INTRODUCTION
Traditional clinical research is considered to increasingly fall short of the needs of clinicians, patients and funding agencies for many reasons (1,2). They include the high cost of clinical trials, slow results, difficult enrollment, often poor generalizability, and challenges in discovering clinical outcomes and side effects in a nuanced and clinically meaningful manner (1,3,4).
In consequence, the reuse of electronic data collected during clinical care has received increased attention as a method for increasing our evidence base (3–7). Reusing data from electronic health records (EHR) is complementary to or synergistic with more traditional research approaches (3,8), and has a number of potential advantages. EHRs can support many types of research, ranging from epidemiology and outcomes of chronic diseases to pharmacovigilance, adverse drug events and comparative effectiveness (7). Using EHR data for research can help increase efficiency (1,4), lower research costs (9), allow the study of patient rather than research participant populations, avoid certain selection biases, implement longitudinal studies, detect rare events, and discover drug side effects earlier than possible with traditional methods (10–12).
Reuse of electronic dental record (EDR) data has become increasingly attractive in the context of the National Dental Practice-based Research Network (NDPRN) initiative by the National Institute of Dental and Craniofacial Research (NIDCR). The experience during the practice-based research network (PBRN)’s initial funding period has shown that there are more relevant research questions than can be practically addressed using the typical PBRN study approach; that some important long-term research questions do not fit very well into the timeframe of a PBRN study; and that costs and practice workflow issues limit the “throughput” of the PBRN system. Given the fact that approximately 75% of DPBRN practitioners use a computer to manage clinical information and 15% are paperless (13), secondary analysis of EDR data is increasingly compelling.
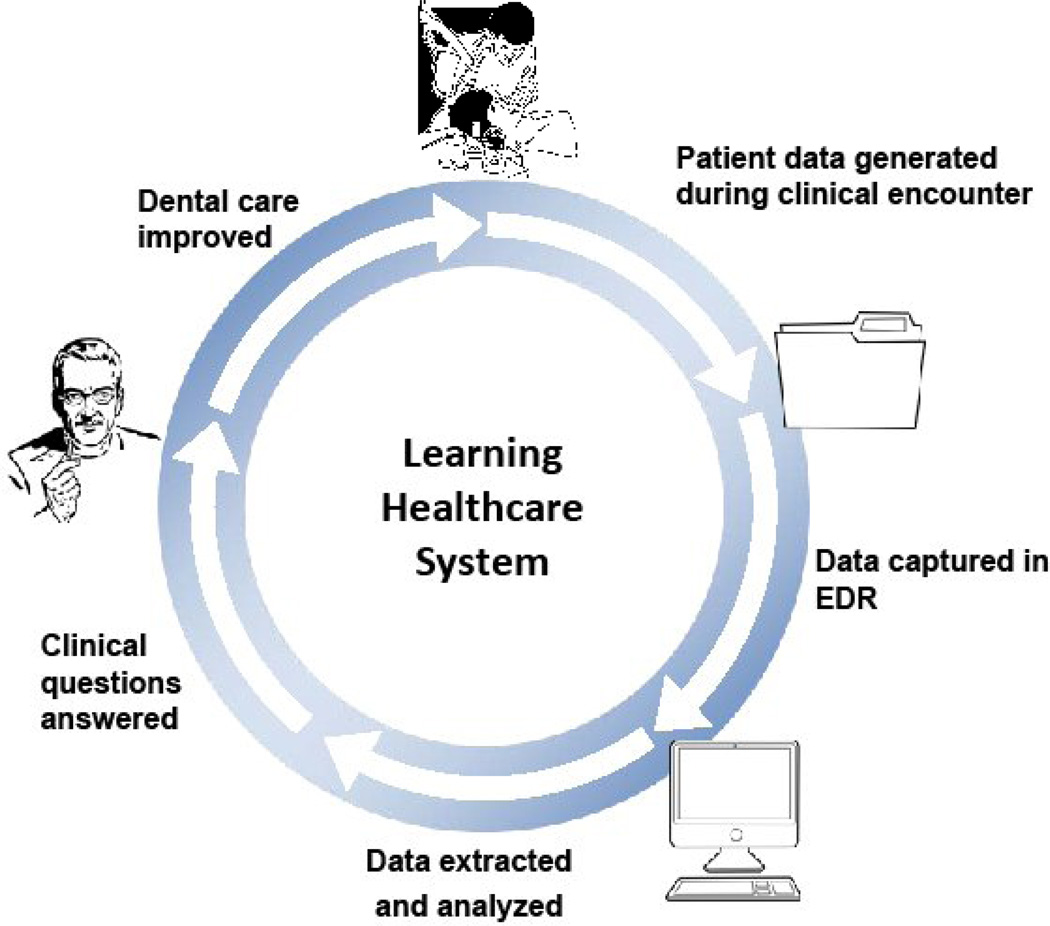
Figure 1 illustrates the workflow of a continuous cycle of improvement based on the analysis of electronic patient data in the context of a Learning Health Care System (3). Initially, patient data generated during the clinical encounter are captured electronically, ideally in standardized form. A data extraction, validation and analysis process produces answers to clinical questions. Once disseminated, those answers can help change clinical practice, resulting in improved care outcomes.
Figure 1.
Workflow of the Learning Healthcare System, in which reuse and analysis of electronic patient data forms the basis of a continuous quality improvement process
Clearly, data from EHRs have multiple limitations compared to the data collected in well-designed and –executed clinical trials. First, EHR data are collected for clinical, not research purposes (6,14). Resulting biases can range from threats to the representativeness of the population and clinician-related biases to missing data and poor characterization of outcomes (3). Second, data in EHRs tend not to be very standardized for multiple reasons (6,15). Many medical systems still favor free text over structured data entry (16); allow users to store the same or similar information in multiple places; and validate data inconsistently. Last, EHR data exhibit variable levels of accuracy (17,18) and typically provide poor support for systematic data extraction (6).
Despite these limitations, EHRs are increasingly seen as a potential source of data for research. This is evidenced in three large-scale initiatives in medicine using electronic medical records (EMR): the Distributed Ambulatory Research in Therapeutics Network (DARTNet) Institute (19), the electronic Primary Care Research Network (ePCRN) Consortium (20), and the Deliver Primary Health Care Information (DELPHI) project in Canada (14). In dentistry, the Consortium for Oral Health Research and Informatics (COHRI) (21) has created a data warehouse for research from patient records at several dental schools (see Appendix A).
As this review shows, there are three compelling reasons to develop our capabilities for reuse of EDR data collected during patient care. First, reuse of EHR data for research has added significantly to our capacity to generate knowledge from routine clinical care. Second, EDR data are a potentially valuable data source for clinical, comparative effectiveness, epidemiology and other research, especially given NIDCR’s recent emphasis on practice-based research. Last, electronic data are increasingly available from private practices due to the rapid adoption of computers. We therefore performed a review of the current status of reuse of electronic patient data for dental research, guided by the following questions: What types of research projects have used EDR/EMR data and what were the characteristics of these studies? What research questions did they examine? How did study characteristics relate to data sources, either EMR, EDR or both? What study variables were extracted from EDR and EMR systems? What advantages did reusing EDR/EMR data convey to these studies? What barriers/limitations were reported?
MATERIALS & METHODS
Data Sources and Search strategy
A list of MeSH terms, Emtree (Embase) thesaurus terms and general keywords was developed to search the MEDLINE and Embase databases. A biomedical librarian (RA) tested multiple combinations of terms to optimize the search (see Appendix B). Searches were limited to English, French, German, Finnish, Norwegian and Swedish language articles between January 1992 and January 2013. The database search was supplemented with hand-searching seven main journals that publish dental and informatics research: Journal of American Dental Association, Journal of Public Health Dentistry, Journal of Periodontology, Journal of Dental Research, Journal of Clinical Periodontology, Journal of Dentistry and Journal of the American Medical Informatics Association. Authors of 35 relevant papers were contacted to recommend additional studies. Searches were also conducted in the Publication Archive of the Dental Informatics Online Community1, an archive of ~ 2,300 articles on informatics and information technology in dentistry.
Study Selection Criteria and Process
Studies on dental and craniofacial topics, alone or in combination with medical aspects (such as conditions, medications and outcomes), were included. Studies had to include at least some data recorded electronically during routine patient care, using electronic records in the clinic. Studies were excluded if they exclusively analyzed electronic insurance/claim, administrative database, patient registry and hospital discharge data; databases that derived data from EDRs/EMRs; electronic data converted from paper records; research registries; and national survey databases. Systematic reviews were also excluded.
Three reviewers (MS, KL and TS) independently screened titles and abstracts of studies retrieved by the initial search for preliminary inclusion. Disagreements were resolved through discussion. Full-text articles for all candidate studies were then reviewed for final inclusion. When information on a study was unclear, the study authors were contacted for clarification.
Data Extraction
The data collected about each study are shown in Table 1. Three reviewers extracted qualitative and quantitative data from the studies independently.
Table 1.
List of data extracted from the studies.
| Type of research* |
|
| Study design | cross-sectional, case control, cohort, longitudinal, quasi-experimental, randomized clinical trials |
| Type(s) of data source(s) | EDR, EMR, paper records, film radiographs, surveys |
| Study population | adults, children, soldiers/veterans |
| Research questions | e.g. survival of root canal therapy |
| Study variables | e.g. patient-level variables, treatment variables, medications |
| Publication year | e.g. 1992, 2012 |
| Sample size | <1000, 1000–5000, 5001–99,999, ≥100,000 |
| Follow-up period | <3 years, 3–9 years, ≥10 years |
| Advantages and limitations of using EDR/EMR data |
extracted and summarized from the articles |
While different definitions exist for the types of research, we used the listed definitions for our study.
Data Analysis
Data analysis followed the guidelines by Popay et al. in 2006 (22). Though this study is not a systematic review, the approach was selected because it provides a coherent framework and permits the synthesis of studies that explore a wide range of research questions with various research designs (23). First, the authors developed a preliminary synthesis by grouping the studies by the type of research they belong to. Data were tabulated and compared to see if type of research correlates to EDR/EMR data usage in certain ways. Then, the studies were regrouped based on the research questions they addressed. Thematic analysis was conducted to identify patterns on how EDR/EMR data was used in relation to specific study characteristics. For instance, does research question dictates the use of certain data source? Whenever possible, we also conducted descriptive quantitative analysis. The first author conducted the initial analysis, checked with the research team and conducted additional analysis based on feedback. The team discussed and reached iteratively consensus about the analysis results through multiple meetings.
RESULTS
Study Selection
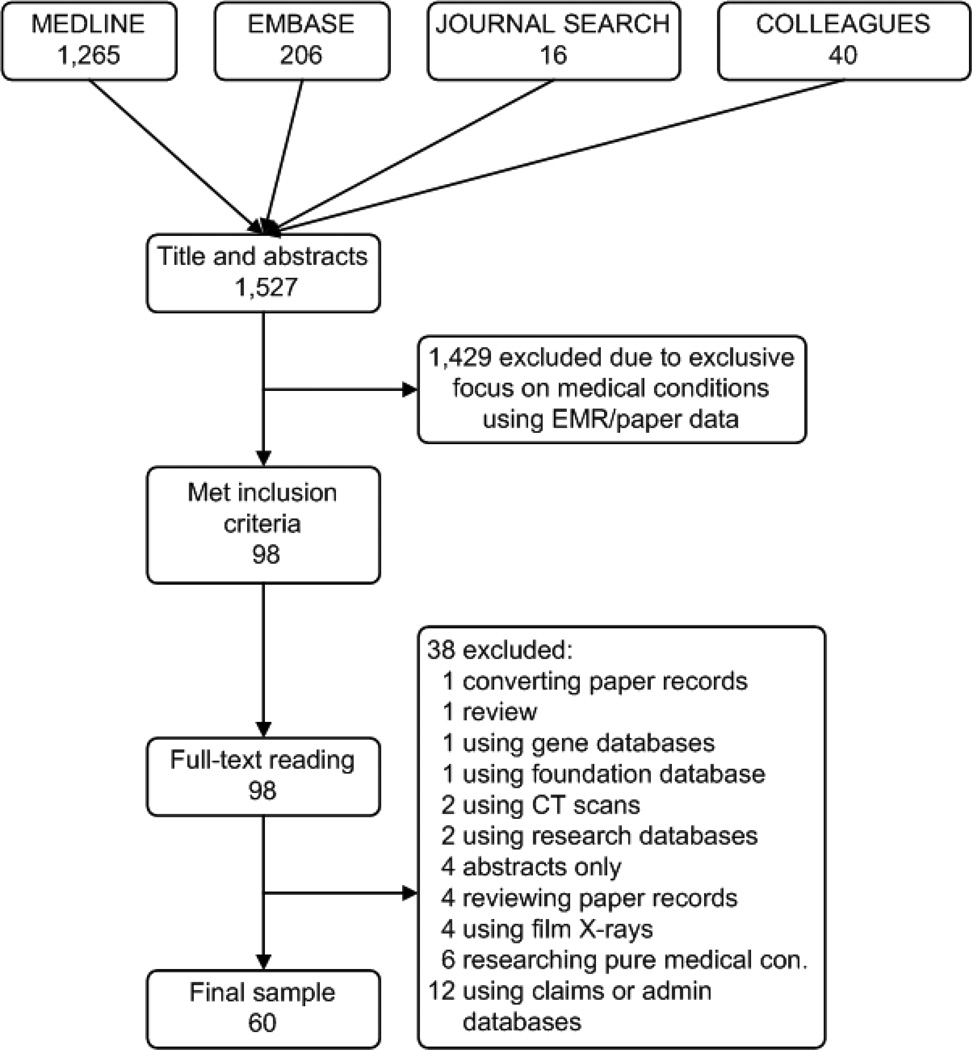
Figure 2 summarizes the results of search and review. Of an initial 1,527 studies, 98 met the criteria for preliminary inclusion, of which 60 remained after detailed review.
Figure 2.
A flowchart of the process of study selection
Study Characteristics
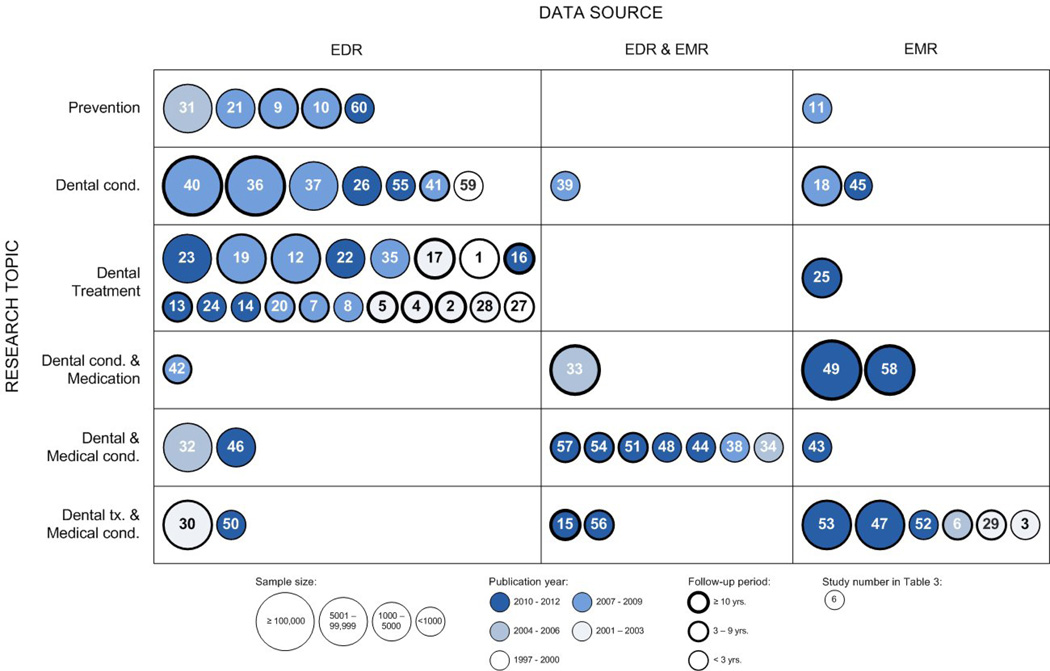
Table 2 summarizes the key characteristics of the studies. More detailed information is provided in Table 3. Figure 3 provides an additional representation that relates research topics to the type of electronic data used.
Table 2.
A summary of key characteristics of studies in the review (n = 60)
| Study characteristics | Frequencies | Percentages |
|---|---|---|
| Type of research | ||
| Epidemiology | 32 | 53 |
| Outcomes | 16 | 27 |
| Health services | 10 | 17 |
| Other | 2 | 3 |
| Research design | ||
| Cross-sectional | 25 | 42 |
| Cohort | 20 | 33 |
| Case control | 8 | 13 |
| Longitudinal | 5 | 8 |
| Quasi-experimental | 1 | 2 |
| Randomized control trial | 1 | 2 |
| Sample size | ||
| 1 – 999 | 35 | 57 |
| 1000 – 5000 | 11 | 19 |
| 5001 – 99,999 | 11 | 19 |
| 100,000 + | 3 | 5 |
| Follow-up period | ||
| 0 – 2 years | 26 | 43 |
| 3 – 9 years | 23 | 38 |
| 10 + years | 11 | 19 |
| Patient care setting | ||
| Dental school clinics | 15 | 25 |
| Dental HMOs | 11 | 19 |
| VA medical centers | 11 | 19 |
| Public dental health centers/nursing home | 10 | 17 |
| Other hospitals/clinics | 7 | 10 |
| Private dental practices | 6 | 10 |
| Research setting | ||
| VA medical centers | 9 | 15 |
| Kaiser Permanente | 9 | 15 |
| Dental insurance groups | 3 | 5 |
| Other | 39 | 65 |
Table 3.
A list of all studies included in the review
| # | Author (yr) | Study domain | Study design | Research questions | Country | Setting | Patient population |
|---|---|---|---|---|---|---|---|
| Outcomes research | |||||||
| 1 | Hujoel, Leroux, Selipsky, and White (2000) |
Dental treatment & medical condition |
Case control | Association between tooth loss and non- surgical periodontal treatment |
US | Dental HMOs | Adults |
| 2 | Aquilino, Shugars, Bader, and White (2001) |
General treatment | Longitudinal | Survival of teeth adjacent to treated and untreated missing tooth |
US | Dental HMOs | Adults |
| 3 | Stewart, Wager, Friedlander, and Zadeh (2001) |
Dental treatment & medical condition |
Case control | Effect of periodontal therapy on glycemic control |
US | VA medical centers |
Veterans |
| 4 | Aquilino and Caplan (2002) |
Endodontic treatment | Cohort | Association between crown placement and survival of endodontically treated teeth |
US | Dental school clinic |
Adults |
| 5 | Caplan, Kolker, Rivera, and Walton (2002) | Endodontic treatment | Cohort | Relationship between number of proximal contacts and survival of RCT teeth |
US | Dental school clinic |
Adults |
| 6 | Jones et al. (2007) | Dental treatment & medical condition | Randomized clinical trial | Efficacy of periodontal care on glycemic control |
US | VA medical centers |
Veterans |
| 7 | Caplan, Cai, Yin, and White (2005) | Endodontic treatment | Cohort | Impact of pulpal involvement and RCT on tooth survival |
US | Dental HMOs | Adults |
| 8 | Shelley, Johnson, and BeGole (2007) | Restoration & endodontic treatment | Cross-sectional | Use of EPR for quality of care assessment | US | Dental School clinic |
Adults |
| 9 | Leskinen et al (2008) |
Dental prevention | Cohort | Outcome of sealant treatment of first | Finland | Public health | Children |
| 10 | Leskinen et al (2008) |
Dental prevention | Cohort | Cost-effectiveness of two caries permanent preventive strategies |
Finland | Public health centers |
Children |
| 11 | Bassim, Gibson, Ward, Paphides, and Denucci (2008) |
Dental prevention & medical condition |
Quasi- experimental |
Association between use of oral hygiene aids and pneumonia mortality |
US | Nursing homes | Adults |
| 12 | Iqbal, Kurtz, and Kohli (2009) |
Endodontic treatment | Cross-sectional | Incidence and factors to endodontic flare- ups |
US | Dental school clinic |
Adults |
| 13 | George et al. (2011) | Implant treatment | Longitudinal | Clinical outcomes of a new implant Ti- Unite |
US | Public hospital | Adults |
| 14 | Worley et al. (2012) | General treatment | Cohort | Outcomes of restoration placed by dentists and RFAs |
US | Dental HMOs | Adults |
| 15 | Helenius-Hietala, Aberg, Meurman, and Isoniemi (2012) |
Dental treatment & medical condition |
Longitudinal | Dental treatment and post liver transplant infection risk |
Finland | University hospital |
Adults |
| 16 | Kolhatkar et al (2012) |
Dental treatment & medical condition |
Cohort | Outcome of CLS in HIV patients | US | Dental school clinic |
Adults |
| Health services research | |||||||
| 17 | Ojima, Hanioka, and Shizukuishi (2001) |
Periodontal treatment | Cohort | Risk factors to compliance of SPT | Japan | Dental school clinic |
Adults |
| 18 | Ladrillo, Hobdell, and Caviness (2006) |
Dental condition | Cross-sectional | Prevalence and characteristics of pediatric ED for dental problems |
US | Children’s hospital |
Children |
| 19 | Okunseri, Bajorunaite, Matthew, and Iacopino (2007) |
General treatment | Cross-sectional | Racial/ethnic differences in the provision of dental procedures |
US | Dental school clinic |
Adults |
| 20 | Luzzi and Spencer (2009) |
General treatment | Longitudinal | Public dental service utilization | Australia | Public dental service |
Adults |
| 21 | Okunseri, Bajorunaite, Mehta, Hodgson, and Iacopino (2009) |
Dental prevention | Cross-sectional | Gender difference in receipts of preventive dental treatment procedures |
US | Dental school clinic |
Adults |
| 22 | Naegele, Cunha- Cruz, and Nadanovsky (2010) |
General treatment | Cohort | Disparity between dental treatment needs and actual treatment completed |
Brazil | Dental private practices |
Adults |
| 23 | Eikenberg, Keeler, and Green (2011) |
General treatment | Cross-sectional | Dental care to soldiers in Iraq | US | Military clinics | Soldiers |
| 24 | Kudiyirickal and Hollinshead (2011) |
General treatment | Cross-sectional | Prescription of antimicrobials for orofacial infections by dentists |
UK | Dental private practices |
Adults |
| 25 | Chaudhari et al (2012) |
General treatment | Cross-sectional | Dental care utilization between adults with/without diabetes |
US | Various dental & medical providers |
Adults |
| 26 | Morgan et al. (2012) | Dental condition | Cross-sectional | Oral health status of people with intellectual and developmental disabilities |
US | Dental school clinic |
Adults |
| Epidemiology | |||||||
| 27 | Caplan and Weintraub (1997) |
Endodontic treatment | Case control | Risk factors to loss of RCT teeth | US | Dental HMOs | Adults |
| 28 | Caplan and White (2001) |
Endodontic treatment | Case control | Risk factors to noncompletion of RCT | US | Dental HMOs | Adults |
| 29 | Elter, White, Gaynes, and Bader (2002) |
Dental & medical condition |
Cohort | Association between depression and periodontal treatment outcome |
US | Dental HMOs | Adults |
| 30 | Fouad and Burleson (2003) |
Dental treatment & medical condition |
Cohort | Diabetes and endodontic treatment outcome |
US | Dental school clinic |
Adults |
| 31 | Lee and Dennison (2004) |
Dental prevention | Cross-sectional | Fluoridated water and oral health difference in children |
New Zealand |
Hospital/public health services |
Children |
| 32 | Byrappagari, Mascarenhas, and Chaffin (2006) |
Dental condition | Cross-sectional | Association between DFC and caries and tobacco risk assessment |
US | Military clinics | Soldiers |
| 33 | Maupomé, Peters, Rush, Rindal, and White (2006) |
Dental condition & medication |
Cohort | Association between Xerogenic medications and crown/root restorations |
US | Dental HMOs | Adults |
| 34 | Meurman, Furuholm, Kaaja, Rintamaki, and Tikkanen (2006) |
Dental & medical condition |
Cross-sectional | Association between oral health and pregnancy outcome |
Finland | Maternity health centers |
Adults |
| 35 | Hyde, Bader, and Shugars (2007) |
Endodontic treatment | Cross-sectional | Incidence of and risk factors of provisional crown failures |
US | Dental school clinic |
Adults |
| 36 | Korhonen, Salo, Suni, and Larmas (2007) |
Dental condition | Cohort | Oral health differences in Finland | Finland | Public health centers |
Adults & children |
| 37 | Forsberg, Sjodin, Lundgren, and Wanman (2008) |
Dental condition | Case control | Use of EDR in monitoring dental health | Sweden | Public dental services |
Adults |
| 38 | Friedlander, Tajima, Kawakami, Wang, and Tomlinson (2008) |
Dental & medical condition |
Case control | Relationship between nutritional status and masticatory function |
US | VA medical centers |
Veterans |
| 39 | Tavares et al. (2008) | Dental condition | Case control | Protection factors related to dental caries in children |
Brazil | Public oral health service |
Children |
| 40 | Korhonen, Gundagar, Suni Salo, and Larmas (2009) |
Dental condition | Cohort | DMF index differences in new and old patients |
Finland | Public health centers |
Adults |
| 41 | Ram, Teruel, Kumar, and Clark (2009) |
Dental condition | Cross-sectional | Prevalence and characteristics of patients with atypical odontalgia |
US | Dental school clinic |
Adults |
| 42 | Sedghizadeh et al (2009) |
Dental condition & medication |
Cross-sectional | Association between oral bisphosphonate and ONJ |
US | Dental school clinic |
Adults |
| 43 | Dissick et al. (2010) | Dental & medical condition |
Cohort | Association between periodontitis and rheumatoid arthritis |
US | VA medical centers |
Veterans |
| 44 | Friedlander, Sung, Chung, and Garrett (2010) |
Dental & medical condition |
Case control | Relationship between radiographic atheromas and chronic dental infection |
US | VA medical centers |
Veterans |
| 45 | Kidd, Beattie, and Campbell-Hewson (2010) |
Dental condition | Cross-sectional | Demographics and mechanisms of facial injury in children |
UK | Pediatric ED | Children |
| 46 | Sanders and Slade (2010) |
Dental & medical condition |
Cohort | Association between dental caries risk and Apgar score |
Australia | Public school dental clinics |
Children |
| 47 | Spangler et al (2010) |
Dental treatment & medical condition |
Cross-sectional | Association between periodontal diseases and GHb level |
US | Various dental & medical providers |
Adults |
| 48 | Alman et al. (2011) | Dental treatment & medical condition |
Cohort | Association between periodontal diseases and CHD |
US | VA medical centers |
Veterans |
| 49 | Fellows et al. (2011) | Dental condition & medication |
Cohort | Oral bisphosphonate and incidence of ONJ | US | Dental HMOs | Adults |
| 50 | Kassab et al. (2011) | Dental treatment & medical condition |
Cross-sectional | Treatment for heart diseases and invasive dental care |
US | Dental school clinic |
Adults |
| 51 | Mador et al. (2011) | Dental & medical condition |
Cross-sectional | Association of OSA and risk of cardiorespiratory complications |
US | VA medical centers |
Veterans |
| 52 | Tami-Maury et al (2011) |
Dental condition & medical treatment |
Cohort | Risk factors of oral manifestation among HIV patients |
US | University clinic | Adults |
| 53 | Newton et al. (2011) | Dental & medical condition |
Cross-sectional | Prevalence of periodontal care among patients with/without diabetes |
US | Various dental & medical providers |
Adults |
| 54 | Chang, Tanner, Harada, Garrett, and Friedlander (2012) |
Dental & medical condition |
Cross-sectional | Prevalence of atheromas of patients with OSA vs patients with syndrome Z |
US | VA medical centers |
Veterans |
| 55 | Kudiyirickal and Hollinshead (2012) |
Dental condition | Cross-sectional | Characteristics of orofacial infections in dental patients |
UK | Dental private practices |
Adults |
| 56 | Mosen, Pihlstrom, Snyder, and Shuster (2012) |
Dental treatment & medical condition |
Case control | Receipt of dental care on diabetes control and care utilization |
US | Dental HMOs | Adult |
| 57 | Tanner et al. (2012) | Dental & medical condition |
Cross-sectional | Association between OSA and Metabolic Syndrome |
US | VA medical centers |
Veterans |
| 58 | Yamazaki et al (2012) |
Dental condition & medication |
Cohort | Risk of oral BPs and other drugs for ONJ | Japan | University hospital |
Adults |
| Other | |||||||
| 59 | Powell, Leroux, Martin, and White (2000) |
Dental condition | Cross-sectional | Use of insurance claim data in identifying caries |
US | Dental HMOs | Adults |
| 60 | Morgan et al. (2012) | Dental prevention | Cross-sectional | Use of EDR to track tobacco use and monitor cessation interventions |
US | Dental school clinic |
Adults |
Note: Abbreviations used in this table are: RCT – Randomized control trial; EPR – Electronic patient records; RFAs – Restorative function auxiliaries; CLS – Crown lengthening surgery; SPT – Supportive periodontal therapy; ED – Emergency department; DFC – Dental fitness classification; EDR – Electronic dental records; DMF – Decayed, missing and filled teeth; ONJ - Osteonecrosis of the jaw; CHD – Coronary heart disease; OSA – Obstructive sleep apnea; BPs - Oral bisphosphonates
Figure 3.
Sample size, publication year and follow-up period for all studies arranged by research topic and use of electronic data source
1. What types of research projects have used EDR/EMR data and what were their characteristics?
In summary, more than half of the studies (32 studies, 53%) addressed research questions on epidemiological topics. All but two studies were retrospective, with cross-sectional as the leading study design (25 studies, 42%). The majority of studies (43, 72%) were conducted in the US. Follow-up periods ranged from 1 to 12 years, with patient data from as early as 1985 and as recent as 2011. Sample sizes varied substantially, from 9 patients with osteonecrosis of the jaw (ONJ) (24) to 153,619 general patients (25). Fifty-three studies focused on adult patients and 7 on children. Patients from 15 studies (25%) were seen at dental school clinics, with dental care provided by private practitioners in only 6 studies. In research settings, researchers from three organizations conducted one-third of the studies (21 studies). Thirty-five studies (58%) used exclusively electronic data while the remaining 25 studies were supplemented with paper data.
2. What research questions did these studies examine?
The studies addressed a variety of research questions. The majority of epidemiological studies investigated the association of risk factors with various dental or medical conditions, such as fluoridated water and caries (26), bisphosphonate therapy and ONJ (24,27), prevalence of atheromas and Obstructive Sleep Apnea (OSA) (28), and periodontal disease and depression (29). Ten health services studies examined access to care, such as pediatric emergency visits for dental problems (30), public dental service utilization (31), and care delivery, such as dental care to soldiers (32), racial difference in provision of dental procedures (33), and disparities between treatment needs and provision (34). Sample outcomes studies looked at the survival of root canal filled teeth (35–37), the effect of periodontal treatment on diabetes control (38) and endodontic treatment outcomes (39).
3. How did study characteristics relate to data sources, either EDR, EMR or both?
When the type of research was correlated with the use of EDR/EMR data, no pattern emerged for either epidemiological or outcomes studies. For health services studies, however, 9 out of 10 studies used exclusively electronic data with one supplementing with paper patient registration data (40).
The relationship between research questions/topics and use of data source was then examined (Figure 3). The 12 studies that described the prevalence and characteristics of a dental disease or a population’s oral health status tended to use only EDR (8 studies) or EMR (4 studies) data. They were often cross-sectional studies with a less than 5-year follow-up period. For instance, Ladrillo et al. in 2006 analyzed two hospital electronic databases to describe the characteristics of pediatric ER visits for dental problems (30), and Ram et al.’s 2009 study used an EMR to determine the prevalence and characteristics of patients with atypical odontalgia (AO) (41).
Among studies on dental treatments, 10 looked at general dental services utilization, of which 9 used EDR data only. Seven studies investigated the risk factors/outcomes of endodontic procedures. All except one relied on both EDR and other data sources and followed patients for 6 years or more. As these studies attempted to identify various risk factors, they required variables at the patient, treatment and tooth levels, some of which may be unavailable in EDRs. In Caplan et al.’s 2002 study on the relationship between the number of proximal contacts and survival of root canal therapy, patient demographics and provider were extracted from an EDR; tooth arch, type and treatment complications from paper treatment notes; and radiographs and dental/medical histories from health questionnaires (37).
For studies exploring the impact of medications on dental diseases, use of data sources depended partially on where medications were documented. In four studies, one used an EDR exclusively, one both EDR and EMR, and two EMR data. Even for a similar research question, data sources varied. For example, to study the relationship between bisphosphonate use and ONJ, Sedghizadeh et al. queried an AxiUm database in 2009 for ONJ diagnosis variables (24) while Fellows et al. resorted to an EMR for the same data in their 2011 study (27).
Another group of 24 studies examined oral-systemic connections, among which 10 explored the association between dental and medical conditions and an equal number the effect of dental treatment on medical conditions. Given the dual focus, these studies used both dental and medical data; however, the two subgroups revealed different patterns in electronic data usage. In the first group, 8 of 10 studies used VA’s integrated electronic medical/dental record to study topics such as periodontal disease and coronary heart disease (CHD) (42) and chronic dental infection and atheromas (43), with only 2 studies using other data sources. Conversely, for studies on dental treatment effect, 7 used data other than electronic sources and, more notably, all medical data were from EMR but dental data from other sources. For example, in Jones et al.’s 2007 study on the efficacy of periodontal care on glycemic control, HbA1c values were extracted from medical records but all periodontal treatment data acquired through a clinical examination (44).
4. What study variables were extracted from EDR and EMR systems?
Table 4 lists the variables most commonly used in the studies and from what sources they were extracted. Predominant patient-level variables were age, gender, type of insurance, but rarely socioeconomic status. Diagnostic variables referred to dental and medical diagnoses, such as caries and oral infections. Treatment procedures, particularly restorative, endodontic and periodontal treatments, were common. In studies involving medications, medication name, dosage and duration were often used. The most extracted medical history variables were diabetes diagnosis, glucose level and smoking status/use. As the results show, patient demographics and medication variables may be available in both EMRs and EDRs; treatment and tooth variables mostly in EDRs; and medical history in EMRs. Variables extracted the least from EMRs/EDRs were health behaviors and social factors.
Table 4.
Study variables extracted from electronic records and other sources
| Study variables extracted | Total # of studies |
# with EDR data |
# with EMR data |
# with other sources |
|---|---|---|---|---|
| Patient-level variables | ||||
| Age | 43 | 22 | 14 | 7 |
| Sex | 34 | 17 | 10 | 7 |
| Race/ethnicity | 16 | 4 | 9 | 3 |
| Weight/height/BMI | 15 | 0 | 14 | 1 |
| Insurance | 13 | 7 | 6 | 0 |
| Social-economic status | 11 | 3 | 3 | 2 |
| Vital status | 3 | 0 | 3 | 0 |
| Medical/primary care use | 3 | 0 | 3 | 0 |
| Marital status | 3 | 2 | 1 | 0 |
| Education level | 2 | 0 | 1 | 1 |
| Other patient-level variables (e.g., birth weight, vaccination, Apgar scores, etc) |
20 | 6 | 8 | 6 |
| Dental treatment variables | ||||
| Restorative treatment | 15 | 13 | 0 | 2 |
| Endodontic treatment | 14 | 11 | 0 | 4 |
| Periodontal treatment | 13 | 6 | 0 | 7 |
| Surgical treatment | 9 | 7 | 0 | 2 |
| PDTP treatment | 6 | 6 | 0 | 0 |
| Surgeries (ENT, face, etc) | 3 | 3 | 0 | 0 |
| Orthodontic treatment | 3 | 1 | 0 | 2 |
| Dentures | 3 | 3 | 0 | 0 |
| Other treatment variables (e.g., diagnoses, techniques, codes, etc) |
15 | 13 | 1 | 1 |
| Tooth-level variables | ||||
| Caries activities | 13 | 8 | 1 | 4 |
| Dmfs and/or DMFS | 8 | 8 | 0 | 0 |
| Tooth type | 7 | 5 | 0 | 2 |
| # of proximal contacts | 4 | 0 | 0 | 4 |
| Tooth arch | 3 | 0 | 0 | 3 |
| Periapical lesion on root | 3 | 0 | 1 | 2 |
| Tooth number | 2 | 2 | 0 | 0 |
| Pulp diagnosis | 2 | 0 | 0 | 2 |
| Other tooth-level variables (# of good, missing teeth, alveolar bone loss, etc) |
17 | 5 | 0 | 12 |
| Dental history | ||||
| Gums bleeding | 6 | 0 | 0 | 6 |
| Orofacial injuries/infections | 4 | 1 | 0 | 3 |
| Osteonecrosis of the jaw | 3 | 2 | 1 | 0 |
| Obstructive sleep apnea | 3 | 0 | 3 | 0 |
| Dental anxiety | 2 | 0 | 0 | 2 |
| History of wearing denture | 2 | 0 | 0 | 2 |
| Atypical odontalgia | 1 | 1 | 0 | 0 |
| Other dental conditions (e.g. pain, dry socket, etc) |
9 | 6 | 2 | 1 |
| Medical history | ||||
| Diabetes (diagnosis, glucose level, GHb, A1c) |
17 | 3 | 12 | 2 |
| Smoking status/use | 16 | 5 | 10 | 1 |
| Heart diseases | 4 | 2 | 2 | 0 |
| Immune disorders (HIV, lupus, etc) | 3 | 0 | 1 | 2 |
| Cancer | 3 | 1 | 2 | 0 |
| Hypertension | 3 | 1 | 2 | 0 |
| Osteoporosis | 3 | 1 | 2 | 0 |
| Cholesterol values (HDL, LDL, triglycerides) |
3 | 0 | 3 | 0 |
| Other medical conditions (e.g. dementia, pneumonia, injuries, etc) |
20 | 4 | 10 | 6 |
| Medications | ||||
| Name/type of medication | 21 | 7 | 9 | 5 |
| Numbers of medication | 4 | 0 | 1 | 3 |
| Dosage/duration of medication | 4 | 2 | 2 | 0 |
| Health behaviors/risks & social factors | ||||
| Oral status (brushing, flossing, stain) | 5 | 0 | 2 | 3 |
| Fluoridated water | 4 | 3 | 0 | 1 |
| Alcohol/substance use | 4 | 0 | 3 | 1 |
| Sugar consumption | 3 | 0 | 0 | 3 |
| Mental health | 2 | 1 | 1 | 0 |
| Caries/perio risk | 4 | 4 | 0 | 0 |
| Oral health (good, fair, etc) | 2 | 0 | 0 | 2 |
| Sore risk | 1 | 0 | 1 | 0 |
| Fall risk | 1 | 0 | 1 | 0 |
| Grind or clench teeth | 1 | 0 | 0 | 1 |
| Activity level | 1 | 0 | 0 | 1 |
| Participation in community | 1 | 0 | 1 | 0 |
| Other variables | ||||
| Provider (type, age, sex) | 9 | 9 | 0 | 0 |
| Number of dental/medical care visits | 6 | 4 | 0 | 2 |
| Date of visits | 5 | 4 | 1 | 0 |
| Experience of provider | 2 | 2 | 0 | 0 |
| New vs. old patients | 2 | 2 | 0 | 0 |
| Type of visits | 2 | 2 | 0 | 0 |
| Home-hospital distance | 1 | 1 | 0 | 0 |
| Diabetes-related visits/hospital admission |
4 | 0 | 4 | 0 |
5. What advantages did reusing EDR/EMR data convey to these studies?
Forty-nine of the 60 studies reported strengths and/or limitations of using electronic data, typically as part of the study limitations (Table 5). The most frequently reported advantage was the ability to conduct studies of significant statistical power due to large sample sizes. For instance, in Newton et al.’s 2011 study on periodontal care and diabetes, linking electronic dental claims and medical record data yielded a sample of more than 46,000 people with data about medical and dental care, one of the largest of its type in the literature. Access to data on multiple medical conditions allowed researchers to obtain well-matched controls and ascertain important potential confounders (45). Similarly, Korhonen et al. in 2009 were able to compare the decayed, missing and filled teeth (DMF) index of 153,619 patients in two Finish towns through access to digital data in public dental offices (25).
Table 5.
Advantages and limitations of using EMR/EDR data reported in the studies
| Advantages & limitations of using EMR/EDR | Studies |
|---|---|
| Advantages | |
| • Study diseases/conditions in a large sample with more statistical power | (14), (31), (42), (47), (53), (60) |
| • Save time compared to reviewing paper charts/records | (14), (36), (59) |
| • Provide a rich resource for outcomes research | (29), (35), (58) |
| • Identify patients with rare diseases (ONJ, AO, etc) | (41), (49) |
| • Track patients for an extended period of time | (30), (31), (60) |
| • Provide valid and representative sample | (23), (26) |
| • More systematic data documentation | (15), (51) |
| • Flexible to add specific fields for data collection | (30) |
| • More valid data than self-reported data | (20) |
| • Provide data on comorbid medical conditions | (6) |
| • Ability to collect data in real time | (52) |
| • Ability to ascertain potential confounders | (53) |
| Limitations | |
| • Some study variables not documented in EDR (history of tobacco use, socio-economic status, education, compliance with treatment, etc) | (1), (2), (4), (5), (7), (8), (19), (23), (25), (28), (29), (37), (49), (53), (54), (56) |
| • Inaccurate, incomplete or missing data | (8), (15), (19), (27), (29), (36), (45), (46), (49), (50), (55), (58), (60) |
| • Study sample limited to patients of one EDR/institution | (18), (21), (37), (41), (57) |
| • Study sample limited to only male population | (6), (43), (44), (54), (57) |
| • Inconsistency in data documentation | (34), (36), (40), (46), (53) |
| • Data validity and reliability in question | (2), (4), (7), (31), (52) |
| • Inability to control experimental conditions | (60) |
Electronic data were also valuable in providing a rich resource for outcomes research, identifying patients with rare diseases and saving study time. Longitudinal clinical data available in both an EMR and EDR facilitated a rich study on the effect of periodontal treatment outcome on depression (29), failures of provisional crowns (46) and the relationship of osteoporosis medications and ONJ (47). For identifying relatively uncommon diseases, such as OA or ONJ, Ram et al’s 2009 study (41) used EMR search functions to identify 64 OA patients in a population of 3,000 over 5 years. Querying an EDR and an EMR, Sedghizadeh in 2009 identified 9 out of 208 patients on alendronate with a diagnosis of active ONJ (24). Other less frequently mentioned advantages of using electronic data included the ability to collect data in real time (48) and more systematic data documentation (49).
6. What barriers or limitations of reusing EDR/EMR data were reported?
In terms of limitations, over half of the studies considered data availability and quality as major problems. Specifically, 16 studies were unable to obtain study-specific variables not routinely captured in EDRs; 12 reported inaccurate, incomplete or missing data; and 5 cited inconsistency in data documentation as a limitation. For instance, socioeconomic status, race, education, smoking and treatment compliance were often used as confounding variables, but they were not routinely documented in most EDRs. In the studies on root canal treatment, variables such as degree of bone loss and number of proximal contacts, were not available electronically (37,39). In other studies, data on patient visits to other providers and pharmacy records on medication usage were not accessible (42,50).
A second limitation was inaccurate, incomplete and missing data, potentially attributed to coding errors and inconsistent data documentation practices when multiple providers or uncalibrated examiners entered data. For example, the recording of the DMF index between dentists varied greatly in Finland, resulting in discrepancies in the data collected from various dental offices (25). In Sanders et al’s 2010 study on the relationship between Apgar score and dental caries risk for children, missing Apgar scores as a primary variable for some participants posed a challenge for statistical analysis (51).
In addition, characteristics of study populations sometimes raised concerns about selection bias and reduced the generalizability of study results, such as in the VA studies with their patient population of predominantly male veterans (52,53).
DISCUSSION
This review has yielded important early insights into the current state of the reuse of EDR/EMR data for dental clinical research. The fact that we were able to identify only 60 studies published between 1992 and 2012 (40% of them published since 2010) indicates that the reuse of electronic data in dentistry is in an early stage but rapidly accelerating. Evidence suggests that the number of medical studies reusing electronic patient data is significantly larger. Key findings from this review include:
Reuse of electronic data supports primarily retrospective research
Electronic patient data are relatively easy and cheap to reuse for research. However, they can only be “after the fact,” restricting most studies to analyzing data retrospectively. However, within this constraint, a variety of study designs are feasible, such as cross-sectional, longitudinal and cohort studies. Even a prospective approach is possible, as long as the necessary variables are accommodated ahead of the study and captured in the system by clinicians (38,44).
Research is focused on epidemiology and risk factors
The fact that thirty-two of 60 studies addressed questions related to epidemiology and risk factors is likely due to the ease with which data about conditions such as caries and periodontal disease can be extracted from highly structured EDRs. Health services research studies (10 in our review) may benefit from the fact that dental records contain more clinical variables than insurance claims databases. Our review did not locate comparative effectiveness research studies, for which electronic patient records are considered to be an essential platform (54).
Research combining EDR and EMR data is limited
Only 10 of the 24 studies that explored oral-systemic connections used both EDR and EMR data, while the remainder supplemented electronic data with clinical exams, questionnaires and insurance claims. Research combining electronic dental and medical data is difficult unless they are maintained in a way that allows them to be linked easily, such as at the VA and HealthPartners.
EDRs in private practice are essentially untapped
Only three studies analyzed EDR data from private dentists, suggesting a huge gap in addressing clinical research questions in private practice. We may be able to reduce this gap as more dentists adopt EDRs, as suggested by our recent survey (13).
EDRs/EMRs often need to be supplemented with other data sources
Close to half the studies supplemented EDR/EMR data with data from other sources. Our results (Table 4) provide important guidance on which data can most likely be found in which data source(s).
Contextual and cultural factors determine study feasibility
Several studies in Europe took advantage of standardized EDRs and databases for monitoring oral health at the local and national level. A higher degree of standardization of electronic records and better adoption of public health databases and registries make data more easily available to dental research than in the US.
While many of the studies appear to have been successful in addressing important research questions, they also highlighted important current limitations in reusing electronic data:
Study samples are often idiosyncratic and not generalizable to the population at large
While the studies in this review often used samples much larger than typically in traditional studies, many were constrained by the population covered in the database(s). For instance, most studies included only patients, not people, limiting inferences for the general population. Depending on the utilization of dental services (in the US, about 70% of the population have at least one dental visit per year, and in Europe the number ranges from 30%–85% across countries) (http://www.cecdo.org/pages/database intro.html), such studies are bound to exclude large segments of the population. Others projects studied special populations, such as military veterans and patients enrolled in a health maintenance organization (HMO), also reducing their generalizability.
Methodological issues threaten validity
Studies reusing data collected in the course of clinical practice differ from rigorously conducted clinical studies in many ways. Clinicians are typically not as well calibrated and trained as examiners in a research study. Inter-individual variation among clinicians injects variability. Lack of consensus on clinical measurements of findings and diagnoses reduce the ability to collect valid data. For instance, the ambiguity of the definition of periodontitis and the methods to measure it (55) make it unclear how EDR data relate to periodontal disease entities, and to what extent these data are accurate and comparable across systems and providers. In addition, data accuracy and reliability are not routinely assessed in clinical care, making the measurement of error difficult.
Design and configuration of electronic record systems constrain data collection
As one of our previous studies (56) has found, EDRs often constrain the clinician’s ability to record specific data. EDRs accommodate some clinical data only poorly or not at all, forcing clinicians to abandon recording or find workarounds. Even if data fields exist, they may not capture data as required for a research study. Second, the process of research data capture is not integrated into EDRs (57). Last, electronic record systems are typically not interoperable, requiring significant effort to synthesize data about individual patients (58).
While reuse of electronic data for dental clinical research is still in its infancy, it is clear that healthcare as a whole is moving towards exploiting clinical data as a source of new knowledge (3). While clinical data suffer from multiple limitations compared to the research data collected in rigorously conducted studies, they are a potentially valuable resource that can complement and enrich the insights traditional research is generating. Part of our current difficulties is that we have never reused clinical data in dentistry broadly and for a variety of topics. Now that we are beginning to do so, we find that many assumptions about the validity, accuracy, reliability and utility of these data may be flawed. However, only through reuse and analysis of these data will we find ways to improve their usefulness for research.
LIMITATIONS
This review has two main limitations. First, our search strategy may not have identified all possible studies of interest due to limitations of database coverage and idiosyncrasies in article indexing. We attempted to compensate for this potential limitation by hand-searching key journals and using a snowball method. We believe that our detail-oriented approach identified as many studies as was possible. Second, some of the studies did not provide detailed descriptions of their data sources. In addition, authors used various terms to describe electronic data sources, such as computerized treatment database, patient database, or practice management systems. This circumstance sometimes impeded exact categorization of particular studies.
Supplementary Material
ACKNOWLEDGEMENT
We thank Michael Dziabiak for his assistance with the preparation of the manuscript, authors for their recommendations for additional studies and several colleagues from the American College of Medical Informatics for their valuable suggestions. This study was supported by NIH grants R21-DE-19683 and R21-DE-21178.
A LIST OF ABBREVIATIONS
- EHR
Electronic health records
- EDR
Electronic dental records
- NDPBRN
National Dental Practice-based Research Network
- NIDCR
National institute of Dental and Craniofacial Research
- PBRN
Practice-based research network
- EMR
Electronic medical records
- ONJ
Osteonecrosis of the jaw
- VA
Veterans Affairs
- OSA
Obstructive sleep apnea
- AO
Atypical odontalgia
- CHD
Coronary heart disease
- DMF
Decayed, missing and filled teeth
- HMO
Health maintenance organization
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declared no conflicts of interest regarding the authorship and/or publication of this article.
Contributor Information
Mei Song, Research Scientist, Center for Dental Informatics, Department of Dental Public Health, University of Pittsburgh School of Dental Medicine, Pittsburgh, PA 15261.
Kaihong Liu, Postdoctoral Scholar, Center for Dental Informatics, Department of Dental Public Health, University of Pittsburgh School of Dental Medicine, 3501 Terrace Street, Pittsburgh, PA 15261.
Rebecca Abromitis, Reference Librarian, Liaison to the School of Dental Medicine, University of Pittsburgh, Health Sciences Library System, 200 Scaife Hall, 3550 Terrace Street, Pittsburgh, PA 15261.
Titus L. Schleyer, Associate Professor and Director, Center for Dental Informatics, Department of Dental Public Health, University of Pittsburgh School of Dental Medicine, 331 Salk Hall, 3501 Terrace Street, Pittsburgh, PA 15261
REFERENCES
- 1.Kahn MG, Kaplan D, Sokol RJ, DiLaura RP. Configuration challenges: implementing translational research policies in electronic medical records. Academic Medicine: Journal of the Association of American Medical Colleges. 2007;82(7):661–669. doi: 10.1097/ACM.0b013e318065be8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.M Smith, R Saunders, L Stuckhardt, JM McGinnis., editors. Committee on the Learning Health Care System in America, et al. Best care at lower cost: the path to continuously learning health care in America. Washington, D.C: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 3.L Olsen, D Aisner, JM McGinnis., editors. Roundtable on Evidence-based Medicine. The learning healthcare system: workshop summary. Washington, D.C: The National Academis Press; 2007. [PubMed] [Google Scholar]
- 4.Sung NS, Crowley WF, Genel M, Salber P, Sandy L, Sherwood LM, et al. Central challenges facing the national clinical research enterprise. JAMA: The Journal of the American Medical Association. 2003 Mar 12;289(10):1278–1287. doi: 10.1001/jama.289.10.1278. [DOI] [PubMed] [Google Scholar]
- 5.Prokosch HU, Ganslandt T. Perspectives for medical informatics. Reusing the electronic medical record for clinical research. Methods of Information in Medicine. 2009;48(1):38–44. [PubMed] [Google Scholar]
- 6.Terry AL, Chevendra V, Thind A, Stewart M, Marshall JN, Cejic S. Using your electronic medical record for research: a primer for avoiding pitfalls. Family Practice. 2010 Feb;27(1):121–126. doi: 10.1093/fampra/cmp068. [DOI] [PubMed] [Google Scholar]
- 7.Pearson JF, Brownstein CA, Brownstein JS. Potential for electronic health records and online social networking to redefine medical research. Clinical Chemistry. 2011 Feb;57(2):196–204. doi: 10.1373/clinchem.2010.148668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tannen RL, Weiner MG, Xie D. Use of primary care electronic medical record database in drug efficacy research on cardiovascular outcomes: comparison of database and randomised controlled trial findings. British Medical Journal. 2009;338:b81. doi: 10.1136/bmj.b81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kohane IS. Using electronic health records to drive discovery in disease genomics. Nature Reviews Genetics. 2011 Jun;12(6):417–428. doi: 10.1038/nrg2999. [DOI] [PubMed] [Google Scholar]
- 10.Seyfried L, Hanauer DA, Nease D, Albeiruti R, Kavanagh J, Kales HC. Enhanced identification of eligibility for depression research using an electronic medical record search engine. International Journal of Medical Informatics. 2009 Dec;78(12):e13–e18. doi: 10.1016/j.ijmedinf.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilke RA, Berg RL, Peissig P, Kitchner T, Sijercic B, McCarty CA, et al. Use of an electronic medical record for the identification of research subjects with diabetes mellitus. Clinical Medicine & Research. 2007 Mar;5(1):1–7. doi: 10.3121/cmr.2007.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brownstein JS, Sordo M, Kohane IS, Mandl KD. The tell-tale heart: population-based surveillance reveals an association of rofecoxib and celecoxib with myocardial infarction. PLoS One. 2007;2(9):e840. doi: 10.1371/journal.pone.0000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schleyer T, Song M, Gilbert GH, Rindal DB, Fellows JL, Gordan VV, et al. Electronic dental record use and clinical information management patterns among practitionerinvestigators in The Dental Practice-Based Research Network. Journal of the American Dental Association. 2013 Jan;144(1):49–58. doi: 10.14219/jada.archive.2013.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart M, Thind A, Terry AL, Chevendra V, Marshall JN. Implementing and maintaining a researchable database from electronic medical records: a perspective from an academic family medicine department. Healthcare Policy. 2009 Nov;5(2):26–39. [PMC free article] [PubMed] [Google Scholar]
- 15.Kristianson KJ, Ljunggren H, Gustafsson LL. Data extraction from a semi-structured electronic medical record system for outpatients: a model to facilitate the access and use of data for quality control and research. Health Informatics Journal. 2009 Dec;15(4):305–319. doi: 10.1177/1460458209345889. [DOI] [PubMed] [Google Scholar]
- 16.Lependu P, Iyer SV, Fairon C, Shah NH. Annotation Analysis for Testing Drug Safety Signals using Unstructured Clinical Notes. Journal of Biomedical Semantics. 2012;3(Suppl 1):S5. doi: 10.1186/2041-1480-3-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hogan WR, Wagner MM. Accuracy of data in computer-based patient records. Journal of the American Medical Informatics Association. 1997 Sep;4(5):342–355. doi: 10.1136/jamia.1997.0040342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faulconer ER, de Lusignan S. An eight-step method for assessing diagnostic data quality in practice: chronic obstructive pulmonary disease as an exemplar. Informatics Primary Care. 2004;12(4):243–254. [PubMed] [Google Scholar]
- 19.Libby AM, Pace W, Bryan C, Anderson HO, Ellis SL, Allen RR, et al. Comparative effectiveness research in DARTNet primary care practices: point of care data collection on hypoglycemia and over-the-counter and herbal use among patients diagnosed with diabetes. Medical Care. 2010 Jun;48(6 Suppl):S39–S44. doi: 10.1097/MLR.0b013e3181ddc7b0. [DOI] [PubMed] [Google Scholar]
- 20.Delaney BC, Peterson KA, Speedie S, Taweel A, Arvanitis TN, Hobbs FD. Envisioning a learning health care system: the electronic primary care research network, a case study. Annals of Family Medicine. 2012 Jan;10(1):54–59. doi: 10.1370/afm.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stark PC, Kalenderian E, White JM, Walji MF, Stewart DC, Kimmes N, et al. Consortium for oral health-related informatics: improving dental research, education, and treatment. Journal of Dental Education. 2010 Oct;74(10):1051–1065. [PMC free article] [PubMed] [Google Scholar]
- 22.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. Lancaster, UK: Institute for Health Research, Lancaster University; 2006. [Google Scholar]
- 23.Centre for Reviews and Dissemination. Systematic reviews: CRD's guidance for undertaking reviews in health care. 3rd ed. CRD, University of York; 2009. [Google Scholar]
- 24.Sedghizadeh PP, Stanley K, Caligiuri M, Hofkes S, Lowry B, Shuler CF. Oral bisphosphonate use and the prevalence of osteonecrosis of the jaw: an institutional inquiry. Journal of the American Dental Association. 2009 Jan;140(1):61–66. doi: 10.14219/jada.archive.2009.0019. [DOI] [PubMed] [Google Scholar]
- 25.Korhonen M, Gundagar M, Suni J, Salo S, Larmas M. A practice-based study of the variation of diagnostics of dental caries in new and old patients of different ages. Caries Research. 2009;43(5):339–344. doi: 10.1159/000231570. [DOI] [PubMed] [Google Scholar]
- 26.Lee M, Dennison PJ. Water fluoridation and dental caries in 5- and 12-year-old children from Canterbury and Wellington. New Zealand Dental Journal. 2004 Mar;100(1):10–15. [PubMed] [Google Scholar]
- 27.Fellows JL, Rindal DB, Barasch A, Gullion CM, Rush W, Pihlstrom DJ, et al. ONJ in two dental practice-based research network regions. Journal of Dental Research. 2011 Apr;90(4):433–438. doi: 10.1177/0022034510387795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang TI, Tanner JM, Harada ND, Garrett NR, Friedlander AH. Prevalence of calcified carotid artery atheromas on the panoramic images of patients with syndrome Z, coexisting obstructive sleep apnea, and metabolic syndrome. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2012 Jan;113(1):134–141. doi: 10.1016/j.tripleo.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 29.Elter JR, White BA, Gaynes BN, Bader JD. Relationship of clinical depression to periodontal treatment outcome. Journal of Periodontology. 2002 Apr;73(4):441–449. doi: 10.1902/jop.2002.73.4.441. [DOI] [PubMed] [Google Scholar]
- 30.Ladrillo TE, Hobdell MH, Caviness AC. Increasing prevalence of emergency department visits for pediatric dental care, 1997–2001. Journal of the American Dental Association. 2006 Mar;137(3):379–385. doi: 10.14219/jada.archive.2006.0188. [DOI] [PubMed] [Google Scholar]
- 31.Luzzi L, Spencer AJ. Public dental service utilization among adults in South Australia. Australian Dental Journal. 2009 Jun;54(2):154–160. doi: 10.1111/j.1834-7819.2009.01109.x. [DOI] [PubMed] [Google Scholar]
- 32.Eikenberg S, Keeler R, Green T. Use of the Army Dental Command Corporate Dental Application as an electronic dental record in the Iraq theater of operations. US Army Medical Department Journal. 2011 Jan;:51–57. [PubMed] [Google Scholar]
- 33.Okunseri C, Bajorunaite R, Matthew R, Iacopino AM. Racial and ethnic variation in the provision of dental procedures. Journal of Public Health Dentistry. 2007;67(1):20–27. doi: 10.1111/j.1752-7325.2007.00004.x. [DOI] [PubMed] [Google Scholar]
- 34.Naegele ER, Cunha-Cruz J, Nadanovsky P. Disparity between dental needs and dental treatment provided. Journal of Dental Research. 2010 Sep;89(9):975–979. doi: 10.1177/0022034510369994. [DOI] [PubMed] [Google Scholar]
- 35.Caplan DJ, Weintraub JA. Factors related to loss of root canal filled teeth. Journal of Public Health Dentistry. 1997;57(1):31–39. doi: 10.1111/j.1752-7325.1997.tb02470.x. [DOI] [PubMed] [Google Scholar]
- 36.Caplan DJ, White BA. Clinical factors related to noncompletion of root canal therapy. Journal of Public Health Dentistry. 2001;61(1):6–13. doi: 10.1111/j.1752-7325.2001.tb03349.x. [DOI] [PubMed] [Google Scholar]
- 37.Caplan DJ, Kolker J, Rivera EM, Walton RE. Relationship between number of proximal contacts and survival of root canal treated teeth. International Endodontic Journal. 2002 Feb;35(2):193–199. doi: 10.1046/j.1365-2591.2002.00472.x. [DOI] [PubMed] [Google Scholar]
- 38.Stewart JE, Wager KA, Friedlander AH, Zadeh HH. The effect of periodontal treatment on glycemic control in patients with type 2 diabetes mellitus. Journal of Clinical Periodontology. 2001 Apr;28(4):306–310. doi: 10.1034/j.1600-051x.2001.028004306.x. [DOI] [PubMed] [Google Scholar]
- 39.Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. Journal of Prosthetic Dentistry. 2002 Mar;87(3):256–263. doi: 10.1067/mpr.2002.122014. [DOI] [PubMed] [Google Scholar]
- 40.Morgan JP, Minihan PM, Stark PC, Finkelman MD, Yantsides KE, Park A, et al. The oral health status of 4,732 adults with intellectual and developmental disabilities. Journal of the American Dental Association. 2012 Aug;143(8):838–846. doi: 10.14219/jada.archive.2012.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ram S, Teruel A, Kumar SK, Clark G. Clinical characteristics and diagnosis of atypical odontalgia: implications for dentists. Journal of the American Dental Association. 2009 Feb;140(2):223–228. doi: 10.14219/jada.archive.2009.0136. [DOI] [PubMed] [Google Scholar]
- 42.Alman AC, Johnson LR, Calverley DC, Grunwald GK, Lezotte DC, Harwood JE, et al. Loss of alveolar bone due to periodontal disease exhibits a threshold on the association with coronary heart disease. Journal of Periodontology. 2011 Sep;82(9):1304–1313. doi: 10.1902/jop.2011.100647. [DOI] [PubMed] [Google Scholar]
- 43.Meurman JH, Furuholm J, Kaaja R, Rintamaki H, Tikkanen U. Oral health in women with pregnancy and delivery complications. Clinical Oral Investigations. 2006 Jun;10(2):96–101. doi: 10.1007/s00784-006-0037-4. [DOI] [PubMed] [Google Scholar]
- 44.Jones JA, Miller DR, Wehler CJ, Rich SE, Krall-Kaye EA, McCoy LC, et al. Does periodontal care improve glycemic control? The Department of Veterans Affairs Dental Diabetes Study. Journal of Clinical Periodontology. 2007 Jan;34(1):46–52. doi: 10.1111/j.1600-051X.2006.01002.x. PM:17137468. [DOI] [PubMed] [Google Scholar]
- 45.Newton KM, Chaudhari M, Barlow WE, Inge RE, Theis MK, Spangler LA, et al. A population-based study of periodontal care among those with and without diabetes. Journal of Periodontology. 2011 Dec;82(12):1650–1656. doi: 10.1902/jop.2011.100609. [DOI] [PubMed] [Google Scholar]
- 46.Hyde JD, Bader JA, Shugars DA. Provisional crown failures in dental school predoctoral clinics. Journal of Dental Education. 2007 Nov;71(11):1414–1419. [PubMed] [Google Scholar]
- 47.Yamazaki T, Yamori M, Yamamoto K, Saito K, Asai K, Sumi E, et al. Risk of osteomyelitis of the jaw induced by oral bisphosphonates in patients taking medications for osteoporosis: A hospital-based cohort study in Japan. Bone. 2012 Nov;51(5):882–887. doi: 10.1016/j.bone.2012.08.115. [DOI] [PubMed] [Google Scholar]
- 48.Tami-Maury I, Willig J, Vermund S, Jolly P, Aban I, Hill J, et al. Contemporary profile of oral manifestations of HIV/AIDS and associated risk factors in a Southeastern US clinic. Journal of Public Health Dentistry. 2011;71(4):257–264. doi: 10.1111/j.1752-7325.2011.00256.x. [DOI] [PubMed] [Google Scholar]
- 49.Helenius-Hietala J, Aberg F, Meurman J, Isoniemi H. Increased infection risk postliver transplant without pretransplant dental treatment. Oral Disease. 2012 Jul 14; doi: 10.1111/j.1601-0825.2012.01974.x. [DOI] [PubMed] [Google Scholar]
- 50.Kidd AJ, Beattie TF, Campbell-Hewson G. Facial injury patterns in a UK paediatric population aged under 13 years. Emergency Medicine Journal. 2010 Aug;27(8):603–606. doi: 10.1136/emj.2009.075127. [DOI] [PubMed] [Google Scholar]
- 51.Sanders AE, Slade GD. Apgar score and dental caries risk in the primary dentition of five year olds. Australian Dental Journal. 2010 Sep;55(3):260–267. doi: 10.1111/j.1834-7819.2010.01232.x. [DOI] [PubMed] [Google Scholar]
- 52.Dissick A, Redman RS, Jones M, Rangan BV, Reimold A, Griffiths GR, et al. Association of periodontitis with rheumatoid arthritis: a pilot study. Journal of Periodontology. 2010 Feb;81(2):223–230. doi: 10.1902/jop.2009.090309. [DOI] [PubMed] [Google Scholar]
- 53.Tanner JM, Chang TI, Harada ND, Santiago SM, Weinreb JE, Friedlander AH. Prevalence of comorbid obstructive sleep apnea and metabolic syndrome: syndrome Z and maxillofacial surgery implications. Journal of Oral and Maxillofacial Surgery. 2012 Jan;70(1):179–187. doi: 10.1016/j.joms.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 54.Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. 2009 doi: 10.1001/jama.2009.1186. [DOI] [PubMed] [Google Scholar]
- 55.Leroy R, Eaton KA, Savage A. Methodological issues in epidemiological studies of periodontitis – how can it be improved. BMC Oral Health. 2010;10(8) doi: 10.1186/1472-6831-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schleyer T, Spallek H, Hernandez P. A qualitative investigation of the content of dental paper-based and computer-based patient record formats. Journal of American Medical Informatics Association. 2007;14:515–526. doi: 10.1197/jamia.M2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schleyer TKL. Collecting research data from clinical practice: how can informatics help?; Presented at: I International Conference on Biodental Engineering; Porto, Portugal. Jun 26, 2009. 2009 Jun 27. [Google Scholar]
- 58.Nora Méray, Johannes BReitsma, Anita CJRavelli, Gouke JBonsel. Probabilistic record linkage is a valid and transparent tool to combine databases without a patient identification number. Journal of Clinical Epidemiology Volume 60. 2007 Sep;:883.e1–883.e11. doi: 10.1016/j.jclinepi.2006.11.021. Issue 9. [DOI] [PubMed] [Google Scholar]
- 59.Hujoel PP, Leroux BG, Selipsky H, White BA. Non-surgical periodontal therapy and tooth loss. A cohort study. Journal of Periodontology. 2000 May;71(5):736–742. doi: 10.1902/jop.2000.71.5.736. [DOI] [PubMed] [Google Scholar]
- 60.Aquilino SA, Shugars DA, Bader JD, White BA. Ten-year survival rates of teeth adjacent to treated and untreated posterior bounded edentulous spaces. Journal of Prosthetic Dentistry. 2001 May;85(5):455–460. doi: 10.1067/mpr.2001.115248. [DOI] [PubMed] [Google Scholar]
- 61.Caplan DJ, Cai J, Yin G, White BA. Root canal filled versus non-root canal filled teeth: a retrospective comparison of survival times. Journal of Public Health Dentistry. 2005;65(2):90–96. doi: 10.1111/j.1752-7325.2005.tb02792.x. [DOI] [PubMed] [Google Scholar]
- 62.Shelley PQ, Johnson BR, BeGole EA. Use of an Electronic Patient Record system to evaluate restorative treatment following root canal therapy. Journal of Dental Education. 2007 Oct;71(10):1333–1339. [PubMed] [Google Scholar]
- 63.Leskinen K, Salo S, Suni J, Larmas M. Comparison of dental health in sealed and nonsealed first permanent molars: 7 years follow-up in practice-based dentistry. Journal of Dentistry. 2008;36:27–32. doi: 10.1016/j.jdent.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 64.Leskinen K, Salo S, Suni J, Larmas M. Practice-based study of the cost-effectiveness of fissure sealants in Finland. Journal of Dentistry. 2008;36:1074–1079. doi: 10.1016/j.jdent.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 65.Bassim CW, Gibson G, Ward T, Paphides BM, Denucci DJ. Modification of the risk of mortality from pneumonia with oral hygiene care. Journal of the American Geriatrics Society. 2008 Sep;56(9):1601–1607. doi: 10.1111/j.1532-5415.2008.01825.x. [DOI] [PubMed] [Google Scholar]
- 66.Iqbal M, Kurtz E, Kohli M. Incidence and factors related to flare-ups in a graduate endodontic programme. International Endodontic Journal. 2009 Feb;42(2):99–104. doi: 10.1111/j.1365-2591.2008.01461.x. [DOI] [PubMed] [Google Scholar]
- 67.George KM, Choi YG, Rieck KL, Van EJ, Ivancakova R, Carr AB. Immediate restoration with ti-unite implants: practice-based evidence compared with animal study outcomes. International Journal of Prosthodontics. 2011 May;24(3):199–203. [PubMed] [Google Scholar]
- 68.Worley DC, Thoele MJ, Asche SE, Godlevsky OV, Schmidt AM, Yardic RL, et al. A comparison of dental restoration outcomes after placement by restorative function auxiliaries versus dentists. Journal of Public Health Dentistry. 2012;72(2):122–127. doi: 10.1111/j.1752-7325.2011.00291.x. [DOI] [PubMed] [Google Scholar]
- 69.Kolhatkar S, Mason SA, Janic A, Bhola M, Haque S, Winkler JR. Surgical crown lengthening in a population with human immunodeficiency virus: a retrospective analysis) Journal of Periodontology. 2012;83(3):344–353. doi: 10.1902/jop.2011.110318. [DOI] [PubMed] [Google Scholar]
- 70.Ojima M, Hanioka T, Shizukuishi S. Survival analysis for degree of compliance with supportive periodontal therapy. Journal of Clinical Periodontology. 2001 Dec;28(12):1091–1095. doi: 10.1034/j.1600-051x.2001.281202.x. [DOI] [PubMed] [Google Scholar]
- 71.Okunseri C, Bajorunaite R, Mehta J, Hodgson B, Iacopino AM. Factors associated with receipt of preventive dental treatment procedures among adult patients at a dental training school in Wisconsin, 2001–2002. Gender Medicine. 2009 Apr;6(1):272–276. doi: 10.1016/j.genm.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 72.Kudiyirickal MG, Hollinshead F. Antimicrobial prescribing practice by dentists: a study from two primary care centres in UK. Minerva Stomatologica. 2011 Oct;60(10):495–500. [PubMed] [Google Scholar]
- 73.Chaudhari M, Hubbard R, Reid RJ, Inge R, Newton KM, Spangler L, et al. Evaluating Components of Dental Utilization among Adults with Diabetes and Matched Controls via Hurdle Models. BMC Oral Health. 2012 Jul 9;12(1):20. doi: 10.1186/1472-6831-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fouad AF, Burleson J. The effect of diabetes mellitus on endodontic treatment outcome: data from an electronic patient record. Journal of the American Dental Association. 2003 Jan;134(1):43–51. doi: 10.14219/jada.archive.2003.0016. [DOI] [PubMed] [Google Scholar]
- 75.Byrappagari D, Mascarenhas AK, Chaffin JG. Association of caries and tobacco risk with Dental Fitness Classification. Military Medicine. 2006 May;171(5):415–419. doi: 10.7205/milmed.171.5.415. [DOI] [PubMed] [Google Scholar]
- 76.Maupomé G, Peters D, Rush WA, Rindal DB, White BA. The relationship between cardiovascular xerogenic medication intake and the incidence of crown/root restorations. Journal of Public Health Dentistry. 2006;66(1):49–56. doi: 10.1111/j.1752-7325.2006.tb02551.x. [DOI] [PubMed] [Google Scholar]
- 77.Korhonen M, Salo S, Suni J, Larmas M. Computed online determination of life-long mean index values for carious, extracted, and/or filled permanent teeth. Acta Odontologica Scandinavica. 2007 Aug;65(4):214–218. doi: 10.1080/00016350701321466. [DOI] [PubMed] [Google Scholar]
- 78.Forsberg H, Sjodin L, Lundgren P, Wanman A. Oral health in the adult population of Vasterbotten, Sweden--a comparison between an epidemiological survey and data obtained from digital dental records. Swedish Dental Journal. 2008;32(1):17–25. [PubMed] [Google Scholar]
- 79.Friedlander AH, Tajima T, Kawakami KT, Wang MB, Tomlinson J. The relationship between measures of nutritional status and masticatory function in untreated patients with head and neck cancer. Journal of Oral and Maxillofacial Surgery. 2008 Jan;66(1):85–92. doi: 10.1016/j.joms.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 80.Tavares MC, Moyses ST, Moyses SJ, Bisinelli JC, Franca BH, Ribeiro FA. Dental caries protection factors in 5-year-old Brazilian children. Journal of Dentistry for Children. 2008 Sep;75(3):264–270. [PubMed] [Google Scholar]
- 81.Friedlander AH, Sung EC, Chung EM, Garrett NR. Radiographic quantification of chronic dental infection and its relationship to the atherosclerotic process in the carotid arteries. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics. 2010 Apr;109(4):615–621. doi: 10.1016/j.tripleo.2009.10.036. [DOI] [PubMed] [Google Scholar]
- 82.Spangler L, Reid RJ, Inge R, Newton KM, Hujoel P, Chaudhari M, et al. Cross-sectional study of periodontal care and Glycosylated Hemoglobin in an insured population. Diabetes Care. 2010 Aug;33(8):1753–1758. doi: 10.2337/dc09-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kassab MM, Radmer TW, Glore JW, Visotcky A, Robertson J, Degroot B. A retrospective review of clinical international normalized ratio results and their implications. Journal of the American Dental Association. 2011 Nov;142(11):1252–1257. doi: 10.14219/jada.archive.2011.0109. [DOI] [PubMed] [Google Scholar]
- 84.Mador MJ, Abo KM, Nag N, Mreyoud A, Jallu S, Mehboob S. Does sleep apnea increase the risk of cardiorespiratory complications during endoscopy procedures? Sleep & Breathing. 2011 Sep;15(3):393–401. doi: 10.1007/s11325-010-0346-3. [DOI] [PubMed] [Google Scholar]
- 85.Kudiyirickal MG, Hollinshead F. Clinical profile of orofacial infections: an experience from two primary care dental practices. Medicina Oral, Patologia Oral Y Cirugia Bucal. 2012 Feb 9;17(4):e533–e537. doi: 10.4317/medoral.17664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mosen DM, Pihlstrom DJ, Snyder JJ, Shuster E. Assessing the association between receipt of dental care, diabetes control measures and health care utilization. Journal of the American Dental. 2012 Jan;143(1):20–30. doi: 10.14219/jada.archive.2012.0014. [DOI] [PubMed] [Google Scholar]
- 87.Powell V, Leroux BG, Martin JA, White BA. Identification of adult populations at high risk for dental caries using a computerized database and patient records: a pilot project. Journal of Public Health Dentistry. 2000;60(2):82–84. doi: 10.1111/j.1752-7325.2000.tb03299.x. [DOI] [PubMed] [Google Scholar]
- 88.Morgan SK, Dumire W, Caudill C, Lewis A. Tracking Dental Patient Tobacco Use and Intervention in the Academic Clinical Setting. Journal of Dental Education. 2012;76(11):1448–1456. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.