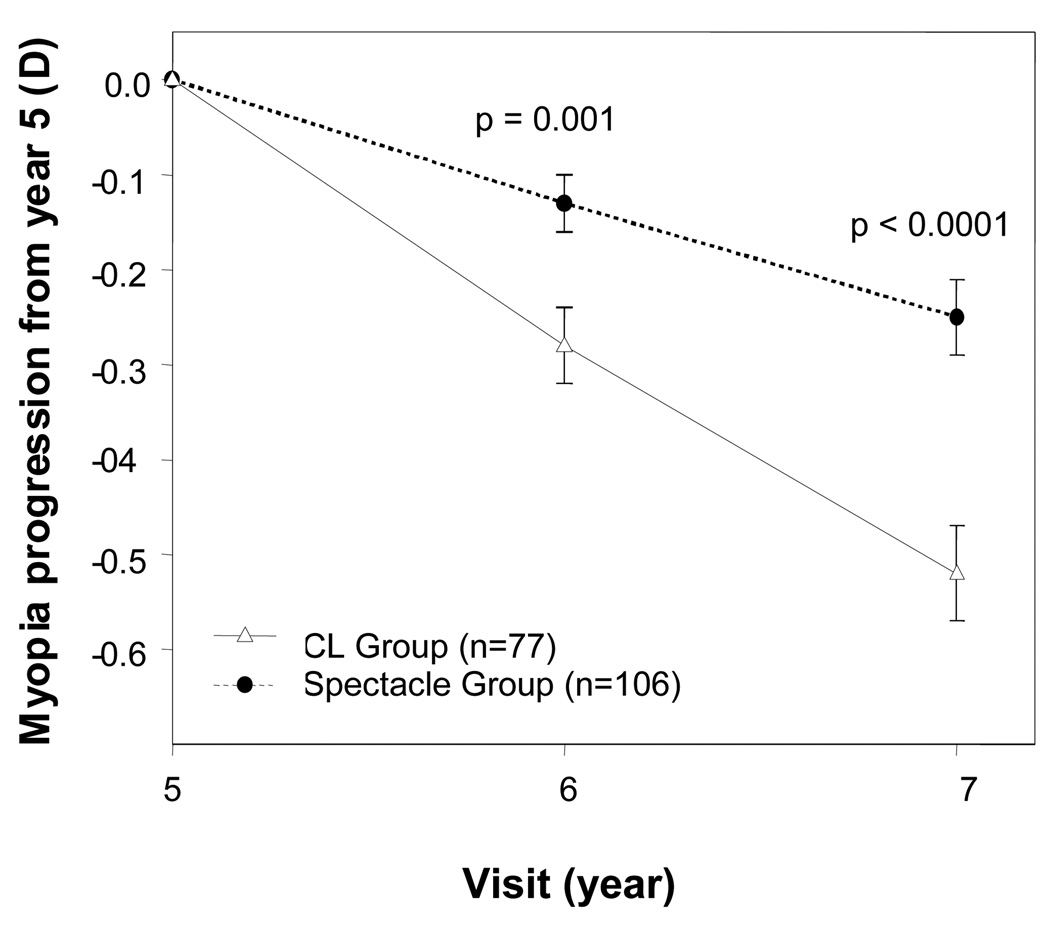
Myopia progression (unadjusted) from the subset of 183 children who continued to wear the same lenses between the 6- and 7- year visits is shown in Figure 2. In these children one-year myopia progression (between the 5- and 6-year visits) was higher by 0.15 D (p=0.001) in the CL subset (−0.28 ± 0.33 D) than in the spectacle subset (−0.13 ± 0.29 D), a one-year difference that was similar to that observed in the larger group during the same period.
Figure 2.
Two-year myopia progression (Diopters) between Years 5 and 7 by lens group. Based on values from the two-year subset, i.e., participants who were classified between years 5 and 6 and remained in the same lens type between years 6 and 7. Error bars= Standard error (SE).
After an additional year of follow-up (between the 6- and 7-year visits), myopia progression remained higher in the CL subset (−0.23 ± 0.32 D) than in the spectacle subset (−0.12 ± 0.27 D; p=0.008). When the full two-year period was considered, a small but statistically significant difference in myopia progression of −0.27 D was observed: −0.52 ± 0.46 D in the CL subset versus −0.25 ± 0.39 D in the spectacle subset (p<0.0001).
Using stepwise regression, only age at the 5-year visit was identified as a significant factor (p=0.001) for myopia progression in the 2-year subset between the 5- and 7-year visits. Therefore, the final model for two-year progression included only age as a covariate with lens status. The difference between the two groups remained similar after adjustment for age: myopia in children in the CL subset progressed 0.27 D more than myopia in the spectacle subset during the two-year period (p<0.0001).
One-Year Axial Elongation
As shown in Table 2, the difference in axial elongation between groups was small. One-year axial elongation (between the 5-and 6-year visit) was lower in the CL (0.07 ± 0.13mm) than the spectacle group (0.11 ± 0.14 mm) by a small, statistically significant amount (0.04 mm, p=0.04). However, when adjusted for age and axial elongation between the 4- and 5- year visit (the two statistically significant factors identified through the stepwise regression procedure), the one-year adjusted difference in axial elongation between the CL and spectacle groups remained small (0.03 mm) and was no longer statistically significant (p=0.11).
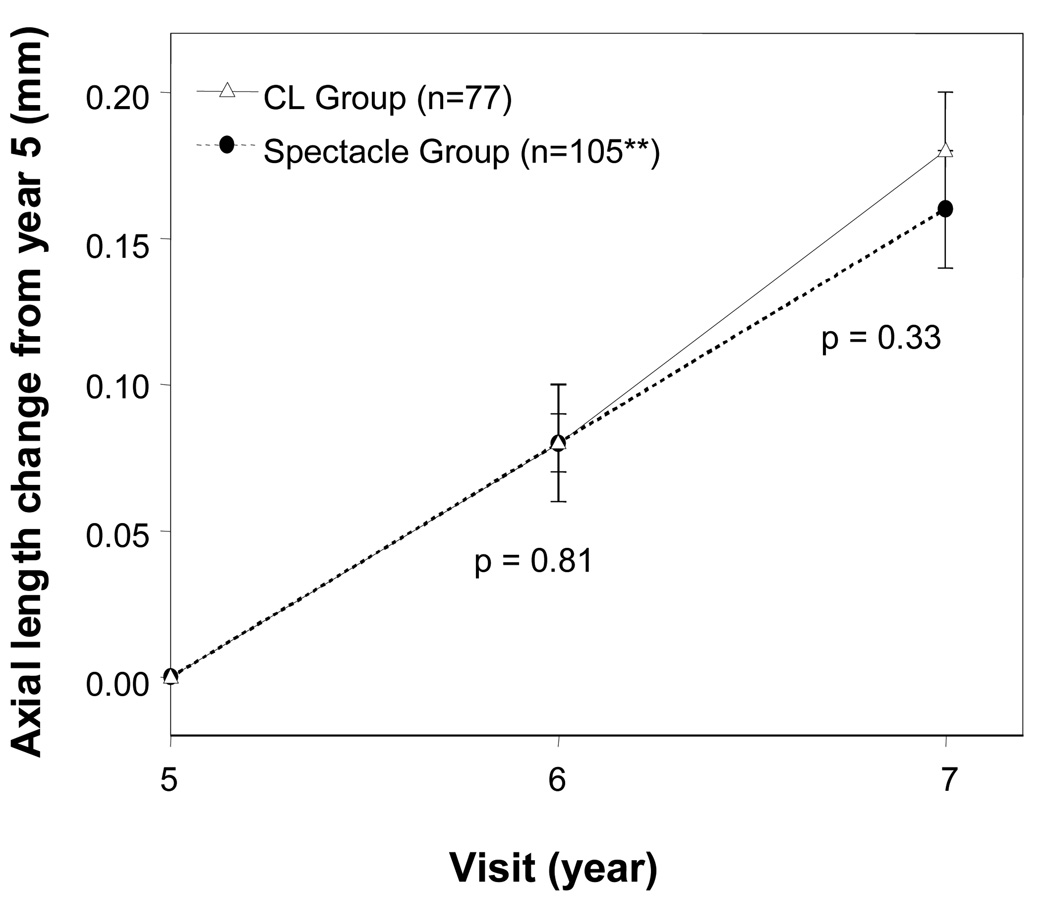
Two-Year Axial Elongation in the Subset of Children
Unadjusted axial elongation from the subset of 183 children is shown in Figure 3. Unlike the higher myopia progression observed in the CL versus spectacle group, one- and two-year axial elongation were similar in the two lens groups. One-year axial elongation (between the 5- and 6-year visits) was 0.08 mm in both groups, and two-year axial elongation (between the 5- and 7-year visits) was 0.18 ± 0.15 mm in the CL group and 0.16 ± 0.19 mm in the spectacle group. After adjusting for age, ethnicity, and average corneal curvature at the 5-year visit, two-year axial elongation (between the 5- and 7- year visits) remained similar in the CL and spectacle subsets.
Figure 3.
Two-year axial length change (mm) between Years 5 and 7 by lens group. Based on values from the two-year subset, i.e., participants who were classified between years 5 and 6 and remained in the same lens type between years 6 and 7. *Axial length data unavailable on one participant. Error bars= Standard error (SE).
Change in Corneal Radii in the One-Year Cohort and Two-Year Subset
Average changes in corneal curvature were minimal and similar in both the CL and spectacle groups (Table 2). Minimal changes also were observed in horizontal and vertical corneal curvature regardless of lens group. No significant differences were found between girls and boys with respect to changes in average, horizontal, or vertical corneal curvature. In addition, in the two-year subset, changes in corneal curvature between the 5- and 6- or between the 5- and 7- year visits were similar between CLs and spectacle groups.
DISCUSSION
Our major finding is a small, statistically significant but clinically inconsequential increase in progression of myopia among children who switched to soft CLs compared to those who remained in spectacles (−0.14 D after one year in the main cohort and −0.27 D after two years in the two-year subset). This difference was much smaller than the difference reported by Fulk et al2, who found one-year myopia progression of −0.74 D in the 19 children who had switched to CLs compared to −0.25 D in the 24 children remaining in spectacles.
Unlike the Fulk et al study, our data do not show significant axial elongation or corneal steepening that might account for the increased myopia observed with CLs. Even though the COMET main outcome data showed a high correlation between myopia progression and axial elongation (0.86 in children wearing PALs and 0.89 for children wearing SVLs for three years7), the correlation in this subset of children was not as high and thus axial elongation cannot account for the increased progression in the CL group. It is possible that COMET did not measure factors that might help to explain the difference in myopia progression between groups. For instance, we cannot rule out increases in corneal thickness8,9 or changes in refractive index that may have resulted from CLs. In any case, such changes are likely to be small.
Results from a recent, randomized clinical trial evaluating myopia progression and axial elongation in children assigned to either CLs or spectacle lenses agree with the current report of no significant differences between lens groups in axial length and corneal curvature.4 Myopia progression in that study was, on average, 0.06 D per year greater for the CL than the spectacle group, a smaller difference than found in the COMET cohort. Unlike in COMET, there was a statistically significant interaction between time and treatment (p = 0.002) but after 3 years the adjusted difference between lens groups was not significant.
Interpretation of these COMET results must consider potential limitations. The cohort used in these analyses is a subset of the original COMET cohort, and thus these children were not randomly assigned to wearing CLs or spectacles after the clinical trial phase ended. The ability of the participants to select their own lens type raises concerns about the potential biases that could result from self selection. For example, we found that more girls than boys chose to wear CLs. Even though girls have shorter eyes and steeper corneas, myopia progression was similar in both gender groups in the present study, indicating that these characteristics should not have affected the differences observed in progression between the CL and spectacle groups. To reduce the influence of potential confounding variables, data analyses were adjusted for those factors found to influence myopia progression. This approach reduces, but does not eliminate the effect that can result from unknown factors or those that were not evaluated. In addition, we had no information on factors such as CL material, base curves, wearing time, or power of the lens, any of which might have influenced myopia progression.
In summary, a statistically significant but clinically inconsequential difference in myopia progression was found after children switched from glasses to CLs. Many children perceive benefits of CLs such as overall satisfaction, improved appearance, and ease of participation in activities.10 Our data also can be used to reassure parents that CLs do not cause an important increase in axial growth of the eye, which is the major factor contributing to retinal or other complications of myopia.
ACKNOWLEDGMENTS
Supported by National Eye Institute Grants EY11805, EY11756, EY11754, EY11740, EY11752, EY11755 and by Essilor of America, Marchon Eyewear, Marco Technologies, and Welch Allyn.
COMET StudyGroup
Study Chair: J Gwiazda (Study Chair/PI); T Norton; K Grice (9/96-7/99); C Fortunato (8/99-9/00); C Weber (10/00-8/03); A Beale (11/03-7/05); D Kern (8/05-8/08); R Pacella (10/96-10/98).
Coordinating Center: L Hyman (PI); MC Leske (until 9/03); M Hussein (until 10/03); LM Dong (12/03-present); E Schoenfeld (until 9/05); L Dias (6/98-present); R Harrison (4/97-3/98); J Thomas (12/00-04/04); M Wasserman (05/04-07/06); Y Chen (10/06-1/08); C Rau (2/99-11/00); E Schnall (11/97-11/98); W Zhu (until 12/06); K Zhang (04/06-present); Y Wang (1/00-12/05); A Yassin (1/98-1/99); L Passanant (2/98-12/04); M Rodriguez (10/00-present); A Schmertz (1/98-12/98); A Park (1/99-4/00); P Neuschwender (until 11/99); G Veeraraghavan (12/99-4/01); A Santomarco (7/01-8/04); L Sisti (4/05-10/06); L Seib (6/07-present).
National Eye Institute: D Everett (Project Officer).
Clinical Centers
University of Alabama at Birmingham School of Optometry
W Marsh-Tootle (PI); K Niemann (9/98-present); C Baldwin (10/98-present); K Becker (7/99-3/03); J Raley (9/97-4/99); A Rawden (10/97-9/98); N Harris (3/98-9/99); T Mars (10/97-3/03); R Rutstein (until 8/03).
New England College of Optometry
D Kurtz (PI until 6/07); E Weissberg (6/99-present; PI since 6/07); B Moore (until 6/99); R Owens; J Smith (1/01-8/08); S Martin (until 9/98); J Bolden (10/98-9/03); B Jaramillo (3/00-6/03); S Hamlett (6/98-5/00); L Vasilakos (2/02-12/05); S Gladstone (6/04-3/07); C Owens (6/06-present); P Kowalski (until 6/01); J Hazelwood (7/01-803).
University of Houston College of Optometry
R Manny (PI); C Crossnoe (until 5/03); K Fern; S Deatherage (until 3/07); C Dudonis (until 1/07); S Henry (until 8/98); J McLeod (9/98-8/04; 2/07-5/08); M Batres (8/04-1/06); J Quiralte (1/98-7/05); G Garza (8/05-1/07); G Solis (3/07-present); A Ketcham (6/07-present).
Pennsylvania College of Optometry
M Scheiman (PI); K Zinzer (until 4/04); K Pollack (11/03-present); T Lancaster (until 6/99); T Elliott (until 8/01); M Bernhardt (6/99-5/00); D Ferrara (7/00-7/01); J Miles (8/01-12/04); S Wilkins (9/01-8/03); R Wilkins (01/02-8/03); J N Smith (10/03-9/05); D D’Antonio (2/05-5/08); L Lear (5/06-1/08); A Grossman (8/01-11/03); M Torres (7/97-6/00); H Jones (8/00-7/01); M Madigan-Carr (7/01-3/03); T Sanogo (7/99-3/03); J Bailey (until 8/03).
Data and Safety Monitoring Committee: R Hardy (Chair); A Hillis; D Mutti; R Stone; Sr. C Taylor.
REFERENCES
- 1.Walline JJ, Jones LA, Rah MJ, Manny RE, Berntsen DA, Chitkara M, Gaume A, Kim A, Quinn N the CLIP Study Group. Contact Lenses in Pediatrics (CLIP) Study: chair time and ocular health. Optom Vis Sci. 2007;84:896–902. doi: 10.1097/OPX.0b013e3181559c3c. [DOI] [PubMed] [Google Scholar]
- 2.Fulk GW, Cyert LA, Parker DE, West RW. The effect of changing from glasses to soft contact lenses on myopia progression in adolescents. Ophthalmic Physiol Opt. 2003;23:71–77. doi: 10.1046/j.1475-1313.2003.00094.x. [DOI] [PubMed] [Google Scholar]
- 3.Horner DG, Soni PS, Salmon TO, Swartz TS. Myopia progression in adolescent wearers of soft contact lenses and spectacles. Optom Vis Sci. 1999;76:474–479. doi: 10.1097/00006324-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Walline JJ, Jones LA, Sinnott L, Manny RE, Gaume A, Rah MJ, Chitkara M, Lyons S. A randomized trial of the effect of soft contact lenses on myopia progression in children. Invest Ophthalmol Vis Sci. 2008;49:4702–4706. doi: 10.1167/iovs.08-2067. [DOI] [PubMed] [Google Scholar]
- 5.Hyman L, Gwiazda J, Marsh-Tootle WL, Norton TT, Hussein M. The Correction of Myopia Evaluation Trial (COMET): design and general baseline characteristics. Control Clin Trials. 2001;22:573–592. doi: 10.1016/s0197-2456(01)00156-8. [DOI] [PubMed] [Google Scholar]
- 6.Gwiazda J, Marsh-Tootle WL, Hyman L, Hussein M, Norton TT. Baseline refractive and ocular component measures of children enrolled in the correction of myopia evaluation trial (COMET) Invest Ophthalmol Vis Sci. 2002;43:314–321. [PubMed] [Google Scholar]
- 7.Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, Leske MC, Manny R, Marsh-Tootle W, Scheiman M. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–1500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 8.Oh JH, Yoo C, Kim YY, Kim HM, Song JS. The effect of contact lens-induced corneal edema on Goldmann applanation tonometry and dynamic contour tonometry. Graefes Arch Clin Exp Ophthalmol. 2009;247:371–375. doi: 10.1007/s00417-008-0954-9. [DOI] [PubMed] [Google Scholar]
- 9.Liu Z, Pflugfelder SC. The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity. Ophthalmology. 2000;107:105–111. doi: 10.1016/s0161-6420(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 10.Walline JJ, Jones LA, Chitkara M, Coffey B, Jackson JM, Manny RE, Rah MJ, Prinstein MJ, Zadnik K. The Adolescent and Child Health Initiative to Encourage Vision Empowerment (ACHIEVE) study design and baseline data. Optom Vis Sci. 2006;83:37–45. doi: 10.1097/01.opx.0000195566.94572.eb. [DOI] [PubMed] [Google Scholar]