Abstract
Objectives:
The present study assesses the accuracy of three-dimensional (3D) cone beam CT (CBCT) and intra-oral radiography (CR) in visualizing peri-implant bone compared with histology.
Methods:
26 titanium dental implants were placed in dog jaws with chronic type vestibular defects. After a healing period of 2 and 8 weeks (n = 12 dogs) the animals were sacrificed. CBCT scans and CR of the specimen were recorded. Dissected blocks were prepared, and histomorphometric analysis was performed. Both modalities were measured twice by two observers and compared with histomorphometry regarding bone levels and thickness around implants as well as length and diameter of implants.
Results:
Measurements of CBCT correlated well with histomorphometry of the vestibular bone level, oral bone thickness and implant length (all p-values <0.05). Compared with histomorphometry, the mean differences between CBCT and histomorphometry were between 0.06 and 2.61 mm. Mesial bone level (MBL) and distal bone level (DBL) were underestimated by both CR and CBCT. CR and histology measurements were only significantly correlated for implant length measurements. All intraclass correlations were highly significant.
Conclusions:
3D CBCT provides usable information about bone in all dimensions around implants with varying accuracy. CR and CBCT perform similar in assessing MBL and DBL, but, within its limits, the CBCT can assess oral and buccal bone. Metallic artefacts limit the visualization quality of bone around implants and further research could elucidate the value of post-processing algorithms. When information about osseous perforation of implants is needed, CBCT may still provide clinically valuable information.
Keywords: cone beam computed tomography, dental implants, digital intra-oral radiographs, osseo-integration
Introduction
Osseous destruction as a result of periodontal disease or peri-implantitis is an increasing problem in the long-term treatment of implant patients. Monitoring periodontal changes, such as vertical bone defects surrounding oral or vestibular aspects of the tooth or implants, remains a challenge for clinical examination, but is, however, essential.1,2 X-rays are frequently applied to visualize anatomic structures like alveolar bone.3 Conventional intra-oral radiographs (CRs) show interproximal alveolar bone levels,4 but three-dimensional (3D) information in oro-vestibular direction is projected onto the two-dimensional (2D) radiographs and therefore is not accessible.5,6 CR suffers from its inherent 2D nature, with anatomical superposition and geometric distortion, limiting the visibility of, for example, intra-osseous defects and their changes over time.7,8 CR measures have proven to estimate the marginal bone level closer to reality when compared with clinical probing in an animal study.9 In cases of vestibular or lingual bone defects, CR provides very limited information owing to its projection method.2,10 The lack of three-dimensional (3D) information in CR hinders distinction between the vestibular and lingual cortical plate and complicates the evaluation of periodontal bone defects.11 Even when high-quality images are produced, CR has been shown to underestimate mild-to-moderate bone loss.12 To improve the sensitivity of CR in detecting marginal bone loss, digital subtraction radiography has been evaluated but not reached common practice.13 Reasons for that might be technical barriers and still limited visualization of oral bone levels (OBLs) and vestibular bone levels (VBLs). To assess the true 3D configuration of periodontal defects and concurrently bone defects, devices powering 3D image information could be useful.6
Until the introduction of cone beam CT (CBCT), 3D visualization of hard tissue in maxillofacial radiology was dominated by CT.14 CT provides high-contrast 3D visualization of bone beds; however, several drawbacks have been met. The high dose absorbed by the patients narrow the use of CT.14 Monitoring bone loss around dental implants is deemed impossible since artefacts caused by the metallic character of implants disguise information around implants.
As a fairly new method of visualizing peri-implant bone, MRI has been proposed. Senel et al15 reported the successful application of MRI for evaluating vertical bone increase after sinus lift procedures. However, no reports exist about horizontal bone loss.
Another technology for visualizing periodontal bone was tuned-aperture CT (TACT). In vitro studies showed that TACT is capable of visualizing periodontal bone and, compared with digital subtraction radiography, it is even superior.16 The first clinical investigations showed a statistically significant preference of TACT over 2D control images.17 However, in clinical practice, TACT has not found significant dissemination.
Since the introduction of CBCT in 1998, indications for this imaging method include implant site assessment, temporomandibular joint examination, visualization of periodontal osseous situation and identification of periodontal ligament spaces.5,18–20
Compared with CT, radiation exposure to the patient is generally lower in CBCT. This technique uses isotopic voxels of a size down to 0.08 mm.6,14 Additionally, metallic artefacts are less severe in CBCT than in CT.
The clinical value of CBCT for monitoring peri-implantitis is currently unknown. As a first step towards answering this question, the aim of the present study is to evaluate the diagnostic accuracy for assessing peri-implant osseo-integration using CBCT, CR and the histology of dogs.
Methods and material
Study design
This study reports on a supplementary radiological analysis of selected tissue biopsies obtained from a previous experimental study employing a total of 12 fox hounds exhibiting a fully erupted permanent dentition.21 The original study protocol was approved by the Animal Care and Use Committee of the Heinrich Heine University, Düsseldorf, Germany, and the local government of Düsseldorf (approval number 8.87-50.10.34.08.089). Along with this study, we also investigated the accuracy of CBCT in measuring peri-implant bone defect regeneration.22 In the study described in this article, we focus on non-augmented sites and also on the radiological accuracy in comparison with CR.
Surgical procedure
The surgical procedures and anaesthesia protocol have been reported in detail previously.21 In brief, the study consisted of three surgical phases. During the first surgical phase, the second, third and fourth pre-molar and both molars were bilaterally extracted from the lower jaws. After 3 months, the second surgical phase started with the creation of standardized vestibular bone defects. After a chronification period of 4 weeks, four titanium implants per specimen were placed and left to heal in a submerged position. The animals were killed after 2 and 8 weeks, including six animals each.
Retrieval of specimens
The jaws were dissected and blocks with the average size of 8 cm containing the experimental specimens were obtained and fixed in 4% formaldehyde solution. For the present radiological analysis, a total of n = 26 non-augmented defect sites were selected at random (Figure 6).
Figure 6.
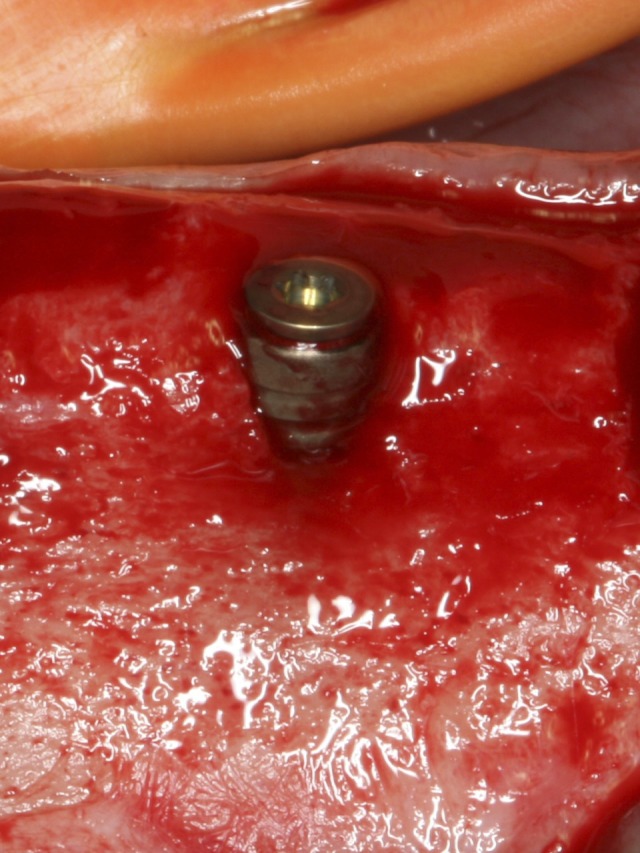
Clinical image of the implant site.
Radiological modes
The blocks containing the experimental specimens were retained in hermetic closable plastic boxes filled with 4% formaldehyde solution to prevent dehydration. Digital CRs within this study were performed with HELIODENTPLUS (60 kV, 7 mAs; Sirona Dental Systems, Bensheim, Germany). An orthoradial ray path was used as the basic calibration in all examinations to position the longitudinal axis of the implants similar to human teeth in clinical situation. All CRs were performed with XIOSPLUS intra-oral sensor (Sirona Dental Systems), which is an active pixel sensor (CMoS-APS) with a resolution of 16.7 mm−1 line pairs. SIDEXIS XG (Sirona Dental Systems) was used as the imaging software.
The radiographs by CBCT were made before jaw dissection as described previously with an imaging system named GALILEOS (Sirona Dental Systems). Within this study, all scans were conducted with manufacturer-suggested standard expose settings (85 kV, 28 mAs and normal contrast mode). Prior to that different exposure settings were evaluated and found not useful owing to over- or underexposure, which was attributed to the original intended use of the machine for human diagnostics. The current of the X-ray source was 7 mAs for all scans. Each scan took 14 s and was reconstructed in 0.3-mm isotropic voxels from 200 raw projections. The volume matrix consisted of 512 × 512 × 512 voxels. The specimens were positioned with the longitudinal axis in the CBCT similar to the longitudinal axis of human teeth, to simulate clinical proceeding. The specimens were stored in a tray containing the fixation solution for CBCT scanning. The specimens were removed from the tray for taking intra-oral radiographs.
Proprietary software named GALAXIS (Sirona Dental Systems) was used to visualize the data.
All CRs and CBCT scans were saved in Windows Bitmap (BMP) format. CRs were exported using the inherent export function of Sidexis (Sirona Dental Systems GmbH). No compression was used. Images had 8 bits and 564 dots per inch (Figure 1).
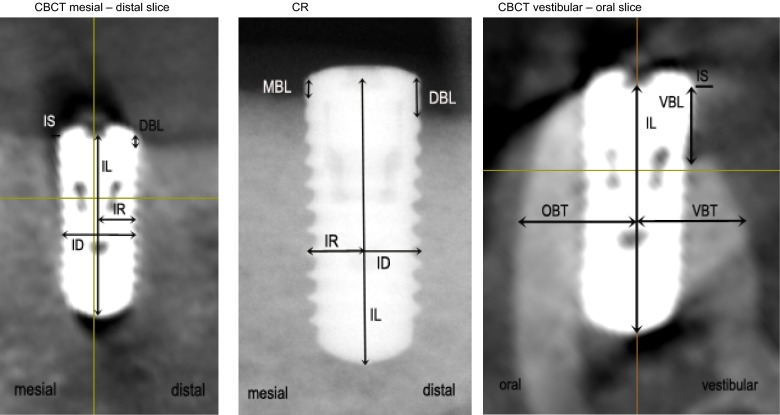
Figure 1.
Data preparation of cone beam CT (CBCT) slices and intra-oral radiographs (CRs). DBL, distal bone level; ID, implant diameter; IL, implant length; IR, implant radius; IS, implant shoulder; MBL, mesial bone level; OBT, oral bone thickness; VBL, vestibular bone level; VBT, vestibular bone thickness.
Data preparation
26 CBCT scans, in each case a demonstration of axial, longitudinal and transversal images, and 26 CRs were measured using ImageJ (Wayne Rasband, National Institutes of Health, Bethesda, MD). To evaluate all images in one common software environment, images were imported into ImageJ. Measurements for CRs were calibrated using the known implant length (IL).
The following measuring points were set: implant shoulder in the mesial, distal, vestibular and oral directions and landmarks for evaluation of the vestibular bone thickness and oral bone thickness (OBT), 4 mm from apical. Supplementary information as mesial (m) and vestibular (v) were inserted in the images. Subsequently, the calibrated scans were analysed in ImageJ to present for evaluation. All radiological images were assessed twice under standardized conditions at the examiners' workplace by two observers. Ambient light conditions were present and a 19-inch thin-film transistor display with a resolution of 1280 × 1024 pixels, brightness of 280 cd m−2 and contrast of 1000:1 were used (Fujitsu Siemens Scenicview P19-2; Fujitsu, Kawasaki, Japan). Examiners were allowed to adjust brightness and contrast, so they could subjectively get the best image presentation. All histological images were measured once by one observer. All hardware components were technically approved for radiological diagnosis by German authorities.
Histological preparation
Histological preparation has been reported in detail previously.21 In brief, ascending grades of alcohol and xylene were used to dehydrate the experimental specimens. For non-decalcified sectioning, the blocks were infiltrated and embedded in methylmethacrylate (Technovit® 9100 NEW; Heraeus Kulzer, Wehrheim, Germany). During a controlled polymerization time of 20 h, the specimens were stored at −4 °C environmental temperature, to exclude any negative impact as polymerization heat. Serial sections with a final thickness of 40 μm were prepared from the respective implant sites in the vestibular–oral direction. For the present analysis, additional mesial or distal sections were prepared.
Histomorphometrical analysis
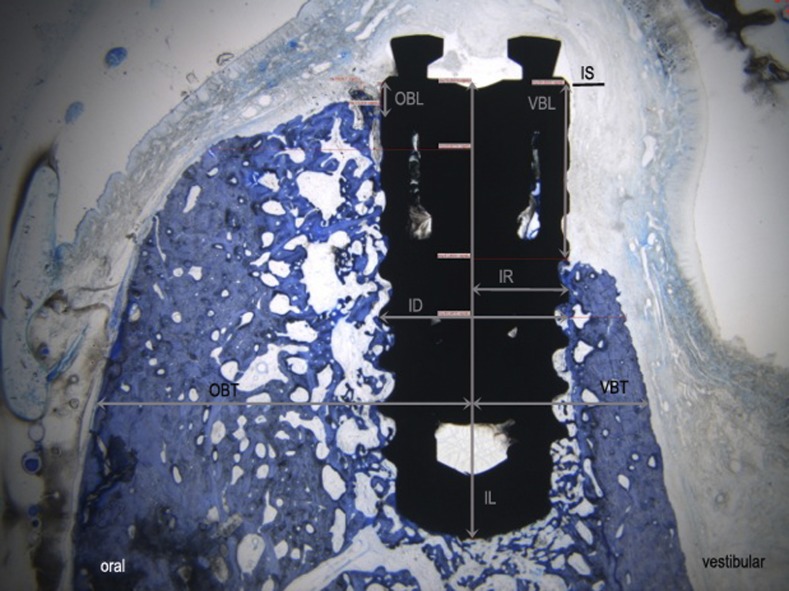
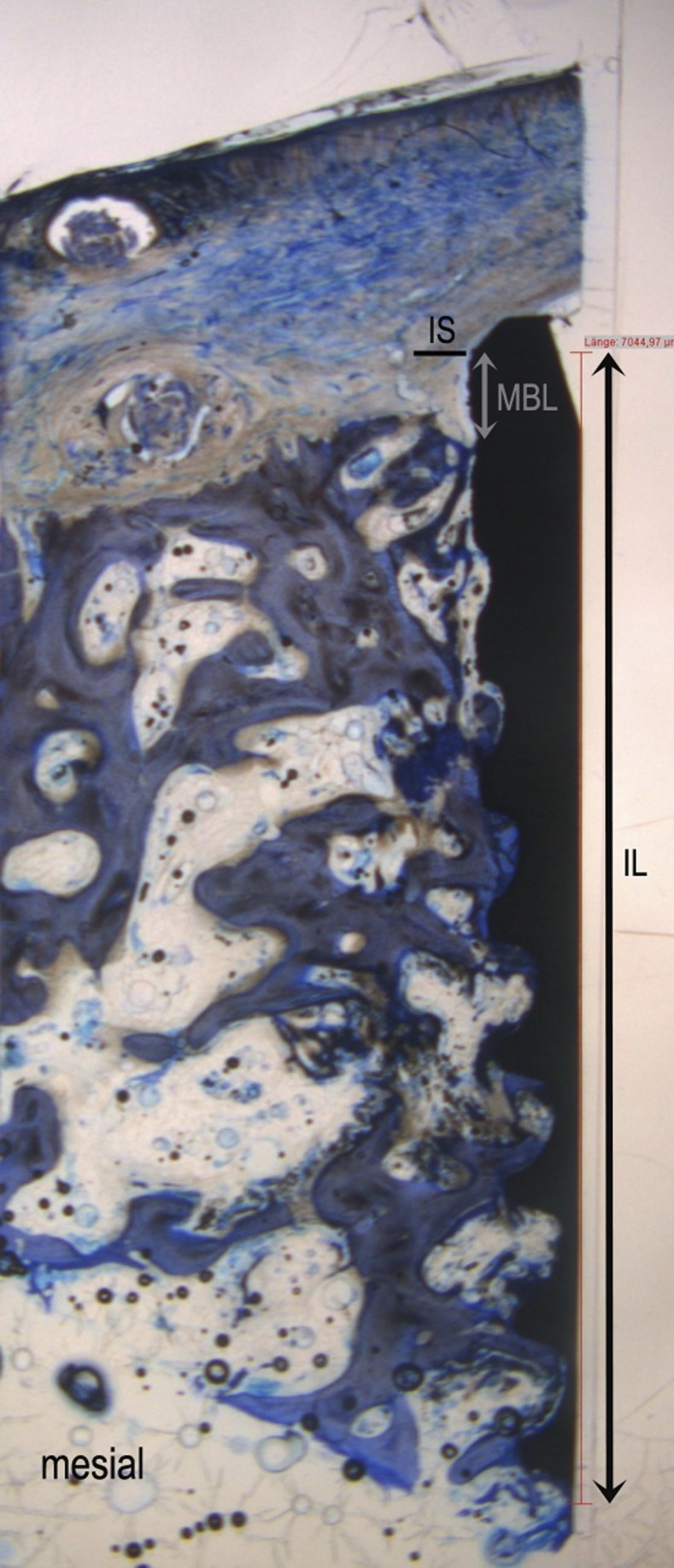
A colour charge-coupled device camera (Color View III; Olympus, Hamburg, Germany) was used for image sourcing. It was assembled on a binocular light microscope (Olympus BX50; Olympus, Hamburg, Germany). The digital images were evaluated using a software program (Cell D; Soft Imaging System, Münster, Germany), which was calibrated before the procedure started. The following landmarks were identified in the histological specimen: the implant diameter, the implant radius, the IL, the most coronal contact point of bone and implant in mesial, distal, vestibular and oral directions and the VBT and OBT in the horizontal direction. Defect length was measured from implant shoulder to the bone level (millimetre). The horizontal bone beds were evaluated in the vestibular and oral directions, 4 mm from apical, measured from the middle of the implant (Figures 2 and 3).
Figure 2.
Histological image in vestibulo-oral direction. ID, implant diameter; IL, implant length; IR, implant radius; IS, implant shoulder; OBL, oral bone level; OBT, oral bone thickness; VBL, vestibular bone level; VBT, vestibular bone thickness.
Figure 3.
Histological image in mesiodistal direction. IL, implant length; IS, implant shoulder; MBL, mesial bone level.
Statistical analysis
The statistical analysis was performed with SPSS® v. 21 for Macintosh (IBM Corporation, Armonk, NY). One-sample Kolmogorov–Smirnov test was used to test for normality of distribution of the collected data. Paired-samples t-tests were applied to test for differences of measured values. Intra- and interclass correlation coefficients were calculated for each parameter to assess the reliability of measurements. The significance level is set at p = 0.05.
Results
All measured values followed a normal distribution according to one-sample Kolmogorov–Smirnov tests. The intraclass correlation coefficient was used to estimate the reliability of measurements and the variability of the observer. Intraclass correlation for Examiner 1 ranged on average for the different measurements from 0.72 to 0.99. For Examiner 2, it ranged from 0.76 to 1.0. Interclass correlation coefficient was between 0.92 and 1.00 for the different items. The interitem correlation of all measured values was between 0.87 and 1.00 (p < 0.01). Statistically significant conformity could be assessed for vestibular bone level CBCT1 and CBCT2, vestibular bone thickness CBCT1 and CBCT2, oral bone level CBCT1 and CBCT2, OBT CBCT1 and CBCT2, IL CBCT1 and CBCT2, and implant diameter CBCT1 and CBCT2 (all p-values <0.01). Statistically significant conformity could also be assessed for all tested parameters in the mesiodistal direction.
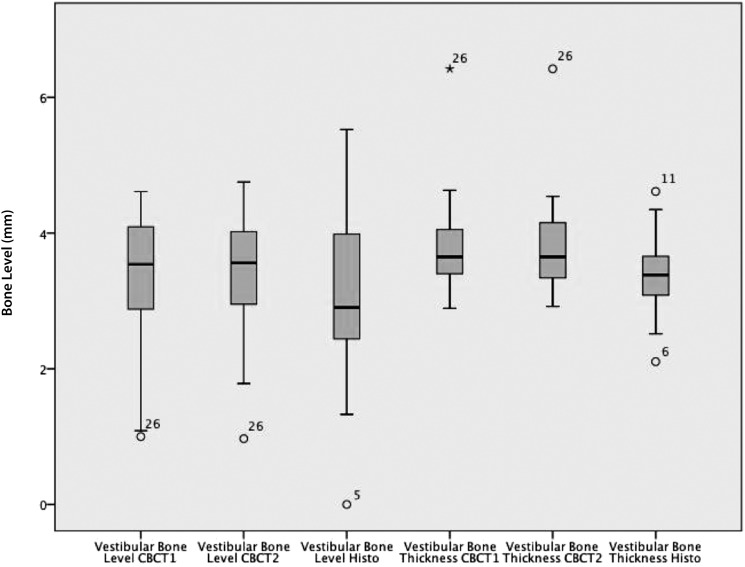
Vestibular bone level and vestibular bone thickness
The measured means of the vestibular bone level in CBCT were 3.41 mm (±0.90 mm) and 3.11 mm (±1.35 mm) in histology (Figure 4 box plot). Measurements of CBCT and histology did not significantly differ in paired t-test (p = 0.26) and showed a significant correlation (p = 0.02). For vestibular bone thickness, mean measurements in CBCT were 3.79 mm (±0.67 mm) and 3.37 mm (±0.55 mm) in histology. Here, a significant difference of means (p = 0.02) could be determined in a t-test. Also, no significant correlation for CBCT and histology could be found (p = 0.85) in paired-samples correlation.
Figure 4.
Box plot of vestibular bone level and vestibular bone thickness. CBCT, cone beam CT; histo, histology.
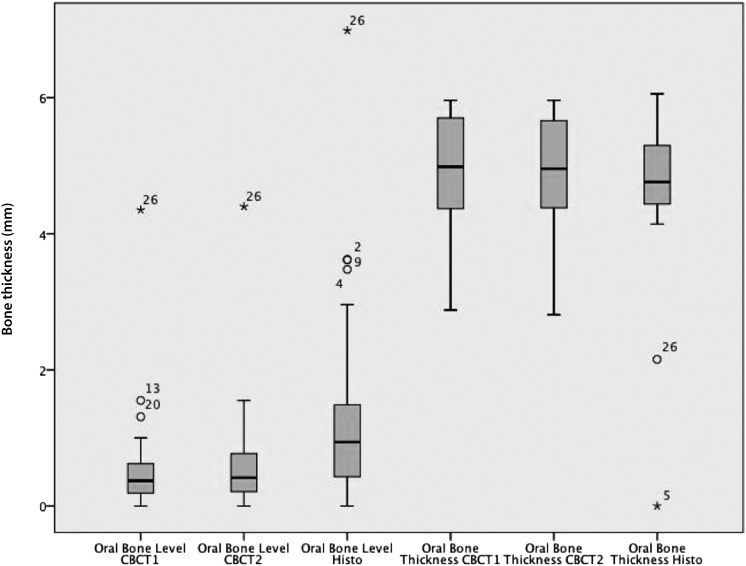
Oral bone level and oral bone thickness
The mean of measurements of oral bone level in CBCT were 0.61 mm (±0.87 mm) and 1.44 mm (±1.57 mm) in histology. The measured data of CBCT and histology were highly significantly correlated (p < 0.01). However, the measurements are significantly different (p < 0.01) in a t-test. The mean measurements of OBT were 4.93 mm (±0.76 mm) and 4.71 mm (±1.25 mm) in histology (Figure 5 box plot). CBCT and histology measures are highly correlated (p < 0.01) in paired-samples correlation and do not differ significantly in a t-test (p = 0.22).
Figure 5.
Box plot of oral bone level and oral bone thickness. CBCT, cone beam CT; histo, histology.
Mesial and distal bone levels
The mean of MBL were 0.84 mm (±1.00 mm) in CR, 0.72 mm (±0.65 mm) in CBCT measurements and 1.23 mm (±0.57 mm) in histology. No significant correlation in paired-samples correlation could be found for measurements of CR and CBCT (p = 0.08), CR and histology (p = 0.26) and CBCT and histology (p = 0.54). Also, the measurements of CR and CBCT (p = 0.54), CR and histology (p = 0.34) and CBCT and histology (p = 0.08) did not differ significantly in t-tests (Tables 1 and 2).
Table 1.
Vestibular–lingual descriptive statistics
| Criteria | n | Minimum (mm) | Maximum (mm) | Mean (mm) | Standard deviation (mm) |
|---|---|---|---|---|---|
| Vestibular bone level, CBCT1 | 26 | 1.00 | 4.61 | 3.40 | 0.86 |
| Vestibular bone level, CBCT2 | 26 | 0.97 | 4.75 | 3.40 | 0.89 |
| Vestibular bone level, CBCT1.1 | 26 | 0.97 | 4.73 | 3.37 | 0.87 |
| Vestibular bone level, CBCT2.1 | 26 | 0.99 | 5.59 | 3.45 | 0.97 |
| Mean vestibular bone level, CBCT | 26 | 0.98 | 4.92 | 3.41 | 0.90 |
| Vestibular bone level, histology | 26 | <0.01 | 5.53 | 3.11 | 1.35 |
| Vestibular bone thickness, CBCT1 | 26 | 2.89 | 6.42 | 3.78 | 0.68 |
| Vestibular bone thickness, CBCT2 | 26 | 2.92 | 6.42 | 3.80 | 0.68 |
| Vestibular bone thickness, CBCT1.1 | 26 | 2.87 | 6.40 | 3.78 | 0.66 |
| Vestibular bone thickness, CBCT2.1 | 26 | 2.90 | 6.39 | 3.78 | 0.66 |
| Mean vestibular bone thickness, CBCT | 26 | 2.90 | 6.41 | 3.79 | 0.67 |
| Vestibular bone thickness, histology | 26 | 2.10 | 4.61 | 3.37 | 0.55 |
| Oral bone level, CBCT1 | 26 | <0.01 | 4.35 | 0.60 | 0.87 |
| Oral bone level, CBCT2 | 26 | <0.01 | 4.40 | 0.63 | 0.88 |
| Oral bone level, CBCT1.1 | 26 | <0.01 | 4.30 | 0.61 | 0.86 |
| Oral bone level, CBCT2.1 | 26 | <0.01 | 4.34 | 0.61 | 0.87 |
| Mean oral bone level, CBCT | 26 | <0.01 | 4.38 | 0.61 | 0.87 |
| Oral bone level, histology | 26 | <0.01 | 6.99 | 1.44 | 1.57 |
| Oral bone thickness, CBCT1 | 26 | 2.88 | 5.96 | 4.93 | 0.77 |
| Oral bone thickness, CBCT2 | 26 | 2.81 | 5.96 | 4.93 | 0.75 |
| Oral bone thickness, CBCT1.1 | 26 | 2.83 | 5.94 | 4.92 | 0.76 |
| Oral bone thickness, CBCT2.1 | 26 | 2.84 | 5.95 | 4.92 | 0.75 |
| Mean oral bone thickness, CBCT | 26 | 2.84 | 5.95 | 4.93 | 0.76 |
| Oral bone thickness, histology | 26 | <0.01 | 6.05 | 4.71 | 1.25 |
| Implant length, CBCT1 | 26 | 9.46 | 10.58 | 9.88 | 0.31 |
| Implant length, CBCT2 | 26 | 9.43 | 10.56 | 9.87 | 0.29 |
| Implant length, CBCT1.1 | 26 | 9.60 | 10.55 | 9.88 | 0.27 |
| Implant length, CBCT2.1 | 26 | 9.62 | 10.54 | 9.89 | 0.27 |
| Mean implant length, CBCT | 26 | 9.53 | 10.56 | 9.88 | 0.29 |
| Implant length, histology | 26 | 9.58 | 10.51 | 9.87 | 0.29 |
| Implant diameter, CBCT1 | 26 | 3.43 | 4.34 | 3.97 | 1.85 |
| Implant diameter, CBCT2 | 26 | 3.48 | 4.29 | 3.97 | 1.82 |
| Implant diameter, CBCT1.1 | 26 | 3.38 | 4.11 | 3.93 | 0.15 |
| Implant diameter, CBCT2.1 | 26 | 3.39 | 4.13 | 3.92 | 0.19 |
| Mean implant diameter, CBCT | 26 | 3.38 | 4.13 | 3.97 | 0.18 |
| Implant diameter, histology | 26 | <0.01 | 4.16 | 3.70 | 0.78 |
CBCT, cone beam CT.
Table 2.
Results of paired-samples correlations and paired-samples test (t-test) and significant p-value
| Criteria | n | p-value (paired samples) | p-value (t-test) |
|---|---|---|---|
| Mean vestibular bone level, CBCT and histology | 26 | 0.02 | 0.26 |
| Mean vestibular bone thickness, CBCT and histology | 26 | 0.85 | 0.02 |
| Mean oral bone level, CBCT and histology | 26 | <0.01 | <0.01 |
| Mean oral bone thickness, CBCT and histology | 26 | <0.01 | 0.22 |
| Mean implant length, CBCT and histology | 26 | <0.01 | 0.84 |
| Mean implant diameter, CBCT and histology | 26 | 0.17 | 0.09 |
| Mean mesial bone level, CR and CBCT | 26 | 0.08 | 0.54 |
| Mean mesial bone level, CR and histology | 6 | 0.26 | 0.34 |
| Mean mesial bone level, CBCT and histology | 6 | 0.54 | 0.08 |
| Mean distal bone level, CR and CBCT | 26 | 0.08 | <0.01 |
| Mean distal bone level, CR and histology | 6 | 0.08 | 0.62 |
| Mean distal bone level, CBCT and histology | 6 | 0.15 | 0.88 |
| Mean implant length, CR and CBCT | 26 | <0.01 | 0.43 |
| Mean implant length, CR and histology | 6 | 0.70 | 0.10 |
| Mean implant length, CBCT and histology | 6 | 0.74 | 0.10 |
| Mean implant diameter, CR and CBCT | 26 | <0.01 | <0.01 |
| Mean implant diameter, CBCT and histology | 26 | 0.17 | 0.09 |
CBCT, cone beam CT; CR, intra-oral radiography.
The measured means of distal bone levels were 0.82 mm (±0.91 mm) in CR, 0.84 mm (±0.92 mm) in CBCT and 1.25 mm (±0.98 mm) in histology. No statistically significant correlation could be found in paired-samples correlation for the data of CR and CBCT (p = 0.08). They were significantly different in a t-test (p < 0.01). No significant correlation could be found for the measurements of CR and histology (p = 0.08) and CBCT and histology (p = 0.15). They did not differ significantly in a t-test (for detailed information, refer to Table 3).
Table 3.
Intraclass correlation coefficient and significance value p
| Measured criterion | Intraclass correlation |
||
|---|---|---|---|
| Single measures | Average measures | p-value | |
| Vestibular bone level | 0.95 | 0.99 | <0.01 |
| Vestibular bone thickness | 1.00 | 1.00 | <0.01 |
| Oral bone level | 1.00 | 1.00 | <0.01 |
| Oral bone thickness | 1.00 | 1.00 | <0.01 |
| Mesial bone level, CR | 1.00 | 1.00 | 0.01 |
| Mesial bone level, CBCT | 1.00 | 1.00 | <0.01 |
| Distal bone level, CR | 0.74 | 0.92 | <0.01 |
| Distal bone level, CBCT | 1.00 | 1.00 | <0.01 |
| Implant length, CR | 0.96 | 0.99 | <0.01 |
| Implant length, CBCT | 0.86 | 0.96 | <0.01 |
| Implant diameter, CR | 0.97 | 0.99 | <0.01 |
| Implant diameter, CBCT | 0.98 | 0.99 | <0.01 |
CBCT, cone beam CT; CR, intra-oral radiography.
Implant length
The mean of CBCT measurements in vestibulo-oral direction for IL was 9.88 mm (±0.29 mm). The mean of CR in the mesiodistal direction was 9.84 mm (±0.24 mm), for CBCT in mesiodistal direction 9.87 mm (±0.29 mm), and the means of histology in both directions were 9.87 mm (±0.29 mm). Measurements of CBCT in vestibulo-oral direction showed a highly significant correlation with histological measurements in paired-samples correlation (p < 0.01) and were not significantly different in a t-test (p = 0.84). The correlation of measurements of CR and CBCT in the mesiodistal direction is statistically significant (p < 0.01), and the average measures were not significantly different in a t-test (p = 0.43). No significant correlation could be found in paired-samples correlation for means of CR and histology (p = 0.70) and for CBCT and histology (p = 0.74) in the mesiodistal direction. Also, no significant difference could be found for CR and histology (p = 0.10) and CBCT and histology (p = 0.10) in t-tests (Table 4).
Table 4.
Mesial–distal descriptive statistics
| Criteria | n | Minimum (mm) | Maximum (mm) | Mean (mm) | Standard deviation (mm) |
|---|---|---|---|---|---|
| Mesial bone level, CR1 | 26 | <0.01 | 3.69 | 0.84 | 1.00 |
| Mesial bone level, CR2 | 26 | <0.01 | 3.67 | 0.84 | 1.00 |
| Mesial bone level, CR1.1 | 26 | <0.01 | 3.60 | 0.84 | 1.00 |
| Mesial bone level, CR2.1 | 26 | <0.01 | 3.62 | 0.84 | 0.99 |
| Mean mesial bone level, CR | 26 | <0.01 | 3.65 | 0.84 | 1.00 |
| Mesial bone level, CBCT1 | 26 | <0.01 | 2.05 | 0.73 | 0.64 |
| Mesial bone level, CBCT2 | 26 | <0.01 | 2.00 | 0.72 | 0.65 |
| Mesial bone level, CBCT1.1 | 26 | <0.01 | 2.03 | 0.72 | 0.65 |
| Mesial bone level, CR2.1 | 26 | <0.01 | 2.03 | 0.72 | 0.65 |
| Mean mesial bone level, CBCT | 26 | <0.01 | 2.03 | 0.72 | 0.65 |
| Mesial bone level, histology | 6 | 0.52 | 2.10 | 1.23 | 0.57 |
| Distal bone level, CR1 | 26 | <0.01 | 3.32 | 0.83 | 0.92 |
| Distal bone level, CR2 | 26 | <0.01 | 3.30 | 0.82 | 0.91 |
| Distal bone level, CR1.1 | 26 | <0.01 | 3.34 | 0.82 | 0.92 |
| Distal bone level, CR2.1 | 26 | <0.01 | 3.62 | 0.84 | 0.99 |
| Mean distal bone level, CR | 26 | <0.01 | 3.31 | 0.82 | 0.91 |
| Distal bone level, CBCT1 | 26 | <0.01 | 3.44 | 0.84 | 0.93 |
| Distal bone level, CBCT2 | 26 | <0.01 | 3.49 | 0.84 | 0.92 |
| Distal bone level, CBCT1.1 | 26 | <0.01 | 3.42 | 0.84 | 0.92 |
| Distal bone level, CBCT2.1 | 26 | <0.01 | 3.39 | 0.83 | 0.91 |
| Mean distal bone level, CBCT | 26 | <0.01 | 3.44 | 0.84 | 0.92 |
| Distal bone level, histology | 6 | <0.01 | 2.58 | 1.25 | 0.98 |
| Implant length, CR1 | 26 | 9.53 | 10.46 | 9.83 | 0.24 |
| Implant length, CR2 | 26 | 9.53 | 10.51 | 9.84 | 0.25 |
| Implant length, CR1.1 | 26 | 9.54 | 10.50 | 9.85 | 0.23 |
| Implant length CR2.1 | 26 | 9.53 | 10.46 | 9.85 | 0.23 |
| Mean implant length, CR | 26 | 9.53 | 10.48 | 9.84 | 0.24 |
| Implant length, CBCT1 | 26 | 9.56 | 10.53 | 9.88 | 0.29 |
| Implant length, CBCT2 | 26 | 9.54 | 10.58 | 9.86 | 0.30 |
| Implant length, CBCT1.1 | 26 | 9.50 | 10.43 | 9.84 | 0.26 |
| Implant length, CBCT2.1 | 26 | 9.51 | 10.74 | 9.89 | 0.31 |
| Mean implant length, CBCT | 26 | 9.53 | 10.57 | 9.87 | 0.29 |
| Implant length, histology | 26 | 9.58 | 10.51 | 9.87 | 0.29 |
| Implant diameter, CR1 | 26 | 3.45 | 4.07 | 3.93 | 0.12 |
| Implant diameter, CR2 | 26 | 3.48 | 4.07 | 3.92 | 0.12 |
| Implant diameter, CR1.1 | 26 | 3.46 | 4.05 | 3.91 | 0.11 |
| Implant diameter, CR2.1 | 26 | 3.48 | 4.04 | 3.92 | 0.11 |
| Mean implant diameter, CR | 26 | 3.48 | 4.06 | 3.92 | 0.12 |
| Implant diameter, CBCT1 | 26 | 3.44 | 4.54 | 4.07 | 0.22 |
| Implant diameter, CBCT2 | 26 | 3.41 | 4.54 | 4.07 | 0.23 |
| Implant diameter, CBCT1.1 | 26 | 3.45 | 4.49 | 4.07 | 0.21 |
| Implant diameter, CBCT2.1 | 26 | 3.45 | 4.50 | 4.07 | 0.21 |
| Mean implant diameter, CBCT | 26 | 3.44 | 4.52 | 4.07 | 0.22 |
| Implant diameter, histology | 26 | <0.01 | 4.16 | 3.70 | 0.78 |
CBCT, cone beam CT; CR, intra-oral radiography.
Implant diameter
The measured mean of the implant diameter in the vestibulo-oral direction was 3.97 mm (±1.84 mm) for CBCT. The mean in the mesiodistal direction of CR was 3.92 mm (±0.12 mm) and, for CBCT, was 4.07 mm (±0.22 mm). The mean of histology was 3.70 mm (±0.78 mm). In paired-samples correlation, there was no significant association between the data of CBCT and histology (p = 0.17). CR and CBCT measurements (p < 0.01) were significantly correlated. Here, no significant difference could be found in t-tests for CBCT and histology (p = 0.09) and the data of CR and CBCT (p = 0.01).
Discussion
In this study, the diagnostic accuracy of peri-implant bone level measurements of CBCT and CR in implanted dog jaws was investigated. To determine ground truth, results were compared with the associated histology measurements.
The results show, for CBCT measurements of vestibular bone level, an overestimation by about +0.3 mm (±0.04 mm) on average. On the contrary, the CBCT measurements of oral bone level underestimated the real bone height by about −0.83 mm (±0.01 mm). The reason for this discrepancy might in part be explained by the orientation of the specimen in the CBCT machine as illustrated in Figure 1: the “direction” of artefacts is diagonal to the implant axis and artificially augments the bone level on the vestibular side, while the oral bone level on the oral side is hidden by extinguishing artefacts. This suggests that the measurements around implants in the vestibular and oral directions might be assessed in submillimetre accuracy using CBCT, but the orientation of the implants with respect to the axis of the X-rays has to be taken into account when interpreting the images. Clearly, the transfer into clinical application requires further investigations for several drawbacks of this animal model. No other sources of artefacts as moving or metallic restorations were present. Also, the orientation of the implant axis was perpendicular to the direction of X-rays not resembling the usual clinical set-up. Besides the limits of this study, the data show values close enough to the measured ground truth to justify further investigation of the matter clinically.
The overestimation of thickness of oral (+0.22 mm ± 0.01mm) and vestibular (+0.42 mm ± 0.01 mm) vestibular by CBCT images has to be seen in similar context. However, this information could not be obtained by CR images at all, and it might be of importance in cases where the position of the implant concerning the cortical bone or nerve channel has to be determined. Also, measurements in the mesial and distal directions show a similar effect: in the mesial direction, beam-hardening artefacts seem to attenuate measured values more strongly compared with histomorphometry than on distal sites. This observation is also in concordance with the direction of artefacts (compare Figure 1). On both sides, mesial and distal, the bone level is not only underestimated in CBCT but also in CR. The mean of the distal bone levels in CBCT was 0.84 mm (±0.92 mm), in CR it was 0.82 mm (±0.91 mm) and the histological mean measurement was 1.25 mm (±0.98 mm). Mesial bone levels were 0.84 mm (±1.00 mm) in CR, 0.72 mm (±0.65 mm) in CBCT measurements and 1.23 mm (±0.57 mm) in histology.
High measuring accuracy could be found regarding the IL. The measurements of CBCT (9.87 mm ± 0.29 mm) achieved superior values. On average, there was no aberration to the average value of histological measurements of dental IL (9.87 mm ± 0.29 mm). The mean of CR evaluation was about 9.84 mm ± 0.24 mm and showed just a marginal aberration. These outcomes are in concordance with research data of studies evaluating the effects of the measurement direction on the accuracy of linear measurements and evaluating the accuracy of CBCT in assessing peri-implant bone defect regeneration.22,23
Analogous studies were made to evaluate the accuracy of CBCT. The fidelity of CBCT images is shown in various studies, for example, identification of the mandibular canal pre-surgical implant planning and diagnosis of periodontal defects.20,24,25 In all these investigations, CBCT imaging was superior to other imaging modalities, for example, intra-oral radiography. The disadvantage of 2D imaging, also shown in the present study, is the missing picture of vestibular and lingual structures whereby no diagnostic findings could be made by observers.
A presumption for inaccuracy of CBCT measurements could be found in image artefacts caused by metallic structures of dental implants.26 Related studies show a high correlation between image quality, accuracy of linear measurement and image artefacts. Future studies have to evaluate the further development of image artefact-reducing algorithms and the approval of beam-hardening artefacts in CBCT.26,27 Another assumption for inaccurate results could be found by little aberrations of the sectional planes of CR, CBCT and histology images. Even if the intra-oral radiographs and CBCTs were performed as close to clinical proceeding as possible, variations in angulation of the X-ray beam can result in small changes in the distance of two measuring points. A further limitation of this study is the absence of movement artefacts during exposure, because the dogs were already sacrificed. Consequently, the results are limited in being assignable to clinical proceeding.
Another aspect confounding results is the small contingent of histology measurements of mesial and distal directions because of the sequence of histological preparation, whereby various implants were lost by preparing the vestibular–oral direction of implants.
Conclusion
In this optimal imaging scenario with no specimen movement, and no fillings present, the results show limitations of CBCT in accurately determining the vestibular and oral bone levels of implants in the vertical as well as the horizontal dimensions. Metal artefacts of four implants placed next to each other were present in this investigation. However, considering the submillimetre differences in CBCT measurements compared with histological measurements, limited yet useful information on bone level measurements of dental implants might be shown in CBCT. The direction of the X-rays with respect to the implant axis should be taken into account when interpreting CBCT images. Compared with conventional radiographs, additional information can be extracted from CBCT; however, owing to metal artefacts, the image impression remains unsightly. Mesial and distal measurements are equally accurate for CBCT and CR. Owing to the experimental design of this study, results are not fully transferable to clinical reality.
References
- 1.Pihlstrom BL. Periodontal risk assessment, diagnosis and treatment planning. Periodontol 2000 2001; 25: 37–58. [DOI] [PubMed] [Google Scholar]
- 2.Schliephake H, Wichmann M, Donnerstag F, Vogt S. Imaging of periimplant bone levels of implants with buccal bone defects. Clin Oral Implants Res 2003; 14: 193–200. [DOI] [PubMed] [Google Scholar]
- 3.Mengel R, Kruse B, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of peri-implant defects: an in vitro study on native pig mandibles. J Periodontol 2006; 77: 1234–41. doi: 10.1902/jop.2006.050424 [DOI] [PubMed] [Google Scholar]
- 4.Tyndall DA, Rathore S. Cone beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am 2008; 52: 825–41. [DOI] [PubMed] [Google Scholar]
- 5.Jervøe-Storm PM, Hagner M, Neugebauer J, Ritter L, Zöller JE, Jepsen S, et al. Comparison of cone-beam computerized tomography and intraoral radiographs for determination of the periodontal ligament in a variable phantom. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e95–101. [DOI] [PubMed] [Google Scholar]
- 6.Mol A. Imaging methods in periodontology. Periodontol 2000 2004; 34: 34–48. [DOI] [PubMed] [Google Scholar]
- 7.Tyndall DA, Brooks SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 630–7. [DOI] [PubMed] [Google Scholar]
- 8.Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J 2009; 42: 507–15. [DOI] [PubMed] [Google Scholar]
- 9.Isidor F. Clinical probing and radiographic assessment in relation to the histologic bone level at oral implants in monkeys. Clin Oral Implants Res 1997; 8: 255–64. [DOI] [PubMed] [Google Scholar]
- 10.Corpas Ldos S, Jacobs R, Quirynen M, Huang Y, Naert I, Duyck J. Peri-implant bone tissue assessment by comparing the outcome of intra-oral radiograph and cone beam computed tomography analyses to the histological standard. Clin Oral Implants Res 2011; 22: 492–9. doi: 10.1111/j.1600-0501.2010.02029.x [DOI] [PubMed] [Google Scholar]
- 11.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: an in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol 2008; 37: 252–60. doi: 10.1259/dmfr/57711133 [DOI] [PubMed] [Google Scholar]
- 12.Eickholz P, Hausmann E. Accuracy of radiographic assessment of interproximal bone loss in intrabony defects using linear measurements. Eur J Oral Sci 2000; 108: 70–3. [DOI] [PubMed] [Google Scholar]
- 13.Jeffcoat MK. Digital radiology for implant treatment planning and evaluation. Dentomaxillofac Radiol 1992; 21: 203–7. doi: 10.1259/dmfr.21.4.1299635 [DOI] [PubMed] [Google Scholar]
- 14.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 1998; 8: 1558–64. [DOI] [PubMed] [Google Scholar]
- 15.Senel FC, Duran S, Icten O, Izbudak I, Cizmeci F. Assessment of the sinus lift operation by magnetic resonance imaging. Br J Oral Maxillofac Surg 2006; 44: 511–14. doi: 10.1016/j.bjoms.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 16.Chai-U-Dom O, Ludlow JB, Tyndall DA, Webber RL. Comparison of conventional and TACT (Tuned Aperture Computed Tomography) digital subtraction radiography in detection of pericrestal bone-gain. J Periodont Res 2002; 37: 147–53. [DOI] [PubMed] [Google Scholar]
- 17.Ramesh A, Ludlow JB, Webber RL, Tyndall DA, Paquette D. Evaluation of tuned aperture computed tomography (TACT) in the localization of simulated periodontal defects. Dentomaxillofac Radiol 2001; 30: 319–24. doi: 10.1038/sj/dmfr/4600635 [DOI] [PubMed] [Google Scholar]
- 18.Neugebauer J, Ritter L, Mischkowski R, Zöller JE. Three-dimensional diagnostics, planning and implementation in implantology. Int J Comput Dent 2006; 9: 307–19. [PubMed] [Google Scholar]
- 19.Small BW. Cone beam computed tomography. Gen Dent 2007; 55: 179–81. [PubMed] [Google Scholar]
- 20.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol 2005; 76: 665–73. doi: 10.1902/jop.2005.76.5.665 [DOI] [PubMed] [Google Scholar]
- 21.Schwarz F, Jung RE, Fienitz T, Wieland M, Becker J, Sager M. Impact of guided bone regeneration and defect dimension on wound healing at chemically modified hydrophilic titanium implant surfaces: an experimental study in dogs. J Clin Periodontol 2010; 37: 474–85. doi: 10.1111/j.1600-051X.2010.01551.x [DOI] [PubMed] [Google Scholar]
- 22.Tsutsumi K, Chikui T, Okamura K, Yoshiura K. Accuracy of linear measurement and the measurement limits of thin objects with cone beam computed tomography: effects of measurement directions and of phantom locations in the fields of view. Int J Oral Maxillofac Implants 2011; 26: 91–100. [PubMed] [Google Scholar]
- 23.Fienitz T, Schwarz F, Ritter L, Dreiseidler T, Becker J, Rothamel D. Accuracy of cone beam computed tomography in assessing peri-implant bone defect regeneration: a histologically study in dogs. Clin Oral Implants Res 2012; 23: 882–7. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci 2011; 19: 240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dreiseidler T, Mischkowski RA, Neugebauer J, Ritter L, Zöller JE. Comparison of cone-beam imaging with orthopantomography and computerized tomography for assessment in presurgical implant dentistry. Int J Oral Maxillofac Implants 2009; 24: 216–25. [PubMed] [Google Scholar]
- 26.Zhang Y, Zhang L, Zhu XR, Lee AK, Chambers M, Dong L. Reducing metal artifacts in cone-beam CT images by preprocessing projection data. Int J Radiat Oncol Biol Phys 2007; 67: 924–32. [DOI] [PubMed] [Google Scholar]
- 27.Schulze RK, Berndt D, d'Hoedt B. On cone-beam computed tomography artifacts induced by titanium implants. Clin Oral Implants Res 2010; 21: 100–7. doi: 10.1111/j.1600-0501.2009.01817.x [DOI] [PubMed] [Google Scholar]