Abstract
Breast pain or mastalgia is the common symptom in the breast. The two most common concerns of patients presenting with mastalgia are: the fear that breast pain is a symptom of breast cancer and the presence of severe pain that affects a woman’s quality of life. Breast pain requires thorough assessment and should be investigated in the same manner as any other breast symptom. We conducted a systematic review of treatment for breast pain. We searched various reviews, randomized controlled trial, and observational studies over Pubmed and Medline via internet. Searches were carried out on MEDLINE (1950–present), EMBASE (1980–present), and CINAHL (1981–present) using the NHS Evidence Healthcare Databases Advanced Search interface. A further search was also carried out on Cochrane Database of Systematic Reviews (issue 12 of 12, Dec 2011) and Central Register of Controlled Trials (issue 4 of 4, Oct 2011). If no abnormality is found in the breast on assessment, then a combination of reassurance, breast support brassiere, and topical NSAID gel massage are usually effective. Antiestrogen (centchroman/tamoxifen) therapy for 3 to 6 months is the second-line treatment of choice. Danazol may be used in resistant cases. Gamma-linolenic acid or evening primrose oil though commonly prescribed is not effective.
Keywords: Mastalgia, Cyclical mastalgia, Noncyclical mastalgia, Centchroman, Danazol, Diclofenac gel
Introduction
Mastalgia is the most common breast symptom in patients attending a breast clinic [1]. Approximately 60 to 70 % of women experience some degree of breast pain at some stages of their lives, and in 10 to 20 % of cases, it is severe [2, 3]. The two most common concerns of patients presenting with mastalgia are: the fear of breast cancer and the presence of severe pain affecting quality of life. The majority of patients with mastalgia can be managed with reassurance and simple drugs. The most important responsibility of the breast specialist is to convincingly rule out cancer and assiduously reassure the patient. Mastalgia is often associated with breast nodularity that may be tender or without a discrete lump. Some amount of breast nodularity and mastalgia are found in normal population [3, 4].
Classification of Breast Pain
Cyclical Mastalgia
Cyclical breast pain occurs 1 to 2 weeks prior to menses. The pain is commonly felt diffusely and bilaterally, with some radiation to the upper arm and axilla. It can be more severe in one breast than the other and it is relieved by the onset of menstrual flow. These patients are usually aged between 30 and 40. Cyclical mastalgia may have spontaneous resolution in up to 22 % of patients and persists in up to 65 % of patients after treatment [4]. However, it can resolve with a hormonal event such as pregnancy or menopause, and because of this, it is postulated that cyclical mastalgia is due to hormonal stimulation of breast parenchyma particularly at the end of the luteal phase of the menstrual cycle [5]. For many, it may be a lifelong suffering to abate at menopause if left untreated [4].
Noncyclical Mastalgia
It is usually unilateral and localized to a particular quadrant of the breast. Patients are usually older, in their 40s or 50s, and are often perimenopausal [5]. There are several causes of noncyclical mastalgia including cysts, periductal mastitis, stretching of Cooper’s ligaments, traumatic fat necrosis, Mondor’s disease, diabetic mastopathy, and neoplasia [3, 5]. Noncyclical mastalgia can resolve without treatment in up to 50 % of cases but can also be more difficult to treat [3].
Finally, non-breast pain can mimic mastalgia. Common causes of chest wall pain include costochondritis (Teitze’s disease), referred nerve root pain as in cervical spondylitis, and herpes zoster. Non-chest wall pain can arise from diverse causes such as ischemic heart disease, biliary pain, and peptic ulcer [5, 6].
Etiology of Mastalgia
Endocrine Abnormalities
Three main theories have emerged regarding etiology of painful nodular breasts:
Increased estrogen secretion from the ovary
Deficient progesterone production
Hyperprolactinemia
The studies of serum hormones levels do not support the first two theories, as hormonal levels were found to be similar in patients and controls [7]; however, study from France showed a significantly depressed level of luteal progesterone, thus supporting the second theory [8].
Peters et al. found that the patients with mastalgia had a significantly greater rise in prolactin compared with the controls [9]. A study at Cardiff Mastalgia Clinic also reported a rise in stimulated prolactin level in women with mastalgia [10].
Water Retention
At the Cardiff Mastalgia Clinic, the total body water was estimated using radioactive water (D2O) in mastalgia patients and asymptomatic normal women. The results showed that there were no significant differences in water gain between the 5th and 25th days of menstrual cycle in mastalgia patients compared to normal controls [10]. So it was concluded that simple retention of body water was not associated with breast pain [11].
Psychoneurosis
Astley Copper suggested that mastalgia patients were neurotic. Using Middlesex Hospital Questionnaire (MHQ), psychoneurotic profiles of 300 patients with mastalgia'(cyclical and noncyclical) and 156 patients with varicose veins were tested. The MHQ scores of mastalgia patients were significantly lower than those of psychiatric patients, thus showing no component of psychoneurosis in occurrence of mastalgia [12].
Caffeine and Methylxanthine
It is suggested that overstimulation of breast cells may occur due to interference with adenosine triphosphate degradation by methylxanthine. Minton et al. reported that caffeine restriction produced improvement in symptoms; however, these studies were uncontrolled [13]. Subsequent randomized trials have failed to demonstrate a benefit of caffeine restriction in relieving mastalgia [14].
Miscellaneous Factors
Peters et al. observed that breast pain was associated positively with degree of ductal dilatation, as demonstrated by ultrasound scan [15].
Clinical Assessment and Investigations
A history and examination will point to the diagnosis in most cases. A prospective pain diary is extremely helpful, as patient’s recollection of events can be inaccurate and incomplete.
Investigations
A mammogram should be performed for women aged 35 years and above. Ultrasound examination is helpful if there is a clinical palpable abnormality or if the patient presents with localized noncyclical pain. Ultrasound of the whole breast may be performed depending on the expertise and resources available to the treating physician. Frequently reported cysts and other benign lesions on X-ray mammogram and ultrasound should not worry the patients unnecessarily in the absence of a discretely palpable lump. Other investigations may be necessary to complete the “triple test” if a lump is present such as image-guided breast biopsy of any suspicious lesion or cytology of serous or bloody nipple discharge.
Management
The following measures can be applied to both noncyclical and cyclical mastalgia.
Daily Breast Pain Charting
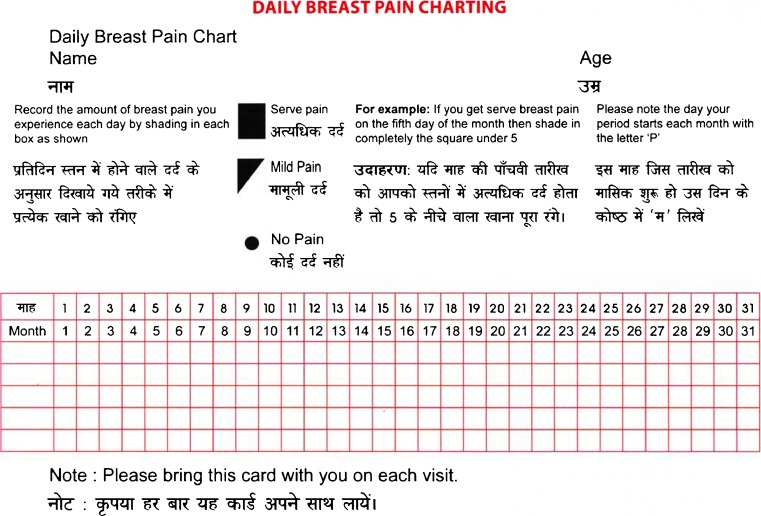
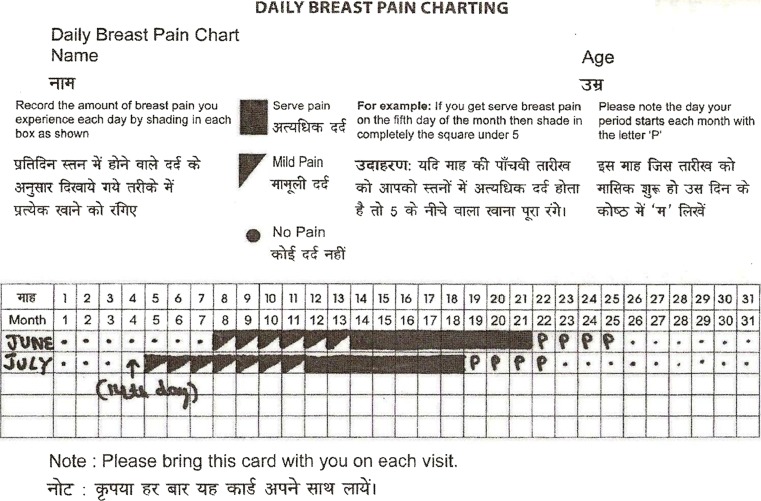
Patients are explained about hormonal changes with menstruation and its relation with mastalgia and requested to record their daily pain experience on a chart (Fig. 1). The days with menses are marked with letter “P” (Fig. 2).
Fig. 1.
A daily breast pain chart
Fig. 2.
A typical pain pattern of cyclical mastalgia with premenstrual exacerbation
The severity of pain is also noted on a visual analogue scale (VAS, also called visual linear analogue). VAS is usually a horizontal line, 10 cm in length, anchored by word descriptors at each end (Fig. 3). The patient marks on the line below, the point that they feel represents their perception of pain. The VAS score is determined by measuring in millimeter from the left hand end of the line to the point that the patient marks. On this VAS, the 0 indicates no pain and 10 indicate very severe excruciating pain in the breast. Most mastalgia experts consider any pain of ≥3 on a VAS of 0 to 10 to be significantly severe to require therapy [16].
Fig. 3.
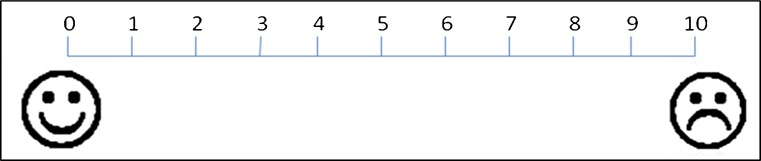
A “Visual Linear Analogue Scale for measuring pain”
Reassurance
A woman who has no abnormality detected on clinical assessment and triple test can be reassured that the possibility of an undetected breast malignancy is less than 5 %. Majority of women feel comfortable and at ease once cancer is ruled out [5].
Physical measures: It is estimated that up to 70 % of women wear improperly fitted bras. Thus, it is important to ensure that the patient is fitted with sufficiently supportive and well-fitting brassiere [17]. It is especially useful in women endowed with large mammary glands. In a randomized trial of 200 women with mastalgia, 100 women received treatment with danazol and the other 100 were asked to wear sports brassieres for 12 weeks. The danazol group had 58 % relief of symptoms (with drug side effects in 42 %), while in the brassiere group, 85 % had relief of symptoms with improved lifestyle [17]. Sports garments relieve pain by reducing the overstretching of the Cooper’s ligament.
Relaxation techniques: Four weeks of relaxation therapy was reported to provide relief in 60 % of patients [18].
Vitamins: There is no convincing evidence to support the use of vitamins in treatment of mastalgia; however, vitamin B1, B6, and E are all used by clinicians. These have no role and should not be misused [23]. A recent meta-analysis described that long-term use of vitamin E may increase risk of hemorrhagic stroke (RR = 1.22; 95 % confidence interval 1 to 1.48; p = 0.045) [19].
Evening primrose oil: Although evening primrose oil has been used in past with some success in a few trials [20, 21], meta-analysis revealed that the benefit in pain reduction is similar to that achieved by placebo [22]. But some centers still prefer to use evening primrose oil for breast pain.
Simple Medications
Nonsteroidal anti-inflammatory medications can be effective in up to 80 % of women and their usefulness is often underestimated. Diclofenac gel applied as local massage to painful areas of breast has been found to be more effective than placebo gel and ibuprofen gel in randomized trials [23]. Colak studied the effects of topical diclofenac gel on cyclic and noncyclical mastalgia in 108 patients: 60 with cyclic (group I) and 48 with noncyclical (group II). Patients within each group were randomized to diclofenac gel or placebo cream, three times daily for 6 months. The pain score decreased significantly in diclofenac gel group compared to placebo. The benefit was seen in both cyclical and noncyclical breast pain. No side effect was reported in any group [23].
Hormone Replacement Therapy and Breast Pain
The response of oral contraceptives and hormone replacement therapy (HRT) on breast pain is variable in different individuals. While some women may develop breast pain on starting oral pills or HRT, others may feel relieved of their mastalgia with these medications. Studies of low-dose oral contraceptives (20 μg ethinyl estradiol) have found no increase in breast symptoms compared with placebo [24].
Topical, oral, and parenteral progestogens have been studied for treatment of breast pain with variable results. The oral progestogens, lynestrenol, and promegestone administered during the luteal phase significantly improved breast pain in 66 to 80 % of women [25, 26]. No systematic review or RCTs could be found to assess the effects of HRT for treating mastalgia. HRT usually increases the risk of breast pain; hence, no trial on HRT for therapy of mastalgia has been conducted. Due to the risk of side effects, hormonal medications should only be used for 2 to 6-month periods.
Tamoxifen: Tamoxifen at a dose of 10 mg daily is reported to relieve cyclical mastalgia in 70 to 90 % and noncyclical mastalgia in 56 % of cases. Side effects at this low dose for 3 months are minimal and include irregular periods and hot flushes. Tamoxifen is the drug of choice for mastalgia in most breast clinics in the West [27]. The patient must be told that tamoxifen is not being given for cancer.
Centchroman: Centchroman or ormeloxifene (marketed as SAHELI by Hindustan latex company India) is a nonsteroidal antiestrogen agent. It is used as “once a week contraceptive pill” which selectively binds with estrogen receptor in the breast and endometrium. This molecule was developed at the Central Drug Research Institute, Lucknow. At the All India Institute of Medical Sciences breast clinic, centchroman has been used for control of mastalgia. Initially a dosage of 30 mg on alternate days was employed in 19 patients. The frequency of dosage was later increased to once daily, as there were no major side effects seen and some women missed doses with alternate day therapy. Hence to improve compliance and effect, in latter part of study, it was given as 30 mg once a day to 23 patients. In a randomized trial of 81 patients (42 randomized to centchroman and 39 to danazol), combining both alternate and daily dosage, centchroman was found to have response of 89.7 % (response being defined as number of women achieving reduction of pain to less than or equal to 3 on VAS of 0 to 10) whereas cases receiving danazol achieved a response of 69.4 % at 12 weeks of therapy [28]. A greater proportion of women in centchroman group continue to enjoy pain-free life even after the drug was stopped, suggesting a longer carry over effect. It is also cheaper than tamoxifen [29]. Moreover, there are no reports of endometrial carcinoma or thromboembolic side effects with long-term use of centchroman as compared to tamoxifen [30]. Patients should be actively informed that centchroman is not being used for contraceptive purpose.
Danazol: It is an antigonadotrophin agent. Danazol is a testosterone derivative and has mild androgenic effect [31]. Current practice in India is to start treatment at 50 mg once daily and then increase to 50 mg twice daily if the response is not complete. The maintenance dose should be given for at least 3 months [32]. In the West, the recommendation is to use a maintenance dose of 100 mg daily or alternate days. The common side effects with danazol are hair growth, weight gain, and menstrual irregularities; hence its use should be reserved for cases of severe mastalgia who have failed on 3–6 months of tamoxifen and centchroman treatment. It is contraindicated during pregnancy due to possible teratogenic effect [33, 34].
Gamolenic acid (GLA): An essential polyunsaturated fatty acid is present in large quantities in evening primrose oil. Women with cyclical mastalgia have been found to have low levels of the metabolites of GLA in the plasma. A multicenter study randomized patients into four groups: (1) GLA and antioxidants, (beta carotene, vitamin c, vitamin B6, zinc, and niacin); (2) placebo, fatty acid, and antioxidants; (3) GLA and placebo antioxidants; and (4) placebo fatty acids. The investigators concluded that GLA efficacy was similar to placebo, regardless of whether antioxidant vitamins were added or not [35].
Bromocriptine: It is a dopamine agonist and stimulates the dopaminergic receptors in the anterior pituitary and blocks the release of prolactin. It is administered at a dose of 2.5 mg twice daily, about 47 to 88 % of patients are reported to have a significant long-lasting relief in breast pain. In a meta-analysis, bromocriptine was found to offer a reduction in mean pain score of 16.31 as compared to placebo [22]. Most mastalgia experts have stopped using bromocriptine because of severe side effects, the commonest being nausea, vomiting, and dizziness.
Lisuride maleate: It is an ergot derivative. It is a dopamine agonist which binds to prolactin receptors. A double blind placebo-controlled randomized study evaluated lisuride therapy for mastalgia at a dose of 0.2 mg/day and found it to be an effective and well-tolerated treatment. Its key advantage over bromocriptine is the lower prevalence of side effects with lisuride [36]. It is not widely used and should be used with caution as it has been associated with pathological gambling and hypersexuality.
Goserelin (LHRH analog): Goserelin in a placebo-controlled randomized trial of 147 premenopausal cases showed a significant reduction in mean days with severe pain from 17.6 to 5.9, i.e., 67 % reduction [37]. It is effective in recurrent mastalgia and mastalgia not responding to other hormonal therapies.
Trigger point pain: In some women, pain is localized to one tiny spot of the breast. If imaging of breast does not reveal any organic lesion, this trigger point may be treated by injection of lignocaine 2 % (2 ml) followed by an injection of long-acting steroid (e.g., triamcinalone acetate 1 ml solution).
Surgery: There is very limited role for surgery in treatment of mastalgia. Surgery can be useful in selected patients with a discrete, small trigger spot whose symptoms may be relieved by excision of spot [38]. For generalized mastalgia, mastectomy is not advised. If patient insist on mastectomy, a careful psychological assessment is advised prior to agreeing to surgery [39]. Patients should be informed of possible complications inherent of reconstructive surgery and warned that in 50 % cases their pain will not be improved [40]. Decision of surgery in mastalgia is a bilateral one after extremely careful and repeated observations usually on the insistence of the patient.
Summary
Breast pain requires thorough assessment and exclusion of an organic cause. If associated with a lump, cancer must be excluded by triple assessment. If no abnormality is found on assessment, then a combination of high quality reassurance, regular clinical assessments at follow-up, breast support garment and diclofenac gel are usually effective. Surgery is not helpful in treatment of these patients. For more severe cases, antiestrogen (centchroman/tamoxifen) is the drug of choice. LHRH analogues (Goserelin) injection should be reserved for severe refractory mastalgia. Vitamins, diuretics, evening primrose oil, and gamolenic acid are obsolete and not effective.
Acknowledgments
Conflict of Interest
None
References
- 1.Barton MB, Elmore JG, Fletcher SW. breast symptom among women enrolled in a health maintenance organization: frequency, evaluation and outcome. Ann Intern Med. 1999;130:651–657. doi: 10.7326/0003-4819-130-8-199904200-00005. [DOI] [PubMed] [Google Scholar]
- 2.Ader DN, South-Paul J, Adera T, Deuster PA. Cyclical mastalgia: prevalence and associated health behavioral factors. J Psychosom Obstet Gynaecol. 2001;22:71–76. doi: 10.3109/01674820109049956. [DOI] [PubMed] [Google Scholar]
- 3.Mansel RE, Webster DJT, Sweetland HM. Breast pain and nodularity. In: Mansel RE, Webster DJT, Sweetland HM, editors. Benign disorders and disease of the breast. 3. Philadelphia: Saunders Elsevier; 2009. pp. 107–138. [Google Scholar]
- 4.Kumar S, Rai R, Das V, Dwivedi V, Kumar S, GG A. Visual analogue scale for assessing breast nodularity in non discrete lumpy breasts: the Lucknow Cardiff breast nodularity scale. The Breast. 2010;19:238–242. doi: 10.1016/j.breast.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Wisbey JR, Kumar S, Mansel RE, Preece PE, Pye JK, Hughes LE. Natural history of breast pain. Lancet. 1983;ii:672–674. doi: 10.1016/S0140-6736(83)92543-6. [DOI] [PubMed] [Google Scholar]
- 6.Smith RL, Pruthi S, Fitzpatrick LA. Evaluation and management of breast pain. Mayo Clin Proc. 2004;79(3):353–372. doi: 10.4065/79.3.353. [DOI] [PubMed] [Google Scholar]
- 7.Malarkey WB, Schrooeder LL, Stevens VC, James AG, Lanese RR. Twenty four hour preoperative endocrine profiles in women with benign and malignant breast disease. Cancer Res. 1977;37:4655–4659. [PubMed] [Google Scholar]
- 8.Sitruk-Ware R, Sterkers N, Mauvais-Jarvis P. Benign breast disease.1: hormonal investigation. Obstet Gynecol. 1979;53:457–460. [PubMed] [Google Scholar]
- 9.Peters F, Pickcardt CR, Zimmerman G. PRL, TSH and thyroid hormones in benign breast disease. Klin Wochenschr. 1981;59:403–407. doi: 10.1007/BF01698519. [DOI] [PubMed] [Google Scholar]
- 10.Kumar S, Mansel RE, Scanlon MF, Hughes LE. Altered responses of prolactin, luteinizing hormone and follicle stimulating hormone secretion to thyrotrophin releasing hormone/gonadotropin releasing hormone stimulation in cyclical mastalgia. Br J Surg. 1984;71:870–873. doi: 10.1002/bjs.1800711123. [DOI] [PubMed] [Google Scholar]
- 11.Preece PE, Richards AR, Owen GM. Mastalgia and total body water. Br Med J. 1975;4:498–500. doi: 10.1136/bmj.4.5995.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Preece PE, Mansel R, Hughes LE. Mastalgia: psychoneurosis or organic disease? Br Med J. 1978;I:9–30. doi: 10.1136/bmj.1.6104.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minton JP, Foeking MK, Webster DJT. Response of fibrocystic disease to caffeine withdrawal and correlation with cyclic nucleotides with breast disease. Am J Obstet Gynaecol. 1979;135:157. [PubMed] [Google Scholar]
- 14.Ernster VL, Mason L, Goodson WH. Effects of caffeine free diet on benign breast disease: a randomized trial. Surgery. 1982;91:263–267. [PubMed] [Google Scholar]
- 15.Peters F, Diemer P, Mecks O. Severity of mastalgia in relation to milk duct dilatation. Obstet Gynaecol. 2003;101(1):54–60. doi: 10.1016/S0029-7844(02)02386-4. [DOI] [PubMed] [Google Scholar]
- 16.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Heal. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 17.Hadi MS. Sports brassiere: is it a solution for mastalgia? Breast J. 2000;6:407–409. doi: 10.1046/j.1524-4741.2000.20018.x. [DOI] [PubMed] [Google Scholar]
- 18.Rosolowich V, Saettler E, Szuck B. Mastalgia. J Obstet Gynaecol Can. 2006;28(1):49–71. doi: 10.1016/S1701-2163(16)32027-8. [DOI] [PubMed] [Google Scholar]
- 19.Shurks M, Glynn RJ, Rist PM, Tzourio C, Kurth T. Effects of vitamin E on stroke subtypes: meta-analysis of randomized controlled trials. BMJ. 2010;341:c5702–1315. doi: 10.1136/bmj.c5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blommers J, de Lange-De Klerk ES, Kuik DJ. Evening primrose oil and fish oil for severe chronic mastalgia: a randomized, double-blind, controlled trial. Am J Obstet Gynecol. 2002;187:1389–1394. doi: 10.1067/mob.2002.127377a. [DOI] [PubMed] [Google Scholar]
- 21.Pashby NL, Mansel RE, Hughes LE. A clinical trial of evening primrose oil in mastalgia. Br J Surg. 1981;68:801. doi: 10.1002/bjs.1800681115. [DOI] [Google Scholar]
- 22.Srivastava A, Mansel RE, Arvinda N. Evidence-based management of mastalgia: a meta-analysis of randomized trials. Breast. 2007;16(5):503–512. doi: 10.1016/j.breast.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 23.Colak T, Ipek T, Kanik A. Efficacy of topical nonsteroidal antiinflammatory drugs in mastalgia treatment. J Am Coll Surg. 2003;196:525–530. doi: 10.1016/S1072-7515(02)01893-8. [DOI] [PubMed] [Google Scholar]
- 24.Coney P, Washenik K, Langley RG, Harrison DD. Weight change and adverse event incidence with a low-dose oral contraceptive: two randomized, placebo-controlled trials. Contraception. 2001;63:297–302. doi: 10.1016/S0010-7824(01)00208-6. [DOI] [PubMed] [Google Scholar]
- 25.Uzan S, Denis C, Pomi V, Varin C. Double-blind trial of promegestone (R 5020) and lynestrenol in the treatment of benign breast disease. Eur J Obstet Gynecol Reprod Biol. 1992;43:219–227. doi: 10.1016/0028-2243(92)90177-Z. [DOI] [PubMed] [Google Scholar]
- 26.Colin C, Gaspard U, Lambotte R. Relationship of mastodynia with its endocrine environment and treatment in a double blind trial with lynestrenol. Arch Gynakol. 1978;225:7–13. doi: 10.1007/BF00672829. [DOI] [PubMed] [Google Scholar]
- 27.Fentiman IS, Caleffi M, Brame K. Double-blind controlled trial of tamoxifen therapy for mastalgia. Lancet. 1986;8376:287–288. doi: 10.1016/S0140-6736(86)90825-1. [DOI] [PubMed] [Google Scholar]
- 28.Tejwani P, Srivastava A, Nerkar H, Dhar A, Hari S, Thulkar S, Chumber S, Kumar S. Centchroman regresses mastalgia: a randomized comparison with danazol. Indian J Surg. 2011;73(3):199–205. doi: 10.1007/s12262-010-0216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Srivastava A, Dhar A. Role of centchroman in regression of mastalgia and fibroadenoma. Word J Surg. 2007;31:1178–1184. doi: 10.1007/s00268-007-9040-4. [DOI] [PubMed] [Google Scholar]
- 30.Kamboj VP, Ray S, Dhawan BN. Centchroman. Drugs Today. 1992;28:227–232. [Google Scholar]
- 31.Greenblatt RB, Dmowske WP, Mhesh VB. Clinical studies with an antigonadotrophin—danazol. Fertil Steril. 1971;22:102–112. doi: 10.1016/s0015-0282(16)38045-1. [DOI] [PubMed] [Google Scholar]
- 32.Shukla HS, Kumar S. Benign breast disorders in nonwestern populations: Part II—benign breast disorders in India. World J Surg. 1989;13(6):746–749. doi: 10.1007/BF01658426. [DOI] [PubMed] [Google Scholar]
- 33.Asch RH, Greenblatt RB. The use of an impeded androgen danazol in the management of benign breast disorders. Am J Obstet Gynecol. 1971;127:130–134. doi: 10.1016/s0002-9378(16)33237-9. [DOI] [PubMed] [Google Scholar]
- 34.Mansel RE, Wisbey JR, Hughes LE. Controlled trial of the antigonadotrophin danazol in painful nodular benign breast disease. Lancet. 1982;1(8278):928–931. doi: 10.1016/S0140-6736(82)91932-8. [DOI] [PubMed] [Google Scholar]
- 35.Goyal A, Mansel RE. A randomized multicenter studies of gamolenic acid (Efamast) with and without antioxidant vitamins and minerals in the management of mastalgia. Breast J. 2005;11:41–47. doi: 10.1111/j.1075-122X.2005.21492.x. [DOI] [PubMed] [Google Scholar]
- 36.Lopez-Rosales C, Aguilar-Guerrero JA, Garcia-Moreno L. Treatment of premenstrual tension syndrome with lisuride maleate. Gynecol Obstet Mex. 1996;64:556–560. [PubMed] [Google Scholar]
- 37.Mansel RE, Goyal A, Preece P, Leinster S, Maddox PR. European randomized multicenter study of goserelin (Zoladex) in the management of mastalgia. Am J Obstet Gynecol. 2004;191(6):1942–1949. doi: 10.1016/j.ajog.2004.06.100. [DOI] [PubMed] [Google Scholar]
- 38.Steinbrunn BS, Zera RT, Rodriguez JL. Mastalgia: tailoring treatment to type of breast pain. Postgrad Med. 1997;102(5):183–184. doi: 10.3810/pgm.1997.11.369. [DOI] [PubMed] [Google Scholar]
- 39.Gateley CA, Mansel RE. Management of the painful and nodular breast. Br Med Bull. 1991;47(2):284–294. doi: 10.1093/oxfordjournals.bmb.a072470. [DOI] [PubMed] [Google Scholar]
- 40.Davies EL, Cochrane RA, Stansfield K, Mansel RE. Is there a role for surgery in the treatment of mastalgia? Breast. 1999;8(5):285–288. doi: 10.1054/brst.1999.0065. [DOI] [PubMed] [Google Scholar]