Abstract
Background:
Information technology can play a vital role in meeting patient needs and reinforcing the relationship among patients and their pain physicians. However, strong resistance remains on the medical side to this type of non-frontal care.
Objectives:
The primary objective of this study was to assess the effectiveness of an E-mail intervention on customers’ satisfaction. The secondary goals were to analyze the messages from patients to their clinician (not only the volume but also the content) and the impact on client, professional and health services outcomes.
Study Design:
A prospective, non-randomized evaluation of patients undergoing treatment for chronic pain from September 2011 to May 2012.
Setting:
A private, specialty referral center in Spain.
Materials and Methods:
Participants were users visiting the Pain Management Unit evaluated by one physician. The E-mail address of the facility was written in every medical report provided. Patient satisfaction at the end of the 8-month trial period was assessed and outcomes recorded.
Results:
Patients reported better communication with their therapist and greater satisfaction with overall care. 780 E-mails were read. Specialists received an average of 5 messages per day (standard deviation 0,3). None of them was unsuitable.
Limitations:
This is a prospective, single center evaluation performed by one doctor. There was no control group due to ethical considerations.
Conclusions:
Electronic communication is a cheap, easy and feasible way to address a wide range of concerns, thus enhancing patients’ satisfaction. More efforts are needed to implement routinely usage of this tool. If used appropriately, E-mail can facilitate physician-dependent interactions, promote access to care, save time and reduce costs. Concerns about billing, improper utilization, privacy and confidentiality might complicate its introduction and acceptance. Internet access remains a significant barrier to online patient-provider transference.
Keywords: Chronic pain, electronic communication, electronic self-reported outcomes, E-mail, internet, net, online communication, pain clinic, pain unit, patient satisfaction, persistent pain, self-report assessment
INTRODUCTION
Consumer demand for online clinical services is growing faster than the professional response.[1] Previous studies have reported that 90% of patients with Internet access would like to contact through E-mail with their physician, regarding administrative issues, medication concerns and other aspects of care.[2] Nevertheless, online patient-provider communication remains uncommon although it is slowly increasing.[3,4,5,6,7,8] According to several Cochrane systematic reviews, E-mail used as an adjuvant to traditional meetings, offers both, advantages and risks.[9,10,11] Benefits include the potential to reach fragile patients, to enhance the relationship and to improve treatment outcomes.[12] Hazards extend over threats to client confidentiality and privacy, liability coverage and the lack of competency standards for this kind of connection.
To better understand these issues, a prospective evaluation was conducted. The effectiveness of an E-mail intervention on customer satisfaction, the messages received and the impact on outcomes were determined.
MATERIALS AND METHODS
The study was conducted in a private, specialty referral center in Spain without any external funding, by two pain physicians using standard electronic mail (Office Outlook Web Access™, Microsoft Corporation, Redmond, WA). All the patients visiting the Pain Management Unit from September 2011 to May 2012 were enrolled. Participants did not change their normal course of treatment. They were perfectly instructed by the clinician while the E-mail address was clearly written in their medical report. Adherence to all confidentiality and Health Insurance Portability and Accountability Act requirements were followed. Every patient treated in the Pain Management Unit were included but those who were unable to understand or unwilled to participate. The study investigated the feasibility of using E-mail messages to promote effective patient-provider communication in the clinical pain practice, including immediate requests.
Outcome measures
Patient satisfaction: Mean measure. Yes or no answer.
Quantitative analysis: Whole number of E-mails received and time implications.
-
Qualitative analysis: The E-mail content was categorized as follows:
- Administrative requests: To reschedule appointments.
-
Medical requests:
- Urgent clinical messages (because of pain escalation or major adverse events): Worst-case scenario. The specialist responded directly to the patient by a telephone call and scheduled a quick visit for the same day or the day after.
- Medication adjustment after performing interventional techniques.
- Notification of medication related side effects.
- Aid managing breakthrough pain with rescue medication.
- Miscellaneous: For test information, psychosocial concern (depression, anxiety, insomnia) or self-reported outcomes.
The investigator cataloged message content according to this schema and daily answered non-urgent E-mails through a smart phone.
STATISTICAL ANALYSIS
Data were collected by one researcher, using Microsoft Access™ (Microsoft Corporation, Redmond, WA). The SPSS™ 9.0 statistical package (IBM Corporation, Armok, NY) was used to analyze them. Effect sizes were reported as mean differences with standard deviation for continuous measures and as proportions for dichotomous measures.
RESULTS
Participant flow
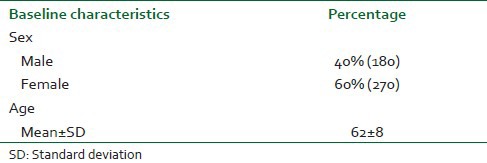
A total of 450 patients were included. Table 1 shows the demographic characteristics. There was significant difference in the ratio of men to women (40% vs. 60%). There were no differences in the age groups. No user was excluded.
Table 1.
Demographic characteristics
Outcomes
Patient satisfaction
At the end of the 8-month span, satisfaction rate rose to 99,8%.
Quantitative analysis
A total of 780 E-mails were received. Almost half of the patients wrote at least once (49.5%). Physicians received an average of five daily mails (standard deviation [SD] 1,6) and spend about an hour (SD 0,3) per day answering clinical queries. The reception staff absorbed work into their routines without adverse time implications. None of the messages was unsuitable.
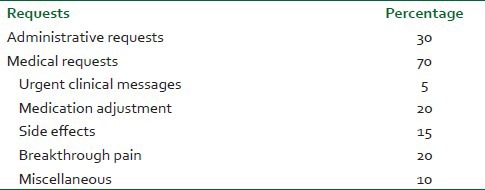
Qualitative analysis
It is illustrated in Table 2.
Table 2.
Qualitative content analysis of administrative requests and clinical messaging
There were no outcomes relating to harm.
DISCUSSION
E-mail communication, properly used, improves patient satisfaction. The implementation of an electronic transference system between pain physicians and customers is feasible without overwhelming caretakers. The qualitative analysis reveals that patients are worry about clinical issues-mainly about medication related problems-but they are also interested in dealing with administrative stuff. Physicians can solve these questions even in real time, avoiding major complications, missing appointments and casual visits.
In general practice, E-mail exchange between patients and caregivers enhances communication, improves the outcome and reduce face-to face consultations even in the management of chronic diseases such as pain.[13,14,15,16] It also plays a useful role in meeting patient needs or situations, adding information, receiving updates, promoting patient empowerment and improving quality of care and quality of life.[17,18] On the other hand, there is no evidence of harm caused by E-mail interventions. Like all technologies, use and misuse will determine whether its chances will become realities. E-mails can be sent (and subsequently read) at an opportune time, outside of traditional office hours where convenient, this could be the reason why there is often strong resistance on the part of physicians to this type of non-frontal care.[19]
There is no guideline strong enough and there are not best-practice standards for using E-mail as a direct practice methodology.[20] Policy-level advances are needed to maximize the availability and effectiveness of online patient-provider communication for both, health care consumers and health care providers.[21]
When E-mail is compared with standard methods, health care professionals as well as patients, prefer E-mail rather than telephone for non-urgent consultations.[22] Those patients, who regularly access the net, usually feel more comfortable with the system and make a better use. Accessibility has been previously assessed not only in patients — suffering from diabetes, general disease, multiple sclerosis, oncological process or psychiatric disorder, but also in physicians. The success rate ranges from 40% in the oldest papers to 90% in the latest ones.[23,24,25,26,27,28]
Billing for online consultation has been approved by the American Medical Association and several medical insurance carriers are evaluating the economic consequences of reimbursement for E-mail consultation.[29]
Even though this study is prospective and has a large sample size, it is not without limitations. First of all, a possible control group was lost because of ethical considerations. Secondly, it is a single center evaluation recorded over an 8-month period. In any observational study, confounding variables are more difficult to control than in randomized studies. However, the recent evaluations of adverse effects have illustrated the superiority of observational studies compared to randomized trials in evaluation of the harms.[30,31] Finally, there was only one physician recording and analyzing data, so bias might be expected.
This study adds to the literature by providing insight into possible underlying mechanisms for patient satisfaction with online connection: convenience, closeness and effectiveness. Another novel finding was the absence of unsuitable messages. These facts may explain the high satisfaction rates reached.
CONCLUSION
Electronic correspondence facilitates specialist-patient interaction, enhances satisfaction, improves access to care, saves time, reduces costs and it is also cheap, easy and feasible. Even patients with handicaps are able to use the service if their relatives assist them. Considering these facts, there is no reason for not having an institutional E-mail account available to customers: The closer the doctor is, the less he miss.
The increasing prevalence of E-mail consultation raises new concerns for pain therapists, which should be addressed by regulatory commissions or in court.
Further research is needed to evaluate electronic services in the pain practice and their impact on patient satisfaction, empowerment and medical outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Atherton H, Sawmynaden P, Sheikh A, Majeed A, Car J. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database Syst Rev. 2012;11:CD007978. doi: 10.1002/14651858.CD007978.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Lin CT, Wittevrongel L, Moore L, Beaty BL, Ross SE. An Internet-based patient-provider communication system: Randomized controlled trial. J Med Internet Res. 2005;7:e47. doi: 10.2196/jmir.7.4.e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giménez-Pérez G, Gallach M, Acera E, Prieto A, Carro O, Ortega E, et al. Evaluation of accessibility and use of new communication technologies in patients with type 1 diabetes mellitus. J Med Internet Res. 2002;4:E16. doi: 10.2196/jmir.4.3.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer M. Physician use of e-mail: The telephone of the 21st century? J Med Pract Manage. 2004;19:247–51. [PubMed] [Google Scholar]
- 5.Guth AA, Diflo T. “You’ve got mail!”: The role of e-mail in clinical breast surgical practice. Breast. 2006;15:713–7. doi: 10.1016/j.breast.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Freed DH. Patient-physician e-mail: Passion or fashion? Health Care Manag (Frederick) 2003;22:265–74. doi: 10.1097/00126450-200307000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Brooks RG, Menachemi N. Physicians’ use of email with patients: Factors influencing electronic communication and adherence to best practices. J Med Internet Res. 2006;8:e2. doi: 10.2196/jmir.8.1.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattison M. Social work practice in the digital age: Therapeutic e-mail as a direct practice methodology. Soc Work. 2012;57:249–58. doi: 10.1093/sw/sws021. [DOI] [PubMed] [Google Scholar]
- 9.Gagnon MP, Légaré F, Labrecque M, Frémont P, Pluye P, Gagnon J, et al. Interventions for promoting information and communication technologies adoption in healthcare professionals. Cochrane Database Syst Rev. 2009;21:CD006093. doi: 10.1002/14651858.CD006093.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawmynaden P, Atherton H, Majeed A, Car J. Email for the provision of information on disease prevention and health promotion. Cochrane Database Syst Rev. 2012;11:CD007982. doi: 10.1002/14651858.CD007982.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pappas Y, Atherton H, Sawmynaden P, Car J. Email for clinical communication between healthcare professionals. Cochrane Database Syst Rev. 2012;9:CD007979. doi: 10.1002/14651858.CD007979.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Vickers AJ, Salz T, Basch E, Cooperberg MR, Carroll PR, Tighe F, et al. Electronic patient self-assessment and management (SAM): A novel framework for cancer survivorship. BMC Med Inform Decis Mak. 2010;10:34. doi: 10.1186/1472-6947-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peleg R, Nazarenko E. Providing cell phone numbers and e-mail addresses to patients: The patient's perspective, a cross sectional study. Isr J Health Policy Res. 2012;1:32. doi: 10.1186/2045-4015-1-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH. Enhancing doctor-patient communication using email: A pilot study. J Am Board Fam Pract. 2005;18:180–8. doi: 10.3122/jabfm.18.3.180. [DOI] [PubMed] [Google Scholar]
- 15.Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient-provider communication: A systematic review. Patient Educ Couns. 2010;80:266–73. doi: 10.1016/j.pec.2009.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient-provider communication: Will it offset office visits and telephone consultations in primary care? Int J Med Inform. 2005;74:705–10. doi: 10.1016/j.ijmedinf.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Couchman GR, Forjuoh SN, Rascoe TG, Reis MD, Koehler B, Walsum KL. E-mail communications in primary care: What are patients’ expectations for specific test results? Int J Med Inform. 2005;74:21–30. doi: 10.1016/j.ijmedinf.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Perlemuter L, Yomtov B. Feasibility and usefulness of dedicated software and e-mail for self-monitoring blood glucose in treating diabetes. Diabet Med. 2002;19:701–2. doi: 10.1046/j.1464-5491.2002.00688_6.x. [DOI] [PubMed] [Google Scholar]
- 19.Boukus ER, Grossman JM, O’Malley AS. Physicians slow to e-mail routinely with patients. Issue Brief Cent Stud Health Syst Change. 2010;21:1–5. [PubMed] [Google Scholar]
- 20.Silk KR, Yager J. Suggested guidelines for e-mail communication in psychiatric practice. J Clin Psychiatry. 2003;64:799–806. doi: 10.4088/jcp.v64n0710. [DOI] [PubMed] [Google Scholar]
- 21.Beckjord EB, Finney Rutten LJ, Squiers L, Arora NK, Volckmann L, Moser RP, et al. Use of the internet to communicate with health care providers in the United States: Estimates from the 2003 and 2005 Health Information National Trends Surveys (HINTS) J Med Internet Res. 2007;9:e20. doi: 10.2196/jmir.9.3.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liederman EM, Morefield CS. Web messaging: A new tool for patient-physician communication. J Am Med Inform Assoc. 2003;10:260–70. doi: 10.1197/jamia.M1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiel JM. The digital divide: Internet and e-mail use by the elderly. Med Inform Internet Med. 2005;30:19–23. doi: 10.1080/14639230500066900. [DOI] [PubMed] [Google Scholar]
- 24.Haase R, Schultheiss T, Kempcke R, Thomas K, Ziemssen T. Use and acceptance of electronic communication by patients with multiple sclerosis: A multicenter questionnaire study. J Med Internet Res. 2012;14:e135. doi: 10.2196/jmir.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bennett AV, Jensen RE, Basch E. Electronic patient-reported outcome systems in oncology clinical practice. CA Cancer J Clin. 2012;62:337–47. doi: 10.3322/caac.21150. [DOI] [PubMed] [Google Scholar]
- 26.Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, et al. Enhancing patient-provider communication with the electronic self-report assessment for cancer: A randomized trial. J Clin Oncol. 2011;29:1029–35. doi: 10.1200/JCO.2010.30.3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neville RG, Marsden W, McCowan C, Pagliari C, Mullen H, Fannin A. A survey of GP attitudes to and experiences of email consultations. Inform Prim Care. 2004;12:201–6. doi: 10.14236/jhi.v12i4.127. [DOI] [PubMed] [Google Scholar]
- 28.Peleg R, Avdalimov A, Freud T. Providing cell phone numbers and email addresses to Patients: The physician's perspective. BMC Res Notes. 2011;4:76. doi: 10.1186/1756-0500-4-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss N. E-mail consultation: Clinical, financial, legal, and ethical implications. Surg Neurol. 2004;61:455–9. doi: 10.1016/j.surneu.2003.09.029. 459. [DOI] [PubMed] [Google Scholar]
- 30.Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board Cochrane Back Review Group. updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 31.Sox HC, Helfand M, Grimshaw J, Dickersin K. Comparative effectiveness research: Challenges for medical journals. In: Tovey D, et al., editors. Am J Manag Care. Vol. 16. PLoS Medicine; 2010. pp. e131–3. [PubMed] [Google Scholar]


