Abstract
Objectives
A healthcare decision-making support model and rule management system is proposed based on a personalized rule-based intelligent concept, to effectively manage chronic diseases.
Methods
A Web service was built using a standard message transfer protocol for interoperability of personal health records among healthcare institutions. An intelligent decision service is provided that analyzes data using a service-oriented healthcare rule inference function and machine-learning platform; the rules are extensively compiled by physicians through a developmental user interface that enables knowledge base construction, modification, and integration. Further, screening results are visualized for the self-intuitive understanding of personal health status by patients.
Results
A recommendation message is output through the Web service by receiving patient information from the hospital information recording system and object attribute values as input factors. The proposed system can verify patient behavior by acting as an intellectualized backbone of chronic diseases management; further, it supports self-management and scheduling of screening.
Conclusions
Chronic patients can continuously receive active recommendations related to their healthcare through the rule management system, and they can model the system by acting as decision makers in diseases management; secondary diseases can be prevented and health management can be performed by reference to patient-specific lifestyle guidelines.
Keywords: Clinical Decision Support Systems, Expert Systems, Knowledge Bases, Personal Health Records, Chronic Disease
I. Introduction
The incidence of chronic diseases around the world is increasing because of increased environmental pollution, incorrect eating habits, and a decrease in physical activity [1]. According to a survey conducted by the National Statistical Office, the three major causes of death in Korea in 2011 were malignant neoplasms, cerebral vascular disease, and heart disease, which had a high probability of being caused by chronic diseases, such as high blood pressure, hyperlipidemia, and diabetes. Further, chronic diseases accounted for 47.4% of the total cause of death. Therefore, it is necessary to provide appropriate guidelines to patients with chronic diseases and to warn them of the risks of such diseases [2].
Chronic diseases cannot be cured through treatment or surgery; however, continuous management is required by patients. They need to modify their daily guidelines and change their lifestyle habits. Therefore, communication is important between clinicians and patients. However, continuously providing customized guidelines is unrealistic because of the continuous changes in the state of patients. Hence, the u-healthcare system is drawing attention as a new system that uses wired and wireless networking information technology (IT) for health management and provides health services beyond the limitations of time and place. The u-healthcare system enables real-time delivery and analysis of data [3,4,5,6,7]. In this system, guidelines are developed for patient management by determining the state of patients through personal health records (PHRs). PHR is a tool to safely manage and record all medical and health information [8]. The proposed system uses Electronic Medical Records (EMRs) [9] in the hospital information system instead of paper sheets by introducing the concept of PHRs and IT in health institutions; the system provides clinical guidelines by considering the lifestyle information of chronic patients, which includes smoking status, exercise, and alcohol consumption, as well as clinical risk variables (total cholesterol, blood pressure, body mass index [BMI], etc.). Information exchange is performed using the standard protocol, Health Level 7 (HL7), of the medical information transmission interface, and mutual operability is ensured independent of a specific hospital system by enabling a linkage between independent systems [10,11].
A healthcare decision support system (HDSS) is the tool selected to provide guidelines, which uses the concept of a clinical decision support system (CDSS) appropriately modified with respect to chronic patients [12]. The HDSS is a newly named decision support system designed in this study. The purpose of the HDSS and the range of user groups are newly established; it mainly focuses on the health management of patients with chronic diseases to distinguish it from CDSS that underscores practicality in the clinical field. The core difference between a HDSS and a CDSS is the service user groups. A CDSS is a physician-centered system that shortens treatment time, prevents the risk of misprescription or misdiagnosis, and systematically focuses on healthcare providers including hospital management. On the other hand, a HDSS presents the unique characteristics of chronic disease patients by consistently providing health content tailored for patients with chronic conditions and aiming for supporting education on treatment and schedule management, in addition to self-management by checking patient behaviors and receiving feedback. A CDSS is an expert system in the medical field, and they are now gradually being used as intelligent computing systems to improve treatment efficiency. Such an intelligent computing system provides clinical guidelines and patients information to physicians and patients [5,13,14,15,16,17,18]. The HDSS could play a significant role in the health management of patients by enabling physicians to produce a customized patient clinical guide through PHR, which includes further lifestyle information; the developed guidelines consider patient feedback.
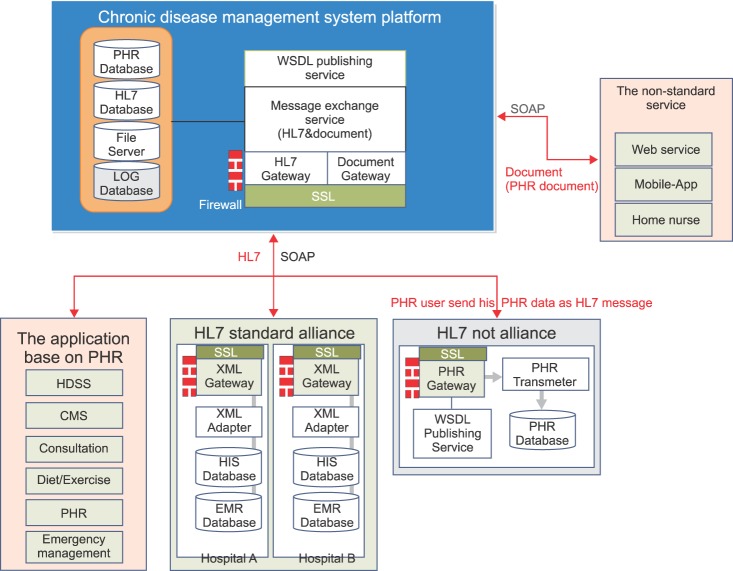
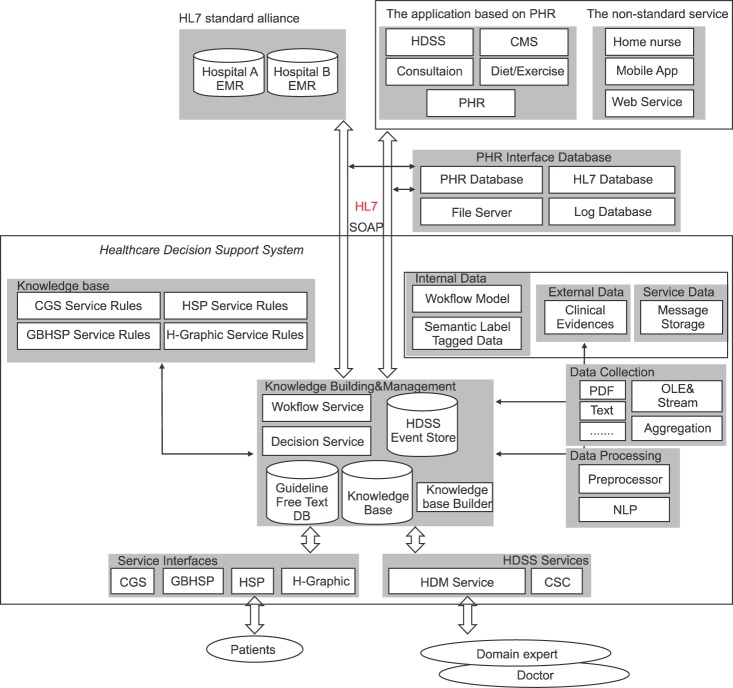
Figure 1 shows an interface roadmap for accessing the PHRs of patients in the HDSS. The interface roadmap provides high reusability and interoperability of message exchange of medical information, which is analyzed using a medical information messaging international standard, HL7. The HDSS knowledge builder and inference engine provide a Web service interface, which is based on the standard message transmission protocol. A knowledge base is developed using synchronous message communication based on the simple object access protocol and asynchronous communication for a stateful session. Then, the developed knowledge base is transmitted to a service terminal. The knowledge base has the characteristics of modifiability and it is developed such that it can incorporate new production, removal, modification, and integration of data; further, business logic is not hard-coded in the service implementation process. The service is based on the interface standard protocol for increasing availability, and the service interface can be produced according to various clients by publishing through Web service description language. Similarly, a linkage between different hospital information systems (HISs) of various hospitals is enabled through compliance with the standard protocol; thus, the usability of an independent system on a client platform is increased.
Figure 1.
Personal health record (PHR) approach standardized interface. HL7: Health Level 7, WSDL: Web service description language, SOAP: simple object access protocol, HDSS: healthcare decision support system, CMS: content management system, XML: extensible markup language, HIS: hospital information system, EMR: Electronic Medical Record.
The proposed system utilizes personal health information at the client level based on PHRs through the service interface to provide a wide range of services for patients. Chronic disease patient's PHRs used in the system are chiefly divided into three types. The first type of health information is the personal health management history recorded during health screening, and it is used to provide tailored clinical guidelines established by the identification of the illness and health status of patients based on surgeries, hospital visits, admissions, and prescriptions in the HDSS. Moreover, PHRs can be applied in consultation service for scheduling of screening and intelligent counseling on a patient's conditions based on health records. Likewise, the content management system (CMS) provides data on related disease management for patients according to their chronic illnesses. The second type of health information comprises medical records on lifestyle habits. The CMS keeps records of nutritional intake status including health functional foods and physical activity levels in a diet/exercise application, manages nutritional supply of chronic disease patients in order for them to sustain safe eating habits appropriate for unique chronic conditions, and it provides advice regarding exercise methods. Finally, the third type of health information is PHRs in the emergency medical system classifying allergy and idiosyncrasies. These data are applied in determining emergency situations according to the conditions of chronic disease patients in the emergency situation management of the HDSS. In addition, the information aids systematic management appropriate for different situations by classifying response measures suitable for each patient and emergency stages.
II. Methods
1. HDSS Services
The HDSS is configured by six services: HDSS management (HDM), chronic disease guideline support (CGS), gene-based health screening personalization (GBHSP), health screening personalization (HSP), health graphics (H-Graphic), and clinical sentence classification (CSC). The main objective of the HDSS is to support physicians in managing the knowledge base, to provide healthcare guidelines to be followed by patients suffering from chronic diseases in their daily lives, and to enable the management of screening scheduling. Moreover, the HDSS provides continuous guidelines for chronic disease management through the aforementioned six services, which is the main goal of the HDSS. The main contents of service in the HDSS are summarized as follows.
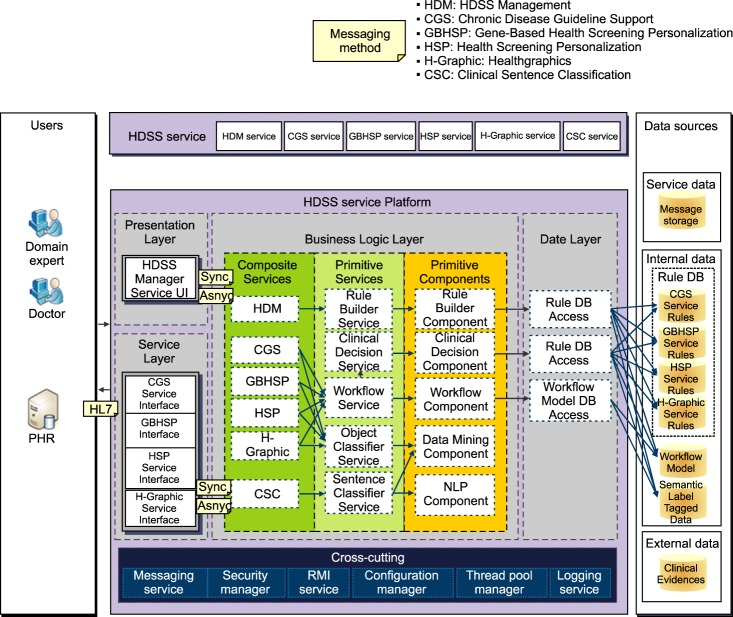
The HDSS is responsible for generating, deleting, and modifying the logic through a manager that manages the knowledge base developed by the decision-making logic of the HDSS. CGS determines the hypertensive phase, the diagnosis phase, the hyperlipidemia phase, diabetes, and other chronic diseases of patients based on screening information, habits, and other lifestyle information. Then, it proposes suitable guidelines for health management. GBHSP personalizes the future screening schedule on the basis of the patient genome code and other information stored in the hospital information record system. In addition, GBHSP provides screening scheduling for chronic diseases based on the possessed genome code of hyperlipidemia, dementia, stomach and colon cancer, etc. HSP is a service that personalizes screening schedules related to diseases, such as stomach cancer, liver cancer, and breast cancer, on the basis of patient information, such as examination date, age and sex, family, and virus diagnosis results, which is stored in the HIS. H-Graphic graphically expresses the screening information by the health examination items of an individual patient and enables patients to determine their health status intuitively. Finally, CSC is the service which receives free text of the medical domain as an input and performs the labeling of semantic tags. Figure 2 shows the model, which specifies each layer of the HDSS, for providing the HDSS. The HDSS service platform is configured into the presentation, service, business logic, and data layers.
Figure 2.
Service layer model. HDSS: healthcare decision support system, PHR: personal health record, NLP: natural language processing.
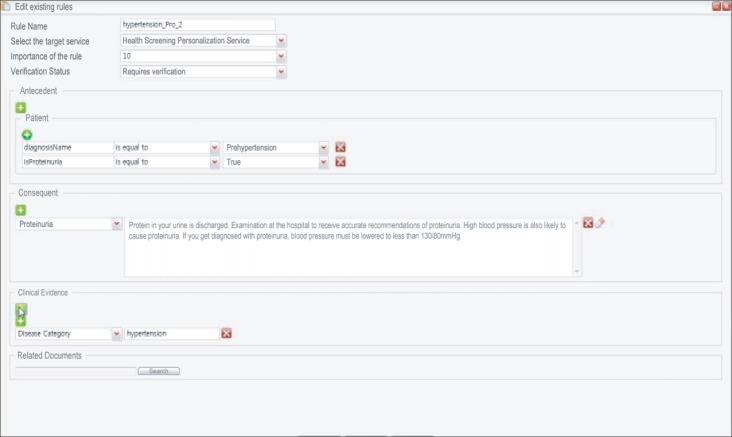
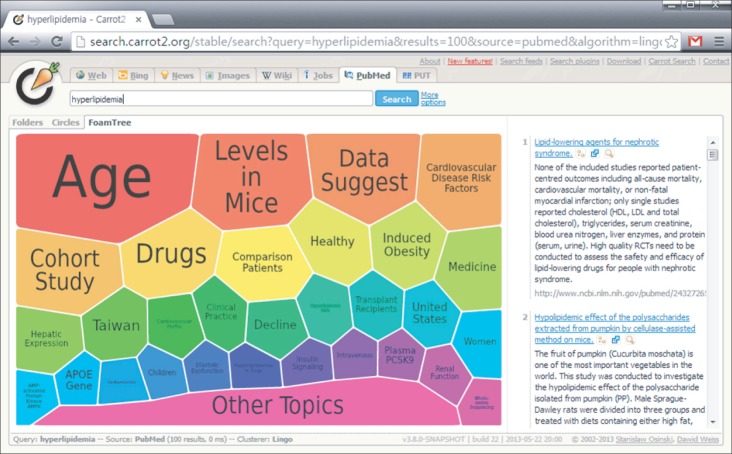
2. Presentation Layer
Diagnosis attributes and occurrence event values are received as input from medical domain experts and physicians, and an individual customized knowledge base is input/output through the user interface of the HDM service of the presentation layer of Web services. A deletion is performed on the basis of this modification. Medical domain experts can reflect new study results by finding a base rule for developing the knowledge base. The base rule is found using visualization techniques explained to physicians, and a method for producing visual effects through a graphical user interface used by clinicians for adding and deleting the rules [17,19]. The HDSS for providing a clinical base expresses the search results of PubMed by visualizing data, using the clustering engine of Carrot [20,21]. Figures 3 and 4 show the process of visualization by finding a base for hyperlipidemia using Carrot in the HDSS engine.
Figure 3.
Evidence representation techniques: hyperlipidemia entered in the search window.
Figure 4.
Evidence representation techniques: hyperlipidemia expressed in the form of a foam tree.
Search results are expressed using intuitive visualization data by searching for papers on each topic. Therefore, the user can easily build a knowledge base for problem areas, and the relevant guidelines can be input and modified effectively.
3. Service Layer
A service interface is provided, which is required for the Web-based service system of CGS, GBHSP, HSP, and H-Graphic.
4. Business Logic Layer
The key point of the HDSS is to provide a decision-making service with respect to content constituted by the events of a healthcare Web service domain. The core processor is implemented in the business logic layer, which can perform addition/deletion/modification of business logic that enables the decision-making process of the HDSS of each service. The synchronous/asynchronous messaging method of the presentation layer and the service layer is used for the linkage of the Web services, and a self-user interface controller may be provided.
1) Composite services
Composite services are constituted by HDM, which inputs the decision-making logic of the HDSS using a dedicated UI, CGS for providing PHR, health management guidelines for an information-based lifestyle, GBHSP for personalizing health examination scheduling based on the genome code using synchronous messaging, HSP for providing the service of personalizing health screening schedules based on personal information, H-Graphic for providing a summary of visual information based on the health screening items, and CSC for classifying medical text sentences.
2) Primitive services
The central module of primitive components and composite services provides a rule builder service, a clinical decision service, a workflow service, an object classifier service, and a sentence classifier service. The object classifier service can be used by each patient to classify the generated events and to use the same events in machine learning; the sentence classifier service includes the business logic of service, which can classify the meaning of sentences consisting of free text used in the field of medicine. The detailed contents of other services will be covered in subsection II-2-3 (Primitive components).
3) Primitive components
Primitive components include five important components: the rule builder component (RBC), the clinical decision component (CDC), the workflow component (WC), the data mining component (DMC), and the natural language processing component (NLPC). The RBC implements the business logic of the Web service to construct the knowledge base required for a healthcare decision-making service using a Web browser or a rich client platform application user interface.
CDC is a service module for constructing the inference logic. CDC receives the state value of patients as an input and generates an action guide message according to the input value. The action guide is generated using the rule database or the inference logic based on the knowledge base. The decision-making service is provided according to the business logic constructed through the HDM service, based on RBC after the domain event object is received as an input from the rule-based inference system. The state of various systems is recorded, and individual decision-making processes are executed by management of the session process of the decision-making Web services by a graph model. The graph model controls the flow of execution of the services required in session management in WC.
The workflow service is provided for medical/healthcare. The execution of the Web service process is controlled, which is required for the management of sessions, such as recording the dynamic state of patients. The DMC is the core of the learning process for the learning classification model or cluster model. The DMC is also a system required for the optimization and personalization of services by modeling of the domain knowledge contained in a log generated collectively by users through a machine learning algorithm and utilization of the results of learning, i.e., the domain event model. Finally, the NLPC provides the interface for the natural language processing and comprehension service for analyzing free text. The NLPC is configured by a natural language processing module (sentence splitter, part of speech, tagger, parser, and a proper noun recognizer) required for the extraction of knowledge from the collected unstructured data or free text.
5. Data Layer
The data layer is responsible for the linkage of the data source of the knowledge base rule database, workflow model, and semantic label tagged data of each service constructed through the business logic layer and the RBC. The business logic layer and the RBC are responsible for the construction of the knowledge base in the HDSS service platform and play a central role in the Web service.
III. Results
The construction of the HDSS system establishes manifold linkage and enables physicians to provide guidelines corresponding to the state of patients on a clinical basis by ensuring a standard patient information exchange among health institutions. The service is provided to chronic disease patients though each layer of the service platform and enables the creation of rules by physicians. Table 1 shows the roles of patients and physicians separately.
Table 1.
Roles of patients and physicians
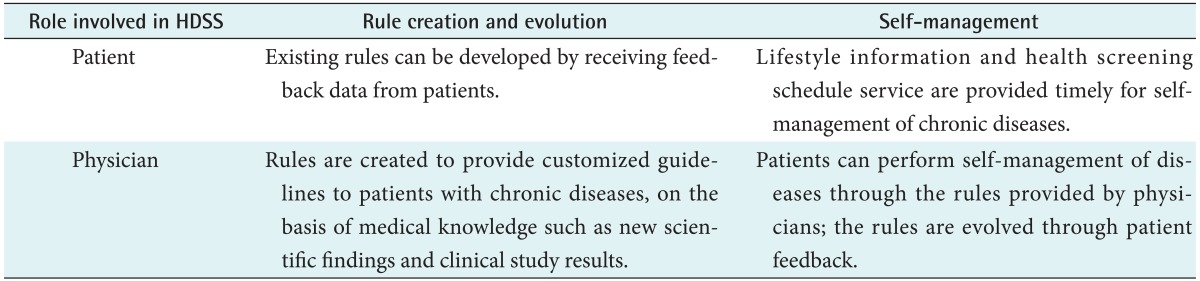
HDSS: healthcare decision support system.
Further, the HDSS provides a customized service to patients through multiple algorithms and a single variable, by constructing a deductive inference engine and providing service according to the state of patients.
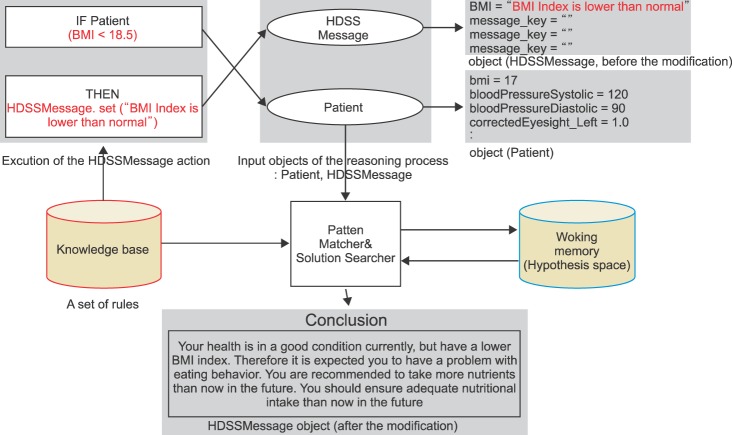
A knowledge base is a set of rules for reproducing the knowledge of a domain. The knowledge base outputs a conclusion message through a pattern matcher & solution searcher by combining with the attribute information of objects possessed by the entity of a patient. The pattern matcher generates a hypothesis by matching the variable value of objects (patients and HDSS message), input to the inference engine with the individual rules of the knowledge base. The working memory performs the networking of the generated hypotheses and increases the networking until further chaining is not possible; finally, the obtained hypotheses are combined as conclusions to produce the output.
The content set corresponding to the health state of a user is generated, and messages are provided. These messages are personalized and finally output to users through the user interface. Figure 5 shows the process of HDSS message output for patients with normal attributes except for lower levels of BMI.
Figure 5.
Rule-based reasoning process in the case of body mass index (BMI). HDSS: healthcare decision support system.
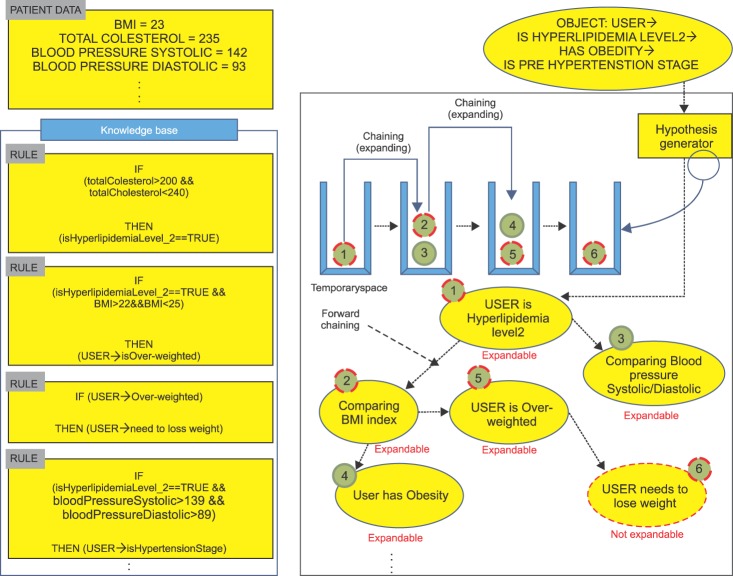
A rule-based inference has certain attributes, which lead to conclusions by deductive derivation of a new fact from the facts (attributes) of any object [22]. A single rule consists of 'antecedent' → 'consequent,' and the storage place of this set is the knowledge base. New hypotheses are generated by the application of rules; an inference is continued until further hypothesis is not possible. When an event generation score of probability is granted to an individual rule, a basis is provided, which enables the selection of an optimum conclusion candidate from various conclusions. The inference progress of the HDSS implements the inference process by the forward chaining method.
Figure 6 shows the increase in inference by the attribute values of BMI level, total cholesterol, and systolic/diastolic blood pressure.
Figure 6.
Example of a simple rule-based inference.
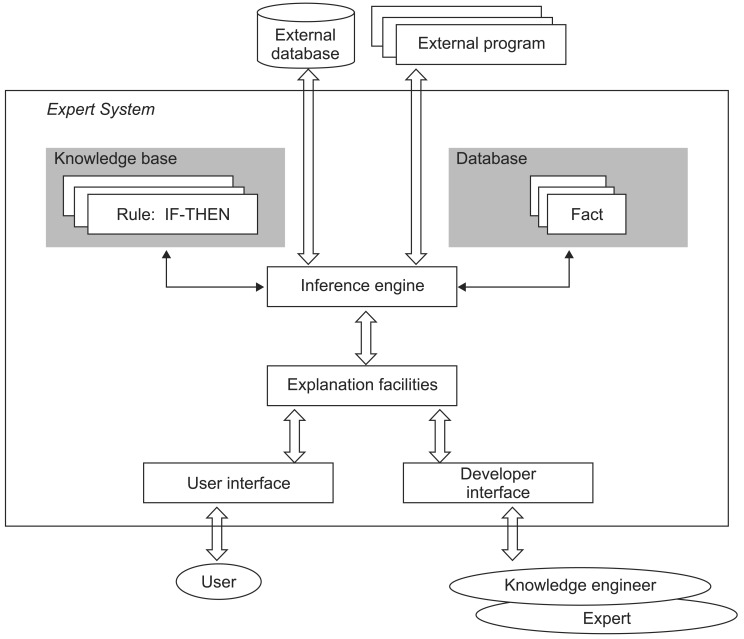
Figure 7 shows an expert system model based on a general rule [23]. Figure 8 shows the HDSS model constructed on the basis of a standard protocol, service construction, and a clinical evidence concept based on machine learning.
Figure 7.
Common structure of a rule-based expert system.
Figure 8.
Structure of healthcare decision support system (HDSS). HL7: Health Level 7, EMR: Electronic Medical Record, PHR: personal health record, CMS: content management system, SOAP: simple object access protocol, CGS: chronic disease guideline support, HSP: health screening personalization, GBHSP: gene-based health screening personalization, NLP: natural language processing.
The present HDSS system establishes data linkage among the HISs of different hospitals using the PHR interface HL7, which includes a standardized external data module. An external program was developed by using the service-oriented architecture method comprising service aspects by providing a HDSS; a CMS; medical counseling services; diet, nutrition, and exercise services; and individual health record information. Patient accessibility was increased by extension of the service through mobile applications, Web services, and home nurses in smart homes. In addition, the HDSS considered rules corresponding to the core service mentioned earlier. The database was also divided inside and outside based on service aspects, and the basic rules were processed, thereby ensuring the scalability and the flexibility of the HDSS. Finally, clinical decision-making was supported for each service user, patient, and physician through the customized interface of the HDSS engine.
IV. Discussion
The present system provides life-friendly guidelines to chronic patients by collecting information through the EMRs of HISs of different hospitals, thus overcoming limitations, such as patient information collection, rule construction, and modifications, faced by the CDSS used in traditional medical institutions. Chronic conditions are difficult to manage and prevent. The current system aids decision-making by analyzing the correlation of prescription, diagnosis, and treatment with their results. Meanwhile, the proposed system is meaningful in that it accurately identifies risk factors based on habit changes to suggest measures to tackle the problems by recommending practical guidelines for the daily lives of patients with chronic illnesses. The knowledge base was constructed to enable service users to follow the guidelines of health management of chronic patients during drug prescription by physicians and diagnostic procedures, such as surgery. Maximum effort was made to maximize convenience for physicians by considering study results and visualization methods while ensuring clinical evidence used in the formulation of the guidelines. A model was designed for use in various clinical environments by designing the HDSS structure using a simple rule-based expert system and a differentiated model. The rule-based expert system requires the user to obtain the knowledge of doctors and clinical domain experts and to create guidelines beforehand; further, it is difficult to access clinicians during the modification and addition of rules. The proposed HDSS system is intended to gradually improve its user interface by using an open visualization tool, such as Carrot, and to provide an intuitive interface for both physicians and patients. Future studies will be aimed at developing expert knowledge and formulating customized guidelines by studies supporting intuitive understanding, and obtaining information, such as IT affinity, and behavior patterns of patients along with an analysis of dietary patterns. Moreover, further studies will be performed to expand the usability of the new system by developing and advancing decision-making algorithms to establish intelligent HDSS considering all situational factors, including diet, physical activity level, allergy, emergency care, and other PHRs based on verification of the established system.
Acknowledgments
This work was supported by the Industrial Strategic Technology Development Program funded by the Ministry of Trade, Industry, and Energy, Korea (No. 10037283).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368(9548):1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 2.Statistics Korea. Cause of death statistics in 2011 [Internet] Daejeon, Korea: Statistics Korea; c2013. [cited at 2013 May 8]. Available from: http://kostat.go.kr. [Google Scholar]
- 3.Kim H, Cho J, Choi Y, Oh J, Lee J, Yoon K. Ubiquitous health care system for chronic disease management. J Korean Inst Commun Sci. 2010;27(9):3–8. [Google Scholar]
- 4.Song J, Lee YJ, Nam GW. Design and implementation of the chronic disease management platform based on personal health records. J Korea Ind Inf Syst Soc. 2012;17(1):47–62. [Google Scholar]
- 5.Gurjar R, Li Q, Bugbee D, Colecchi J, Sperling M, Karson A, et al. Design and implementation of a clinical rule editor for chronic disease reminders in an electronic medical record. AMIA Annu Symp Proc. 2006;2006:936. [PMC free article] [PubMed] [Google Scholar]
- 6.Song TM, Ryu S, Lee SH. U-health service for managing chronic disease: a case study on managing metabolic syndrome in a health center in South Korea. Healthc Inform Res. 2011;17(4):260–266. doi: 10.4258/hir.2011.17.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shepherd T, Hain S. eHealth in Queensland: progressing towards a patient centric, networked model of care. Healthc Inform Res. 2011;17(3):190–195. doi: 10.4258/hir.2011.17.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi JS, Lee WB, Rhee PL. Cost-benefit analysis of electronic medical record system at a tertiary care hospital. Healthc Inform Res. 2013;19(3):205–214. doi: 10.4258/hir.2013.19.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shin SY, Chung CK. A future of medical information system: establishment of hospital-oriented personal health record. J Korean Med Assoc. 2009;52(11):1115–1121. [Google Scholar]
- 10.Lee SY. Development of HIS system through the HL7-based combination of legacy system. J Korea Soc Comput Inf. 2004;9(3):55–62. [Google Scholar]
- 11.HL7. Health Level Seven International [Internet] Ann Arbor (MI): HL7; c2013. [cited at 2013 Dec 19]. Available from: http://www.hl7.org. [Google Scholar]
- 12.Park DK, Jung EY, Jeong BH, Moon BC, Kang HW, Tchah H, et al. Smart information system for Gachon University Gil Hospital. Healthc Inform Res. 2012;18(1):74–83. doi: 10.4258/hir.2012.18.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright A, Sittig DF. A four-phase model of the evolution of clinical decision support architectures. Int J Med Inform. 2008;77(10):641–649. doi: 10.1016/j.ijmedinf.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoon Y, Kim IK, Yi BK. Medical app's CDSS service using mobile cloud; Proceedings of the Korean Information Science Society Conference; 2011 Jun 29-Jul 1; Gyeongju, Korea. pp. 323–326. [Google Scholar]
- 15.Yun T, Yi GS. Application of random forest algorithm for the decision support system of medical diagnosis with the selection of significant clinical test. Trans Korean Inst Electr Eng. 2008;57(6):1058–1062. [Google Scholar]
- 16.Kong G, Xu DL, Liu X, Yang JB. Applying a belief rule-base inference methodology to a guideline-based clinical decision support system. Expert Syst. 2009;26(5):391–408. [Google Scholar]
- 17.Achour SL, Dojat M, Rieux C, Bierling P, Lepage E. A UMLS-based knowledge acquisition tool for rule-based clinical decision support system development. J Am Med Inform Assoc. 2001;8(4):351–360. doi: 10.1136/jamia.2001.0080351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eun SJ, Do JH, Kim KH, Whangbo TK. An implementation of oriental medicine u-healthcare service model using CDSS. J Korean Soc Internet Inf. 2010;11(5):59–70. [Google Scholar]
- 19.Regier R, Gurjar R, Rocha RA. A clinical rule editor in an electronic medical record setting: development, design, and implementation. AMIA Annu Symp Proc. 2009;2009:537–541. [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzales-Aguilar A, Ramirez-Posada M. Carrot2: búsqueda y visualizacicón de la información. El Profesional de la Información. 2012;21(1):105–112. [Google Scholar]
- 21.PubMed. PubMed Central (PMC) [Internet] Bethesda (MD): PubMed; c2013. [cited at 2013 Dec 19]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/ [Google Scholar]
- 22.Kamel Boulos MN. Expert system shells for rapid clinical decision support module development: an ESTA demonstration of a simple rule-based system for the diagnosis of vaginal discharge. Healthc Inform Res. 2012;18(4):252–258. doi: 10.4258/hir.2012.18.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Negnevitsky M. Artificial intelligence: a guide to intelligent systems. 3rd ed. Edinburgh: Pearson Education; 2011. [Google Scholar]