Abstract
Objectives
Diabetes is a chronic disease of continuously increasing prevalence. It is a disease with risks of serious complications, thus warranting its long-term management. However, current health management and education programs for diabetes mainly consist of one-way communication, and systematic social support backup to solve diabetics' emotional problems is insufficient.
Methods
According to individual behavioral changes based on the Transtheoretical Model, we designed a non-drug intervention, including exercise, and applied it to a mobile based application. For effective data sharing between patients and physicians, we adopted an SNS function for our application in order to offer a social support environment.
Results
To induce continual and comprehensive care for diabetes, rigorous self-management is essential during the diabetic's life; this is possible through a collaborative patient-physician healthcare model. We designed and developed an SNS-based diabetes self-management mobile application that supports the use of social groups, which are present in three social GYM types. With simple testing of patients in their 20s and 30s, we were able to validate the usefulness of our application.
Conclusions
Mobile gadget-based chronic disease symptom management and intervention has the merit that health management can be conducted anywhere and anytime in order to cope with increases in the demand for health and medical services that are occurring due to the aging of the population and to cope with the surge of national medical service costs. This patient-driven and SNS-based intervention program is expected to contribute to promoting the health management habits of diabetics, who need to constantly receive health guidance.
Keywords: Mobile Health, Social Support, Intervention Studies, Diabetes Mellitus, Self Care
I. Introduction
The aging of the global population has played a key role in the rise of chronic diseases. In an analysis of the statistics of death causes by Statistics Korea in 2012, it was found that the most widely occurring chronic diseases were cancer, cardiovascular disease, cerebrovascular disease, intentional self-harm (suicide), diabetes, and pneumonia, in that order [1]. Of those, diabetes is on the rise globally. According to the World Health Organization (WHO), about 20 million people have currently been diagnosed as diabetics. About 11 million people died of diabetes in 2005, and the WHO forecast that death from diabetes would increase to twice this number by 2030 [2].
Like most chronic disease patients, diabetics, with effective disease control achieved through systematic and continuous treatment and management, can live the same healthy lives as those of normal people. However, the conventional diabetes treatment and management process, which is centered on hospitals, has several limitations, as shown in the following, in its attempts to satisfy the above requirements. First, diabetes health management and education programs are mainly operated in a form of one-way communication. One-way communication means physician-centered and physician-led communication. Second, there is inadequate systematic assistance via social support to solve the problem of emotional support for diabetics, who need to receive lifelong treatment. Third, adopting advanced health information technology is required for effective healthcare. Beyond the conventional method, social networking service (SNS) communication-based treatment and mobile application based treatment [3,4,5,6,7] have emerged recently. This study proposes an SNS-based mobile application for diabetes self-management; the system offers tailored information that can induce changes in patient behavior through relevant and helpful messages, exchanges, and information.
II. Case Description
1. Health and Treatment Behavior Prediction Tools
As a patient's active participation and own responsibility are required in chronic disease management, the paradigm of diabetes self-management interventions has shifted to an approach that is focused on patient-centered behavioral change techniques that consider training in problem solving, self-efficacy enhancement, attitudes on behavioral change, and individual awareness change, including conversion from one-sided, information-oriented education. In this context, we adopted a Transtheoretical Model (TTM) to health behavior intervention, focusing on such factors as diabetics' exercise and diet [8].
This model is based on the premise that a certain process of stages can be followed when patients change their behavior. The model explains health behavior in terms of cognitive motivation factors that affect an individual's behavior instead of focusing on behavioral results [9]. The TTM model has proven effective in stopping smoking and in attempts to implement diabetes intervention programs after varying a program's intensity based on a patient intention [10,11].
The TTM model consists of five stages: the precontemplation stage, contemplation stage, preparation stage, action stage, and maintenance stage. Using such a stage paradigm, we designed an intervention program for each stage based on the most influential variables in each individual's behavioral change stage [12,13].
2. User Interface of HealthTWITTER
HealthTWITTER is composed of three major functions: 1) messaging and SNS function, 2) health profile, and 3) group management (Figure 1B). The messaging and SNS function pertains to posting messages on the board of HealthTWITTER by registered users when they upload their messages in their groups or in public. The health profile function refers to the logging and monitoring of patient medication, symptoms, laboratory results, and demographic information, such as body weight and blood sugar level. It also contains exercise and dietary logging data, with compliance information from the treatment intervention program, which works based on our developed TTM model-based intervention algorithm. Figure 1C is one example of intervention, in which the exercise intervention program has four functional buttons. 'Intervention Status' shows how the user is ready to exercise using an exercise status by conducting the auto-run process of intervention algorithm. 'My Mission' announces the exercise goal set by the user. 'Today's Mission' shows an individual's daily exercise goal and reminds the user of this goal through the Push Alarm function. 'Social group status (Social GYM)' shows how much classified group members exercise, as represented by their exercise patterns.
Figure 1.
The HealthTWITTER user interface: (A) login screen where only authorized (registered) users can use the application, (B) the main menu bar representing three major functions (it pops up from the left side), (C) the intervention function menu composed of 'Intervention Status,' 'My Mission,' 'Today's Mission,' and 'Social Group Status.'
To build the initial classified social group with a sufficient number of patients, we utilized data from the Incheon Chronic Disease Management System (iCDMS), which is a chronic disease management system that contains data from chronic disease patients (high blood pressure patients, diabetics, and child obesity patients). The data cover the period from their initial registration to their follow-up management [14].
3. Self-Management Algorithm Based on TTM Model
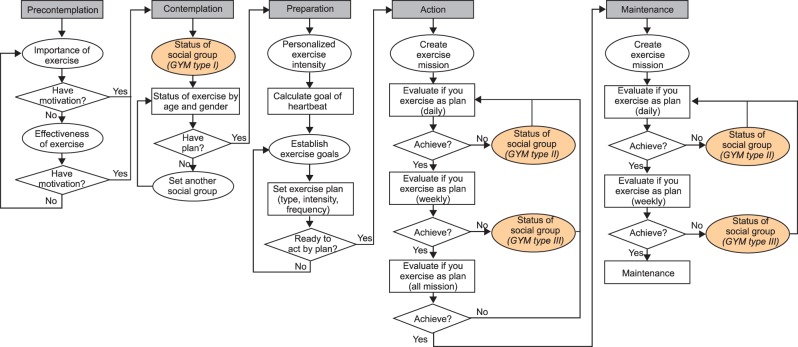
HealthTWITTER has three intervention programs focusing on diet, exercise, and blood sugar level information necessary for diabetes management. Each intervention program is conducted according to a self-management algorithm based on serial stages. As an example, we show how the TTM model and SNS-based exercise intervention work (Figure 2).
Figure 2.
Algorithm for exercise assessment.
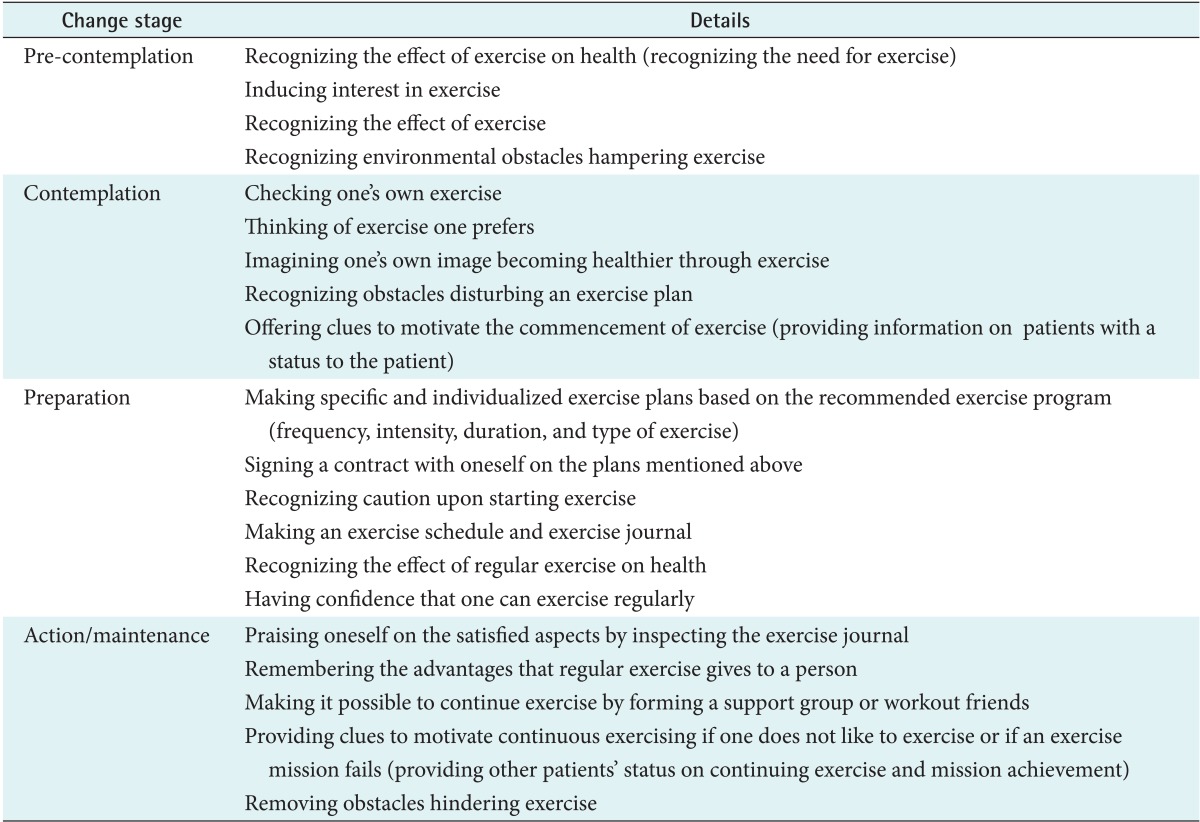
We also adopted the contents of the self-assessment model (Table 1), which was built by Prochaska and Diclemente [15] and which refers to the TTM in order to operate HealthTWITTER with consistency.
Table 1.
Self-assessment model by health behavior change stages
III. Discussion
HealthTWITTER is a social network-based intervention program created for the prevention of diabetes and the disease's continuous management. It has been designed using an algorithm that offers tailored health management service for individuals. Unlike original diabetes management apps [16,17,18], which only represent input information, HealthTWITTER may be supported through SNS and is designed based on the reliable TTM model for effective health behavior intervention. As a result of these developments, it is thought that HealthTWITTER will have high application rates for patients in their 20s and 30s, who receive less intensive health management since attentive supervision is focused on the age brackets of 65 and older. To test our application for the targeted group, we gathered preliminary outcomes from the participants of the '2030 Camp' operated by the Korean Diabetes Association in July 2012 [19]. More than 80% of the participants said they had the intention to use HealthTWITTER. Although this study can play a pivotal role in promoting the SNS-based health care industry's development, the following limitations exist:
First, there is limitation in the study target. This study limited the research target to diabetics in their 30s and 40s, who have low awareness rates and treatment rates, with the intention of increasing attention paid to them. The development of an algorithm that can be applied to all age brackets will be necessary in the future.
Second, there is difficulty in securing reference group data. To create a reference group, exercise-related data from the initial stage of contracting diabetes is necessary. Although clustering was conducted based on the iCDMS data, which targeted elderly people aged 65 or older, there was a limitation in that the data were different in direction from the data used in this study. Further studies will need to present a reference group through the acquisition of reliable cumulative data by linking with the Seoul City Metabolic Syndrome Management Service, which manages chronic disease patients with minimum ages of at least in the 30s [20].
In October 2013, the Ministry of Health and Welfare issued an announcement of legislation on the revision of the Medical Service Act to allow u-health care between patients and doctors; this idea was focused on neighborhood medical centers, with the hope of enhancing treatment effects by offering chronic disease management anytime. Through the HealthTWITTER app, a collaborative patient-physician health care model will be developed with two advantages; namely, the reduction of poor adherence to chronic disease treatment and the decline in increasing health and medical service costs.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (No. 2010-0023700).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Statistics Korea. Causes of death statistics in 2012 [Internet] Daejeon, Korea: Statistics Korea; 2012. [cited at 2014 Jan 14]. Available from: http://kostat.go.kr. [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Wu JH, Wang SC, Lin LM. Mobile computing acceptance factors in the healthcare industry: a structural equation model. Int J Med Inform. 2007;76(1):66–77. doi: 10.1016/j.ijmedinf.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008;77(6):399–404. doi: 10.1016/j.ijmedinf.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Arsand E, Tatara N, Ostengen G, Hartvigsen G. Mobile phone-based self-management tools for type 2 diabetes: the few touch application. J Diabetes Sci Technol. 2010;4(2):328–336. doi: 10.1177/193229681000400213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grajales FJ, 3rd, Sheps S, Ho K, Novak-Lauscher H, Eysenbach G. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16(2):e13. doi: 10.2196/jmir.2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi I, Kim S, Kwon YD. Key aspects of using Web-based diabetes telemedicine systems in multiple clinical settings. J Korean Soc Med Inform. 2007;13(4):375–383. [Google Scholar]
- 8.Plack K, Herpertz S, Petrak F. Behavioral medicine interventions in diabetes. Curr Opin Psychiatry. 2010;23(2):131–138. doi: 10.1097/YCO.0b013e3283366555. [DOI] [PubMed] [Google Scholar]
- 9.Vallis M, Ruggiero L, Greene G, Jones H, Zinman B, Rossi S, et al. Stages of change for healthy eating in diabetes: relation to demographic, eating-related, health care utilization, and psychosocial factors. Diabetes Care. 2003;26(5):1468–1474. doi: 10.2337/diacare.26.5.1468. [DOI] [PubMed] [Google Scholar]
- 10.Fava JL, Velicer WF, Prochaska JO. Applying the transtheoretical model to a representative sample of smokers. Addict Behav. 1995;20(2):189–203. doi: 10.1016/0306-4603(94)00062-x. [DOI] [PubMed] [Google Scholar]
- 11.Evers KE, Paiva AL, Johnson JL, Cummins CO, Prochaska JO, Prochaska JM, et al. Results of a transtheoretical model-based alcohol, tobacco and other drug intervention in middle schools. Addict Behav. 2012;37(9):1009–1018. doi: 10.1016/j.addbeh.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 13.Di Noia J, Contento IR, Prochaska JO. Computer-mediated intervention tailored on transtheoretical model stages and processes of change increases fruit and vegetable consumption among urban African-American adolescents. Am J Health Promot. 2008;22(5):336–341. doi: 10.4278/ajhp.22.5.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seo HJ, Yim J, Lim JS, Kang KH, Kim EJ, Park IB, et al. Development of Incheon Chronic Disease Management System through Local Community Connection: an example of one Metropolitan City. J Korean Soc Health Inf Health Stat. 2008;33(2):77–88. [Google Scholar]
- 15.Prochaska JO, DiClemente CC. Towards a comprehensive model of change. In: Miller WR, Heather N, editors. Treating addictive behaviors: processes of change. New York (NY): Plenum Press; 1986. pp. 3–27. [Google Scholar]
- 16.iCare-D app [Internet] Seoul, Korea: Ubiquitous Health Care Research Center, Catholic University of Korea; 2012. [cited at 2014 Jan 15]. Available from: https://play.google.com/store/apps/details?id=tw.project.diabetes. [Google Scholar]
- 17.Q-Care app [Internet] Suwon, Korea: Gyeonggi Province; 2013. [cited at 2014 Jan 15]. Available from: https://play.google.com/store/apps/details?id=com.brenex. [Google Scholar]
- 18.U-Care Note app [Internet] Incheon, Korea: Gachon University Gil Medical Center; 2014. [cited at 2014 Jan 15]. Available from: https://play.google.com/store/apps/details?id=com.smartcare. [Google Scholar]
- 19.Korean Diabetes Association. Camp for 2030 [Internet] Seoul, Korea: Korean Diabetes Association; 2012. [cited at 2014 Jan 15]. Available from: http://www.diabetes.or.kr/general/camp/index.php. [Google Scholar]
- 20.Park SS, Oh SW. Strategy for the management of metabolic syndrome of Seoul citizen. Food Ind Nutr. 2010;15(1):10–16. [Google Scholar]