Abstract
Objective:
The aim of the following study is to determine the effect of primary closure or dressing on post-operative morbidity after impacted lower third molar surgery.
Materials and Methods:
This was a randomized clinical study of 72 patients who had surgical extraction of impacted mandibular third molars. The subjects were divided into two groups of A and B. Group A had total closure (primary closure) and Group B had whitehead varnish dressing of the socket. Pain, swelling and trismus were evaluated pre-operatively using visual analogue scale, flexible tape measuring method and inter-incisal distance measurement with Vernier Callipers respectively as well as post-operatively on 1st, 2nd, 3rd, 5th and 7th day.
Results:
The study participants consisted of 27 males and 45 females in a ratio 1:1.7. With a mean age of 24.7 ± 4.9 years (range 19-33 years) for Group A and 25.5 ± 4.3 years (range 20-39 years) for Group B. Post-operative pain was not significantly affected by the closure techniques (P > 0.05). Dressing was found to significantly reduce the degree of swelling and trismus peaking on the 2nd day (P = 0.0207 and P = 0.010 respectively).
Conclusion:
The use of dressing was more effective than primary closure to reduce the degree of swelling and trismus though its effect on post-operative pain reduction was not significant.
KEYWORDS: Dressing, primary closure, randomized, surgery, third molars
INTRODUCTION
Impacted third molars are developmental pathological medical deformities characteristic of modern civilization accounting for 98% of all impacted teeth.[1]
Studies have shown that there is significant deterioration in oral health related quality of life such as trismus, swelling,[2] pain and delayed healing of extraction socket[3,4] in the immediate post-operative periods following third molar surgery. Economically, much fund is being spent on analgesics and antibiotics to reduce the post-operative morbidity associated with lower third molar surgery.[5]
Few studies have been devoted to the influence of operative techniques on the post-operative course. One of the factors most linked to the intensity of pain and swelling is the technique of closure of the socket after surgical extraction of impacted mandibular third molar.[6] Two types of closure techniques namely the primary (total) and secondary (partial) closure techniques have been studied.[7,8,9,10] Primary closure technique is the complete closure of extraction socket by way of repositioning of the flaps by sutures aimed at wound healing by primary intention.[8] Primary closure is derived from the basic surgical principle and is still widely practiced in Nigeria.[9] Osunde et al.,[10] in their study have reported that primary closure of the wound prevents drainage of the latter, worsening the post-operative pain and swelling. However, other authors report that with this technique, complete wound healing is achieved and contamination from the oral cavity is avoided.[11] Secondary closure technique involves healing of the socket by secondary intention.
Some of the secondary closure techniques explored in the literature range from the use of drains, single sutures to sutureless techniques. Drains commonly used in oral and maxillofacial surgery are the gauze drains, suction drains and simple rubber drains. Akota et al.,[2] evaluating the effect of locally applied gauze drain impregnated with chlortetracycline ointment in mandibular third molar surgery concluded that there was a reduction in post-operative alveolitis but had no beneficial effect on pain, swelling and trismus. This finding was supported by de Brabander and Cattaneo[12] following use of gauze drain partially submerged into the socket. However, other investigators[13,14,15] using Penrose drains or small tube drains concluded that there was a significant reduction in swelling and trimus though pain reduction was minimal. The use of drains have been associated with complications such as tissue reaction to drain materials, irritation and erosion of adjacent structures, creation of dead space about the drain itself and potentiation of infection in clean wounds.[16]
The use of single suture and sutureless techniques to achieve secondary closure following third molar surgery have been reported.[10,17] These emerging techniques have the advantages of reducing the operative time and less tissue manipulation. Pain, swelling and trismus are reported to be significantly reduced within the first 48 h of surgery. However, sutureless technique might only be limited to cases in which minimal incisions are used for third molar surgery.[18]
The creation of a “window” by way of mucosa excision as advocated by Dubois et al.,[8] raises questions as to the rationale for sacrificing normal tissue. Studies by Rakprasitkul and Pairuchvej,[14] have reported that the duration of surgery is 4 min longer for secondary closure technique compared with primary closure. This increase in length of surgical intervention has been found to lead to increase pain, swelling and trismus following lower third molar surgery. Thus, there is the need for a secondary closure technique that may ameliorate these observed setbacks.
This study is aimed at comparing the effect of primary closure or dressing on post-operative morbidity after lower third molar surgery. It is hoped that the outcome of this study would provide the oral and maxillofacial surgeon a better alternative to ameliorate post-operative morbidity sequel to third molar surgery as well as improving patient's quality of life and disposition to surgery.
MATERIALS AND METHODS
This study was a prospective randomized clinical trial with subjects drawn from consecutive patients attending the Oral and Maxillofacial Surgery Department of the University of Benin Teaching Hospital, Benin, Edo State, Nigeria for impacted mandibular third molar surgery. All patients (18-45 years) who met the National Institute of Health criteria (NIH, 1980) were recruited. Those patients with missing central incisors in either of the jaws were however excluded in order to standardized measurement of maximum inter-incisal distance during opening.
Permission to conduct this study was sought from the Ethics Committee of the Hospital, while written informed consent from the individual patient to participate in the study was also obtained.
The study population was randomly divided into two equal groups - Group A had primary closure only while Group B had Whitehead's Varnish dressing in the socket. A study population of 80 cases based on calculated sample size was drawn into a pool of 80 cards. The 80 cards were divided into two equal groups of 40 cards - 40 cards Group A and 40 cards Group B. To match for gender, 45 females and 35 males were recruited and the first patient in each gender group was made to ballot which type of closure technique would be instituted through the toss of a coin. Subsequent patient of each gender group alternated the closure technique. Patient's maximum mouth opening from the maxillary central mesioincisal edge to the mandibular central mesioincisal edge was measured in centimeters using vernier callipers as described by Ustun et al.[19] Two readings were taken and the average was calculated. All patients had pre-operative facial measurements. The flexible tape measuring method designed by Neupert et al. and reported by Weupert et al.,[20] and Chukwuneke et al.,[21] was used [Figure 1]. This was done by taking the sum of measurements between three standard points. The first measurement was taken from the tragus to the pogonium and the second measurement was taken from the tragus to the labio-angular commissure. This was done twice and the mean calculated value was used. Pain score was measured using a visual analogue scale.
Figure 1.
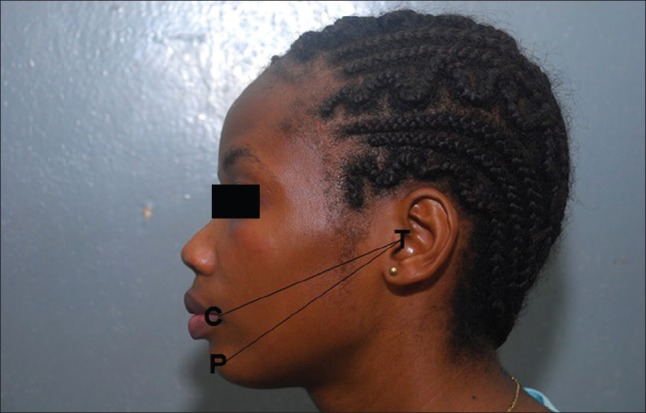
Measurement of facial width. T - tragus, C - commisure, P - pogonium
All the surgical procedures were performed by the same surgeon using the guttering technique. A local anesthetic agent (2% lidocaine with 1:100,000 adrenalin) was administered to all patients using a dental syringe and a 3.5 cm long 27 gauge dental needle through an intraoral approach. A full thickness three sided buccal mucoperiosteal flap was made and reflected with an anterior relieving incision running from the buccal sulcus to the midpoint of the first or second molar depending on the nature of impaction and continued through the gingival sulcus of the second molar. The posterior incision was made distally and laterally over the external oblique ridge in the retromolar ascending ramus area. Bone was removed using a round bur (carbide no: 8) in a high speed straight hand piece under constant irrigation with sterile normal saline solution. The delivery of the tooth was carried out with tooth division done where indicated.
In line with predetermined closure techniques for each patient those requiring dressing had the distal incision over the patient's oblique ridge sutured and a small Whitehead varnish (Medex UK-East-Anglia) dressing was also sutured to the apex of the flap. The dressing was inserted into the socket. For patients indicated for primary closure, the anterior and distal relieving incisions were sutured using 3/0 silk to ensure total closure of socket. The duration of the procedure was recorded from the time of first incision to the placement of the last suture by an assistant using a stopwatch on the instruction of the operating surgeon.
All patients were administered prophylactically, 500 mg amoxicillin and 200 mg metronidazole 8 hourly per oral for 5 days except in two patients that had a history of allergy to penicillins who had to be given 250 mg erythromycin 6 hourly. Diclofenac potassium (50 mg twice daily) was administered orally as the analgesic for 5 days. Post extraction instructions were given and all patients were given an appointment to report in the clinic on the 1st, 2nd, 3rd, 5th and 7th day for evaluation of post-operative morbidity.
Evaluation of facial swelling and mouth opening was done by a colleague who had been trained on assessment techniques and was oblivious of the type of closure technique employed for each patient. Post-operative measurements of facial swelling and mouth opening on the 1st, 2nd, 3rd, 5th and 7th day for all patients was carried out. The pre-operative value was subtracted from the post-operative values to ascertain the degree of change if any. Post-operative pain assessment was determined by patients using the visual analogue scale[22] (a 10 cm baseline scale where 0 cm was no pain and 10 cm was worst possible pain) on the 1st, 2nd, 3rd, 5th and 7th day post-operatively. This reading was taken at 7 am on the specified days.
The data that was recorded in the proforma designed for the study was analyzed using the Statistical Package for Social Sciences (SPSS, version 17; SPSS, Chicago). Results were analyzed using Student's t-test and significance level was set at P < 0.05 and adopted power of 95%.
RESULTS
A total of 80 patients participated in the study. There were however 8 dropouts (5 from Group A and 3 from Group B) due to failure to keep an appointment. Thus, 72 subjects were analyzed. The study with a mean age of 25.1 ± 4.6 years (range 19-39 years). The mean duration of surgery for primary closure was 30.5 min (range, 20-36 min) and for dressing, it was 32.1 min (range 28-40 min).
Pain assessment
The difference in mean pain score was not statistically significant (P = day 1 0.061; day 2 0.082; day 3 0.086; day 4 0.082; day 5 0.796) between the study groups. However, the mean pain scores for patients in group B (Dressing) was consistently lower than those in group A (Primary closure) for the corresponding days of post-operative pain evaluation [Figure 2].
Figure 2.
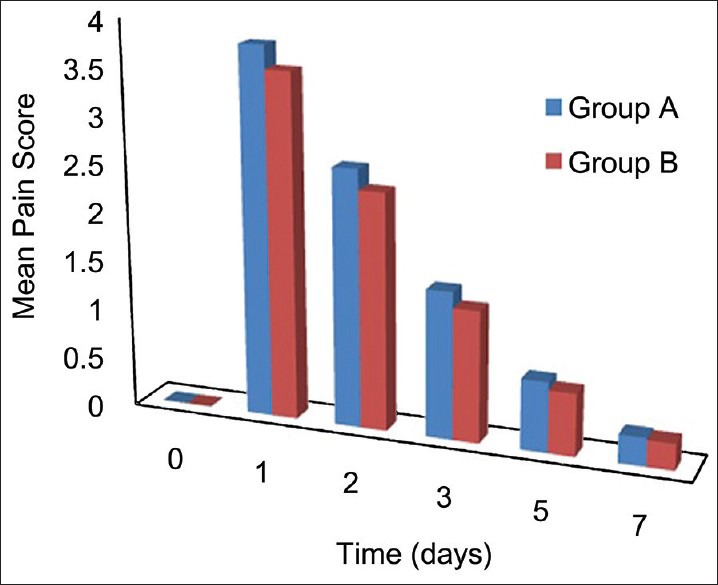
Post-operative pain according to time-point and technique employed
Facial swelling
Table 1 shows that the mean facial swelling between the two groups measuring the Tragus-commissure (TC) distance was statistically significant for the 1st and 2nd day post-operatively (P = 0.010 and 0.010 respectively). Similarly, Tragus-pogonium (TP) mean measurements were significant only on the 2nd day. This was similar to the combined measurements of TC + TP which were also statistically significant on the 2nd day (P = 0.020). The mean facial swelling was less in patients that had secondary closure compared to those with primary closure in the three degrees of measurements. There was also an observed decrease in mean facial swelling to pre-operative values during the course of post-operative evaluation [Figure 3].
Table 1.
Comparison of primary closure (Group A) or dressing (Group B) on post-operative swelling after third molar surgery

Figure 3.
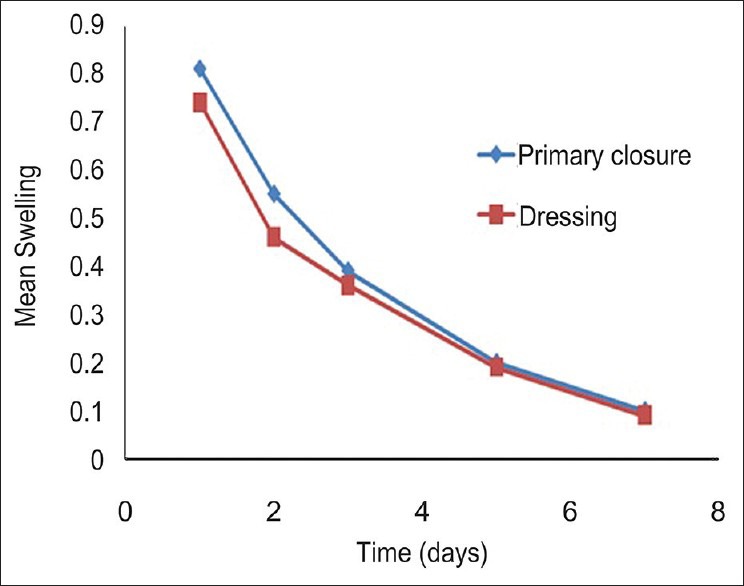
Post-operative swelling according to time-point and technique used
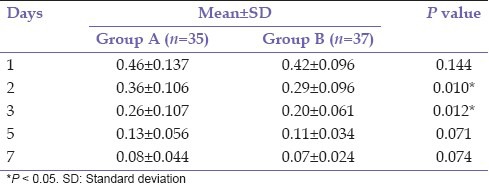
Trismus
Table 2 shows a higher mean reduction in mouth opening for patients who had primary closure (Group A) compared with those who had dressing (Group B). The differences in the mean reductions were statistically significant on the second and third post-operative days (P = 0.010 and 0.012 respectively).
Table 2.
Comparison of primary closure (Group A) or dressing (Group B) on post-operative trismus after third molar surgery
DISCUSSION
Surgery of impacted third molars can lead to immediate post-operative pain and discomfort.[23] Various researches have been carried out especially in the developed countries to finding ways of ameliorating these morbidities to their barest minimum.[17,24] One of the measures used was comparing the efficacy of primary and secondary closure post-operatively. Most studies[2,7,11,25] are of the opinion that post-operative sequelae were less with secondary closure while others[12,26] claim there is no statistical difference to advocate one over the other.
Mean pain score as assessed using the visual analogue scale showed that the pain score for each day of the evaluation was higher in those who had primary closure. This agrees with the findings by Holland and Hindle[27] and Pasqualini et al.[6] However, it was noteworthy that the difference in pain score observed was not statistically significant between the study populations. This agrees with the findings of Chukwuneke et al.[15] and Chaudhary et al.[28] who found no significant difference between primary and secondary closure techniques with respect to pain.
In evaluating the closure techniques on post-operative swelling, the use of secondary closure technique had a statistical differential between the techniques in the post-operative measures of tragus to commissure on the 1st and 2nd day, tragus to pogonium on the 2nd day and on the summation of the two measurements on the 2nd day. These outcomes were similar to those of Dubois et al.,[8] who reported greater swelling when surgical wound healed by first intention. Maximum facial swelling is presumed to occur at 48 h post-operatively. The findings of statistical difference on the 2nd day of evaluation could be attributed to prevention of drainage of the wound by primary closure leading to worsening of post-operative pain and swelling as suggested by Flynn et al.[16] However, de Brabandar and Caltaneo[12] reported no differences between the two groups of patients subjected to both closure techniques.
There was a significant reduction in limitation of mouth opening in the cohort that had secondary closure. This is consistent with those of previous studies.[12,29] The findings of this study showed that the degree of post-operative reduction in trismus is associated with reduction in post-operative swelling for patients who had dressing. This observed reduction in trismus following the use of dressing has been attributable to the reduction in post-operative edema as supported by studies by Carrillo et al.[30]
Alling et al.,[31] reviewing the role of intra-alveolar dressing on post-operative morbidity following third molar surgery reported that its primary function is to preserve vital coagulum within the socket and thus prevent infection. The authors reported that dressing also acts as a space-occupying agent which is gradually displaced or absorbed as the coagulum vitalizes. The space-occupying effect places less demand on the coagulum to be vitalized throughout its entire extent. The authors observed a marked reduction in post-operative inflammatory complications such as pain and swelling though the reason for this was not known.
CONCLUSION
We observed a significant reduction in post-operative swelling and trismus in subjects that had dressing of the sockets compared with those with primary closure. Though the effect on pain reduction was better with dressing of the socket, it was not statistically significant. Furthermore, in the light of the observed drawbacks in other techniques of secondary closure, dressing provides a simple cost-effective means of improving patient's quality-of-life following third molar surgery.
ACKNOWLEDGMENT
We want to thank the nursing staff of the department as well as the Mr. Waka for assisting with the statistics.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Worrall SF, Riden K, Haskell R, Corrigan AM. UK National third molar project: The initial report. Br J Oral Maxillofac Surg. 1998;36:14–8. doi: 10.1016/s0266-4356(98)90740-9. [DOI] [PubMed] [Google Scholar]
- 2.Akota I, Alvsaker B, Bjørnland T. The effect of locally applied gauze drain impregnated with chlortetracycline ointment in mandibular third-molar surgery. Acta Odontol Scand. 1998;56:25–9. doi: 10.1080/000163598423027. [DOI] [PubMed] [Google Scholar]
- 3.Saheeb BD, Obuekwe ON. An audit of mandibular third molar surgery. Niger J Surg Res. 2001;3:66–74. [Google Scholar]
- 4.Oginni FO, Ugboko VI, Assam E, Ogunbodede EO. Postoperative complaints following impacted mandibular third molar surgery in Ile-Ife, Nigeria. SADJ. 2002;57:264–8. [PubMed] [Google Scholar]
- 5.Brickley MR, Shepherd JP. An investigation of the rationality of lower third molar removal, based on USA National Institutes of Health criteria. Br Dent J. 1996;180:249–54. doi: 10.1038/sj.bdj.4809044. [DOI] [PubMed] [Google Scholar]
- 6.Pasqualini D, Cocero N, Castella A, Mela L, Bracco P. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: A comparative study. Int J Oral Maxillofac Surg. 2005;34:52–7. doi: 10.1016/j.ijom.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 7.MacGregor AJ, Hart P. Effect of bacteria and other factors on pain and swelling after removal of ectopic mandibular third molars. J Oral Surg. 1969;27:174–9. [PubMed] [Google Scholar]
- 8.Dubois DD, Pizer ME, Chinnis RJ. Comparison of primary and secondary closure techniques after removal of impacted mandibular third molars. J Oral Maxillofac Surg. 1982;40:631–4. doi: 10.1016/0278-2391(82)90111-2. [DOI] [PubMed] [Google Scholar]
- 9.Owotade FJ, Ugboko VI, Fatusi OA, Akinmoladun VI, Obuekwe ON, Olasoji HO. Management of impacted third molars among Nigerian dentists. Odontostomatol Trop. 2002;25:27–32. [PubMed] [Google Scholar]
- 10.Osunde OD, Saheeb BD, Adebola RA. Comparative study of effect of single and multiple suture techniques on inflammatory complications after third molar surgery. J Oral Maxillofac Surg. 2011;69:971–6. doi: 10.1016/j.joms.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 11.Sanchis Bielsa JM, Hernández-Bazán S, Peñarrocha Diago M. Flap repositioning versus conventional suturing in third molar surgery. Med Oral Patol Oral Cir Bucal. 2008;13:E138–42. [PubMed] [Google Scholar]
- 12.de Brabander EC, Cattaneo G. The effect of surgical drain together with a secondary closure technique on postoperative trismus, swelling and pain after mandibular third molar surgery. Int J Oral Maxillofac Surg. 1988;17:119–21. doi: 10.1016/s0901-5027(88)80164-4. [DOI] [PubMed] [Google Scholar]
- 13.Ayad W, Jöhren P, Dieckmann J. Results of a comparative prospective randomized study of surgical removal of mandibular wisdom teeth with and without rubber drainage. Fortschr Kiefer Gesichtschir. 1995;40:134–6. [PubMed] [Google Scholar]
- 14.Rakprasitkul S, Pairuchvej V. Mandibular third molar surgery with primary closure and tube drain. Int J Oral Maxillofac Surg. 1997;26:187–90. doi: 10.1016/s0901-5027(97)80817-x. [DOI] [PubMed] [Google Scholar]
- 15.Chukwuneke FN, Oji C, Saheeb DB. A comparative study of the effect of using a rubber drain on postoperative discomfort following lower third molar surgery. Int J Oral Maxillofac Surg. 2008;37:341–4. doi: 10.1016/j.ijom.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 16.Flynn TR, Hoekstra CW, Lawrence FR. The use of drains in oral and maxillofacial surgery: A review and a new approach. J Oral Maxillofac Surg. 1983;41:508–11. doi: 10.1016/0278-2391(83)90241-0. [DOI] [PubMed] [Google Scholar]
- 17.Osunde OD, Adebola RA, Saheeb BD. A comparative study of the effect of suture-less and multiple suture techniques on inflammatory complications following third molar surgery. Int J Oral Maxillofac Surg. 2012;41:1275–9. doi: 10.1016/j.ijom.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Waite PD, Cherala S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. J Oral Maxillofac Surg. 2006;64:669–73. doi: 10.1016/j.joms.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Ustun Y, Erdogan O, Esen E, Karsli ED. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:535–9. doi: 10.1016/S1079210403004645. [DOI] [PubMed] [Google Scholar]
- 20.Weupert EA, Lee JW, Philput CB, Gordon JR. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992;50:1177–82. doi: 10.1016/0278-2391(92)90149-t. [DOI] [PubMed] [Google Scholar]
- 21.Chukwuneke FN, Saheeb BD. The effect of patient age and length of surgical intervention on postoperative morbidity following lower third molar surgery. J Maxillofac Oral Surg. 2008;7:420–3. [Google Scholar]
- 22.Langley GB, Sheppeard H. The visual analogue scale: Its use in pain measurement. Rheumatol Int. 1985;5:145–148. doi: 10.1007/BF00541514. [DOI] [PubMed] [Google Scholar]
- 23.Falconer DT, Roberts EE. Report of an audit into third molar exodontia. Br J Oral Maxillofac Surg. 1992;30:183–5. doi: 10.1016/0266-4356(92)90154-b. [DOI] [PubMed] [Google Scholar]
- 24.Sanchis-Bielsa JM, Hernández-Bazán S, Peñarrocha-Diago M. Flap repositioning versus conventional suturing in third molar surgery. Med Oral Patol Oral Cir Bucal. 2008;13:E138–42. [PubMed] [Google Scholar]
- 25.Hellem S, Nordenram A. Prevention of postoperative symptoms by general antibiotic treatment and local bandage in removal of mandibular third molars. Int J Oral Surg. 1973;2:273–8. doi: 10.1016/s0300-9785(73)80022-5. [DOI] [PubMed] [Google Scholar]
- 26.Suddhasthira P, Chinwat S, Sattapongsda P. The comparison study of primary and secondary closure technique after removal of impacted mandibular third molars. Thai J Oral Maxillofac Surg. 1991;5:67–77. [Google Scholar]
- 27.Holland CS, Hindle MO. The influence of closure or dressing of third molar sockets on post-operative swelling and pain. Br J Oral Maxillofac Surg. 1984;22:65–71. doi: 10.1016/0266-4356(84)90011-1. [DOI] [PubMed] [Google Scholar]
- 28.Chaudhary M, Singh M, Singh S, Singh SP, Kaur G. Primary and secondary closure technique following removal of impacted mandibular third molars: A comparative study. Natl J Maxillofac Surg. 2012;3:10–4. doi: 10.4103/0975-5950.102141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sağlam AA. Effects of tube drain with primary closure technique on postoperative trismus and swelling after removal of fully impacted mandibular third molars. Quintessence Int. 2003;34:143–7. [PubMed] [Google Scholar]
- 30.Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J. 1990;40:31–6. [PubMed] [Google Scholar]
- 31.Alling CC, Helfrick JF, Alling RD. 1st ed. Pennsylvania, the Curtis Center Independence Square: W.B. Saunders; 1993. Impacted Teeth; p. 177. [Google Scholar]


