Abstract
Background
Headache is one of the most common symptoms in primary care. Most headaches are due to primary headaches and many headache sufferers do not receive a specific diagnosis. There is still a gap in research on how GPs diagnose and treat patients with headache.
Aim
To identify GPs’ diagnostic approaches in patients presenting with headache.
Design and setting
Qualitative study with 15 GPs in urban and rural practices.
Method
Interviews (20–40 minutes) were conducted using a semi-structured interview guideline. GPs described their individual diagnostic strategies by means of patients presenting with headache that they had prospectively identified during the previous 4 weeks. Interviews were taped and transcribed verbatim. Qualitative analysis was conducted by two independent raters.
Results
Regarding GPs’ general diagnostic approach to patients with headache, four broad themes emerged during the interviews: ‘knowing the patient and their background’, ‘first impression during consultation’, ‘intuition and personal experience’ and ‘application of the test of time’. Four further themes were identified regarding the management of diagnostic uncertainty: ‘identification of red flags’, ‘use of the familiarity heuristic’, ‘therapeutic trial’, and ‘triggers for patient referral’.
Conclusion
GPs apply different strategies in the early diagnostic phase when managing patients with headache. Identification of potential adverse outcomes accompanied by other strategies for handling uncertainty seem to be more important than an exact diagnosis. Established guidelines do not play a role in the diagnostic workup.
Keywords: diagnosis, general practice, headache, qualitative research
INTRODUCTION
Headache is one of the most common symptoms in primary care1–3 and can lead to relevant reduction of health-related quality of life for the individual patient.4 Most patients experience primary headaches which includes, according to the International Classification of Headache Disorders (ICHD), migraine, tension-type headache, trigeminal autonomic cephalgias, and other primary headache disorders.5 Patients with headache reflect a broad spectrum of symptom frequency and severity and the vast majority of patients is managed in the primary care setting.2,6,7
There are conflicting views on the importance of an exact diagnosis in patients with headache. While it is stressed that headache treatment needs to be tailored to an exact diagnosis8 and several authors see knowledge deficits in GPs concerning the diagnosis and management of headache,9,10 others question the relevance of an exact diagnosis in the primary care setting as in most patients headache is of benign and self-limiting origin.7
There is still little evidence on how GPs diagnose patients with headache11 and about how they make decisions during the further workup of these patients.7,12 There has also been a call for wider use of qualitative methods, especially in headache research, that can contribute to the already existent quantitative data and to shed more light on the issues mentioned above.13
This study analyses the early diagnostic phase of the decision-making process, where in many instances no specific diagnosis (like tension-type headache or migraine) is reached. It explores how GPs manage patients presenting with headache and which strategies they use to handle diagnostic uncertainty. An additional study explored how, in a second step, GPs reach a definite diagnosis in some of the patients.14
METHOD
Study design
A qualitative research approach was used to address the study question and to gain a deeper insight into GPs’ unique experiences, strategies, heuristics, and interpretations of their findings when dealing with patients with headache.13 Single interviews were chosen as the most appropriate technique for data collection, as it created the best environment to talk to each GP about their own individual diagnostic strategies.
Setting and data collection
Fifteen GPs in the federal states of Hessen, Bavaria and North Rhine Westphalia (Germany) were approached. GPs were recruited via personal contacts and among GPs affiliated with the University department. GPs were contacted in advance, given an explanation of the aim of the study and they gave written permission for inclusion in the study. A flexible interview guide was designed based on recent literature on headache in primary care. It was explained to the GPs that the study was about understanding how they managed patients with headache, and what role intuition, clinical experience, and diagnostic uncertainty played in their daily routine with these patients. To elucidate their diagnostic approaches, the participating GPs were asked to collect information on every patient presenting with headache in their practice during the following 4 weeks. After these 4 weeks a second appointment for the interview was arranged. The collected patient data were exclusively used by the GPs to aid recall during the interview (‘stimulated recall’),15 but were not presented to the interviewer.
How this fits in
GPs use a broad range of diagnostic strategies in the workup of patients with headache. GPs found it more important to have effective strategies for handling uncertainty than to make an exact diagnosis.
The semi-structured interview began with a question about the overall number of patients and the diagnoses collected by the respective GP. Afterwards, GPs were invited to recall the consultation of these patients. A semi-structured interview guideline was used to cover all relevant topics (history taking, examination and further diagnostic investigations, identification of red flags, GPs diagnostic strategies and individual heuristics, and dealing with uncertainty). Participants were asked about central aspects of clinical history and physical examination, the use of scores or any other (also individual) algorithms that helped GPs in the differential diagnosis of their specific cases. Additionally, the authors were interested in determining what GPs thought about the role of intuition and gut feeling. GPs’ reflections on their diagnostic reasoning or individual diagnostic strategies concluded the interview. Interviews were arranged at the GPs’ convenience and lasted between 20–40 minutes each.
Data analysis
Interviews were taped and transcribed verbatim. To assist data handling, the material was transcribed and analysed using MAXQDA-10. A content analytic approach was applied and, based on the interview guideline, a coding system (coding tree) was deductively developed as a first step. The coding tree and coding were tested and refined within the study qualitative working group. All interviews were coded by two independent raters; differences in coding were resolved by discussion. In an iterative process inductively derived new codes and themes were added to the coding tree. Emerging concepts and themes were repeatedly discussed and refined by all authors in regular meetings.
In summary, this analysis can be categorised as a thematic survey, executed stepwise, with each step informing the next.16,17 Interviews were conducted in the German language, translated into English, and crosschecked by a native speaker for both languages.
RESULTS
Sample characteristics
Nineteen GPs from urban and rural areas were approached and four declined participation. Table 1 shows the characteristics of the 15 interviewed GPs.
Table 1.
GP characteristics (n = 15)
| Sex | |
| Male | 8 |
| Female | 7 |
|
| |
| Years of clinical experience | |
| <10 | 3 |
| 10–20 | 8 |
| >20 | 4 |
|
| |
| Practice location | |
| Urban | 4 |
| Sub-urban | 7 |
| Rural | 4 |
Diagnostic approach to patients with headache
Regarding the general diagnostic approach to patients with headache, four broad themes emerged during the interviews.
Knowing the patient and their background
Most participants mentioned the crucial and central meaning of the long-term relationship that most GPs have with their patients. In-depth knowledge of the whole context of a patient’s extended family, sometimes reaching back several generations, was assigned an especially high diagnostic value:
‘I am glad that I know many families over several generations. This is very helpful ... especially in patients that present repeatedly with similar symptoms.’
(A14, §70–71)
First impression during consultation
Nearly all GPs mentioned that the first patient impression triggers several thoughts regarding the differential diagnosis of headache. Although GPs judged the overall diagnostic relevance of this process differently, most agreed that the first impression:
‘… is crucial regarding the decision on what I will do with this patient and on what further diagnostic procedures I will initiate.’
(A14, §38)
It was not deemed so relevant ‘what’ the patient was saying but ‘how’ this occurred. The patient’s posture, facial expression, gestures, or intonation were important clues in the diagnostic process for many GPs:
‘The posture and facial expression, and how the patient behaves, give the first essential clues, […] How he describes [the problem] leads to a first idea on what may lie behind it.’
(A 13, §22+46)
Intuition and personal experience
GPs said they intuitively knew the right diagnosis without having tangible criteria to prove that they were right in several instances. Many interviewees stressed that this gut feeling emerged from a combination of long-term contact with individual patients and increasing personal professional experience in dealing with patients with headache:
‘Like in many other instances, you need a little bit of gut feeling [laughs] … or one could also more elegantly characterise it as intuition. This you do not have from the first day, this just grows.’
(A7, §50)
Application of the test of time
In many instances GPs did not make a specific diagnosis like tension-type headache or migraine. To reach a specific diagnosis was even often considered as less relevant. After exclusion of red flags, virtually all GPs used the course of time as a diagnostic tool as:
‘... most headaches go as they came.’
(A4, §102)
‘With some [headaches] one can wait, and only if certain alarm signals occur, then something has to happen immediately. […] Time heals. It applies to many people that time fixes a lot.’
(A12, §36+70)
Almost all GPs considered this process of watchful waiting not as careless, but on the contrary as more sensible and appropriate than immediately starting with further extensive diagnostic procedures.
Dealing with diagnostic uncertainty
When asking GPs how they manage diagnostic uncertainty, four further themes emerged.
Identification of red flags
Identification of red flags helped GPs make an early decision for referral. Most GPs asked and looked systematically for these signs and symptoms. Neurological symptoms and the quality and time pattern of pain (sudden, new, or excruciating) were the most frequently mentioned red flags:
‘I had a patient who had cavernous sinus thrombosis. She complained of a headache, and what puzzled me, was that she could no longer hit the keys properly on her mobile phone … Another patient had a brain tumour, he came in and said that he had dropped things out of his hand that morning.’
(A8, §28+86)
Figure 1 shows a summary of the different red flags mentioned by the interviewed GPs.
Figure 1.
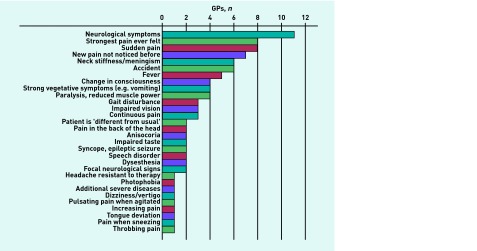
Different red flags for headache mentioned by GPs.
Use of the familiarity heuristic
When dealing with diagnostic uncertainty, six of the 15 doctors mentioned that they try to determine whether the patient is familiar with their pain and symptoms. Familiarity on the patients’ side reduced uncertainty on the GPs’ side, while new and unfamiliar symptoms increased the physicians’ awareness:
‘If the patient takes it seriously, then it is serious. The patients who say “this is something I know, this is how it always is” … tend to reassure me.’
(A4, §36)
‘I had a patient […] who knew his headaches, but the pain character was completely new to him […] … this worried him a lot and was the reason he came to me. […] In the end he had basilar artery thrombosis.’
(A14, §12)
Therapeutic trial
In some cases, most GPs used therapeutic trials to reach a diagnosis. The patient’s response to therapy was considered to be helpful in reducing uncertainty, as it reduced the chance of an underlying serious disease:
‘When I encounter somebody with a headache during out-of-hours service, he receives paracetamol when there are no neurological deficits… and I say “ok” […]. When he [the patient] comes back the next day saying “the pill helped a great deal” you have a great clue, and if not, you start a further diagnostic workup.’
(A6, §98)
Figure 2 summarises the different approaches applied by GPs to use therapy for diagnostic purposes.
Figure 2.
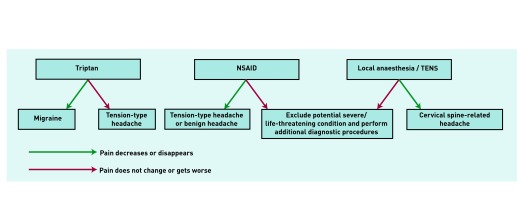
GPs’ approaches to use of therapy for diagnostic purposes in patients presenting with headache. The first row shows the different strategies applied by GPs; the arrows indicate whether the patient shows a positive or negative response to it. Boxes in the second row show the resulting diagnostic conclusions of the next steps taken by GPs.
Triggers for patient referral
While the identification of red flags helped GPs reduce acute diagnostic uncertainty, referral was used to control the remaining diagnostic uncertainty. Specialists were normally only consulted if therapy initiated by the GPs did not show any signs of success and/or symptoms did not resolve after applying the test of time:
‘As I said, if therapy is unsuccessful or the diagnosis is questionable, and I say to myself “hmm, this could be something different”, then I’ll refer to a specialist.’
(A3, §112)
Figure 3 summarises different quotes made by the interviewees with regard to indications for specialist referral.
Figure 3.
Indications for specialist referral in patients with headache.
None of the interviewed GPs used established guidelines for the diagnosis of headache, neither in the early diagnostic phase, where uncertainty had to be handled, nor at a later point when a specific diagnosis was obtained for selected patients:
Interviewer: ‘You don’t use any guidelines”?
GP: ‘No.’
(A2, §63)
‘Our problem is […] that guideline-medicine is born […] out of hospital experience […]. And this presents a big dilemma for our basic patient care […]. They [the specialists] create things […] that cannot be applied to daily practice in a meaningful way.’
(A1, §70)
DISCUSSION
Summary
GPs’ diagnostic management of patients presenting with headache were identified. In the general diagnostic workup, a long-term relationship with the patient and their family, along with the first impression gained during consultation combined with intuition and the GPs’ personal experience, all played important roles. GPs also frequently used the test of time. GPs reduced diagnostic uncertainty by early identification of red flags, usage of the familiarity heuristic or a therapeutic trial and by identifying triggers for patient referral.
Strengths and limitations
The data presented have limitations; for example, another way to capture doctors’ diagnostic reasoning, such as videotaped interviews, may have more internal validity, however, this method is difficult to implement in a primary care setting. Using standardised patients would have been a possible alternative. Although feasible, this approach would not have captured the diagnostic significance of long-term relationships between GPs and their patients, and the GPs reasoning about the chosen diagnostic approach. The current study was conducted in German and the transcript translation into English may have resulted in some distortion of the original meaning. In an attempt to minimise this effect, the manuscript was corrected by a native English speaker with a medical background. Finally, these findings relate to the specific context of the German health system, which has high patient contact rates with both GPs and specialists, and lacks specific guidelines for the diagnosis and management of headache in primary care.
The strength of this study lies in the prospective identification of patients used in the interview, which allowed examination of the diagnostic process in a defined clinical situation. However, it is not possible to rule out that GPs reinterpreted their diagnostic arguments afterwards or tried to change first intuitional diagnostic hypotheses into more rational thoughts during the interview. This kind of bias was minimised by encouraging GPs to give their very own individual accounts of diagnostic methods and strategies, stressing the lack of primary care research in this area to create an atmosphere of open and self-critical reflection. The study sample is largely representative of general practice in Germany.
Comparison with existing literature
GPs stressed the importance of the long-term relationship with the patient, often including their extended family. Other studies confirm that previous knowledge about an individual patient and the systematic attention to the contextual issues of the consultation helps in the diagnostic workup.18,19 This contextual information feeds into both analytical and non-analytical diagnostic reasoning.20
Most GPs regarded the first patient impression as an important element. Studies mainly conducted with simulated patients showed how different patient characteristics influenced physician’s behaviour.21,22 Wilm et al showed that the affective components of female patients’ presentation of their headache to male GPs resulted in significantly more costly further investigations in comparison to neutral or anxious patients.23
GPs additionally stressed the role of intuition and personal experience. Stolper et al confirm the important role of gut feelings together with analytical reasoning and personal experience in GPs’ diagnostic reasoning.20 The initial steps of the diagnostic process are often non-analytical or intuitive24 before, in a further step, one or several hypotheses are generated.25 This process is reflected in these data.
In many instances GPs did not make a specific diagnosis. Most headaches were considered of benign nature responding to symptomatic therapy. Consequently, GPs used the test of time as a diagnostic tool after exclusion of red flags. These findings are supported by a retrospective analysis of a large primary care database, in which 70% of adult patients with new-onset headache were not given a diagnostic label.11 The relevance of a precise headache diagnosis in primary care patients is debatable,7 as many headache episodes will disappear spontaneously, or with rather generic treatment. The time-efficiency principle is considered a core diagnostic strategy in low-prevalence settings, and safely as well as efficiently reduces the number of patients who need to be formally tested to make a correct or specific diagnosis for a given person.26,27
In dealing with diagnostic uncertainty, all GPs screened their patients for certain red flags and some of the GPs applied the familiarity heuristic. The aforementioned red flags largely corresponded with warning signs for secondary headache mentioned in guidelines.28 Adapted heuristics, often based on the principle of familiarity versus discrepancy, are widely used in primary care,29 and there is support for the relevance of the familiarity heuristic in suspected secondary headache disorders.30,31
Most GPs used a therapeutic trial in certain patients. A positive response was judged as an indicator for primary headache and reduced diagnostic uncertainty. The test of treatment is a well-established principle in primary care,27 although spontaneous patient recovery and placebo effects can lead to bias.32 While tension-type headache normally does not respond to triptans,33 a response to individual triptans in patients with migraine is idiosyncratic,28 and a negative treatment result can therefore be misleading. In addition, the test of treatment approach could trigger the continued use of over-the-counter drugs and could go along with a higher risk of medication-overuse headache.
Implications for practice
This study’s findings underline the need for further guidance in the workup of patients with headache. This may be in the form of effective strategies for handling uncertainty including guidance on specialist referral or the development of simple guidelines that allow making an exact diagnosis in the specific context of primary care.
In conclusion, GPs use a broad range of strategies to manage patients with headache. Effective strategies for handling uncertainty are more important than an exact diagnosis. Established guidelines do not play a role in the diagnostic workup.
Acknowledgments
We thank all the participating GPs for their cooperation.
Funding
The study received no external funding.
Ethical approval
The study protocol was approved by the Ethics Committee of the Faculty of Medicine, University of Marburg (AZ 192/09).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Morrell DC. Symptom interpretation in general practice. J R Coll Gen Pract. 1972;22(118):297–309. [PMC free article] [PubMed] [Google Scholar]
- 2.Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. J Neurol Neurosurg Psychiatry. 2006;77(3):385–387. doi: 10.1136/jnnp.2005.073221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ponka D, Kirlew M. Top 10 differential diagnoses in family medicine: headache. Can Fam Physician. 2007;53(10):1733. [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon GD, Skobieranda FG, Gragg LA. Quality of life and well-being of patients with headache: measurement by the medical outcomes study instrument [abstract] Headache. 1993;33(7):351–358. doi: 10.1111/j.1526-4610.1993.hed3307351.x. [DOI] [PubMed] [Google Scholar]
- 5.The International Classification of Headache Disorders. Cephalalgia. 2013;33(9):629–808. doi: 10.1177/0333102413485658. 3rd ed (beta version) [DOI] [PubMed] [Google Scholar]
- 6.Charles J, Ng A, Britt H. Presentations of headache in Australian general practice. Aust Fam Physician. 2005;34(8):618–619. [PubMed] [Google Scholar]
- 7.O’Flynn N, Ridsdale L. Headache in primary care: how important is diagnosis to management? Br J Gen Pract. 2002;52(480):569–573. [PMC free article] [PubMed] [Google Scholar]
- 8.Pryse-Phillips WE, Dodick DW, Edmeads JG, et al. Guidelines for the diagnosis and management of migraine in clinical practice. Canadian Headache Society. CMAJ. 1997;156(9):1273–1287. [PMC free article] [PubMed] [Google Scholar]
- 9.Diego EV de, Lanteri-Minet M. Recognition and management of migraine in primary care: influence of functional impact measured by the headache impact test (HIT) Cephalalgia. 2005;25(3):184–190. doi: 10.1111/j.1468-2982.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 10.Khu JV, Siow HC, Ho KH. Headache diagnosis, management and morbidity in the Singapore primary care setting: findings from a general practice survey. Singapore Med J. 2008;49(10):774–779. [PubMed] [Google Scholar]
- 11.Kernick D, Stapley S, Hamilton W. GPs’ classification of headache: is primary headache underdiagnosed? Br J Gen Pract. 2008;58(547):102–104. doi: 10.3399/bjgp08X264072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ridsdale L. ‘I saw a great star, most splendid and beautiful’: headache in primary care. Br J Gen Pract. 2003;53(488):182–184. [PMC free article] [PubMed] [Google Scholar]
- 13.Peters M, Abu-Saad HH, Vydelingum V, Murphy M. Research into headache: the contribution of qualitative methods. Headache. 2002;42(10):1051–1059. doi: 10.1046/j.1526-4610.2002.02238.x. [DOI] [PubMed] [Google Scholar]
- 14.Bösner S. Diagnostische Strategien bei Patienten Diagnostische Strategien bei Patienten mit Kopfschmerz in der Hausarztpraxis — eine qualitative Untersuchung [Diagnostic strategies in headache patients seen in primary care — a qualitative study] Z Allg Med. 2014;90(7):36–42. [Google Scholar]
- 15.Elstein A, Shulman L, Sprafka S. Medical problem solving: an analysis of clinical reasoning. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- 16.Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qual Health Res. 2003;13(7):905–923. doi: 10.1177/1049732303253488. [DOI] [PubMed] [Google Scholar]
- 17.Kuckartz U. Einführung in die computergestützte Analyse qualitativer Daten. 3rd ed. Wiesbaden: VS, Verl. für Sozialwiss; 2010. [Introduction in computer aided analysis of qualitative data] [Google Scholar]
- 18.Donner-Banzhoff N. Wie stellt der Allgemeinarzt eine Diagnose? [How does the general practitioner make a diagnosis?] Z Allg Med. 1999;75:744–749. [Google Scholar]
- 19.Lykke K, Christensen P, Reventlow S. ‘This is not normal …‘ — signs that make the GP question the child’s well-being. Fam Pract. 2008;25(3):146–153. doi: 10.1093/fampra/cmn021. [DOI] [PubMed] [Google Scholar]
- 20.Stolper E, van de Wiel M, van Royen P, et al. Gut feelings as a third track in general practitioners’ diagnostic reasoning. J Gen Intern Med. 2011;26(2):197–203. doi: 10.1007/s11606-010-1524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hooper EM, Comstock LM, Goodwin JM, Goodwin JS. Patient characteristics that influence physician behavior. Med Care. 1982;20(6):630–638. doi: 10.1097/00005650-198206000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Gerbert B. Perceived likeability and competence of simulated patients: influence on physicians’ management plans. Soc Sci Med. 1984;18(12):1053–1059. doi: 10.1016/0277-9536(84)90164-3. [DOI] [PubMed] [Google Scholar]
- 23.Wilm S, Brockmann S, Spannaus-Sakic C, et al. Machen Hausärzte Unterschiede, wenn sie mit Kopfschmerzpatienten umgehen? Eine Querschnittsstudie mit ängstlich oder neutral gespielten standardisierten Patienten [Variation in General practitioners’ performance towards patients with acute headache] Z Allg Med. 2008;84(07):273–279. [Google Scholar]
- 24.Norman G, Young M, Brooks L. Non-analytical models of clinical reasoning: the role of experience. Med Educ. 2007;41(12):1140–1145. doi: 10.1111/j.1365-2923.2007.02914.x. [DOI] [PubMed] [Google Scholar]
- 25.Norman G, Barraclough K, Dolovich L, Price D. Iterative diagnosis. BMJ. 2009;339:b3490. doi: 10.1136/bmj.b3490. [DOI] [PubMed] [Google Scholar]
- 26.Irving G, Holden J. The time-efficiency principle: time as the key diagnostic strategy in primary care. Fam Pract. 2013;30(4):386–389. doi: 10.1093/fampra/cmt007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heneghan C, Glasziou P, Thompson M, et al. Diagnostic strategies used in primary care. BMJ. 2009;338:b946. doi: 10.1136/bmj.b946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diagnosis and management of headache in adults: a national clinical guide. Edinburgh: Scottish Intercollegiate Guidelines Network; 2008. Scottish Intercollegiate Guidelines Network. [Google Scholar]
- 29.Andre M, Borgquist L, Foldevi M, Molstad S. Asking for ‘rules of thumb’: a way to discover tacit knowledge in general practice. Fam Pract. 2002;19(6):617–622. doi: 10.1093/fampra/19.6.617. [DOI] [PubMed] [Google Scholar]
- 30.Cady R, Dodick DW. Diagnosis and treatment of migraine. Mayo Clin Proc. 2002;77(3):255–261. doi: 10.4065/77.3.255. [DOI] [PubMed] [Google Scholar]
- 31.Salander P, Bergenheim AT, Hamberg K, Henriksson R. Pathways from symptoms to medical care: a descriptive study of symptom development and obstacles to early diagnosis in brain tumour patients. Fam Pract. 1999;16(2):143–148. doi: 10.1093/fampra/16.2.143. [DOI] [PubMed] [Google Scholar]
- 32.Glasziou P, Rose P, Heneghan C, Balla J. Diagnosis using ‘test of treatment’. BMJ. 2009;338:b1312. doi: 10.1136/bmj.b1312. [DOI] [PubMed] [Google Scholar]
- 33.Bendtsen L. Review: Drug and nondrug treatment in tension-type headache. Ther Adv Neurol Disord. 2009;2(3):155–161. doi: 10.1177/1756285609102328. [DOI] [PMC free article] [PubMed] [Google Scholar]



