Abstract
In the United States, livers for transplantation are distributed within donation service areas (DSAs). In DSAs with multiple transplant centers, competition among centers for organs and recipients may affect recipient selection and outcomes in comparison with DSAs with only 1 center. The objective of this study was to determine whether competition within a DSA is associated with posttransplant outcomes and variations in patients wait-listed within the DSA. United Network for Organ Sharing data for 38,385 adult cadaveric liver transplant recipients undergoing transplantation between January 1, 2003 and December 31, 2009 were analyzed to assess differences in liver recipients and donors and in posttransplant survival by competition among centers. The main outcome measures that were studied were patient characteristics, actual and risk-adjusted graft and patient survival rates after transplantation, organ quality as quantified by the donor risk index (DRI), wait-listed patients per million population by DSA, and competition as quantified by the Hirschman-Herfindahl index (HHI). Centers were stratified by HHI levels as no competition or as low, medium (or mid), or high competition. In comparison with DSAs without competition, the low-, mid-, and high-competition DSAs (1) performed transplantation for patients with a higher risk of graft failure [hazard ratio (HR) = 1.24, HR = 1.26, and HR = 1.34 (P < 0.001 for each)] and a higher risk of death [HR = 1.21, HR = 1.23, and HR = 1.34 (P < 0.001 for each)] and for a higher proportion of sicker patients as quantified by the Model for End-Stage Liver Disease (MELD) score [10.0% versus 14.8%, 20.1%, and 28.2% with a match MELD score of 31-40 (P < 0.001 for each comparison)], (2) were more likely to use organs in the highest risk quartile as quantified by the DRI [18.3% versus 27.6%, 20.4%, and 31.7% (P ≤ 0.001 for each)], and (3) listed more patients per million population [18 (median) versus 34 (P = not significant), 37 (P = 0.005), and 45 (P = 0.0075)]. Significant variability in patient selection for transplantation is associated with market variables characterizing competition among centers. These findings suggest both positive and negative effects of competition among health care providers.
In the United States, organs for transplantation are scarce resources. Patients on transplant lists are essentially in competition with one another through transplant centers, which represent the patients and commonly act as surrogate decision makers for the patients in decisions concerning patient and organ suitability. Transplant centers need to perform transplantation for patients at rates high enough to meet their fixed costs, to make incremental profits with each additional transplant, and to preserve their market share. These motives may conflict with decisions about the patients who should undergo transplantation, the best matching of organs with recipients, and, therefore, the best allocation of this scarce resource.
Under the current system for organ distribution employed in the United States, the national list is subdivided into regional and local units, and the local unit is called the donation service area (DSA). A DSA can be composed of 1 or more transplant centers; when there is more than 1 transplant center, the centers' patients are combined into a single list. When an organ becomes available, it is offered to patients ranked on a DSA list. In liver transplantation, the primary ranking of patients on these lists is done with the Model for End-Stage Liver Disease (MELD) score.1 Patients with the highest scores are at the greatest risk of death and are the first to be offered organs that are offered within a DSA. When a transplant center is the only member of its DSA, it has no competition for an organ if the organ is used in a patient with a MELD score greater than 15. In a DSA with more than 1 transplant center, competition exists among the centers for an organ, and this may affect the use of the organ in comparison with its use within a DSA without competition. This competition may affect patient and organ selection, and the degree of competition could lead to different decisions by transplant centers. In this article, we examine empirically the effects of transplant center competition within DSAs.
Patients and Methods
Data for adult deceased donor liver transplants between January 1, 2003 and December 31, 2009 were obtained from the United Network for Organ Sharing (through Standard Transplant Analysis and Research files created on March 31, 2011) to evaluate the risks of graft loss and patient death by competition. Transplants occurring at children's hospitals or at centers with fewer than 7 transplants during the study period (equivalent to less than 1 transplant per study year) were excluded from the study.
The Hirschman-Herfindahl index (HHI) was used to measure competition. The HHI for each DSA was calculated as the sum of the squares of market share for all centers within the DSA. The market share for a given center was defined as the proportion of liver transplants within the DSA performed at the given center from 2003 to 2009. The HHI was rescaled to 1 for this analysis. High HHI values indicated low competition, whereas low HHI values indicated high competition. We compared centers without competition to those with competition, but we segregated the latter into HHI tertiles to allow for comparisons between patients undergoing transplantation at centers with no competition (HHI = 1.00), low competition (HHI = 0.53-0.99), medium (or mid) competition (HHI = 0.38-0.52), or high competition (HHI < 0.38). The DSAs in New York, Ohio, and Tennessee were covered under statewide sharing agreements during the time of this study and were combined into single DSAs including all active centers in the states. Two centers, Oregon Health and Sciences University and the Portland Veterans Administration Medical Center, act as a single center and were regarded as a single center for this analysis. The number of active transplant centers fluctuated by the calendar year, with 14 centers initiating liver transplantation and 6 centers eliminating liver transplantation. The volume at new centers (median number of liver transplants in the first year = 4, range = 1-21) and closing centers (median number of liver transplants in the final year = 15, range = 6-21) was relatively small, and this suggested a limited volume of liver transplants at these centers. The small numbers of center transitions and patients limited the feasibility of evaluating any effects and were, therefore, not assessed.
Frequency distributions and medians (with interquartile ranges) for recipient and donor characteristics were compared by no competition, low competition (high HHI values), mid competition (intermediate HHI values), or high competition (low HHI values). The covariates included those significantly associated with 1-year graft survival in the Scientific Registry of Transplant Recipients (SRTR) report2: recipient age, previous abdominal surgery, life support, dialysis 2 times per week before transplantation, portal vein thrombosis, previous liver transplantation, recipient functional status, diagnosis at liver transplant, recipient albumin level, recipient creatinine level, donor age, donation after cardiac death, donor desmopressin, donor diuretics, liver type (partial/split or whole), cold ischemia time, donor height, and recipient hepatitis C virus diagnosis–donor age interaction [(donor age − 50)/10]. Also included were other relevant variables such as the match MELD score, hepatocellular carcinoma (HCC) exception status, insurance status, donor race, region, days on the wait list, length of stay after transplantation, and donor risk index (DRI).3 Differences and trends in recipient and donor characteristics across HHI levels were assessed with the chi-square test (categorical variables), the Wilcoxon rank-sum test (continuous variables), or the Cochran-Armitage trend test. We accounted for multiple comparisons across HHI levels with a Bonferroni-corrected P value (P < 0.008; Supporting Table 1).
The Kaplan-Meier method was used to estimate observed 1- and 3-year graft and patient survival rates by HHI levels. The posttransplant follow-up status and date were updated with data from the Social Security Death Certificate Master File for patients reportedly alive or lost to follow-up who also had a valid Social Security death date. The time to graft loss was measured in days from liver transplantation to patient death or retransplantation. The time to patient death was measured in days from liver transplantation to patient death. Patients alive or lost to follow-up were censored at the date of last follow-up (for graft and patient survival), and patients undergoing retransplantation were censored at the date of retransplantation (for patient survival). Survival differences by HHI levels were assessed with a log-rank test with Bonferroni-corrected P values. Univariate and adjusted hazard ratios (HRs) for posttransplant graft and patient survival were calculated for the different HHI levels with a Cox proportional hazards model. The multivariate HRs were adjusted for variables significantly associated with survival in the SRTR reports.
We evaluated center-level clustering in the multivariate model. When we accounted for clustering, the HR estimates for the HHI and the statistical significance of graft and patient survival by the HHI remained unchanged with 1 exception: the P value for patient survival in the mid-competition category increased to 0.06 (data not shown). We report here the multivariate model without center-level clustering.
We also examined DSA characteristics, including the HHI, the number of centers, and the transplant and listing practices. The number of liver transplants and the number of new listings per year at DSAs were calculated as means for the study years 2007-2009. Liver transplants and listings per year were adjusted per million population with 2008 census data. Census data for states with county population estimates were obtained from online US census data.4 Counties were assigned to the DSAs from the SRTR annual organ procurement organization report for the time period5 (Table 10 in that report was used for each organ procurement organization). Differences in DSA-level characteristics were compared across HHI levels with the Wilcoxon rank-sum test. All statistical analyses were conducted with SAS 9.2 (SAS, Inc., Cary, NC).
This research was considered exempt by the Committee on Human Research of the University of California San Francisco because no patient identifiers were provided in the Standard Transplant Analysis and Research files.
Results
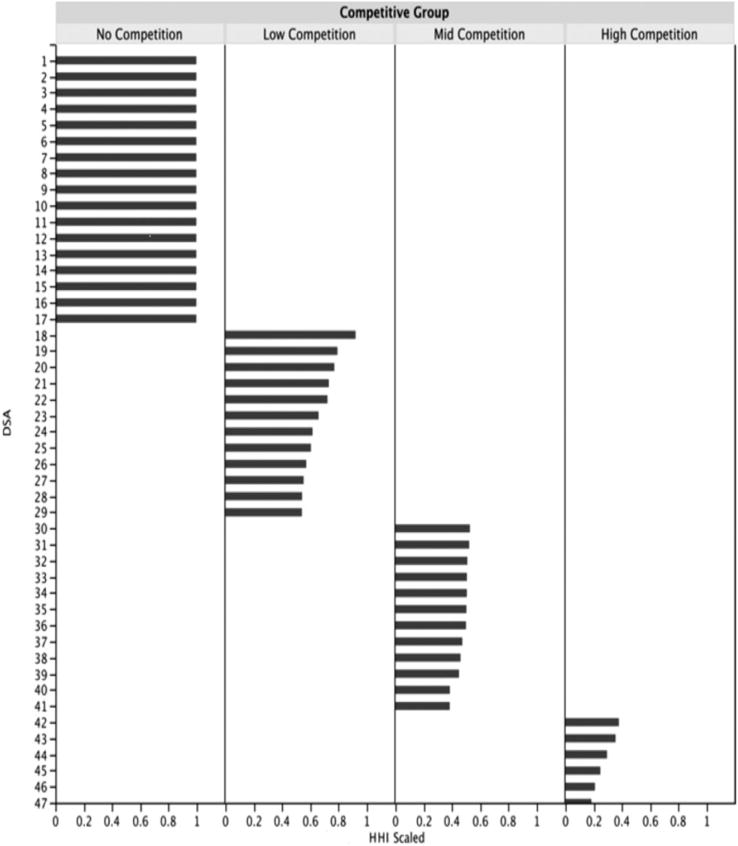
From 2003 to 2009, there were 38,385 transplants in 112 transplant centers, 47 DSAs, and 11 United Network for Organ Sharing regions. Two DSAs in New York, 3 DSAs in Ohio, and 2 DSAs in Tennessee were collapsed into single statewide DSAs, and 2 centers in Oregon were combined into a single center. A histogram of the DSAs by HHI values is shown in Fig. 1. In Table 1, we list descriptive statistics for the variables of interest and compare transplant patients by HHI levels. In comparison with transplant patients at centers without competition, a greater proportion of transplant patients at centers with low-, mid-, or high-competition levels were status 1; they were more likely to have match MELD scores greater than 20, HCC or non-HCC exceptions, dialysis in the week before transplantation, a previous liver transplant, life support, a functional status requiring total assistance, and higher albumin levels, and a lower proportion previously underwent abdominal surgeries. Transplant recipients at the mid- and high-competition levels had higher serum creatinine levels in comparison with recipients at the no-competition level. Donors at the low-, mid-, and high-competition levels were generally older (ie, there was a greater proportion of donors ≥ 60 years old) and included lower proportions of white donors, donors receiving desmopressin, and local organs and greater proportions of donors with DRIs in the upper quartile in comparison with donors at the no-competition level. Patients at the mid- and high-competition levels had greater proportions of partial/split liver transplants and lower proportions of grafts with cold ischemia times less than 9 hours in comparison with patients at the no-competition level. Because of the large number of transplants, relatively small differences may have been statistically significant. Clinically important differences were found in the percentages of patients undergoing transplantation with high MELD scores, with HCC, and on life support or dialysis, in the recipient functional status, in some of the components of the DRI (donor race, older donor age, share type, and cold ischemia time), and in the DRI itself.
Figure 1.
HHI distribution by DSAs and competitive groupings. The HHI (scaled) was calculated for each DSA. Competitive groups were designated as no competition or as low, mid, or high competition (by HHI tertile) for comparison.
Table 1. Characteristics of Liver Transplant Recipients and Donors (2003-2009) With Comparisons by HHI Levels.
| Characteristic | Total Population (n = 38,385) |
HHI Level | Comparison of HHI Levels: P Value | Trend: P Value |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| No Competition (n = 6613) |
Low Competition (n = 10,316) |
Mid Competition (n = 11,346) |
High Competition (n = 10,110) |
No Versus Low |
No Versus Mid |
No Versus High |
Low Versus Mid |
Low Versus High |
Mid Versus High |
|||
| Recipients | ||||||||||||
| Match MELD score (%) | ||||||||||||
| Status 1/1a/1b | 5.4 | 3.9 | 4.9 | 5.9 | 6.4 | 0.003 | <0.001 | <0.001 | 0.001 | <0.001 | 0.12 | <0.001 |
| 6-10 | 2.0 | 2.1 | 2.7 | 1.0 | 2.4 | 0.10 | <0.001 | 0.19 | <0.001 | 0.14 | <0.001 | 0.16 |
| 11-20 | 23.7 | 39.1 | 28.4 | 19.4 | 13.6 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 21-30 | 49.8 | 44.8 | 49.2 | 53.6 | 49.3 | <0.001 | <0.001 | <0.001 | <0.001 | 0.90 | <0.001 | <0.001 |
| 31-40 | 19.1 | 10.0 | 14.8 | 20.1 | 28.2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Other | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.75 | 0.90 | 0.12 | 0.62 | 0.03 | 0.06 | 0.02 |
| Active exception (%) | ||||||||||||
| No exception | 72.5 | 78.2 | 76.2 | 70.7 | 67.1 | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Yes, non-HCC | 7.6 | 4.4 | 5.9 | 9.6 | 9.0 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.15 | <0.001 |
| Yes, HCC | 19.9 | 17.3 | 17.9 | 19.7 | 23.9 | 0.37 | <0.001 | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 |
| Abdominal surgery (%) | 41.8 | 47.6 | 44.4 | 41.8 | 35.3 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Life support (%) | 7.0 | 4.4 | 6.5 | 8.7 | 7.2 | <0.001 | <0.001 | <0.001 | <0.001 | 0.05 | <0.001 | <0.001 |
| Dialysis (%) | 9.9 | 6.3 | 8.3 | 11.4 | 12.2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.06 | <0.001 |
| Previous transplant (%) | 8.0 | 6.5 | 8.7 | 8.2 | 7.9 | <0.001 | <0.001 | 0.001 | 0.20 | 0.04 | 0.39 | 0.05 |
| Functional status (%) | ||||||||||||
| No assistance | 46.8 | 49.6 | 48.9 | 46.1 | 43.8 | 0.32 | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 |
| Some assistance | 24.1 | 24.9 | 27.6 | 24.9 | 19.1 | <0.001 | 0.93 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Total assistance | 16.5 | 9.4 | 14.9 | 17.1 | 21.9 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Missing | 12.6 | 16.0 | 8.6 | 11.9 | 15.1 | <0.001 | <0.001 | 0.11 | <0.001 | <0.001 | <0.001 | 0.002 |
| Donors | ||||||||||||
| Age (%) | ||||||||||||
| <40 years | 45.2 | 48.8 | 44.5 | 47.7 | 40.8 | <0.001 | 0.16 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 40-49 years | 20.0 | 20.5 | 19.1 | 20.6 | 19.8 | 0.03 | 0.90 | 0.30 | 0.008 | 0.21 | 0.18 | 0.96 |
| 50-59 years | 19.1 | 19.0 | 19.1 | 18.6 | 19.6 | 0.87 | 0.44 | 0.32 | 0.29 | 0.35 | 0.44 | 0.46 |
| 60-69 years | 10.8 | 9.4 | 11.3 | 10.0 | 12.0 | <0.001 | 0.16 | <0.001 | 0.003 | 0.13 | <0.001 | <0.001 |
| >70 years | 5.0 | 2.3 | 6.0 | 3.2 | 7.8 | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Race (%) | ||||||||||||
| White | 67.9 | 77.7 | 65.3 | 68.5 | 63.6 | <0.001 | <0.001 | <0.001 | <0.001 | 0.01 | <0.001 | <0.001 |
| Black | 15.7 | 11.0 | 16.5 | 16.2 | 17.5 | <0.001 | <0.001 | <0.001 | 0.59 | 0.04 | 0.009 | <0.001 |
| Hispanic | 13.0 | 7.5 | 15.9 | 11.9 | 14.9 | <0.001 | <0.001 | <0.001 | <0.001 | 0.06 | <0.001 | <0.001 |
| Asian | 2.3 | 2.0 | 1.4 | 2.5 | 3.0 | 0.003 | 0.06 | <0.001 | <0.001 | <0.001 | 0.02 | <0.001 |
| Other | 1.1 | 1.8 | 0.9 | 0.9 | 1.0 | <0.001 | <0.001 | <0.001 | 0.98 | 0.83 | 0.84 | <0.001 |
| Desmopressin (%) | 26.0 | 33.9 | 26.3 | 21.6 | 25.3 | <0.001 | <0.001 | <0.001 | <0.001 | 0.10 | <0.001 | <0.001 |
| Partial/split liver (%) | 1.4 | 0.7 | 1.1 | 1.4 | 2.1 | 0.01 | <0.001 | <0.001 | 0.02 | <0.001 | <0.001 | <0.001 |
| Cold ischemia time (%) | ||||||||||||
| <9 hours | 67.9 | 72.0 | 71.1 | 67.9 | 61.7 | 0.22 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 9-11.9 hours | 17.2 | 17.9 | 18.3 | 13.4 | 19.8 | 0.46 | <0.001 | 0.003 | <0.001 | 0.009 | <0.001 | 0.52 |
| >12 hours | 6.5 | 4.8 | 7.2 | 5.1 | 8.6 | <0.001 | 0.39 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Missing | 8.4 | 5.3 | 3.4 | 13.5 | 10.0 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Share type (%) | ||||||||||||
| Local | 70.8 | 78.6 | 63.8 | 71.8 | 71.6 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.71 | 0.01 |
| Regional | 22.9 | 17.4 | 29.7 | 26.2 | 15.9 | <0.001 | <0.001 | 0.02 | <0.001 | <0.001 | <0.001 | <0.001 |
| National | 6.3 | 4.1 | 6.4 | 1.9 | 12.5 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| DRI quartiles (%) | ||||||||||||
| 1 (<1.12) | 25.4 | 33.3 | 22.7 | 27.9 | 20.4 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 2 (>1.12-1.37) | 24.7 | 24.6 | 24.3 | 26.9 | 22.8 | 0.62 | 0.001 | 0.006 | <0.001 | 0.01 | <0.001 | 0.10 |
| 3 (>1.37-1.68) | 24.9 | 23.8 | 25.4 | 24.9 | 25.2 | 0.02 | 0.09 | 0.04 | 0.40 | 0.66 | 0.69 | 0.17 |
| 4 (>1.68) | 24.9 | 18.3 | 27.6 | 20.4 | 31.7 | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| MELD score of 31-40 and DRI > 1.68 (%) | 3.6 | 1.8 | 2.8 | 3.2 | 6.2 | <0.001 | 0.001 | <0.001 | 0.05 | <0.001 | <0.001 | <0.001 |
| Days on wait list* | 63 (14-230) | 46 (12-153) | 49 (13-175) | 69 (14-267) | 98 (18-306) | 0.02 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Albumin (g/dL)* | 2.9 (2.4-3.4) | 2.8 (2.4-3.3) | 3.0 (2.5-3.4) | 2.9 (2.4-3.4) | 2.9 (2.4-3.4) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.35 | 0.03 |
| Creatinine* | 1.1 (0.8-1.7) | 1.1 (0.8-1.5) | 1.1 (0.8-1.6) | 1.16 (0.8-1.8) | 1.18 (0.8-2.0) | 0.86 | <0.001 | <0.001 | <0.001 | <0.001 | 0.12 | <0.001 |
| Donor height (cm)* | 173 (165-180) | 173 (165-180) | 173 (165-180) | 173 (165-180) | 171 (165-178) | <0.001 | 0.005 | <0.001 | 0.05 | <0.001 | <0.001 | <0.001 |
| Length of stay (days)* | 10 (7-18) | 9 (7-15) | 10 (7-18) | 11 (7-19) | 10 (7-19) | <0.001 | <0.001 | <0.001 | <0.001 | 0.03 | 0.005 | <0.001 |
NOTE: Some groups of percentages do not add up to exactly 100 because of rounding. To account for multiple comparisons, only P < 0.008 was considered statistically significant.
The data are presented as medians and interquartile ranges.
We examined the data to determine the degree of elasticity of the data. Using P trends, we found evidence of trends for oldest patient age, MELD scores (except for 6-10), exception scores (HCC and non-HCC), life support, dialysis, recipient functional status, multiple DRI factors, and highest and lowest DRI scores.
Table 2 documents the effects of univariate and adjusted multivariate HRs for the risks of graft failure and patient death by HHI levels. The risks of graft failure and patient death were significantly elevated at the low-, mid-, and high-competition levels in comparison with the no-competition level. Despite adjustments for the variables significantly associated with graft survival in the SRTR center-specific reports, the HRs for graft failure and patient death remained significantly different from the HRs of the centers without competition, and this suggested unaccounted-for variance. The matching of high-DRI organs (defined as the upper quartile of transplanted organs with a DRI > 1.68) with recipients with high MELD scores (defined as MELD scores of 31-40) increased with competition [1.8% with no competition, 2.8% with low competition, 3.2% with mid competition, and 6.2% with high competition, P ≤ 0.001 for all comparisons except for low competition versus mid competition (P = 0.05)]. However, this was not independently associated with graft (P = 0.62) or patient survival (P = 0.09) in the multivariate analysis.
Table 2. Univariate and Adjusted Multivariate HRs for the Risks of Graft Failure and Patient Death After Liver Transplantation by HHI Levels.
| HHI Level | Univariate Analysis | Multivariate Analysis* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Risk of Graft Failure | Risk of Patient Death | Risk of Graft Failure | Risk of Patient Death | |||||||||
|
|
|
|
|
|||||||||
| HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | |
| No competition (1.00) | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Low competition (0.53-0.99) | 1.24 | 1.17-1.32 | <0.001 | 1.21 | 1.13-1.29 | <0.001 | 1.17 | 1.11-1.24 | <0.001 | 1.15 | 1.08-1.23 | <0.001 |
| Mid competition (0.38-0.52) | 1.26 | 1.19-1.34 | <0.001 | 1.23 | 1.16-1.32 | <0.001 | 1.18 | 1.11-1.25 | <0.001 | 1.13 | 1.06-1.21 | <0.001 |
| High competition (<0.38) | 1.34 | 1.26-1.42 | <0.001 | 1.34 | 1.26-1.43 | <0.001 | 1.17 | 1.10-1.24 | <0.001 | 1.17 | 1.09-1.25 | <0.001 |
Adjusted for recipient age, previous abdominal surgery, life support, dialysis, portal vein thrombosis, previous liver transplantation, functional status, diagnosis, donor age, donation after cardiac death, donor desmopressin, donor diuretics, partial/split liver, cold ischemia time, albumin level, creatinine level (logarithm), donor height, and recipient hepatitis C virus diagnosis-donor age interaction [(donor age − 50)/10].
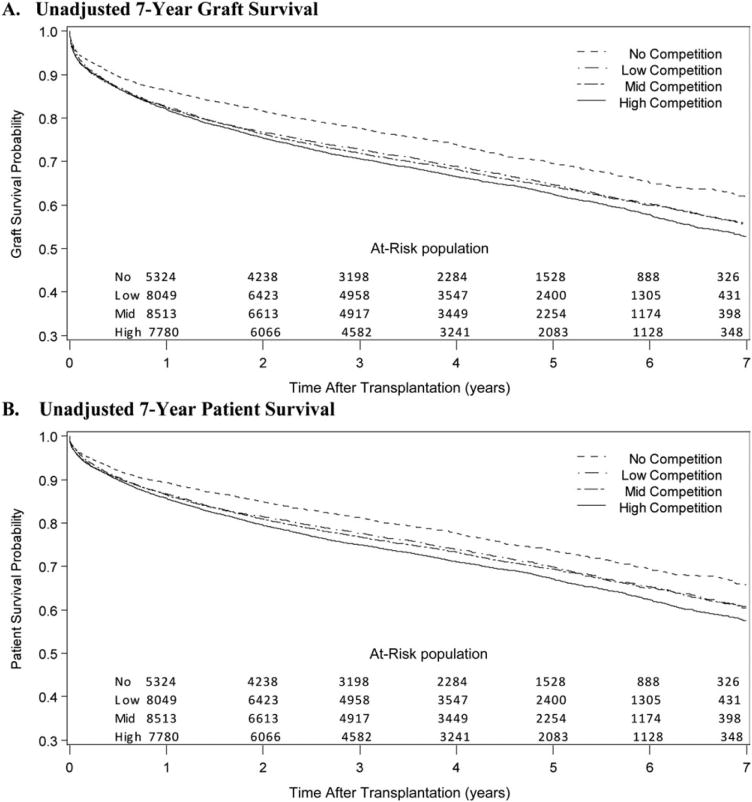
Figure 2 depicts unadjusted 7-year graft and patient survival. Overall, there was a decrease in the observed graft and patient survival with more competition. The observed 3-year graft and patient survival rates were significantly lower at the low-, mid-, and high-competition levels in comparison with the no-competition level (P < 0.001).
Figure 2.
Comparison of (A) observed graft survival and (B) observed patient survival after liver transplantation by the HHI level.
Table 3 demonstrates the DSA categorization by the HHI. The median listings per million population in DSAs differed by the degree of competition within DSAs, with DSAs without competition having significantly fewer listings per million population in comparison with DSAs with mid- and high-competition levels.
Table 3. Characteristics of DSAs Within Each HHI Level.
| DSA Characteristic | HHI Level | Comparison of HHI Levels: P Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| No Competition (17 DSAs) |
Low Competition (12 DSAs) |
Mid Competition (12 DSAs) |
High Competition (6 DSAs) |
No Versus Low |
No Versus Mid |
No Versus High |
Low Versus Mid |
Low Versus High |
Mid Versus High |
|
| HHI | 1.00 (1.00-1.00) | 0.64 (0.56-0.75) | 0.50 (0.46-0.51) | 0.27 (0.21-0.36) | <0.001 | <0.001 | <0.001 | <0.001 | 0.004 | 0.004 |
| Transplant centers per DSA | 1 (1-1) | 2 (2-2) | 3 (2-4) | 6 (5-6) | <0.001 | <0.001 | <0.001 | 0.15 | 0.003 | 0.02 |
| Liver transplants: 2003-2009 | 355 (158-588) | 778 (501-1157) | 818 (593-1142) | 1573 (1197-1739) | 0.10 | 0.002 | 0.002 | 0.55 | 0.03 | 0.03 |
| Liver transplants per year: 2007-2009 | 55 (28-84) | 112 (65-168) | 130 (93-189) | 227 (182-235) | 0.009 | 0.001 | 0.002 | 0.38 | 0.02 | 0.04 |
| Liver transplants per year per million* | 14 (11-20) | 18 (16-27) | 20 (17-26) | 19 (18-20) | 0.10 | 0.04 | 0.23 | 0.69 | 0.89 | 0.52 |
| New listings for liver transplantation: 2003-2009 | 573 (283-792) | 1318 (882-1860) | 1481 (1132-1796) | 3414 (3048-4171) | 0.002 | <0.001 | 0.002 | 0.48 | 0.004 | 0.01 |
| New listings for liver transplantation per year: 2007-2009 | 86 (44-118) | 186 (103-249) | 226 (166-268) | 575 (422-588) | 0.004 | <0.001 | 0.002 | 0.31 | 0.005 | 0.01 |
| New listings for liver transplantation per year per million* | 18 (16-28) | 34 (26-44) | 37 (30-43) | 45 (35-52) | 0.02 | 0.005 | 0.0075 | 0.78 | 0.18 | 0.19 |
Note: The data are presented as medians and Interquartile ranges.
Liver transplants and new listings for liver transplantation were estimated as the mean for calendar years 2007 to 2009. Estimates were adjusted with 2008 census data.
Discussion
When we consider competition among transplant centers, we assume that transplant centers desire to perform more liver transplants (ie, gain market share) because of the advantages gained by performing transplants. The presence of more than 1 transplant center in a DSA increases competition among centers for patients and organs, both of which are necessary for gaining market share. Because livers are allocated to the patients on the list by the ranking of their degree of illness (as captured by the MELD score), increased competition would be expected to be associated with higher MELD scores at transplantation. These patients with high MELD scores are more likely to be on life support and on dialysis and to have a worse functional status. Patients with these characteristics have been shown to have higher costs associated with transplantation and lower survival rates after transplantation.6,7
Another center strategy for increasing transplantation is to use organs associated with a higher risk of graft failure as measured by the DRI. The use of higher DRI organs is associated with higher transplant costs and worse recipient outcomes.8 It has also been shown recently that higher DRI organs in patients with higher MELD scores is associated with increased costs.9 A recent article demonstrated that multiple centers in an organ procurement organization were associated with the use of higher DRI organs, but a measure of market share was not used.10
We have examined the trends of donor and recipient characteristics (see Table 1). The results suggest an elasticity of the effect, particularly in the characteristics by which competition would affect donor and recipient selection at the margin. We cannot argue that there is not some level of a threshold effect, particularly when one is going from no competition to any competition, but there does remain evidence of an association with the HHI, that is, increasing levels of competition and changes in patient and donor selection.
The behavior of performing transplantation for higher risk patients and using higher DRI organs is associated with a decrease in the expected survival of patients at centers with increased competition. When there is no competition, a center may not benefit from performing transplantation with higher DRI organs for patients with higher MELD scores because of the costs associated with this strategy. Because transplant centers typically receive a fixed payment for a transplant from Medicare and private health care payers, a lower cost for transplantation would increase the profits of transplantation. This strategy may result in lower listings per million population by centers without competition, as we have noted in Table 3.
Table 2 documents an association between the level of competition and the HRs of graft and patient survival. The fact that the variables used in the SRTR survival analyses do not account for all of the variance associated with competition is unexpected, and it suggests that unaccounted-for patient, donor, or center characteristics affect these outcomes. One potential explanation is that when there is 1 transplant center per DSA, the transplant center will have all the patients on the list and can turn down an organ for a patient higher on the list if there is the perception of better donor and recipient matching with a patient further down the list without any concern about losing the organ for transplantation to a competitive center. When there are multiple transplant centers per DSA, if a center declines an offer for a patient, this may lead to a competitor using the organ and result in an incremental decrease in the number of transplants at the first center. This ability for a center without competition to match donor and recipient characteristics may be reflected in an unmeasured donor-recipient interaction term that affects patient and graft survival.
The presented findings suggest an association between competition (as measured by the HHI) and certain characteristics of patients who are listed and undergo transplantation within a DSA. This does not prove that competition causes the effect but proves only that there is a relationship.
Our finding that the adjusted patient and graft survival rates are lower in DSAs with more competition may be confounded by a number of factors, such as unmeasured donor and recipient characteristics, interactions between donor and recipient characteristics, and differences in medical care.
Competition between liver transplant centers may be looked at in both positive and negative lights. One positive aspect is that competition is associated with increased patient access for sicker patients, who derive the greatest benefit from transplantation. According to the listings per million population, there also appears to be greater access for patients in these DSAs to transplantation. Another positive aspect is that there appears to be increased utilization of higher risk organs by centers in competitive DSAs. Because higher risk organs continued to be discarded in the United States, this usage can be viewed as positive. A negative aspect is that transplantation for higher risk patients and the use of higher risk organs are associated with higher costs, and there is the question whether competition decreases the ability of a center to better match donor and recipient characteristics. Where the correct balance of these positive and negative effects of competition lies is unclear. Competition has been advocated as important for bettering market performance, but these findings suggest that there may be limits to the value of competition in the health care setting.
Supplementary Material
Abbreviations
- CI
confidence interval
- DRI
donor risk index
- DSA
donation service area
- HCC
hepatocellular carcinoma
- HHI
Hirschman-Herfindahl index
- HR
hazard ratio
- MELD
Model for End-Stage Liver Disease
- SRTR
Scientific Registry of Transplant Recipients
Footnotes
No authors of this research have any potential conflicts of interest such as relevant financial interests, activities, relationships, or affiliations.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Freeman RB, Jr, Wiesner RH, Roberts JP, McDiarmid S, Dykstra DM, Merion RM. Improving liver allocation: MELD and PELD. Am J Transplant. 2004;4(suppl 9):114–131. doi: 10.1111/j.1600-6135.2004.00403.x. [DOI] [PubMed] [Google Scholar]
- 2.Scientific Registry of Transplant Recipients. Deceased donor graft survival model description 1 year (and 1 month) after transplant. Organ: liver. Adult (age 18+) [Accessed October 2012];Transplants between 07/01/2008 and 12/31/2010. http://srtr.org/csr/current/modtabs.aspx.
- 3.Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783–790. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 4.United States Census Bureau. Vintage. [Accessed October 2012];national tables. 2008 http://www.census.gov/popest/data/historical/2000s/vintage_2008/index.html.
- 5.Scientific Registry of Transplant Recipients. OPO-specific reports. [Accessed October 2012]; http://www.srtr.org/opo/Default.aspx.
- 6.Dutkowski P, Oberkofler CE, Béchir M, Müllhaupt B, Geier A, Raptis DA, Clavien PA. The Model for End-Stage Liver Disease allocation system for liver transplantation saves lives, but increases morbidity and cost: a prospective outcome analysis. Liver Transpl. 2011;17:674–684. doi: 10.1002/lt.22228. [DOI] [PubMed] [Google Scholar]
- 7.Åberg F, Maklin S, Räsänen P, Roine RP, Sintonen H, Koivusalo AM, et al. Cost of a quality-adjusted life year in liver transplantation: the influence of the indication and the Model for End-Stage Liver Disease score. Liver Transpl. 2011;17:1333–1343. doi: 10.1002/lt.22388. [DOI] [PubMed] [Google Scholar]
- 8.Axelrod DA, Schnitzler M, Salvalaggio PR, Swindle J, Abecassis MM. The economic impact of the utilization of liver allografts with high donor risk index. Am J Transplant. 2007;7:990–997. doi: 10.1111/j.1600-6143.2006.01724.x. [DOI] [PubMed] [Google Scholar]
- 9.Salvalaggio PR, Dzebisashvili N, MacLeod KE, Lentine KL, Gheorghian A, Schnitzler MA, et al. The interaction among donor characteristics, severity of liver disease, and the cost of liver transplantation. Liver Transpl. 2011;17:233–242. doi: 10.1002/lt.22230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Volk ML, Reichert HA, Lok AS, Hayward RA. Variation in organ quality between liver transplant centers. Am J Transplant. 2011;11:958–964. doi: 10.1111/j.1600-6143.2011.03487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.