Abstract
The Partners HealthCare system's Clinical Fellowship in Pathology Informatics (Boston, MA, USA) faces ongoing challenges to the delivery of its core curriculum in the forms of: (1) New classes of fellows annually with new and varying educational needs and increasingly fractured, enterprise-wide commitments; (2) taxing electronic health record (EHR) and laboratory information system (LIS) implementations; and (3) increasing interest in the subspecialty at the academic medical centers (AMCs) in what is a large health care network. In response to these challenges, the fellowship has modified its existing didactic sessions and piloted both a network-wide pathology informatics lecture series and regular “learning laboratories”. Didactic sessions, which had previously included more formal discussions of the four divisions of the core curriculum: Information fundamentals, information systems, workflow and process, and governance and management, now focus on group discussions concerning the fellows’ ongoing projects, updates on the enterprise-wide EHR and LIS implementations, and directed questions about weekly readings. Lectures are given by the informatics faculty, guest informatics faculty, current and former fellows, and information systems members in the network, and are open to all professional members of the pathology departments at the AMCs. Learning laboratories consist of small-group exercises geared toward a variety of learning styles, and are driven by both the fellows and a member of the informatics faculty. The learning laboratories have created a forum for discussing real-time and real-world pathology informatics matters, and for incorporating awareness of and timely discussions about the latest pathology informatics literature. These changes have diversified the delivery of the fellowship's core curriculum, increased exposure of faculty, fellows and trainees to one another, and more equitably distributed teaching responsibilities among the entirety of the pathology informatics asset in the network. Though the above approach has been in place less than a year, we are presenting it now as a technical note to allow for further discussion of evolving educational opportunities in pathology informatics and clinical informatics in general, and to highlight the importance of having a flexible fellowship with active participation from its fellows.
Keywords: Clinical informatics curriculum, clinical informatics teaching, pathology informatics, pathology informatics curriculum, pathology informatics teaching
BACKGROUND
The Pathology Informatics Fellowship
The Partners HealthCare system's Clinical Fellowship in Pathology Informatics (Boston, MA, USA) has been described previously.[1,2,3,4] The program was established at an academic medical center (AMC) in a large health care network in 2008, and its charter was approved by the network's education committee for an enterprise-wide fellowship in 2010. It currently operates at two AMCs, as well as community hospitals, enterprise-wide clinical laboratories and research facilities. It has 28 active faculty members, who collectively represent all pathology's subspecialties and devote significant parts of their practices to pathology informatics and its advancement through research. Three members of this faculty comprise the fellowship's executive group with one of these individuals serving as the program director. The program has six active fellows and has graduated eight fellows since 2009.
The educational structure of the fellowship is divided into customized and required components [Table 1]. The customized components include operational and research rotations in addition to clinical concentrations (all with the opportunity for mentorship). Though they are individualized to each fellow's interests and career goals and are designed to cultivate expertise in specific areas of pathology informatics, it is the diversity of faculty interests that engenders the diversity of educational opportunities available to the fellows.
Table 1.
Pathology informatics fellowship program components (adapted from McClintock et al.)
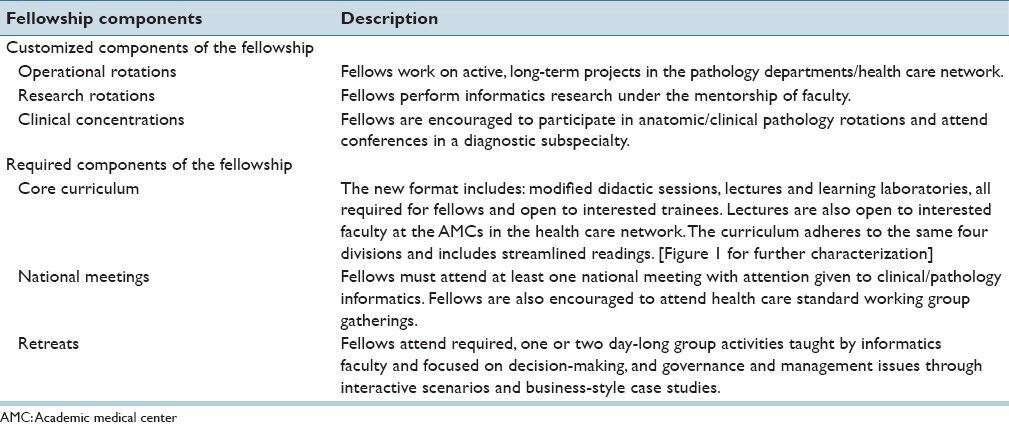
The required components of the fellowship consist of group activities for the fellows and include participation in a core curriculum and educational retreats, in addition to attendance at national meetings. These fixed elements are designed to provide a shared view of the breadth of pathology informatics. The core curriculum is the heart of the required portion of the fellowship. It was conceived of and developed by the fellowship classes of 2011 and 2012 when the program began accepting more than one fellow. Of note, these classes tailored the construction of the core curriculum to meet their educational and scheduling needs. This initiative of fellows (with faculty oversight and support) defining the educational structure of the fellowship is a significant one and consistent with our belief that fellows are in the best position to determine those educational techniques that work best for them. Nevertheless, in keeping with the new subspecialty certification examination for clinical informatics, the fellowship has been demonstrated to be comparable to those initial guidelines elaborated upon by the American Medical Informatics Association,[1] and will continue to develop as more information concerning clinical informatics fellowships becomes available.
The core curriculum includes 92 topics, each with associated readings, distributed across four main divisions: Information fundamentals, information systems, workflow and process, and governance and management. Briefly, these divisions were derived from an exhaustive review of the informatics literature and are, in the authors’ opinion, the broadest, yet most precise categories for an approach to understanding and mastering the scope of the field. Though no system is perfect, these four divisions have served as the cornerstones for all assigned and elective readings, which themselves date back to informatics-related pursuits in the Boston medical community as early as 1940. Since the curriculum's inception, the mechanism for discussing these 92 topics and reviewing accompanying readings has been weekly group didactic sessions with the program director. The curriculum is thus designed to last approximately two years, but its duration can be modified as needed. An extensive description of the core curriculum has been published previously.[2]
Changes to the Delivery of the Core Curriculum
At the beginning of the 2013-14 academic year the fellows, in conjunction with the faculty, made several major changes to the delivery of the core curriculum:
The weekly didactic sessions with the program director were changed from a review of the curriculum and reading assignments to group discussions of each fellow's current activities and updates on the major enterprise-wide informatics projects, both with focused questions about and points of emphasis from a streamlined body of literature.
A weekly informatics lecture series was instituted. It is required for fellows, and made available to all residents and faculty at the network's AMCs.
Monthly “learning laboratories”, led by members of the fellowship's executive group, were implemented. The learning laboratories are required for fellows, but open to interested residents and rotating medical students.
The Reasons for Change
The changes to the delivery of the core curriculum were driven by the fellows, all of whom are authors of this manuscript. The reasons for this new approach are as follows:
-
The latest class of fellows has a distinct personality, group dynamic and approach to learning. The back and forth nature of the original didactic sessions neither complemented nor maximized the fellows’ collective and individual capabilities.
- As has been demonstrated in the educational field, there exists no one-size-fits-all approach to teaching or learning. Some evidence suggests that educators will benefit their students by tailoring educational approaches to learning styles because students will be more satisfied with their learning experiences and because they will spend less time realigning the materials they take in with their own learning styles.[5] With this dynamic in mind, it is not surprising that, in a fellowship containing only a fluctuating handful of fellows from year to year and in its infancy with no well-established standards to date, the educational needs and tactics of the latest group of faculty and fellows differ from those in previous years. We expect this trend to continue moving forward.
-
Large, enterprise-wide information technology (IT) projects have put time pressure on the program director and become educational undertakings in their own right.
- In late 2012, the network began near-side-by-side implementations of an electronic health record (EHR) and laboratory information system (LIS). The demands associated with installing these systems, in conjunction with the simultaneous initiative of the network's five primary pathology departments to operate more as an enterprise-wide unit, placed significant demands on the resources and schedules of the program director. Said implementations also quickly became useful educational tools, discussions of which ultimately competed with those intended for the core curriculum's didactic sessions. The latest group of fellows likewise found themselves consistently needing to augment the existing collection of readings so as to facilitate a better understanding of the new technologies being installed and the business and IT models underpinning this installation process. These additional, real-time demands thus necessitated modifications to the previously adopted approach of discussing weekly readings. Likewise, developing methods to better weave such projects into the fellowship's fabric, both from educational and fellow participation standpoints, subsequently became higher priorities.
-
A desire to better leverage the growing number of pathology informatics faculty members (and their wide range of interests, knowledge and skills) in the fellowship program
- During the first five years of the fellowship, the number of pathology informatics faculty across the network has increased from 11 to 28 with representation from virtually all pathology domains and subspecialties. It is the opinion of the authors that the pathology informatics faculty across the network possesses a collective body of experience and interests that can sufficiently deliver the content of the core curriculum and simultaneously demonstrate its clinical and research interests. It thus seemed appropriate to distribute teaching responsibilities from the program director to the rest of the faculty.
-
A need to support resident education in pathology informatics
- A growing excitement surrounding pathology informatics has emerged across the network, particularly at its AMCs. Of late, trainees have become increasingly aware of pathology informatics as a discipline and increasingly interested in taking part in related clinical, educational and investigational activities. This has led to increasing pressure to provide informatics teaching for the approximately 75 residents in the two pathology training programs at the network's AMCs. Though it had always made sense to incorporate particular aspects of the fellowship (especially the didactic sessions) into residency training, this rise in popularity called for new teaching accommodations, approaches and venues.
-
Geographic distribution and the 1 + 1 pathology informatics track
- The fellowship program has a fairly large number of active fellows (six at the time of manuscript submission) and operates over a sizable region (the greater Boston area). As previously described, our fellows seeking to meld pathology informatics into a traditional pathology subspecialty follow a 1 + 1 fellowship track, in which one commits to a year of informatics and a year of a second subspecialty.[3] In this way, the combination of space and varying commitments has made it increasingly difficult for six fellows to meet in the same location and at the same time every week, thus necessitating the distribution of teaching over a wider range of mediums and venues.
This manuscript serves to characterize the fellowship's solutions to the challenges identified above via: (1) A modification of the existing didactic session structure, (2) the establishment of a network-wide pathology informatics lecture series and (3) the creation of regular learning laboratories. Though the approach is still in a pilot phase, given the active discussion surrounding clinical informatics fellowships, its timely characterization allows for a continued dialogue on evolving approaches to education in pathology informatics and clinical informatics.
PROCEDURE AND APPROACH
The modalities the fellowship has adopted (modified didactic sessions, lectures and learning laboratories) represent a distributed responsibilities approach that involves more faculty members and includes more teaching avenues [Figure 1].
Figure 1.
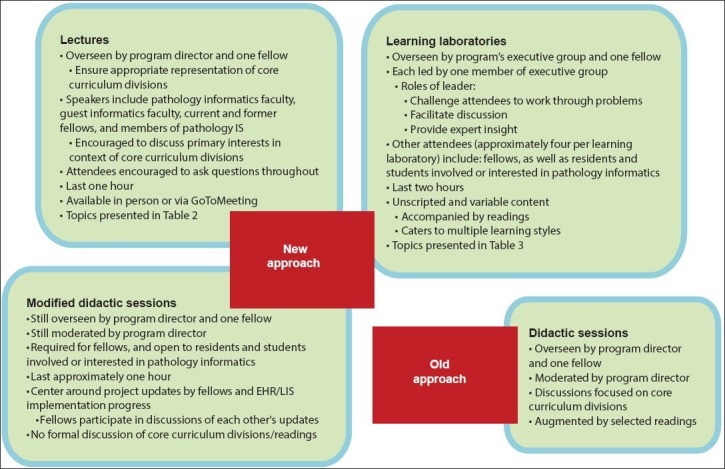
Approaches to delivering the core curriculum of a pathology informatics fellowship; IS -information systems, EHR - electronic health record, LIS - laboratory information system
Weekly Didactic Sessions
Weekly group meetings between the fellows, interested residents, rotating medical students and the program director continue, but formal discussions of the core curriculum's divisions, associated topics and readings have been de-emphasized. Instead, the meetings center around a discourse between the program director and each fellow regarding updates on her or his clinical or research projects with the director highlighting teaching points where applicable. The fellows are expected to participate in each other's updates by way of constructive comments and questions. There are also discussions about the progress of the enterprise-wide EHR and LIS projects, especially on those aspects of each to which the fellows seldom have direct access. Given these modifications, the new didactic sessions last approximately one hour. When appropriate, we examine themes from the week's readings in the context of the above discussions. As part of this effort, the reading list has been streamlined to a shorter selection of articles, texts and text excerpts. Nevertheless, the original list is still available to those who wish to delve deeper into any of the 92 topics.
Lectures
The lectures are overseen by the program director in association with one of the fellows. The series commenced in September 2013 and will span the current and future academic years. Each lecture has duration of one hour. Speakers include the pathology informatics faculty within the network, guest informatics faculty, current and former fellows, and members of the pathology information systems team. Subjects cover a wide array of clinical, investigational and operational aspects of pathology informatics, and the director encourages speakers to provide as much context as possible with respect to the topics contained in the four divisions of the core curriculum. The director and fellow also track the distribution of lectures among these four divisions to ensure each is represented appropriately. Table 2 shows those lectures that have transpired as of the time of manuscript submission, in addition to several future topics.
Table 2.
Pathology informatics lecture topics (in order of presentation)
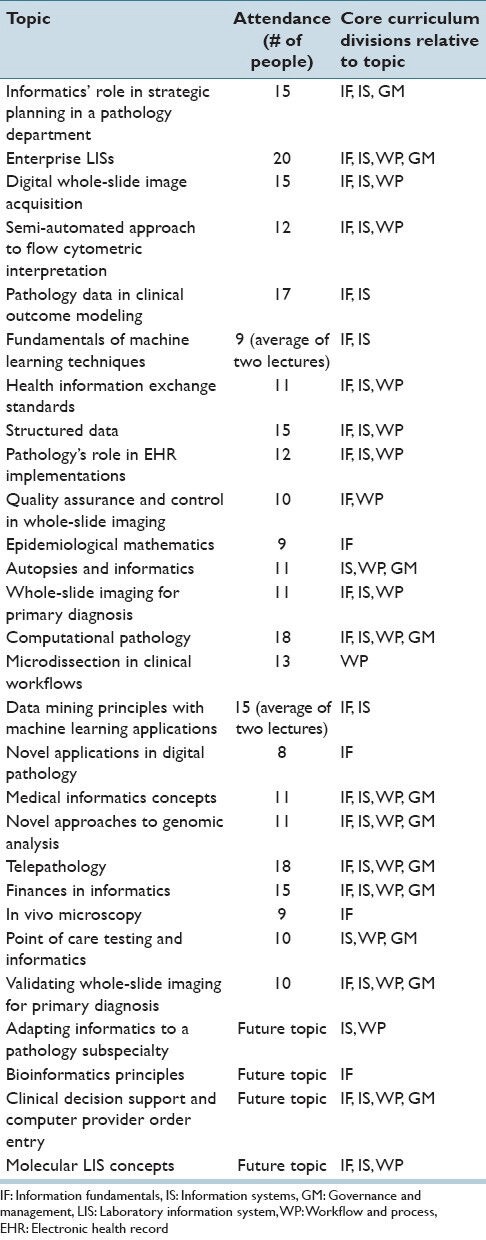
Though the lectures are given in a conference room at one of the AMCs, each is also available across the network through GoToMeeting (Citrix Systems, Inc., Santa Barbara, CA, USA). In a departure from traditional pathology lectures at the AMCs in the network, attendees are encouraged to ask questions and facilitate discussions throughout each lecture. The average attendance to date is 13 people, of which approximately one-third participate through GoToMeeting.
Learning Laboratories
The learning laboratories are overseen by the faculty members of the executive group in association with one of the fellows. Each learning laboratory is led by one such faculty member and lasts approximately two hours. Non-faculty attendees, who typically number approximately four, include fellows, residents and students at the AMCs who are involved or interested in pathology informatics.
The learning laboratories’ content consists of a kaleidoscope of subjects in pathology informatics [Table 3]. The overarching principle of each learning laboratory is to build upon the four divisions of the core curriculum. Unlike the lectures, the manner in which this content is delivered and digested is variable and unscripted [Table 3]. Approaches not yet incorporated into a learning laboratory session include: Interface development, large data set evaluation (with or without statistical software analyses), programming and software training. As Table 3 suggests, the goal of the learning laboratory is to create an educational environment that diverges from those of the lectures and features active participation by all attendees. Likewise, the role of a learning laboratory's faculty leader is to challenge the attendees to work through a variety of problems and topics, facilitate (but not dominate) discussion among attendees, and provide expert insight. The typical learning laboratory is accompanied by reading assignments in advance of the session. The faculty leader and fellows select readings and topic formats after a discussion of the objectives of a given learning laboratory.
Table 3.
Pathology informatics learning laboratory topics and formats
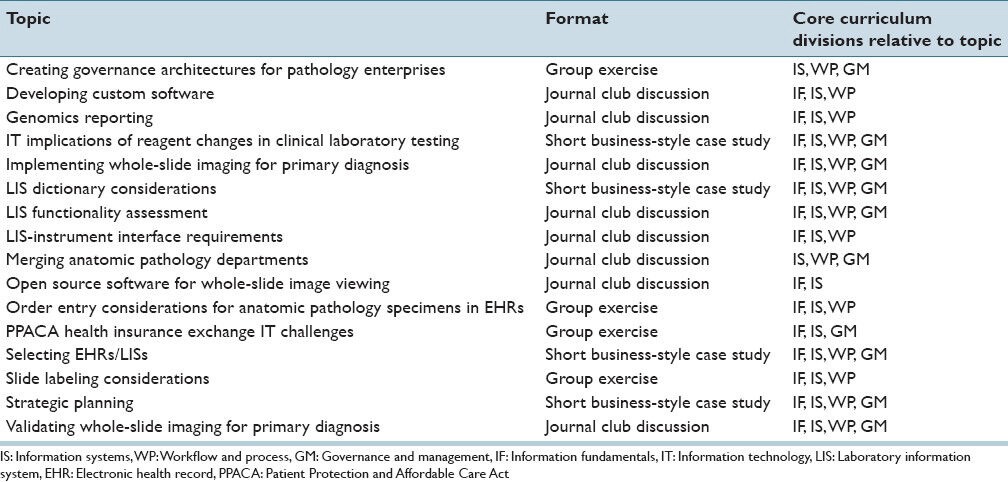
The concept of the learning laboratory is a product of the requests of the fellows, in part, to re-create the give-and-take of the business-style case studies from the retreats. Again, though business-style case studies are not the only medium employed, the authors’ goal is to, as Lee et al. described, “better simulate activities such as brainstorming, consensus-building, and decision-making by a group of individuals”.[4] Additional objectives include the creation of a forum for discussing real-time and real-world pathology informatics matters, developing differential diagnoses for challenges in health care IT and bringing to light creative and viable solutions for these challenges, and incorporating awareness of and timely discussions about the latest pathology informatics literature. From a learning style standpoint, another goal is to engender a teaching session that caters to multiple such styles. Lastly, as learning laboratories are driven mostly by their non-faculty attendees, they also allow for a certain level of self-teaching and learning from making mistakes in a constructive and experience-rich environment.
DISCUSSION
The Partners HealthCare system's Clinical Fellowship in Pathology Informatics is a work in progress in many respects, owing to its relative infancy, the shifting concepts of education in pathology informatics and the inherent broad scope of the field itself. With these factors in mind, this fellowship was instituted with attention to fellow participation and flexibility. In reality, the fellowship has undergone major changes almost every year since its inception [Figure 2]. Such changes exemplify the anticipated growth and maturation (but not maturity) of the fellowship.
Figure 2.
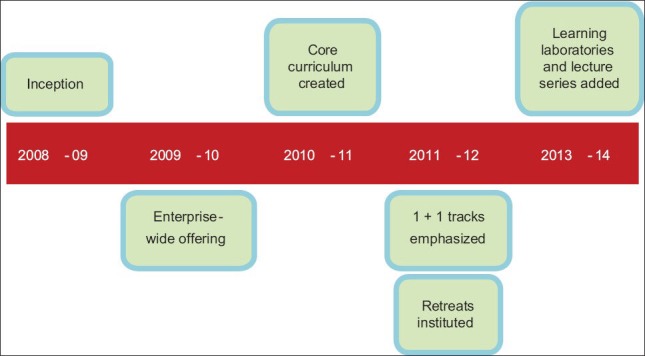
Evolution of the educational activities of a pathology informatics fellowship; 1 + 1 track -one year of pathology informatics training followed by one year of training in another pathology subspecialty with continued participation in the core curriculum
Recent developments within the health care network, including the ramping up of EHR and LIS implementation efforts, an exciting increase in interest in pathology informatics at the network's AMCs, and the demands of each fellow's unique set of activities and learning styles have challenged the previous approach to delivering the fellowship's core curriculum. In response, the fellowship has modified said delivery via the restructuring of its existing didactic course and the institution of lectures and learning laboratories. Though the lecture series and the learning laboratories would not be possible without continued support by departmental leadership and an ever-growing pathology informatics faculty, it is the engaged and sizeable group of fellows who have most driven this natural evolution, which will only continue as the program grows. For example, our program is working with other organizations within the network to implement an Accreditation Council for Graduate Medical Education-accredited clinical informatics fellowship. Though many aspects of the existing clinical fellowship in pathology informatics will integrate into this new clinical informatics fellowship, as the majority of our fellows are now planning to take the Clinical Informatics Subspecialty Board Examination, we will need to tailor training opportunities in this regard as well.[3] We are also in the process of leveraging the fellowship, including the modified didactic sessions, lecture series and learning laboratories, to reconfigure resident training in pathology informatics. In these contexts, this technical note serves to highlight mechanisms or mediums by which to teach the content of a core curriculum in pathology informatics.
Though there are only six fellows, lecture attendance averages 13 people. Keeping in mind that this is a new, subspecialty educational lecture series, the authors are quite encouraged by this figure, especially since no other subspecialty at either AMC in the network holds such a regular lecture series. The fellowship hopes to further boost attendance by offering continuing medical education (CME) credits in the coming academic year and opening each lecture to a broader audience, including the entire pathology community in the network and affiliated groups outside the network. In so doing, the fellowship also hopes to recruit more speakers, not only in pathology informatics, but in the larger clinical informatics community as well. From a logistics standpoint, the lecture series has indeed helped to relieve the program director of his responsibilities as the primary instructor of the fellows. As expected, it has also increased the visibility of the fellows to the faculty and vice versa. This has already resulted in three new collaborative efforts, and we expect it will serve our fellowship well moving forward.
Though the learning laboratories do not feature any one new approach to education, their variable structure, specifically their focus on active participation by all attendees, has created an environment for a diverse delivery of the core curriculum to the disparate learning styles of the latest class of fellows. In addition, the learning laboratories’ reliance on the fellows to drive every discussion has resulted in better participation by the fellows in both the lectures and restructured didactic sessions, as well as in other components of the fellowship. These learning laboratories have also served to more fully engage each of the members of the fellowship's executive group in the educational process. The authors feel that the learning laboratories represent a simple avenue for incorporating informatics into residency education (and perhaps CME initiatives). We also believe that the learning laboratories can serve as a model for incorporating other non-sign-out driven activities into a pathology residency program.
Of note, the changes to the delivery of the core curriculum were desired, driven and instituted by the current class of fellows. While aspects of these changes reach every level of pathology professional at the AMCs in the network, their primary purpose has been to enhance the educational experiences of the fellows. Per the discussion that follows, the majority of the literature on pathology informatics education focuses on appropriate measures for residents. Though this is certainly the most pressing endeavor for education in the subspecialty, we feel that the subsequent narrative addresses salient tenets for engagement by all levels of professional in pathology informatics.
Indeed, Henricks et al. proposed an integrated, diverse pathology informatics learning environment for trainees more than a decade ago.[6] In so doing, Henricks et al. stressed adaptability, flexibility, reliance on local faculty and the use of “core knowledge and competency bases”. Rinder and Smith further underscored the importance of such an approach to education in laboratory medicine by demonstrating an array of delivery preferences among trainees at 29 residency programs.[7] Unfortunately, there are few studies that demonstrate a definite positive correlation between learning preferences and learning styles. In other words, though distinct styles exist, people are generally unaware of their own styles. Furthermore, in medical education settings, there appears to be no link between learning styles and test results.[5] Nevertheless, Rinder and Smith also emphasized the importance of teaching residents how to teach during their residencies.[7] In a like-minded review, Wamsley et al. concluded that “there is evidence that teaching courses improve resident self-assessed teaching behaviors, self-confidence as a teacher, and result in higher learner evaluations”.[8]
To that end, Park et al. recently described an endeavor for delivering genomics, research and informatics principles to pathology trainees via an annual two-week course that covers an array of sub-disciplines within each field in a variety of formats and with the assistance of contributions to and interactions with a wiki software construction.[9] By employing pre- and post-course evaluations, Park et al. were able to show a significant benefit from this course in the subset of their trainees that employed wiki software in their approach to the course. While an evaluation method is ideal, the pathology residents at the AMCs in our network previously had no formal exposure to informatics, so any educational experience will suffice to start. Likewise, the two-week course Park et al. described is quite commendable in both its length and status as a protected activity. Unfortunately, scheduling constraints within each AMC's residency program prohibit such commitments, leaving our significantly shorter approach of interspersed, one- and two-hour sessions the only viable option.
The work of Park et al. can be thought of as an evolution of the three-week program originally reported by Harrison and Stewart in 2003.[10] Like the newly diversified approach to our core curriculum, this predecessor featured an array of educational approaches, including lectures, laboratory sessions, field trips and demonstrations, as well as a core reading list. Unlike our approach, Harrison and Stewart's featured much more in the way of IT principles and, to reiterate, was geared toward residency training. Furthermore, the potential of wiki software in pathology informatics education was first described in 2010 by Kim et al., who deployed a wiki that mines entries from Wikipedia. Through the employment of indices of recent activity, Kim et al. were able to demonstrate the overarching principle of pathology informatics education – that it is a “moving target”.[11]
Kang et al. have characterized a series of on-line modules as another viable option for incorporating pathology informatics into a training program.[12] Their study demonstrated, again via pre- and post-module evaluations, an improvement in trainees’ collective understanding of pathology informatics principles. Of note, the studies of Kang et al. and Park et al. took place at the same AMC, with the former pre-dating the latter by approximately three years. This point further stresses the importance of and necessity for evolution and flexibility in pathology informatics education.
Neither the new approach to the core curriculum nor its predecessor has any indices by which to measure fellow performance. This lack of statistical pre- and post-comparisons represents a weakness from the standpoint of proving merit to pathology residency programs, which are all facing the challenge of ensuring adequate competency among trainees amid an ever-expanding array of disciplines. Though the intent of this technical note is to make pathology educators aware of additional teaching tools and not necessarily establish them as standards, we do recommend that any residency program that may adopt these or similar measures considers complementing them with long-term performance assessments - be they examinations, exit interviews, surveys, etc.
Additional potential concerns are the novelty of the restructured delivery process itself and the limited audience to which it has been offered thus far. As previously alluded to, the next class of fellows may institute another approach or perhaps revert the delivery of the core curriculum to its original format, rendering the current delivery model obsolete. Likewise, when the new approach is offered to the broader pathology community within the health care network (or beyond), it may not be well-received. While either fate might argue against the efficacy or sensibility of the redesign or suggest an element of impermanence to the curriculum itself, it is again worth noting that two main goals of this exercise have been to explore new educational possibilities in a pilot setting and raise awareness throughout the pathology informatics community about potential educational opportunities. To reiterate, the changes we describe reflect a work in progress, which will and must evolve with the passage of time. An additional point of emphasis is that the content of the core curriculum is largely unchanged under the new delivery model and thus remains the standard for educational endeavors within the fellowship. Furthermore, to reiterate, we designed the core curriculum to be flexible and to adapt to changes in both its content and the methods needed to communicate its content.
Finally, though having many pathology faculty members in one health care network committed to informatics is a blessing in so many respects, allowing these individuals, many of whom do not have regular contact with the fellowship, to participate in the delivery of the core curriculum does present a challenge with respect to ensuring that all aspects of the core curriculum are covered in a consistent and education-rich manner. As discussed previously, the program director and fellow overseeing the lecture series are constantly monitoring this undertaking and providing feedback to each faculty participant.
CONCLUSIONS
Commensurate with our principle objective, we have presented a redesign to the delivery, but not the content of the core curriculum of a clinical fellowship in pathology informatics. This approach has accomplished the ends of appealing to fellows’ requests for a more diverse educational experience, relieving the program director of the significant majority of teaching responsibilities and increasing exposure of the fellows to the informatics faculty. This undertaking has also highlighted that all components of the fellowship will likely need constant and ongoing reconsideration and reconfiguration - tasks to which the fellowship itself appears well-suited in both its flexible design and forward-looking mission. As with all changes the fellowship has experienced, the major driver will forever need to be the continued participation of its fellows, who are best positioned to understand the dynamic between education and service commitments. To that end, the authors encourage all pathology educators and informaticians to consider implementing and evaluating the above educational activities in their own practices and training programs, and to continue to develop new ways to bring our growing field to the attention of the greater pathology and medical communities.
ACKNOWLEDGMENTS
The authors would like to thank Partners HealthCare for allowing for and creating a flexible educational environment.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2014/5/1/22/137717
REFERENCES
- 1.Gilbertson JR, McClintock DS, Lee RE, Onozato M, Kuo FC, Beckwith BA, et al. Clinical fellowship training in pathology informatics: A program description. J Pathol Inform. 2012;3:11. doi: 10.4103/2153-3539.93893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McClintock DS, Levy BP, Lane WJ, Lee RE, Baron JM, Klepeis VE, et al. A core curriculum for clinical fellowship training in pathology informatics. J Pathol Inform. 2012;3:31. doi: 10.4103/2153-3539.100364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levy BP, McClintock DS, Lee RE, Lane WJ, Klepeis VE, Baron JM, et al. Different tracks for pathology informatics fellowship training: Experiences of and input from trainees in a large multisite fellowship program. J Pathol Inform. 2012;3:30. doi: 10.4103/2153-3539.100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee RE, McClintock DS, Balis UJ, Baron JM, Becich MJ, Beckwith BA, et al. Pathology informatics fellowship retreats: The use of interactive scenarios and case studies as pathology informatics teaching tools. J Pathol Inform. 2012;3:41. doi: 10.4103/2153-3539.103995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romanelli F, Bird E, Ryan M. Learning styles: A review of theory, application, and best practices. Am J Pharm Educ. 2009;73:9. doi: 10.5688/aj730109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henricks WH, Boyer PJ, Harrison JH, Tuthill JM, Healy JC. Informatics training in pathology residency programs: Proposed learning objectives and skill sets for the new millennium. Arch Pathol Lab Med. 2003;127:1009–18. doi: 10.5858/2003-127-1009-ITIPRP. [DOI] [PubMed] [Google Scholar]
- 7.Rinder HM, Smith BR. Innovative methods in laboratory medicine resident teaching. Clin Lab Med. 2007;27:255–67. doi: 10.1016/j.cll.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Wamsley MA, Julian KA, Wipf JE. A literature review of “resident-as-teacher” curricula: Do teaching courses make a difference? J Gen Intern Med. 2004;19:574–81. doi: 10.1111/j.1525-1497.2004.30116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park S, Parwani A, Macpherson T, Pantanowitz L. Use of a wiki as an interactive teaching tool in pathology residency education: Experience with a genomics, research, and informatics in pathology course. J Pathol Inform. 2012;3:32. doi: 10.4103/2153-3539.100366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison JH, Jr, Stewart J., 3rd Training in pathology informatics: Implementation at the University of Pittsburgh. Arch Pathol Lab Med. 2003;127:1019–25. doi: 10.5858/2003-127-1019-TIPIIA. [DOI] [PubMed] [Google Scholar]
- 11.Kim JY, Gudewicz TM, Dighe AS, Gilbertson JR. The pathology informatics curriculum wiki: Harnessing the power of user-generated content. J Pathol Inform. 2010;1:10. doi: 10.4103/2153-3539.65428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang HP, Hagenkord JM, Monzon FA, Parwani AV. Residency training in pathology informatics: A virtual rotation solution. Am J Clin Pathol. 2009;132:404–8. doi: 10.1309/AJCP6YXB6ODKTDQI. [DOI] [PubMed] [Google Scholar]


