Abstract
Background
In 2009 Malawi introduced a new protocol to screen potential blood donors for anaemia, using the WHO Haemoglobin Colour Scale (HCS) for initial screening. Published studies of the accuracy of the HCS to screen potential blood donors show varying levels of accuracy and opinion varies whether this is an appropriate screening test. The aim of the study was to assess the validity of the HCS, as a screening test, by comparison to HemoCue in potential blood donors in Malawi.
Study design and methods
This was a blinded prospective study in potential blood donors aged over 18 years, at Malawi Blood Transfusion Service in Blantyre, Malawi. Capillary blood samples were analysed using the HCS and HemoCue, independent of each other. The sensitivity and specificity of correctly identifying ineligible blood donors (Hb≤12g/dL) were calculated.
Results
From 242 participants 234 (96.7%) were correctly allocated and 8 (3.3%), were wrongly allocated on the basis of the Haemoglobin Colour Scale (HCS) compared to HemoCue, all were subjects that were wrongly accepted as donors when their haemoglobin results were ≤12.0g/dL. This gave a sensitivity of 100% and specificity of 96.7% to detect donor eligibilty. The negative predictive value of the HCS was 100% but the positive predictive value to identify ineligible donors on the basis of anaemia was only 20%.
Conclusions
Initial screening with the HCS correctly predicts eligibility for blood donation in the majority of potential blood donors at considerable cost saving compared with use of HemoCue as the first line anaemia screening test, however, by this method a small number of anaemic patients were allowed to donate blood.
Introduction
Anaemia is a major public health concern in Malawi and most low and middle income countries. A 1993–2005 World Health Organisation study estimated that it affected over 1620 million people, representing 24.8% of the world population.1 Despite the high prevalence rates, detection of the condition remains a problem in the developing world with most cases diagnosed clinically. Clinical diagnosis has a sensitivity of 29–44% and a specificity of 81–89%, limiting its usefulness in diagnosing anaemia.2 The Haemoglobin Colour Scale (HCS) was developed in 1995 as an inexpensive, simple alternative for assessing anaemia.3,4 It does not aim to compete with a haemoglobinometer in the laboratory, but it is intended for use when the latter is not available or practical. The HCS uses a strip of chromatography paper and a standard colour chart. The method relies on comparing the colour of a drop of blood absorbed onto chromatography paper with standard colours on a laminated card, varying from pink to dark red. These colours correspond to haemoglobin (Hb) levels of 4, 6, 8, 10, 12, and 14 g/dl. Intermediate shades can be identified, allowing haemoglobin levels to be judged to 1 g/dL.3
Laboratory and community studies have assessed the accuracy of the HCS for diagnosing anaemia, but controversy over its validity and usefulness remains.5–8 A meta-analysis, including validation studies conducted in the laboratory and in the field (ie. ‘real life’), has shown that the sensitivity of the HCS to detect any anaemia is approximately 75–97% with a specificity of 41–98%. The sensitivity and specificity are increased for severe anaemia (<7 g/dL or <6 g/dL in different studies).8,9 Laboratory based studies show a far greater accuracy than real life clinical studies, but accuracy in clinical settings can be improved after training.8 The accuracy varies depending on the prevalence of anaemia in the population, being more accurate in populations with a higher prevalence.9
Screening of blood donors to exclude those who are ineligible due to anaemia is a prerequisite of any blood donation service. Many different methods of donor screening can be used but in resource poor countries low cost methods are essential. In 2001 Lewis and Emmanuel published a validation of the HCS as a screening test for blood donor eligibility, showing it to be highly sensitive and specific and superior to the semi-quantitative copper sulphate method which had been widely used since the 1950s.10 The Malawi Blood Transfusion Service (MBTS) is the national blood service for Malawi which collects about 50,000 donor whole blood units per year. Since 2009 the MBTS has used the HCS to screen all blood donors to determine their eligibility for blood donation and to detect those that will need additional testing with HemoCue before their eligibility can be decided. The SOP stipulates that all blood donors are screened with HCS. Those with Hb <12g/dL are deferred for blood donation, those with Hb >12g/dL are accepted for blood donation, those with Hb =12g/dL are referred for testing with HemoCue and are accepted for donation if the Hb is ≥12.5g/dL.
Validation of the use of HCS in a real world setting, using our own staff following the local protocol for pre-donation anaemia screening, is necessary to ensure that ineligible individuals are not being accepted to donate blood and that eligible potential blood donors are not being rejected unnecessarily. The objective of the study was to assess the accuracy of the Haemoglobin Colour Scale by comparison to results obtained using a HemoCue in a donor population, to assess the validity of the MBTS protocol of using the HCS and HemoCue in screening for anaemia in potential blood donors.
Materials and Methods
A convenience sample of 242 potential blood donors aged 19–65 years of age were independently tested with both HCS (Copack GmbH, Germany) and HemoCue (HemoCue Hemoglobin system, HemoCue AB, Ängelholm, Sweden) at the MBTS blood donor clinics in Blantyre during the month of January. The investigators were trained to use the validated HemoCue machines by MBTS staff. Routine capillary blood samples were collected by the Malawi Blood transfusion staff through a skin puncture and measured using the Haemoglobin Colour Scale for their decision making on the eligibility of the donors. On any day 2 MBTS staff are on duty screening donors and the team changes every 3 days so at least 4 MBTS staff were involved in taking HCS readings. The investigators also collected finger prick samples from the same donors and measured the sample using the HemoCue. The HemoCue results were collected independent of the HCS results and the MBTS staff were not informed of the HemoCue result. The investigators did not have prior knowledge of the HCS results. The donor had an ID number which was recorded by the donor staff and the investigators so that the blinding was achieved. Thereafter, the different set of results was compared.
Statistical Analysis
Sensitivity and specificity are terms used to evaluate a clinical test. Sensitivity measures the proportion of actual positives. Specificity measures the proportion of negatives which are correctly identified. The sensitivity, specificity and predictive values of the HCS for identifying ineligible blood donors were calculated. Bias and limits of agreement (LOA) were calculated, using the method of Altman and Bland, for the complete dataset and after excluding those with Hb >15g/dL on HemoCue as the upper limit of HCS is 14g/dL.11The study was approved by the College Of Medicine Research and Ethics Committee (COMREC).
Results
Measurements were obtained for 242 donors. Table 1 shows the comparison of the HCS results to those of HemoCue. On HCS screening there were 197 subjects (81%) correctly identified as eligible to donate blood and 2 subjects (0.8%) were correctly identified as ineligible to donate. Thirty five subjects (14.5%) had borderline results (Hb=12g/dL) by HCS and, according to the MBTS SOPs would have gone on to have HemoCue to determine their eligibility for donation. For calculation of sensitivity and specificity these 35 have been excluded. Eight subjects (3%) were wrongly assessed to have Hb >12 g/dL and were wrongly allocated as eligible to donate by HCS. The Hb values in these subjects were; 8.6, 10.0, 11.2, 11.4, 11.6, 11.8, 11.8 and 12.0 g/dL. No subjects were wrongly excluded as donors.
Table 1.
Haemoglobin Colour Scale and HemoCue results by haemoglobin-based categories. *These 35 subjects require a further confirmatory test (HemoCue) to determine donor eligibility according to the MBTS SOP and would have been correctly allocated after the second test.
| HemoCue result (g/dL) | |||
| <12.5 | ≥12.5 | ||
| HCS | ineligible | eligible | Total |
| <12 ineligible | 2 | 0 | 2 |
| =12 re-test | *35 | ||
| >12 eligible | 8 | 197 | 205 |
| Total | 10 | 197 | 242 |
The sensitivity of the HCS to detect those ineligible for donation was 100% (2/2) and the specificity was 96.1% (197/205). The positive predictive value (PPV) of the HCS to detect ineligible donors was 20% (2/10) and the negative predictive value (NPV) was 100% (197/197).
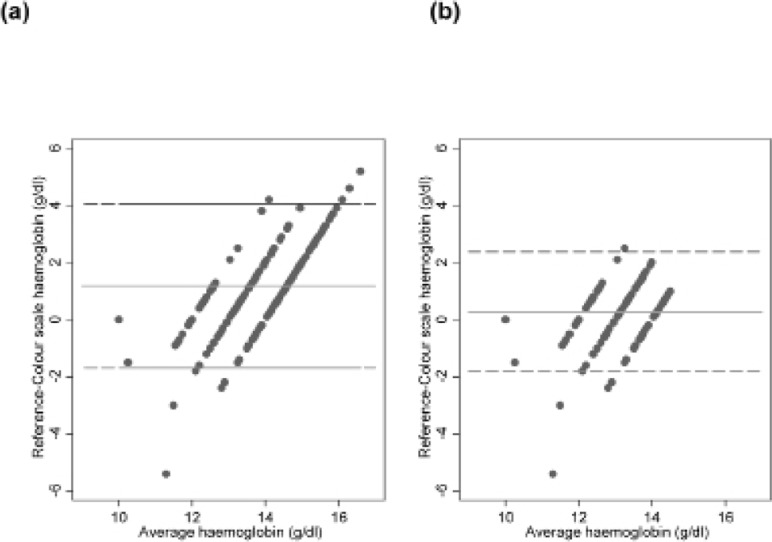
Overall 50 results (20.7%) showed a discrepancy of >1g/dL between HCS and HemoCue (excluding those with Hb >15g/dL on HemoCue as the upper limit of HCS is 14g/dL). In the majority this did not affect eligibility allocation. The extent of the discrepancy between the methods is reflected in the limits of agreement. Figure 1 shows the Bland-Altman plots for the complete and restricted dataset. For samples with Hb≤15g/dL the bias (95% limits of agreement) was estimated to be 0.27 (−1.82, 2.37) ie 95% of HCS values are expected to lie between 2.37 g/dL below and 1.82 g/dL above the HemoCue value.
Figure 1.
Bland-Altman plots for Haemoglobin Colour Scale compared with the reference (a) for complete data set (b) for blood samples in which HemoCue≤15g/dL
Discussion
These results demonstrate the high sensitivity, specificity and negative predictive values, but relatively poor positive predictive value of the HCS as a screening tool for blood donor eligibility when used according to the Malawi BTS protocol. Misallocation was on the side of accepting ineligible donors. The risk of this is two-fold; firstly an anaemic donor may be made even more anaemic through blood donation. This may have significant consequences, eg for the subject in our survey with an Hb of 8.6g/dL who was allowed to donate. This may worsen the anaemia and deny them the opportunity to be diagnosed with anaemia and investigated and managed appropriately. Secondly the recipient of the blood may receive fewer red cells than was expected by a standard transfusion.
Published evaluations of the use of the HCS as part of a screening protocol prior to blood donation have shown mixed results. One study from India investigated HCS as a predonation screening test. The Hb was measured using HCS in the laboratory on venous whole blood and compared to the same sample measured on an automated analyser. Similar to our own study they found that in 23% of samples the Hb measured by HCS lay > 1g/dL from the gold standard value.12 The sensitivity of HCS was reported as 87% and specificity as 82%, for diagnosing anaemia, with limits of agreement from −4.7 to +5.6g/dL, but it is not clear how many donors were incorrectly allocated as a result of this. The authors concluded that HCS is not a good screening tool for blood donors and recommended that copper sulphate screening was more accurate. Conversely a study from Indonesia found that HCS was superior to the copper sulphate test for donor screening.13 Sawant and colleagues in India compared the HCS to an autoanalyser in subjects that had already been rejected for donation, on the basis of anaemia.14 They found the sensitivity and specificity of HCS to be 97% and 93% respectively and recommended that HCS should be used for predonation screening. Finally a study that looked at randomly selected blood samples in a UK laboratory found that in 46% of samples, the Hb value with the HCS lay more than 1g/dL from the value with an autoanalyser and gave limits of agreement from −3.5 to +3.1 g/dL. Despite this the HCS performed better than the copper sulphate test in the same setting.15 All of these studies were methodologically different to ours, for example capillary samples may give higher Hb values that venous blood16 and most were conducted in the laboratory, rather than in a blood donor clinic. In our hands the HCS performed well as a screening tool for donor eligibility and gave limits of agreement better than those reported above.
In the Malawi Blood Transfusion Service the cost of consumables for HCS testing is less than a third of those for HemoCue testing (US$0.15 vs US$0.53). The MBTS screens approximately 50,000 potential donors per annum. According to our survey 14.5% of them will need a second test, HemoCue to determine eligibility. Based on current prices the cost of using HCS for primary screening, followed by HemoCue, according to current Malawian practice is $11,342.5 per annum as compared to $26,500 if HemoCue was used for initial screening. It would be interesting and useful to carry out a more detailed cost benefit analysis of the MBTS approach but sufficient economic data was not available.
The HCS does have limitations. It is more operator dependent than HemoCue. This study was conducted at a time MBTS was experiencing a high staff turn over due to uncompetitive salaries. To address this MBTS undertakes regular, annual staff training to maintain high standards of accuracy. It also only grades haemoglobin values within 1g/dL and does not exceed 14g/dL, however, for the purpose of blood donor screening this may not matter. Our study also had limitations. The observations were made at a single donor centre. It is necessary to repeat the survey at other centres and with other staff to see if similar levels of sensitivity and specificity are obtained. A more detailed economic evaluation of current practice is also needed including a comparison to the copper sulphate test.
Blood donation is life-saving. A recent study of 104 transfusions at a district hospital in Malawi showed that the average Hb of recipients prior to transfusion was 4.8g/dL. Fifty seven per cent of recipients were children and 17% pregnant women17. The study also showed that, at the time of the survey, blood was available within 1 hour of requisition. Our survey suggests that, when used with HemoCue, the Haemoglobin Colour Scale allows for implementation of an acceptable donor eligibility screening protocol which facilitates donation to such a vital service.
In conclusion we have demonstrated that our current practice of initial screening with the Haemoglobin Colour Scale correctly predicts eligibility for blood donation in the majority of potential blood donors at considerable cost saving compared with direct use of HemoCue, however, it should be remembered that by this method a small number of anaemic patients were allowed to donate blood.
Acknowledgements
We are extremely grateful to the nursing staff at the Malawi Blood Transfusion Services head office in Blantyre for their support and cooperation during data collection. The College of Medicine Research Support committee funded the project.
References
- 1.WHO, author. Worldwide prevalence on anaemia 1993–2005. [19th september 2013]. http://www.who.int/vmnis/anaemia/prevalence/summary/anaemia_status_summary/en/index.html.
- 2.Chalco JP, Huicho L, Alamo C, et al. Accuracy of clinical pallor in the diagnosis of anaemia in children: a meta-analysis. BMC Pediatri. doi: 10.1186/1471-2431-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott GJ, Lewis SM. A simple and reliable method for estimating haemoglobin. Bull World Health Organ. 1995;73:369–373. [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis S M, Stott G J, Wynn K J. An inexpensive and reliable new haemoglobin colour scale for assessing anaemia. J Clin Pathol. 1998;51:21–24. doi: 10.1136/jcp.51.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montresor A, Ramsan M, Khalfan N, et al. Performance of the Haemoglobin Colour Scale in diagnosing severe and very severe anaemia. Trop Med Int Health. 2003;8:619–624. doi: 10.1046/j.1365-3156.2003.01072.x. [DOI] [PubMed] [Google Scholar]
- 6.Lindblade KA, Mwololo K, van Eijk AM, et al. Evaluation of the WHO Haemoglobin Colour Scale for diagnosis of anaemia in children and pregnant women as used by primary health care nurses and community health workers in western Kenya. Trop Med Int Health. 2006;11:1679–1687. doi: 10.1111/j.1365-3156.2006.01721.x. [DOI] [PubMed] [Google Scholar]
- 7.Aldridge C, Foster HME, Albonico M, et al. Evaluation of the diagnostic accuracy of the Haemoglobin Colour Scale to detect anaemia in young children attending primary healthcare clinics in Zanzibar. Trop Med Int Health. 2012;17:423–429. doi: 10.1111/j.1365-3156.2011.02944.x. [DOI] [PubMed] [Google Scholar]
- 8.Ingram CF, Lewis SM. Clinical use of WHO haemoglobin colour scale:validation and critique. J Clin Pathol. 2000;53:933–937. doi: 10.1136/jcp.53.12.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Critchley J, Bates I. Haemoglobin colour scale for anaemia diagnosis where there is no laboratory: a systematic review. International Journal of Epidemiology. 2005;34:1425–1434. doi: 10.1093/ije/dyi195. [DOI] [PubMed] [Google Scholar]
- 10.Lewis SM, Emmanuel J. Validity of the haemoglobin colour scale in blood donor. Screening Vox Sanguinis. 2001;80:28–33. doi: 10.1046/j.1423-0410.2001.00013.x. [DOI] [PubMed] [Google Scholar]
- 11.Bland JM, Altman DG. Statistical methods for asessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 12.Tondon R, Verma A, Pandey P, et al. Quality evaluation of four hemoglobin screening methods in a blood donor setting along with their comparative cost analysis in an Indian scenario. Asian J Transfus Sci. 2009 Jul;3(2):66–69. doi: 10.4103/0973-6247.53874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Timan IS, Tatsumi N, Aulia D, et al. Comparison of haemoglobinometry by WHO Haemoglobin colour scale and copper sulphate against haemoglobincyanide reference method. Clin Lab Haematol. 2004;26:253–258. doi: 10.1111/j.1365-2257.2004.00622.x. [DOI] [PubMed] [Google Scholar]
- 14.Sawant RB, Bharucha ZS, Rajadhyaksha SB. Evaluation of hemoglobin of blood donors deferred by the copper sulphate method for hemoglobin estimation. Transfusion and Apheresis Science. 2007;36:143–148. doi: 10.1016/j.transci.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Paddle JJ. Evaluation of the Haemoglobin colour Scale and comparison with the HemoCue haemoglobin assay. Bull World Health Organ. 2002;80:813–816. [PMC free article] [PubMed] [Google Scholar]
- 16.Radtke H, Polat G, Kalus U, et al. Hemoglobin screening in prospective blood donors: Comparison of different blood samples and different quantitative methods. Transfus Apher Sci. 2005;33:31–35. doi: 10.1016/j.transci.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Bugge HF, Karlsen NC, Oydna E, et al. A study of blood transfusion services at a district hospital in Malawi. Vox Sang. 2013 Jan;104(1):37–45. doi: 10.1111/j.1423-0410.2012.01628.x. [DOI] [PubMed] [Google Scholar]