Abstract
Background:
Learning pathology is fundamental for a successful medical practice. In recent years, medical education has undergone a profound transformation toward the development of an integrated curriculum incorporating both basic science and clinical material. Simultaneously, there has been a shift from a magisterial teaching approach to one centered around problem-based learning. Now-a-days, informatics tools are expected to help better implement these strategies.
Aim:
We applied and evaluated a new teaching method based on an active combination of clinical problems, gross pathology, histopathology, and autopsy pathology, all given through informatics tools, to teach a group of medical students at the Universidad de Santander, Colombia.
Design:
Ninety-four medical students were followed in two consecutive semesters. Students were randomized to receive teaching either through traditional methodology or through the new integrated approach.
Results:
There was no significant difference between the intervention group and the control group at baseline. At the end of the study, the scores in the intervention group were significantly higher compared to the control group (3.91/5.0 vs. 3.33/5.0, P = 0.0008). Students and tutors endorsed the benefits of the integrated approach. Participants were very satisfied with this training approach and rated the program an 8.7 out of 10, on average.
Conclusion:
This study confirms that an integrated curriculum utilizing informatics systems provides an excellent opportunity to associate pathology with clinical medicine early in training of medical students. This can be possible with the use of virtual microscopy and digital imaging.
Keywords: Experimental study, learning strategies, medical education, pathology, pathology museum, virtual autopsy, virtual microscopy
INTRODUCTION
A solid understanding of pathology is fundamental for a successful medical practice. In medical education, the subject of pathology has been classically imparted through a combination of theoretical and practical teaching activities, oral lectures, practical clinical autopsies, and exhibition of macro- and micro-scopic specimens in medical museums.[1,2] However, in recent years, medical education has undergone a revolution with the development of a core curriculum that integrates clinical medicine with basic science.[2] Traditional medical curriculum used in western universities teaches pathology as an isolated subject in the preclinical years, and basic science concepts are imparted with limited clinical correlation.[2] There has been a shift away from this magisterial teaching approach toward a system with problem-based learning, where basic science and clinical education are integrated. Such a system better mirrors real medical practice.[3]
Furthermore, the use of new informatics tools is expected to improve the learning process and expand access to medical knowledge.[1,3] Recent years have seen multimedia and information technology rise to dominance in medical education. Concurrently, there has been the gradual disappearance of traditional medical museums and autopsies, despite proven utility in medical education.[2,3,4,5,6] Potentiating the use of these traditional teaching methods through digital strategies should be a priority. In addition, the number of medical students is increasing, and several new medical schools have been opened in response to a recognized need for more doctors. Unfortunately, limitations in direct contact between professors and students are currently well-characterized. At the same time, in this era of personalized and genomic medicine, there has been an explosion of medical knowledge needed to be assimilated by students.[5] Improving student access to information generated from genomics research should remain a priority.[3,7]
In this study, we applied and evaluated a teaching method, which actively combines theoretical lectures with practical sessions in the same classroom setting. Clinical cases were detailed through digital images and videos. Fundamental to this method was exposing students simultaneously to clinical and morphological data. We hypothesize that this method enables students to better understand the pathogenesis and distinctive clinical manifestations of important diseases. Our goals for this combined didactic method were to increase medical student curiosity, better correlate clinical cases with basic science, and improve interactions between students and professors.
MATERIALS AND METHODS
Design
An experimental study was performed between July 2009 and September 2010 to evaluate the efficacy of a new teaching strategy for the subject of pathology. This study compares 3rd year medical students placed in either an intervention group or a control group, with a similar number of participants (47 subjects) in each group [Figure 1]. In both groups, pathology teaching was provided with similar time intensity (10 h/week over a period of 4 months), during the same time of day (afternoon classes and laboratories), and by professors with similar academic background (physicians with board certifications in pathology), following a previously developed curriculum. This study was designed, evaluated, and analyzed by the same group of researchers. The students have not influence in be selected in any of the groups. All educational material was intended to meet medical curriculum requirements recommended by the Colombian National Accreditation Council of Higher Education (CNA) (http://www.cna.gov.co/), under the Latin-America Andres Bello standards (http://www.convenioandresbello.org/) to grant academic titles recognized in Latin-America countries. CNA approval for the intervention was received 1 year before the study, and our curriculum was evaluated as “high quality” (maximum score). Previously, the CNA have also approved the traditional teaching strategy used in the control group.
Figure 1.
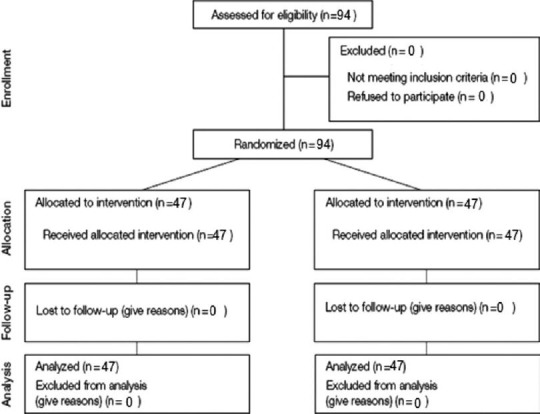
Flow diagram of subject progression through the different phases of the study
Medical Students
All medical students participating in this study were in their 3rd year of medical training (from a total of 6 years) and were followed for two consecutive semesters. Students were randomly assigned to either the intervention group or the control group. The randomization process, evaluations, and analysis were performed in a blinded manner with respect to teaching method and student identifying information. The eligibility criteria were: (1) Be an active student (full-time student) and (2) be able to interact with personal computers during classes. All students participated in the study, and all were deemed eligible for the study. All participants were allocated to one of the study arms, and none were excluded or lost during the study [Figure 1].
Intervention and Control Curriculum
Our medical program is a 5-year academic program followed by 1-year internship and 1-year of supervised general practice. Pathology is taught during the 3rd year, in two consecutive semesters. Each academic semester has duration of 24 weeks for a total of 48 weeks of training in pathology. During this training, students in both the interventional and control groups receive training in general pathology, anatomic pathology (AP), and pathophysiology. The training program is divided into 24-units schedules (2 weeks per unit), and within each unit, the students receive six classes with six clinical cases, covering the following topics:
Basis of human disease
Methods of studying human pathology
Cellular and tissue response to injury and stress
Acute and chronic inflammation
Infectious diseases and poverty-associated diseases
Hemodynamic disorders
Neoplastic diseases
Environmental and nutritional diseases
Genetic, congenital, and childhood diseases
Cardiovascular diseases
Hematologic diseases
Respiratory system diseases
Diseases of the immune system
Diseases of the head and neck
Diseases of the gastrointestinal system
Diseases of the genitourinary system
Diseases of the male genital system
Diseases of the female genital tract and breast
Diseases of the endocrine system
Diseases of the skin
Diseases of the bones, joints, and soft tissue
Diseases of the peripheral nerve and skeletal muscle
Diseases of the central nervous system
Special sensory diseases.
Intervention
Students assigned to receive the new methodology (intervention group) were taught using an integrated system of pathology education with concurrent use of the following components: (a) Theoretical lessons, (b) clinical cases, and (c) virtual autopsy cases, in each unit. In addition, gross pathology and microscopic images were presented digitally in the same classroom as the lectures. The clinical cases, gross pathology images, microscopic images, and virtual autopsies were presented during the classes to meet the requirements of the curriculum. Digital images and videos of physical exam findings, histology, microscopy, radiology, and autopsy associated with different pathologies were presented through a digital projector to be viewed by the class.
Classes proceeded in the following format:
On the 1st day of classes, students formed working groups with 3-5 of their peers (1st day of classes only, 30 min duration)
At the beginning of class, the professor explained the class themes and learning objectives for the day (all sessions, 30 min duration)
-
Molecular, macroscopic, and microscopic characteristics of each pathologic process were detailed and correlated with clinical manifestations and disease complications (all sessions, 90 min duration).
- Presentation of the clinical case
- Presentation of macroscopic and microscopic findings on gross pathology through digital projection
- Presentation of histological and molecular pathology for each case through digital projection
- Correlation of clinical case with pathology by lecture
Elaboration of summaries and conceptual maps for each theme and for each student group (all sessions, 30 min duration)
Assignment of selected reading material for homework to further develop critical reading skills and complement classwork
Ongoing review of prior week's content. Unclear or difficult concepts are clarified, and student questions are resolved (one session during the week, generally the first class after the weekend, 45 min duration).
Information Technology Used
To provide students with a realistic pathology experience, multimedia included digital videos, digital photographs, whole slide images, digital photomicrographs and audio recording. All information was provided to the class using an Epson cinema projector. The digital videos and audios of autopsies and physical exams were recorded using a Samsung Camcorder with 2.7” LCD Screen and HD video recording (Import). The digital photographs of radiology images and gross pathology were obtained using a Nikon Coolpix digital camera. Finally, microphotographs were obtained using an Olympus C × 31 microscope with a digital camera adapter, and a NanoZoomer whole-slide scanner.
Control
Students in the control group received traditional teaching method. This approach includes standard auditorium-based theoretical lectures (90 min duration) and separate laboratory sessions involving microscopic and gross pathology (90 min). Laboratory sessions are guided by a professor who explains key pathological features and resolves any questions. The material provided to the intervention group for homework was also provided to the control group.
Evaluation
After completing the course, students in both arms of the study were evaluated with the same theoretical/practical exam. The exam was previously designed to quantify student performance and evaluate their knowledge of course material. The exam is composed of 100 multiple-choice questions, each with five options and only one right answer. The exam assesses whether medical school students can apply important concepts of pathology to the practice of medicine. Each Student's score was calculated from 0.0 to 5.0, with each correct answer yielding 0.05 points. This test has been administered after every pathology course over the last 10 years, and is modeled after the Colombian National Examination for Higher Education in Medicine (Saber-pro), a professional exam sponsored by the Colombian Institute for the Promotion of Higher Education (http://www.icfes.gov.co/examenes/saber-pro). The exam is mandatory for aspiring physicians to obtain a Colombian Medical License and access to Graduate Medical Education (http://tramites.minsalud.gov.co/tramitesservicios/tarjetaMedico/Default.aspx).
Survey
To evaluate the new teaching methodology, a three-question anonymous survey was provided to medical students in the interventional group and to professors. The following questions were asked:
Are you satisfied with the methodology of teaching used in your pathology classes? Participants were asked to rate the teaching method from 0.0 (poorly recommended) to 10 (highly recommended)
Do you consider yourself well-prepared in the subject of pathology? (yes or no question)
Were these activities stressful or anxiety-provoking? (yes or no question).
Ethical Aspects
This study was planned according to the Declaration of Helsinki and approved by the Institutional Review Board of the University of Santander. This experiment was categorized as having minimal risk to participants in either the intervention or control group. Informed consent was obtained from all medical students involved in the study. Consent from patients and family members who provided the clinical information was previously obtained. Confidentiality of all data was maintained.
Statistical Analysis
Nominal variables were evaluated with proportional statistics and differences between groups were calculated using the Chi-square test. Means and central tendency statistics of exam scores were calculated for each group and compared with an independent samples t-test. The significance level was set at 0.05. Statistical analysis was performed in Stata 11.0.
RESULTS
Ninety-four medical students, enrolled in the pathology course, were analyzed. The students were divided into two groups with similar demographics [Table 1, and Figure 2] at baseline. After the course, higher exam scores were observed in the intervention group compared to the control group (3.91 vs. 3.33, P = 0.0008) [Figure 3]. No gender differences were observed. The two groups did not differ with respect to academic performance in concurrent classes (immunology and microbiology): no failing grades were noted in either group, or both groups attained similar proficiency in these subjects. The survey distributed to students and tutors in the intervention group revealed a high satisfaction score, averaging an 8.7 out of 10 in students and 8.5 out of 10 in professors. A large percentage of students (95.7%) find this method not stressful or anxiety provoking, and 89.3% (42 students) consider themselves well-prepared in the subject of pathology.
Table 1.
Comparison of features between intervention and control groups
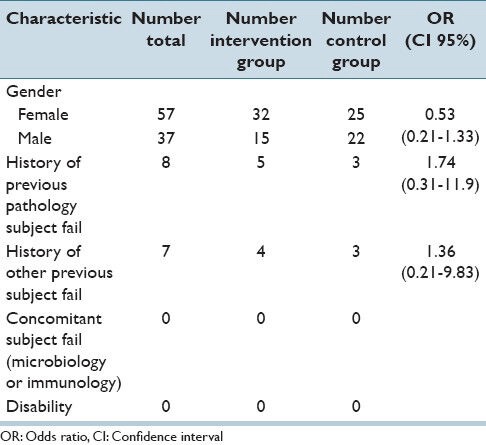
Figure 2.
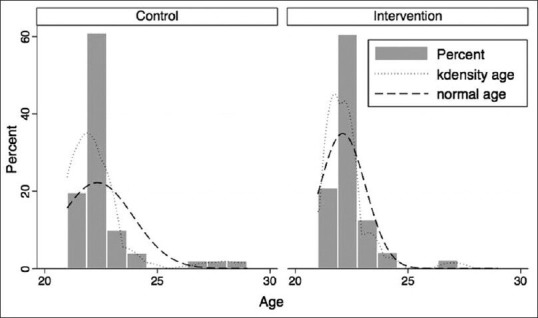
Age distributions of intervention and control groups
Figure 3.
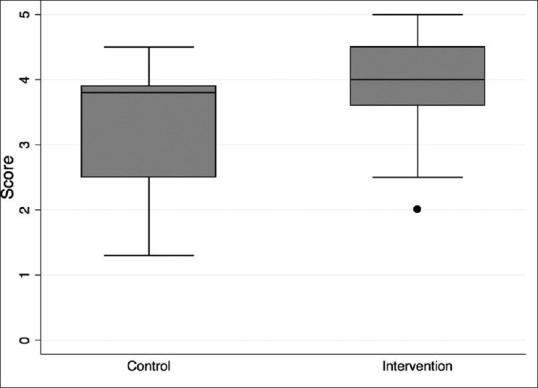
Score distribution between control and intervention groups. The score mean for the control group was 3.33 ± 0.9 versus 3.91 ± 0.7 in the intervention group (F test = 12.1091; P = 0.0008)
DISCUSSION
Medical education is constantly evolving. Appropriate training in anatomical and functional pathology is essential for a satisfactory medical practice.[2,3] Pathology is defined as the study of disease, and the all-encompassing nature of this definition reflects the importance of this subject matter in medical education. However, the optimal approach for pathology teaching in medical students is currently debated.[6] Traditional learning systems utilize textbooks, oral lectures, gross specimens, and microscopy of tissue on glass sides. Recently, however, the availability of new informatics tools has created the opportunity for new strategies in teach this subject matter.[6] Potential benefits include the capacity to teach multiple students simultaneously, avoidance of ethical and biological risks implicit in using human specimens, cost-effectiveness, and better distribution of clinically relevant knowledge to students.[1,6,8,9] Currently, these benefits are still under evaluation.
Traditional pathology education has been previously shown to be fairly effective. However, multiple problems have been identified with each aspect of the traditional approach, thus driving the search for new educational methods.[6,10]
Medical knowledge has increased exponentially in recent years, to the point where thousands of scientific papers and hundreds of textbooks are produced each year in AP alone.[10] This quantity of information is far too vast for a medical student to efficiently digest and also apply to clinical medicine.[11,12,13] Oral lectures focus on providing summaries of this information to a passive audience of students.[11] The medical classroom needs a pedagogical basis in order to be meaningful for students.[9,12] Unfortunately, passive learning limits the opportunity for reflection, interaction, creativity, clinical correlation and generative thinking.[2,4,8,11] A structural change in how medical schools educate students in the subject of pathology is necessary.[2] Without a peer-based learning group, students also have reduced opportunity to develop social skills in an academic setting. Other limitations of the lecture format include the lack of opportunity for self-reflection and social awareness. There is very limited individual interaction when one professor lectures hundreds of students in an auditorium, and most communication is unidirectional.[14,15,16] These obstacles limit the opportunity for burgeoning physicians to develop the collaborative skills vital for a thriving clinical practice.
In AP, the practical component of the traditional teaching strategy is based around the analysis of macroscopic specimens and histology slides in medical museums, as well as, the use of clinical autopsies.[15,16,17] These methods are extremely effective in teaching medical students, because they provide a first-hand look at morphological manifestations of disease.[15] However, they are not without limitations, including the lack of clinical correlation,[11,12] a limited number of samples for analysis, and the biological and ethical risks of specimen manipulation.[13] Macroscopic samples are usually preserved in glass jars containing a formalin-based solution. These specimens are usually fully labeled such that medical students can view and study them in a self-guided fashion.[15,16] This exposure of medical students to formalin solution, an oncogenic compound, is currently an area of debate.[17] Furthermore, preserved pathology specimens are fragile, and the cost of maintaining these specimens is increasing. As a result, it would be useful to study certain alternatives to this approach. For microscopic study, most medical schools have teaching laboratories equipped with optical microscopes and histological slides from a number of diseases.[3,18] However, laboratory work is limited by time and personnel restrictions because in this setting, professors and students typically interact on a one-on-one basis.[19] Finally, the use of clinical autopsy as a teaching tool has significantly declined, strongly influenced by worldwide reduction in consented clinical autopsies.[16] Reasons for this decline include negative public attitudes in the wake of organ retention scandals,[19,20] medical provider attitudes, biological risks, legal concerns, and family ethical and religious dilemmas.[20] Autopsies, as a teaching tool, provide valuable information to preclinical medical students by integrating knowledge with clinical skills, while promoting both deductive reasoning and clinical problem solving.[16,19] Some have also suggested that exposure to autopsies during medical school will help future doctors understand the autopsy process and its utility, potentially making students more likely to recommend autopsies to family members of future patients.[19,20]
Integration of biomedical disciplines is fundamental to excellence in research and medical education. Pathology, which studies the entire spectrum of human disease, is a keystone of this process.[21] Now, more than ever, there is a need to integrate different areas of medicine to help unveil important disease characteristics at both the molecular and clinical level.[21,22,23] The need for integrated medical training has become more urgent today. With the recent introduction of competency-based programs, time limitations and financial constraints are contributing to decreased opportunities for “learning by doing” in clinical areas.[23,24] However, with rising availability of high-resolution imaging, classroom-based computers with audiovisual systems have provided a new teaching tool within this environment.
In this study, we evaluate a strategy based around an integrated medical curriculum, which maximizes student learning by correlating basic science pathology with clinical scenarios. Learning is further facilitated with the use of informatics tools, virtual microscopy, and digital imaging. This system also highlights the importance of teamwork and prepares medical students for the healthcare environment.[9,22,23]
This strategy is particularly useful in this era of genomic medicine, where large quantities of molecular data are generated, and appropriate clinical correlation is needed. This can increase the ability of future physicians to better interpret genetic and molecular tests.
This strategy was developed based on cognitive load theory, which assumes that the human cognitive system has a limited working memory.[9,24] In contrast, long-term memory has no such restrictions.[9] Through problem-solving activities applied to clinical cases, our curriculum attempts to construct and organize information for easy recall later.[23,24,25,26] This strategy of integrating information can help students establish fully automated schemas for understanding human disease and health during medical school.[27,28,29,30,31,32,33]
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2014/5/1/25/137729
REFERENCES
- 1.Gabril MY, Yousef GM. Informatics for practicing anatomical pathologists: Marking a new era in pathology practice. Mod Pathol. 2010;23:349–58. doi: 10.1038/modpathol.2009.190. [DOI] [PubMed] [Google Scholar]
- 2.Mortimer R, Lakhani S. Pathology in education and practice: A time for integration? Aust Health Rev. 2008;32:319–21. doi: 10.1071/ah080319. [DOI] [PubMed] [Google Scholar]
- 3.Venkatesh SK, Wang G, Seet JE, Teo LL, Chong VF. MRI for transformation of preserved organs and their pathologies into digital formats for medical education and creation of a virtual pathology museum. A pilot study. Clin Radiol. 2013;68:e114–22. doi: 10.1016/j.crad.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Donner RS, Bickley H. Problem-based learning in American medical education: An overview. Bull Med Libr Assoc. 1993;81:294–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Edelbring S, Dastmalchi M, Hult H, Lundberg IE, Dahlgren LO. Experiencing virtual patients in clinical learning: A phenomenological study. Adv Health Sci Educ Theory Pract. 2011;16:331–45. doi: 10.1007/s10459-010-9265-0. [DOI] [PubMed] [Google Scholar]
- 6.Charlton R. Autopsy and medical education: A review. J R Soc Med. 1994;87:232–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Kalinski T, Zwönitzer R, Rossner M, Jonczyk-Weber T, Hofmann H, Roessner A, et al. Treasures from the attic: Transparencies digitally remastered and used for web-based pathology training and education. Histopathology. 2011;59:1263–6. doi: 10.1111/j.1365-2559.2011.03972.x. [DOI] [PubMed] [Google Scholar]
- 8.Holland L, Bosch B. Medical students’ perceptions of pathology and the effect of the second-year pathology course. Hum Pathol. 2006;37:1–8. doi: 10.1016/j.humpath.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 9.van Merriënboer JJ, Sweller J. Cognitive load theory in health professional education: Design principles and strategies. Med Educ. 2010;44:85–93. doi: 10.1111/j.1365-2923.2009.03498.x. [DOI] [PubMed] [Google Scholar]
- 10.Ogino S, King EE, Beck AH, Sherman ME, Milner DA, Giovannucci E. Interdisciplinary education to integrate pathology and epidemiology: Towards molecular and population-level health science. Am J Epidemiol. 2012;176:659–67. doi: 10.1093/aje/kws226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamilton PW, Wang Y, McCullough SJ. Virtual microscopy and digital pathology in training and education. APMIS. 2012;120:305–15. doi: 10.1111/j.1600-0463.2011.02869.x. [DOI] [PubMed] [Google Scholar]
- 12.Dee FR. Virtual microscopy in pathology education. Hum Pathol. 2009;40:1112–21. doi: 10.1016/j.humpath.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Nelson D, Ziv A, Bandali KS. Going glass to digital: Virtual microscopy as a simulation-based revolution in pathology and laboratory science. J Clin Pathol. 2012;65:877–81. doi: 10.1136/jclinpath-2012-200665. [DOI] [PubMed] [Google Scholar]
- 14.Kanthan R, Senger JL. The impact of specially designed digital games-based learning in undergraduate pathology and medical education. Arch Pathol Lab Med. 2011;135:135–42. doi: 10.5858/2009-0698-OAR1.1. [DOI] [PubMed] [Google Scholar]
- 15.Marreez YM, Willems LN, Wells MR. The role of medical museums in contemporary medical education. Anat Sci Educ. 2010;3:249–53. doi: 10.1002/ase.168. [DOI] [PubMed] [Google Scholar]
- 16.Talmon G. The use of autopsy in preclinical medical education: A survey of pathology educators. Arch Pathol Lab Med. 2010;134:1047–53. doi: 10.5858/2009-0333-OA.1. [DOI] [PubMed] [Google Scholar]
- 17.Hope CK, Griffiths DA, Prior DM. Finding an alternative to formalin for sterilization of extracted teeth for teaching purposes. J Dent Educ. 2013;77:68–71. [PubMed] [Google Scholar]
- 18.Mattick K, Marshall R, Bligh J. Tissue pathology in undergraduate medical education: Atrophy or evolution? J Pathol. 2004;203:871–6. doi: 10.1002/path.1601. [DOI] [PubMed] [Google Scholar]
- 19.Bamber AR, Quince TA, Barclay SI, Clark JD, Siklos PW, Wood DF. Medical student attitudes to the autopsy and its utility in medical education: A brief qualitative study at one UK medical school. Anat Sci Educ. 2014;7:87–96. doi: 10.1002/ase.1384. [DOI] [PubMed] [Google Scholar]
- 20.Burton JL. The autopsy in modern undergraduate medical education: A qualitative study of uses and curriculum considerations. Med Educ. 2003;37:1073–81. doi: 10.1046/j.1365-2923.2003.01710.x. [DOI] [PubMed] [Google Scholar]
- 21.Magid MS, Cambor CL. The integration of pathology into the clinical years of undergraduate medical education: A survey and review of the literature. Hum Pathol. 2012;43:567–76. doi: 10.1016/j.humpath.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Farah CS, Maybury T. Implementing digital technology to enhance student learning of pathology. Eur J Dent Educ. 2009;13:172–8. doi: 10.1111/j.1600-0579.2009.00570.x. [DOI] [PubMed] [Google Scholar]
- 23.Lyon P, Letschka P, Ainsworth T, Haq I. An exploratory study of the potential learning benefits for medical students in collaborative drawing: Creativity, reflection and ‘critical looking’. BMC Med Educ. 2013;13:86. doi: 10.1186/1472-6920-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fastré GM, van der Klink MR, van Merriënboer JJ. The effects of performance-based assessment criteria on student performance and self-assessment skills. Adv Health Sci Educ Theory Pract. 2010;15:517–32. doi: 10.1007/s10459-009-9215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruch LA, De Young BR, Kreiter CD, Haugen TH, Leaven TC, Dee FR. Competency assessment of residents in surgical pathology using virtual microscopy. Hum Pathol. 2009;40:1122–8. doi: 10.1016/j.humpath.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Janssen-Noordman AM, Merriënboer JJ, van der Vleuten CP, Scherpbier AJ. Design of integrated practice for learning professional competences. Med Teach. 2006;28:447–52. doi: 10.1080/01421590600825276. [DOI] [PubMed] [Google Scholar]
- 27.Fokkema JP, Teunissen PW, Westerman M, van der Lee N, van der Vleuten CP, Scherpbier AJ, et al. Exploration of perceived effects of innovations in postgraduate medical education. Med Educ. 2013;47:271–81. doi: 10.1111/medu.12081. [DOI] [PubMed] [Google Scholar]
- 28.Nelson EA, McGuire AL. The need for medical education reform: Genomics and the changing nature of health information. Genome Med. 2010;2:18. doi: 10.1186/gm139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bok HG, Teunissen PW, Favier RP, Rietbroek NJ, Theyse LF, Brommer H, et al. Programmatic assessment of competency-based workplace learning: When theory meets practice. BMC Med Educ. 2013;13:123. doi: 10.1186/1472-6920-13-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tjiam IM, Schout BM, Hendrikx AJ, Scherpbier AJ, Witjes JA, van Merriënboer JJ. Designing simulator-based training: An approach integrating cognitive task analysis and four-component instructional design. Med Teach. 2012;34:e698–707. doi: 10.3109/0142159X.2012.687480. [DOI] [PubMed] [Google Scholar]
- 31.Feero WG, Green ED. Genomics education for health care professionals in the 21st century. JAMA. 2011;306:989–90. doi: 10.1001/jama.2011.1245. [DOI] [PubMed] [Google Scholar]
- 32.Szymas J, Lundin M. Five years of experience teaching pathology to dental students using the webmicroscope. Diagn Pathol. 2011;6(Suppl 1):S13. doi: 10.1186/1746-1596-6-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fónyad L, Gerely L, Cserneky M, Molnár B, Matolcsy A. Shifting gears higher – Digital slides in graduate education – 4 years experience at Semmelweis University. Diagn Pathol. 2010;5:73. doi: 10.1186/1746-1596-5-73. [DOI] [PMC free article] [PubMed] [Google Scholar]


