Abstract
Objectives:
The aim of this study is to evaluate the success rate and complications of mandibular reconstruction with nonvascularized bone graft in Ile-Ife, Nigeria.
Patients and Methods:
A total of 25 patients who underwent reconstruction of mandibular discontinuity defects between January 2003 and February 2012, at the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife constituted the study sample. Relevant information was retrieved from the patients’ records. This information include patients’ demographics (age and sex) as well as the type of mandibular defect, cause of the defect, type of mandibular resection done, source of the bone graft used, and the method of graft immobilization. Morbidity associated with the graft procedures were assessed by retrieving information on graft failures, length of hospital stay following surgery, rehabilitation device used and associated graft donor and recipient site complications.
Result:
There were 12 males and 13 females with a male:female ratio was 1:1.1. The age of the patients ranged from 13 to 73 years with a mean age for males 32.7 ± standard deviation (SD) 12.9 and for females 35.0 ± SD 17.1. Jaw defect was caused by resection for tumours and other jaw pathologies in 92% of cases. Complete symphyseal involvement defect was the most common defect recorded 11 (44%). Reconstruction with nonvascularized rib graft accounted for 68% of cases while iliac crest graft was used in 32% of the patients. Successful take of the grafts was recorded in 22 patients while three cases failed. Wound dehiscence (two patients) and postoperative wound infection (eight patients) were the most common complications recorded.
Conclusion:
The use of nonvascularized graft is still relevant in the reconstruction of large mandibular defects caused by surgical ablation of benign conditions in Nigerians. Precise surgical planning and execution, extended antibiotic therapy, and meticulous postoperative care contributed to the good outcome.
KEYWORDS: Mandibular defect, mandibular reconstruction, nonvascularized bone graft
INTRODUCTION
Mandibular reconstruction principles and techniques have evolved steadily over the last century. Free nonvascularized autogenous bone grafting was the main standard of care for mandibular reconstruction in the past until the advent of microvascular surgery in the early 1970s.[1,2,3,4] Today, this traditional technique for the reconstruction of the mandible is indicated mainly to bridge segmental defects of the mandible where adjuvant radiotherapy is not indicated after ablative surgery as well as the reconstruction of the condyle, wide palatal clefts and in preprosthetic surgery.[5,6,7]
Defects of the mandible may result from treatment of benign and malignant tumours, congenital abnormalities, trauma, infections, and osteoradionecrosis. The ideal goal of reconstruction is to achieve sufficient anatomical bulk (height and width) of the mandible that will accommodate implant insertion and adequate muscle attachments to allow for normal form and function, preservation of the inferior alveolar nerve and subsequent restoration of sensation.[5] Restoration of the form (esthetics) and function (mastication, deglutition, and saliva control) have been achieved by the use of autogenous grafts harvested from the iliac crest, rib, radius, fibula, tibia, scapula, and calvarium.[5] The choice of a particular donor site for grafts depends on the type and extent of hard tissue defect, rehabilitation expectation of the patient, condition of the recipient bed, surgical capability, availability of equipment, and expertise of the surgeon.[8] At present, many surgeons will opt for a cortico-cancellous block graft from the iliac crest for the reconstruction of mandibular defects. It provides a good contour with excellent bulk and height necessary for osseointegrated implant rehabilitation.[5] Tie et al.[9] investigated the biomechanical effect of human mandibular reconstruction with autogenous bone graft and concluded that the stress distribution following iliac crest graft was similar to that of the normal mandible. Costochondral graft is mainly indicated in the reconstruction of temporomandibular joint and appears to be the most popular and widely used graft for this purpose.[5,7,10,11]
The limitations of a nonvascularized graft lies in the fact that it is avascular, which makes it susceptible to infection and increases the chances of failure with increasing length of the defect.[12] Pogrel et al.[8] in their study have reported a 17% failure for 6 cm defect and 75% for 12 cm defect or more for nonvascularized graft. They recommended the use of vascularized bone grafts for mandibular replacements over 9 cm in length. Furthermore, pre- and post-operative radiotherapy, simultaneous reconstruction of soft- and hard-tissue defects and the need for primary implant rehabilitation have largely limited the use of nonvascularized grafts in oromandibular reconstruction. Osteocutaneous free flaps can now be used in these situations with about 95% success rates or more.[8,13,14] Other available and recent developments in oromandibular reconstruction include the use of transport disc distraction osteogenesis and genetically engineered bone.
Apart from the pioneering work of Adekeye[15] in 1978, very few reports[16,17] on mandibular reconstruction have emanated from Nigeria. Perhaps, the high cost of this type of surgery in a resource scares economy coupled with limited available expertise have contributed largely to this paucity of information.[17,18] This study therefore aimed at highlighting the outcomes of mandibular reconstruction with nonvascularized bone graft in Ile-Ife, Nigeria.
PATIENTS AND METHODS
During the period of the months between January 2003 and February 2012, 25 patients underwent reconstruction of mandibular discontinuity defects at the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife. For this study, relevant information was retrieved from patients’ records. This information include patients’ demographics (age, sex) as well as information about the cause of mandibular defect, type of defect, extent of mandibular resection done, the bone graft used, and method of graft immobilization. Mandibular defect was classified according to a modified Urken's scheme suggested by van Gemert et al.[19] as follows: True lateral (condyle, ramus, body, ramus-body), hemisymphyseal (Sh) and complete symphyseal [Table 1 and Figure 1].
Table 1.
Type of mandibular defect
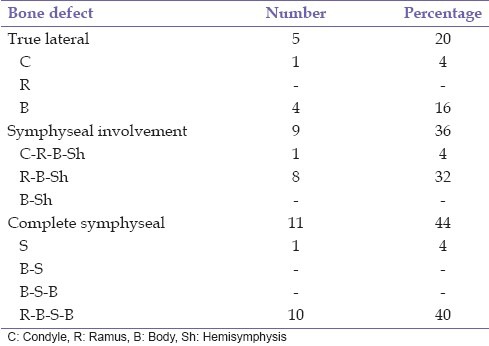
Figure 1.
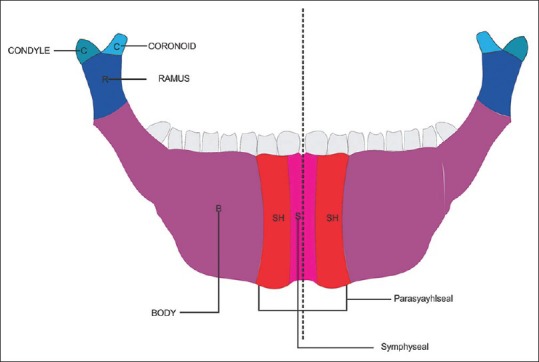
A schematic diagram of the mandible illustrating the defects described in Table 1
Morbidity associated with the graft procedures were assessed by retrieving information on graft failures, length of hospital stay following surgery, rehabilitation device used, and associated graft donor and recipient site complications.
All the patients received intravenous antibiotics for a minimum period of 10 days. Placement of maxillomandibular fixation with two or three eyelet wires or plaster of Paris head cap was done 48 h after surgery, depending on the presence or absence of teeth after tumour ablation. This was maintained for a period of 5 weeks for noninfected grafts, but retained in situ for as long as it took infection to be controlled in infected grafts.
Success of the procedure was adjudged as maintenance of bone continuity and complete consolidation, with the absence of any evidence of infection both on clinical and radiographic examinations. Failure was regarded as loss of the whole graft or part of it which necessitated another reconstructive surgery.
The reconstruction was considered functionally complete if prosthetic rehabilitation was accomplished or if there was a sufficient remaining dentition for mastication. 15 patients were followed-up for a minimum of 12 months postoperatively.
Data were analyzed using the Statistical Package for Social Sciences (SPSS Inc., IL. Chicago) version 16.0 and the results were converted to relative values in frequency tables.
RESULT
The 25 patients consisted of 12 males and 13 females with a male:female ratio of 1:1.1. The age of the patients ranged from 13to 73 years with a mean age for males 32.7 ± 12.9 and for females 35.0 ± 17.1. Jaw defect was caused by resection for tumours and other jaw pathologies in 92% of cases. Others were caused by gunshot injury (4%) and hemifacial hypoplasia (4%) [Table 2 and Figures 2 and 3].
Table 2.
Cause of mandibular defect
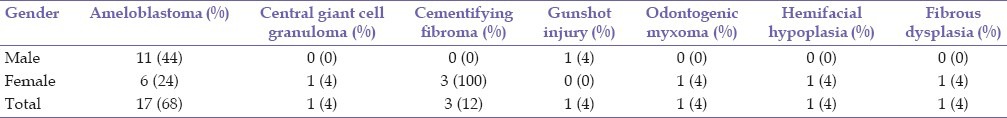
Figure 2.

A patient with mandibular central ameloblastoma. Note the jaw expansion involving the right body and angle region
Figure 3.
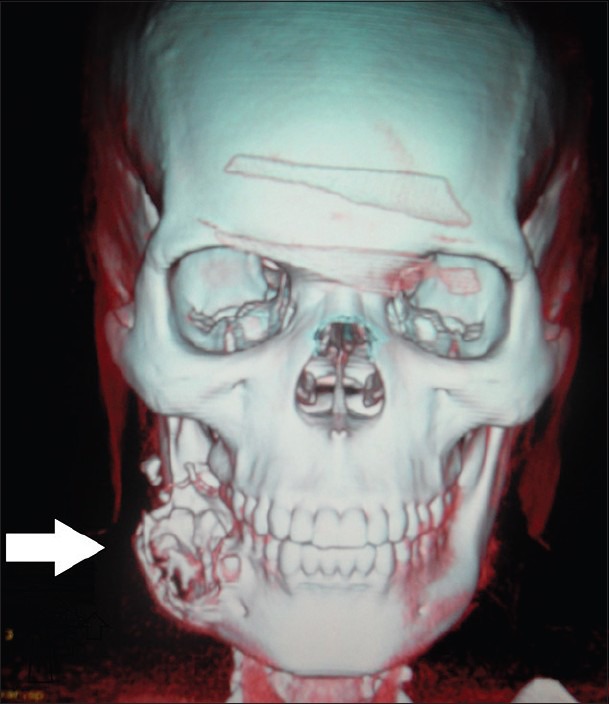
Three-dimensional computed tomography scan of mandibular ameloblastoma showing bony destruction extending from the right angle of the mandible to the first premolar region
Table 1 shows the extent of mandibular defects. True lateral defect was the least common defect 5 (20%) followed by symphyseal involvement 9 (36%). Complete symphyseal involvement was the most common defect recorded 11 (44%).
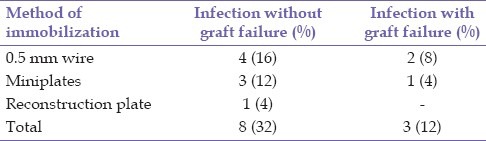
Reconstruction with nonvascularized rib graft accounted for 68% of cases, while iliac crest graft was used in 32% of the patients [Table 3]. Successful take of the grafts was recorded in 22 patients while three cases failed. All the three grafts that failed were rib grafts used for the reconstruction of a subtotal mandibular resection. Two of these grafts were immobilized with 0.5 mm soft stainless steel wires and the other graft was fixed with a 2 mm titanium mini plate. Bacterial infection was contributory to graft failure [Tables 4 and 5].
Table 3.
Type of resection and graft used
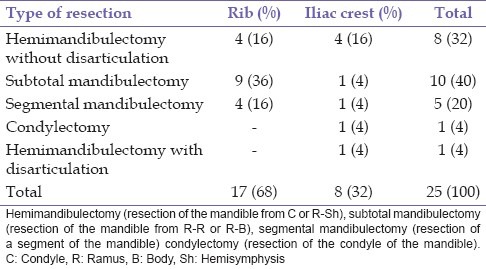
Table 4.
Type of resection and associated complications
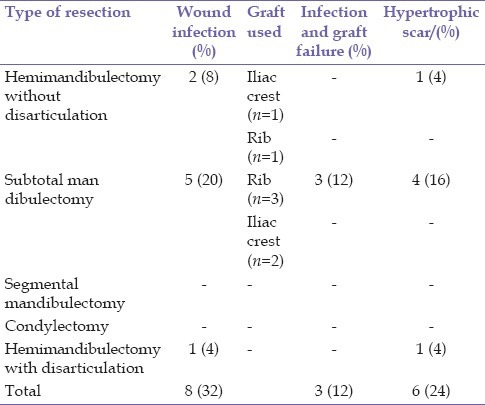
Table 5.
Method of immobilization and failure of graft
The length of hospital stay ranged from 11 to 42 days (median, n = 23.14 days). Grafts loading with acrylic denture were performed after sulcoplasty in three patients and without sulcoplasty in 12 patients while seven patients were lost to follow-up after graft take.
Complications recorded involved recipient sites only. The entire donor site wound healed uneventfully. Wound dehiscence (two patients) and postoperative wound infection (eight patients) were the most common complications recorded. Three patients (12%) who developed infection had graft failure [Tables 4 and 5]. Hypertrophic scar occurred in six patients [Figure 4] and five of these patients had postoperative wound infection.
Figure 4.

Patient with hypertrophic scar after mandibular reconstruction
DISCUSSION
The reconstruction of mandibular defects with a nonvascularized bone graft is still the mainstay of mandibular reconstruction in Nigeria.[15,16,17] Although, the use of nonvascularized graft is largely limited in the reconstruction of large defects with or without soft tissue loss or in cases where adjuvant radiotherapy is indicated, the advantages of this option in restoring good facial esthetics and function in properly selected cases have been well-documented.[8]
Jaw resection following pathological lesions has been reported as the most common cause of mandibular defects requiring reconstruction in Oral and Maxillofacial Surgery.[8,15,16,17] In this study, pathological lesions accounted for 92% of the mandibular discontinuity defects. All the pathological lesions were benign lesions. Recent reports[17,18] on oromandibular reconstruction agree that nonvascularized grafts are best suited for the reconstruction of segmental defects created after ablation of benign lesions. Although, van Gemert et al.[19] have reported a good measure of success with only 19% failure rate in the 27 irradiated patients reconstructed with nonvascularized iliac crest graft. Their patients received adjuvant pre- and post-operative hyperbaric oxygen therapy in addition to an extended postoperative intravenous antibiotic therapy for 10 days.
The overall success rate of 88% recorded in this study is in agreement with those reported in the literature where success rates have been reported to be between 46% and 100%.[8,19,20] About 76% of the continuity defects recorded in our series were long span mandibular defects created after hemimandibulectomy with or without condylectomy and subtotal mandibulectomy, n = 19. Pogrel et al.[8] observed a75% failure rate for long span defects measuring up to 12 cm or more in their study and suggested that such length of mandibular defects should be reconstructed with vascularized grafts. Their suggestion is in agreement with modern day concept on oromandibular reconstruction.[17,18] However, where conditions preclude free flap transfer (e.g. high cost of treatment, patient's medical condition, non-availability of armamentarium, and expertise) nonvascularized graft could be a viable alternative. The fact that the patients in the present study had maxillomandibular fixation for a minimum of 5 weeks, which allowed for a considerable time for bone healing and the extended intravenous antibiotic for a minimum of 10 days may have contributed to the success rate observed. Rigid fixation appeared to have aided healing too, as two out of the three cases of graft failure in the present study had wire fixation. These patients were the earlier cases managed in our centre when 0.5 mm stainless steel wires were the only materials available for graft fixation. Nonrigid fixation of the graft allows for movement which may lead to neoarthrosis or infection with subsequent loss of the graft.[19]
Wound dehiscence caused by infection was the most common recipient site complication recorded. Intraoral wound dehiscence allows saliva and fluid to seep into the graft bed which may result in infection. Eight patients (32%) developed infections in the course of treatment. This figure is in agreement with the reported figures of 20-36% infection rate in the literature;[17,19,21] however, the infection rate resulting in graft failure (12%) was lower than the rate reported in most studies.[8,17,19] Some of the reported factors that increase the chances of postoperative infections include immediate reconstruction, reconstruction in an irradiated recipient site, reconstruction via the intra-oral route.[17,19,21] The high rate of infection in our study could be explained on the basis of the fact that the patients in our study received immediate reconstruction via the intra-oral approach with intra-operative wound contamination by salivary organisms and substrates [Figure 5]. However, the extension of the antibiotic regimen may have been responsible for the effective control of majority of these infections resulting in only three graft failures.
Figure 5.
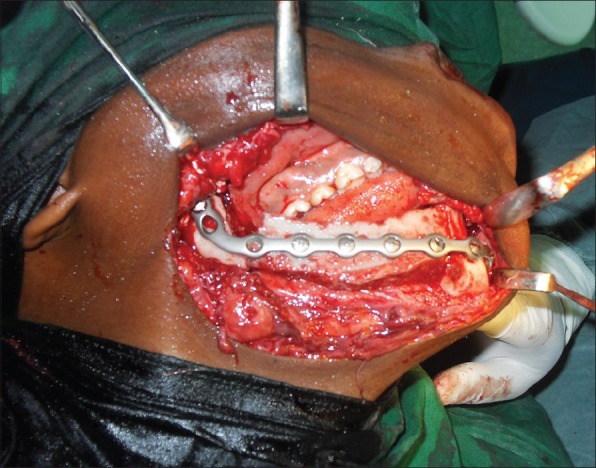
Mandibular reconstruction with autogenous iliac crest graft. Note the graft in place and immobilized with a 2.4 mm KLS Martins right angle recon plate and screws
Hypertrophic scar formation is not a commonly reported oromandibular reconstruction complication in the literature. Six patients (24%) developed hypertrophic scar in our study. Five (83%) of these had postoperative wound infection [Figures 6 and 4]. Healing by secondary intention appeared to have aided this process. Full functional rehabilitation was achieved by the placement of dentures and 3 (%) of these patients had vestibuloplasty to aid denture retention. Modern day functional rehabilitation[8,13,19] of mandibular defects is achieved by the placement of osseointegrated implants, which was rather unaffordable to our patients.
Figure 6.

Patient 3 months after mandibular reconstruction
CONCLUSION
The use of nonvascularized graft is still relevant in the reconstruction of large mandibular defects caused by surgical ablation of benign conditions in Nigerians. Precise surgical planning and execution, extended antibiotic therapy and meticulous post-operative care contributed to the high success rate.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Snyder CC, Bateman JM, Davis CW, Warden GD. Mandibulo-facial restoration with live osteocutaneous flaps. Plast Reconstr Surg. 1970;45:14–9. doi: 10.1097/00006534-197001000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Strauch B, Bloomberg AE, Lewin ML. An experimental approach to mandibular replacement: Island vascular composite rib grafts. Br J Plast Surg. 1971;24:334–41. doi: 10.1016/s0007-1226(71)80086-3. [DOI] [PubMed] [Google Scholar]
- 3.Conley J. Use of composite flaps containing bone for major repairs in the head and neck. Plast Reconstr Surg. 1972;49:522–6. doi: 10.1097/00006534-197205000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55:533–44. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Goh BT, Lee S, Tideman H, Stoelinga PJ. Mandibular reconstruction in adults: A review. Int J Oral Maxillofac Surg. 2008;37:597–605. doi: 10.1016/j.ijom.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Morrison A, Brady J. Mandibular reconstruction using nonvascularized autogenous bone grafting. Curr Opin Otolaryngol Head Neck Surg. 2010;18:227–31. doi: 10.1097/MOO.0b013e32833a46ed. [DOI] [PubMed] [Google Scholar]
- 7.Khadka A, Hu J. Autogenous grafts for condylar reconstruction in treatment of TMJ ankylosis: Current concepts and considerations for the future. Int J Oral Maxillofac Surg. 2012;41:94–102. doi: 10.1016/j.ijom.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Pogrel MA, Podlesh S, Anthony JP, Alexander J. A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J Oral Maxillofac Surg. 1997;55:1200–6. doi: 10.1016/s0278-2391(97)90165-8. [DOI] [PubMed] [Google Scholar]
- 9.Tie Y, Wang DM, Ji T, Wang CT, Zhang CP. Three-dimensional finite-element analysis investigating the biomechanical effects of human mandibular reconstruction with autogenous bone grafts. J Craniomaxillofac Surg. 2006;34:290–8. doi: 10.1016/j.jcms.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Cheung LK, Zheng LW, Ma L, Shi XJ. Transport distraction versus costochondral graft for reconstruction of temporomandibular joint ankylosis: Which is better? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:32–40. doi: 10.1016/j.tripleo.2009.02.030. [DOI] [PubMed] [Google Scholar]
- 11.Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009;67:1966–78. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 12.Vu DD, Schmidt BL. Quality of life evaluation for patients receiving vascularized versus nonvascularized bone graft reconstruction of segmental mandibular defects. J Oral Maxillofac Surg. 2008;66:1856–63. doi: 10.1016/j.joms.2008.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Mehta RP, Deschler DG. Mandibular reconstruction in 2004: An analysis of different techniques. Curr Opin Otolaryngol Head Neck Surg. 2004;12:288–93. doi: 10.1097/01.moo.0000131444.50445.9d. [DOI] [PubMed] [Google Scholar]
- 14.Anthony JP, Foster RD, Pogrel MA. The free fibula bone graft for salvaging failed mandibular reconstructions. J Oral Maxillofac Surg. 1997;55:1417–21. doi: 10.1016/s0278-2391(97)90641-8. [DOI] [PubMed] [Google Scholar]
- 15.Adekeye EO. Reconstruction of mandibular defects by autogenous bone grafts: A review of 37 cases. J Oral Surg. 1978;36:125–8. [PubMed] [Google Scholar]
- 16.Obiechina AE, Ogunlade SO, Fasola AO, Arotiba JT. Mandibular segmental reconstruction with iliac crest. West Afr J Med. 2003;22:46–9. doi: 10.4314/wajm.v22i1.27979. [DOI] [PubMed] [Google Scholar]
- 17.Arotiba JT, Obimakinde OS, Ogunlade SO, Fasola AO, Okoje VN, Akinmoladun VI, et al. An audit of mandibular defect reconstruction methods in a Nigerian Tertiary Hospital. Niger Postgrad Med J. 2011;18:172–6. [PubMed] [Google Scholar]
- 18.Bak M, Jacobson AS, Buchbinder D, Urken ML. Contemporary reconstruction of the mandible. Oral Oncol. 2010;46:71–6. doi: 10.1016/j.oraloncology.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 19.van Gemert JT, van Es RJ, Van Cann EM, Koole R. Nonvascularized bone grafts for segmental reconstruction of the mandible – a reappraisal. J Oral Maxillofac Surg. 2009;67:1446–52. doi: 10.1016/j.joms.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 20.Tidstrom KD, Keller EE. Reconstruction of mandibular discontinuity with autogenous iliac bone graft: Report of 34 consecutive patients. J Oral Maxillofac Surg. 1990;48:336–46. doi: 10.1016/0278-2391(90)90427-4. [DOI] [PubMed] [Google Scholar]
- 21.August M, Tompach P, Chang Y, Kaban L. Factors influencing the long-term outcome of mandibular reconstruction. J Oral Maxillofac Surg. 2000;58:731–7. doi: 10.1053/joms.2000.7255. [DOI] [PubMed] [Google Scholar]


