Abstract
Background
In spite of the strong role of traditional medicine in childcare in the pluralistic healthcare system in Western Africa, little information is known on mothers’ domestic plant knowledge. Identifying local perspectives and treatments of children’s illnesses, including folk illnesses, is essential to having a comprehensive understanding of how mothers make healthcare treatment decisions. We aimed to identify which infant illnesses Beninese and Gabonese mothers knew to treat with medicinal plants and for which illnesses they sought biomedical care or traditional healers.
Methods
We conducted 81 questionnaires with mothers in Bénin and Gabon and made 800 botanical specimens of cited medicinal plants. We calculated the number of species cited per illness and the proportion of participants knowledgeable on at least one herbal remedy per illness. Using qualitative data, we described folk illnesses in each country and summarized responses on preferences for each of the three healthcare options.
Results
Participants from both countries were most knowledgeable on plants to treat respiratory illnesses, malaria, diarrhea, and intestinal ailments. Mothers also frequently mentioned the use of plants to encourage children to walk early, monitor the closure of fontanels, and apply herbal enemas. Major folk illnesses were atita and ka in Bénin and la rate and fesses rouges in Gabon. Traditional healers were reported to have specialized knowledge of cultural bound illnesses. Malaria was frequently cited as an illness for which mothers would directly seek biomedical treatment.
Conclusion
Mothers largely saw the three systems as complementary, seamlessly switching between different healing options until a remedy was found. Folk illnesses were found to give insight into local treatments and may reveal important neglected diseases. Due to high reported levels of knowledge on treating top statistical causes of infant mortality and folk illnesses, mothers’ medicinal plant knowledge should be included in the analysis of healthcare-seeking behavior for childcare.
Introduction
Sub-Saharan African healthcare is essentially pluralistic, structured around three main systems: biomedical care, traditional healers, and popular knowledge [1]–[2]. In spite of the promotion of biomedicine by international healthcare organizations, traditional medicine remains the primary form of healthcare for more than 80% of African populations [3]. Traditional medical systems include not only traditional healers, but also the popular knowledge of local populations, known as domestic medicine or home remedies. Most ethnobotanical literature on traditional medicine is concentrated on the knowledge of traditional healers and largely overlooks domestic medicine, the knowledge of women [4], and more specifically, the knowledge of mothers [5]–[6]. Since home remedies (self-treatment with herbs) comprise the majority of African medicine [1], [7]–[8], domestic knowledge needs to be prioritized in medical research and reinforced in order to improve healthcare and enhance local populations’ responses to illness. This point is especially critical in high priority health populations, such as infants and children in sub-Saharan Africa [9].
African mothers’ knowledge of health is directly associated with children’s well-being, as women are largely responsible for childcare [8], [10]. Recent ethnobotanical research has found that mothers’ knowledge of herbal medicine has a positive effect on child health outcomes, including a decrease in infections [10]–[11]. Mothers who had high levels of plant knowledge and use have been shown to have healthier children [6] and a greater likelihood to take ill children to a dispensary, suggesting that knowledge in one healthcare domain corresponds with better overall understanding of health [10].
In spite of these correlations, biomedical studies have largely measured mother’s health-seeking behavior on factors related to biomedical care, such as formal education, distance to provider, and cost of obtaining care [12]. This literature overlooks if and what role local concepts of illness have in treatment choices and results in the loss of incorporating this information into infant health programs [13]. Local concepts of illness include not only local names, perceptions, and symptoms of biomedical illnesses, but also cultural bound syndromes, “a group of folk illnesses, each of which is unique to a particular group of people, cultural, or geographical area” [14]. Some scholars have cautioned that the “cultural” component of the term cultural bound syndromes emphasizes the biomedical perspective that biological illnesses are more objective than folk illnesses [14]. We use the term in order to designate those illnesses not generally defined and recognized in biomedicine.
Understanding local perspectives of the treatment of major children’s illnesses identified by the WHO [15], such as malaria [13], [16] and diarrhea [17], [18], as well as the treatment of children’s folk illnesses [19], [20], is essential to having a comprehensive understanding of childcare in Africa. In this study, we assessed how mothers make healthcare decisions by identifying which infant illnesses mothers in Western Africa treat with medicinal plants and for which illnesses they seek biomedical care or consult traditional healers. We worked in Bénin and Gabon, two African countries with diverse populations, vegetation types, cultures, and levels of human development. Our research was based on the following research questions: Which children’s illnesses do Beninese and Gabonese mothers treat with medicinal plants? What are the major children’s folk illnesses in each country? For which ailments do mothers seek treatment from biomedical doctors? Which illnesses do mothers prefer to be treated by traditional healers?
Methods
Study areas
Bénin is located in West Africa, with a surface area of 112,622 sq. km and a population of 9.8 million people [21]. It is ranked below the Sub-Saharan average in the Human Development Index (HDI) and considered a country of “low human development” [22]. It has an infant mortality ratio of 58 deaths per 1,000 live births [21]. Gabon is located in Western Central Africa, with a surface area of 267,667 sq. km, and a population of 1.7 million people [23]. The UNDP ranked Gabon 106th in the Human Development Index, slightly above countries of “medium human development” [24]. It has an infant mortality ratio of 48 deaths per 1,000 live births [23].
Data collection and analysis
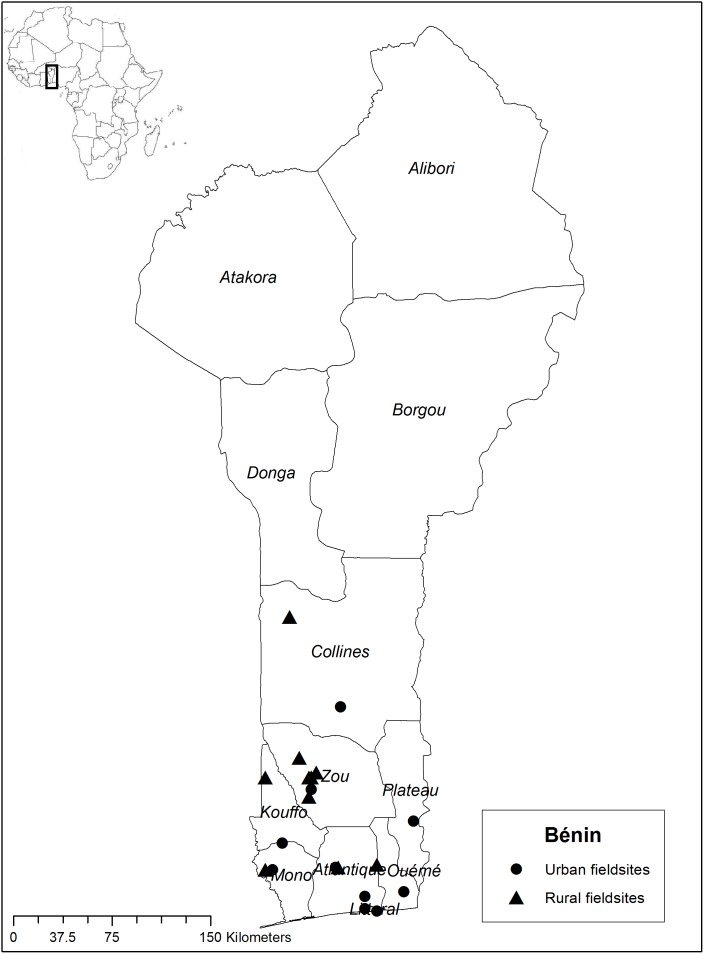
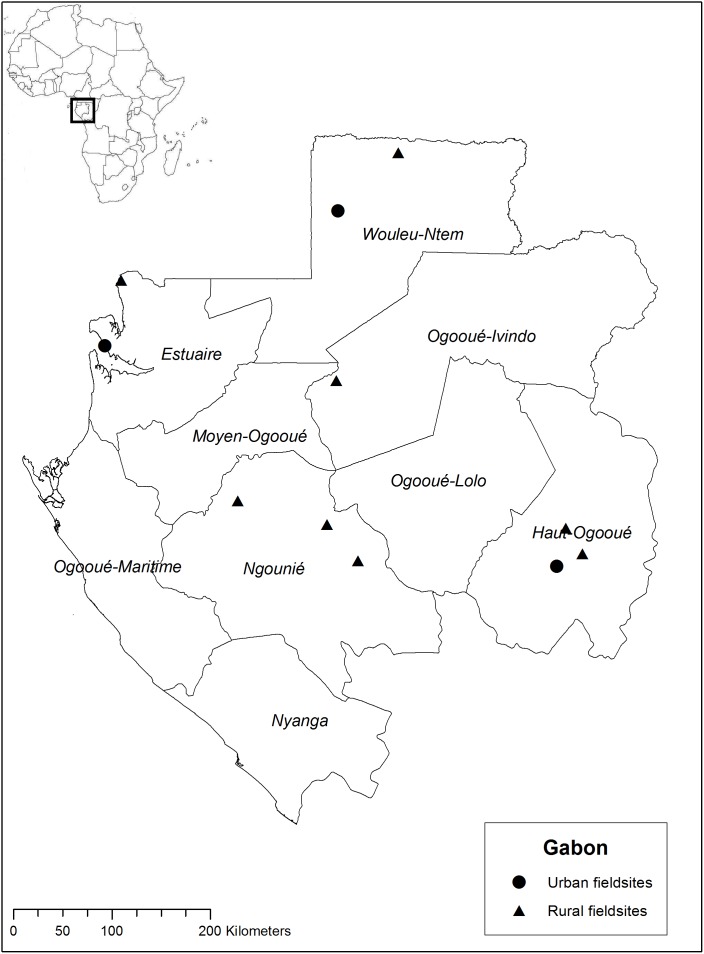
Between April and October 2011 we worked in rural and urban areas of Bénin, mainly with Fon and Yoruba ethnic groups in the southern departments Collines, Kouffo, Zou, Plateau, Ouémè, Atlantique, Mono, and Littoral (Figure 1). From June until December 2012, we worked with Bantu-speaking ethnic groups in Gabon, namely, the Fang, Mitsogo, Obamba, and Bapounou peoples, in the departments of Estuaire, Woleu-Ntem, Haut-Ogooué, Ngounié, and Ogooué-Ivindo (Figure 2).
Figure 1. Map of the Bénin fieldwork sites in 2011.
Figure 2. Map of the Gabon fieldwork sites in 2012.
We started our research at the herbal medicine marketplaces in each country, taking time to familiarize ourselves with commonly utilized species, local illnesses and healthcare practices. From these initial market contacts, we utilized snowball sampling to identify women from surrounding urban and rural communities. We conducted an ethnobotanical questionnaire on practices related to childcare, including questions on herbal remedies for specific illnesses, definitions of folk illnesses, and preferences for the three types of healthcare. In total we interviewed 43 Beninese and 38 Gabonese mothers. In Bénin we worked with the following ethnic groups: Fon and related (70%), Yoruba and related (14%), Adja and related (5%) and mixed ethnicities (11%). In Gabon we worked with the following ethnic groups: Fang (45%), Mitsogo (16%), Babungu (16%), Obamba (8%), Bapounou (5%), and other (Ossimba, Omiene, Bateke) (10%). All women received financial compensation equivalent to local salaries for their time and involvement. We conducted the questionnaires orally in French, at participants’ homes and workplaces, and employed local language interpreters when needed.
After each of the 81 questionnaires, we accompanied participants to collect the plants that were cited in the interviews. We used standard botanical collection methods [25] to make vouchers of plants from the surrounding gardens, forests, and savanna landscapes. For women that we interviewed on the market, we purchased plants directly from market stalls and made trips into the field together to collect fresh samples when possible. In addition to collecting voucher specimens, we also gathered detailed information on their use, effects, and local names (see Tables S1 and S2). We deposited vouchers of all collected plants at the Herbier National du Bénin (BEN) and the Herbier National du Gabon (LBV). A complete set of duplicates was exported to the Wageningen branch of National Herbarium of the Netherlands (WAG), now merged with Naturalis Biodiversity Center (L), where the specimens were identified by the research team and several botanical specialists. Our plant collection did not involve endangered or protected plant species.
We assessed mothers’ knowledge of domestic medicine by calculating the number of species for each health issue and the percentage of mothers who knew at least one herbal recipe for each illness. We then summarized descriptions of folk illnesses and selected qualitative data from our interviews to illustrate which illnesses mothers treated with the three systems of healthcare: biomedicine, their own plant knowledge, or traditional healers. Maps of the fieldwork locations were created in ArcGIS 10.1 using open source geospatial data from DIVA-GIS (http://www.diva-gis.org/).
Ethics statement
We adhered to all components of the Code of Ethics of the International Society of Ethnobiology [26], including carefully explaining the nature of our research, receiving oral consent, providing monetary compensation for involvement in the work, anonymizing informants' identities during data analysis, and working in a fully mindful and respectful manner. Oral consent was acquired in place of written consent due to the largely illiterate populations with whom we worked. We followed all research procedures and protocols at Leiden University, Naturalis Biodiversity Center, and the host institutes in each country. For the Bénin fieldwork, we acquired a formal invitation from the Faculté des Sciences Agronomiques, Université d’Abomey-Calavi (UAC), received a research permit (#041511) from the Faculté des Sciences et Techniques (UAC), and obtained a plant export permit (#0000591) from the Service de la Protection des Vegetaux et du Control Phytosanitaire, Ministre de l’Agriculture, de l’Elevage et de la Peche. For the Gabon fieldwork, the Centre National de la Recherche Scientifique et Technologique (CENAREST) provided a letter of invitation (#176). After approving our research proposal, CENAREST granted a research permit (#AR0028/12). We acquired authorization to enter the National Parks of Gabon (#000026) from the Agence Nationale des Parcs Nationaux (ANPN), and authorization to export botanical specimens (#00145, #00219) from the L’Institut de Pharmacopée et de Médecine Traditionelles (IPHAMETRA). We received formal administrative approval from our host institutes and were not required to submit our proposals to a human subjects review board for further review.
Results
Mothers’ knowledge of treating biomedical childhood illnesses with plants
Beninese participants cited 255 medicinal plant species and Gabonese participants cited 179 species. All species, together with vernacular names, scientific names and specific uses, are listed in Table S1 (Bénin) and Table S2 (Gabon). The highest percentages of plants in both countries were used to treat those child illnesses considered to be of major concern by the WHO: diarrhea, respiratory conditions, and malaria. Over 95% of participants from Bénin and over 84% of participants from Gabon knew at least one recipe to treat those diseases (Table 1). Respiratory-related ailments included illnesses such as the flu, cough, asthma, bronchitis, and specific folk illnesses related to respiratory problems in the case of Gabonese informants. Mothers also mentioned children’s ailments such as earache, chicken pox, colic, stomachache and vomiting, which we left out of the table because few plants and treatments were cited.
Table 1. Children’s health issues treated with medicinal plants by mothers in Bénin and Gabon.
| Health Issue | # species(%) N = 255 | # participants1(%) N = 43 | # species(%) N = 179 | # participants1(%) N = 38 |
| Bénin | Bénin | Gabon | Gabon | |
| respiratory-related | 53 (21) | 42 (98) | 49 (27) | 32 (84) |
| diarrhea | 39 (15) | 41 (95) | 27 (15) | 34 (89) |
| malaria | 54 (21) | 41 (95) | 36 (20) | 33 (87) |
| intestinal cleanse* | 58 (23) | 41 (95) | 31 (17) | 33 (87) |
| measles | 34 (13) | 37 (86) | 17 (9) | 30 (79) |
| strengthener* | 59 (23) | 40 (93) | 21 (12) | 22 (58) |
| fontanels * | 31 (12) | 35 (81) | 23 (13) | 28 (74) |
| post-circumcision | 32 (13) | 37 (86) | 14 (8) | 21 (55) |
| walk early * | 22 (8) | 28 (65) | 17 (9) | 29 (76) |
| umbilical cord | 13 (5) | 32 (74) | 12 (7) | 24 (63) |
| convulsions/crisis* | 32 (13) | 33 (77) | 4 (2) | 4 (10) |
| teething | 25 (10) | 30 (70) | 2 (1) | 4 (10) |
| anti-sorcery* | 21 (8) | 25 (58) | 6 (3) | 6 (16) |
| fever | 37 (15) | 19 (44) | 14 (7) | 7 (18) |
| atita * | 31 (12) | 35 (81) | - | - |
| ka * | 26 (10) | 29 (67) | - | - |
| fesses rouges * | - | - | 26 (15) | 28 (74) |
| la rate * | - | - | 34 (19) | 26 (68) |
| pogha * | - | - | 10 (6) | 6 (16) |
Percentage of mothers from each country who knew at least one herbal recipe.
*Folk illness or treatment.
Children’s folk illnesses in Bénin
Mothers from Bénin mentioned two main folk illnesses, atita (Fon) and ka (Fon), and several cultural practices. Atita was described as a rash with “red bumps coming from the anus” or “itchy and stinging” red bumps in the groin and armpits. It was reported to be caused by the over-consumption of sugar or peanuts by the child or by the mother during pregnancy. The most common treatment for atita was an herbal bath or boiled plants consumed as tea (Table S1). Ka was described as an infection with large red bumps that were caused by the heat. It was reported to be treated by herbal baths, ingested teas, and through applying macerated plants directly to the infection.
The care and maintenance of open fontanels was a common practice in Bénin. Mothers’ considered it to be important for the soft spot of the fontanel to be able to “breathe” and eventually close. They used various herbal pomades, washes, and ingested teas for young children whom became ill from the failure of the fontanels to close. Beninese mothers highly valued their children to walk early in life. They encouraged their children with massages, herbal baths, and ingested teas. Walking early was seen as a sign that the child was developing normally and gaining independence, which would enable the mother to rest. Enemas were administered to newborn infants to remove the meconium, as well as to older infants for daily cleanses and constipation relief. These enemas frequently contained ground red peppers (Capsicum annuum) or different species of melegueta pepper (Aframomum spp.) mixed with water. Strengtheners were used in herbal treatments for premature birth, to strengthen newborns, and to assist in infant growth. Delayed and stunted growth were explained by mothers to be caused either by malnutrition or if an expectant mother came in contact with a praying mantis (hence the hunched over appearance and thin arms of an infant). It was treated with an herbal bath with an herbal recipe that included the eggs of a praying mantis. Various herbal treatments were applied to the umbilical cord of newborns to hasten the recovery period, as well as the application of herbs to assist in the healing process of circumcision.
Children’s folk illnesses in Gabon
Gabonese and Beninese mothers shared the cultural practices of monitoring the closure of the fontanels, encouraging children to walk early, and bathing newborns and young children to give strength. Monitoring the closure of fontanels (abobane in Fang) in Gabon was considered necessary to avoid “bad wind or spirits” that could enter, resulting in a child’s stunted growth. Herbal treatments included applying pomade made from leaves directly to the infants’ head and applying peanut butter to the palate of the mouth (Table S2). Mothers pointed out that not all children suffered from open fontanels. Encouraging children to walk early also was seen as the mothers’ recuperation of independence; they could do more work because the child could play outside with its siblings. One of the most commonly mentioned Gabonese folk illnesses was known as fesses rouges in French (ntcheke in the Babungu language, kusu in Punu, tzogho in Fang, and kengey in Teke). Like its literal French translation, the main symptom of fesses rouges was a red, irritated bottom caused “by sitting in the dirt,” “by microbes,” or “during childbirth when heat enters the body through the anus”. Treatments included applying herbal pomades and herbal enemas.
Folk illness la rate (tzit in Fang and kabama in Teke) which in English is translated as “the spleen,” was characterized by a tender, swollen left side of the body and a skinny overall physical build. An earlier stage of la rate, known as ebem in Fang, was characterized by high fever and green feces. Although most respondents were not aware of the cause of la rate, some participants mentioned God’s will, anemia, and malnutrition as possible causes. Treatments included herbal massages, herbal enemas, and traditional “vaccinations”- the creation of small incisions on the left side of the body with a razor blade and application of the fresh juice of plants into the cuts. Folk illness pogha (in Mitsogo and Babungu languages) was characterized by fever, fatigue, convulsions, but distinct from the symptoms of malaria. It was reported to be caused either by God’s will or the mother’s food consumption when the child was young. Herbal baths were the primary form of treatment. Included in the calculations for respiratory-related ailments (Table 1) were several recipes mentioned by Fang women for respiratory-related folk illnesses, including onkoe abijel: “respiratory problems caused by bad water during delivery,” onkouabial: “bad lungs after birth,” and ebulonkuk: “bad lungs caused by sorcery”.
Mothers’ knowledge of treating folk illnesses with plants
Aside from the use of plants for intestinal cleansing, fewer women knew how to treat folk illnesses than biomedical illnesses (Table 1). In Bénin, percentages of mothers who knew recipes for them ranged from 80% for atita to 65% for ka. In Gabon, over two-third of all participants knew herbal treatments for common children’s folk illnesses. With the exception of fontanels and walk early, Beninese folk illnesses like atita and ka were unknown to Gabonese mothers, while fesses rouges and la rate were not known in Bénin. Although the terms and perceived causes of atita in Bénin and fesses rouges in Gabon do not coincide, the two folk illnesses were somewhat similar in description. The folk illness pogha was only mentioned as an illness by mothers in the Gabonese department of Ngounie.
Health-seeking behaviors of Beninese mothers
Although there was little consensus on one preference for healthcare (Table 2), Beninese women in our study generally reported starting to treat their children with medicinal herbs, following up with biomedical care, and seeking traditional healers as a third resort. An 80-year old Mina woman said “Traditional medicine is first. Some use the hospital first, for example for fever or if one needs blood. A traditional healer is called upon to consult the fa (oracle) and for sacrifices”. Women who reported to never consult traditional healers mentioned the church and prayer as spiritual forms of treatment. Self-administered herbal medicine was reported to be preferred for treating children’s illnesses due to its ability to help defecate well, its use as preventative medicine, and its perceived effectiveness. Respondents often mentioned using plants to self-treat for a certain number of days (ranging from two days to one week) and then seeking biomedical care. Biomedicine was acknowledged to have the advantage of having advanced technology and materials but was perceived as being more expensive. A 36-year old Yoruba woman said, “Traditional medicine is used for constipation and atita- those you can treat at home. Modern medicine is used for difficult cases- they are better equipped. Traditional healers are consulted for superhuman cases because they know more about this domain”. Advanced forms of illnesses, especially malaria, were commonly reported to be treated with biomedicine. Seeking traditional healers to treat victims of sorcery and folk illnesses were strong themes. Traditional healers were reported to treat illnesses “that surpass the knowledge of doctors,” and for causes such as sorcery or witchcraft. A minority of mothers reported that common folk illnesses and asthma were “men’s knowledge,” outside of the maternal domain of skills. It was not clear if men’s knowledge meant the specialized knowledge of (male) traditional healers or more generally, fathers in the community. An 80 year old Fon woman said, “First try to treat at home with herbs for a couple of days. If they do not work, go to the hospital. If this does not work, go to a traditional healer. Asthma and fetus health are men’s knowledge. Fontanels are traditional healers’ knowledge”.
Table 2. Most frequent responses by mothers to healthcare seeking options question in Bénin (N = 43) and Gabon (N = 38).
| Response | % of mothersBénin | % of mothersGabon |
| Ranking of three health care options | ||
| First choice self-treatmentwith plants | 42 | 29 |
| First choice biomedicine(malaria, anemia, fever) | 16 | 32 |
| First choicebiomedicine (always) | 0 | 21 |
| First choicetraditional healer | 7 | 18 |
| Second choicebiomedicine | 30 | 13 |
| Second choice self-treatmentwith plants | 0 | 11 |
| Third choicetraditional healer | 23 | 3 |
| Never consulttraditional healer | 5 | 11 |
| Healthcare choice for specific cases | ||
| Traditional healerfor sorcery | 44 | 5 |
| Biomedicine for advancedcases (malaria, anemia) | 35 | 5 |
| Self-treat with plantsfor specific illnesses(diabetes, measles, stomachache) | 21 | 13 |
| Self-treat with plantsfor simple cases(malaria, diarrhea) | 28 | 0 |
| Traditional healerfor specific cases(fontanels, paralysis) | 12 | 8 |
| Men for specificillnesses (walk early, asthma) | 9 | 0 |
Health-seeking behaviors of Gabonese mothers
There was also a large range of responses from the Gabonese women involved in our study (Table 2). Nearly the same number of Gabonese mothers preferred self-treatment as a first form of healthcare as mothers who preferred treating children first with biomedicine. The strongest consensus of women cited specific illnesses, especially malaria, in which they would seek biomedical care directly. A 40-year old Obamba woman said “Use modern medicine for malaria, etc. We’re evolved for serious illness. Use traditional medicine if modern medicine doesn’t work, or if it’s not serious. A ganga is outdated, we no longer use them”. However, other women favored the consultation of a ganga, the spiritual leader of the community, or the nyembe, the spirit in a women’s secret society, in order to know where to treat the illness. This was a reoccurring theme, suggesting a strong the role of spirituality and religion in childcare, especially for folk illnesses. A 50 year old Fang woman said, “One should seek modern medicine for an operation; injections go straight to the blood and therefore work faster… Traditional medicine depends on God’s grace; prayer helps too. Go to a ganga for sorcery”. We found a reoccurring theme among Gabonese mothers that three systems were largely complementary. A 42-year old Fang woman said: “Try traditional medicine, if it does not work, the genies (spirits) will tell you to go to modern medicine. Work with the spirits! Between modern medicine and traditional medicine, there is a good collaboration. Gabon is currently in good position between the two systems”. A 61-year old Omiene women said “The three systems are complementary; you will find a solution between the three. It also depends on one’s belief system; some people are hesitant to go to a ganga”.
Discussion and Conclusion
Biomedical illnesses and their treatment
The majority of participants from Bénin and Gabon knew herbal treatments to treat the top causes of infant mortality: respiratory problems (98%, 84% respectively), malaria (95%, 87%), and diarrhea (95%, 89%). This outcome suggests that traditional medicine, and more specifically mothers’ knowledge of plants, is a major factor in the management of these common childhood health ailments. Even though mothers were knowledgeable on treating these illnesses, however, they also distinguished situations where they would seek biomedical care prior to using domestic medicine, such as complicated cases of malaria, anemia, or fever. Studies in other African countries also found that mothers preferred to treat malaria with biomedical care [27]. Only a few mothers mentioned diarrhea specifically as a case that they would seek biomedical care as a first option, suggesting diarrhea is largely treated by mothers with plants as was found in a recent study in Sierra Leone [28]. Likewise, respiratory ailments were not specifically mentioned as a case for seeking biomedical care. The high percentage of women who know how to treat these illnesses and the high number of plants attributed to their treatment suggest a parallel recognition of major causes of infant morbidity and mortality between the mothers and the statistics of the WHO. This agreement between medical priorities is not always the case, in a similar study on women’s health in Bénin and Gabon, we found that local and biomedical priorities did not coincide [29].
Folk illnesses and their treatment
Folk illnesses ranked directly after the major biomedical illnesses for children in terms of mothers’ medicinal plant knowledge. Our research supports ethnobotanical studies from other parts of the world that have indicated local populations commonly prefer to treat folk illnesses with traditional medicine [5], [30]–[31]. While many participants in our study knew herbal remedies to treat folk illnesses, it is clear that traditional healers and religion have a strong role in this domain. Men, more generally speaking, were also regarded as having specialized knowledge in Bénin. Fathers also have a role in the treatment of children’s illnesses, in terms of their own knowledge of medicinal plants [6] and their role in family decision-making [27].
Folk illnesses are of interest to biomedical health care providers, not only because they often make up a significant portion of local health complaints [5] but they may address underlying neglected diseases. Fontanels are common children’s folk illnesses around the world, and in other African countries such as Swaziland, Zimbabwe, Botswana and Malawi [32]. Certain (bulging or sinking) appearances of the fontanels may be symptoms of a range of disorders from dehydration to malnutrition to Down Syndrome [33]. Moreover, when mothers apply paste on the fontanel prior to arriving at the hospital, doctors cannot fully assess the fontanel (because of the plant pomades) and may misdiagnose the child’s illness. La rate resembles the symptoms of sickle-cell disease, a common yet neglected illness of children in Western Africa [34], especially its characteristic concentrated pain on the left side and spleen enlargement [35]. This overlap is a fertile ground for improved research and educational programs on sickle cell disease [36]. Enemas for intestinal cleanses, especially for newborns and small children, were a common practice in both countries. In the Ivory Coast, Gottlieb [37] found that enemas were used to make a baby defecate at a given time. Biomedical research has highlighted the danger in using enemas, especially among young children [38].
Even if these illnesses are not recognized as biological in nature, their treatment nevertheless has consequences, either positive or negative, on children’s health. Taking local perspectives and treatments into account not only informs biomedicine of cultural concepts of illness and healing [39], it also facilitates an understand of plant’ effects through pharmacological studies [40], and enables an understanding of how traditional systems of healing and biomedicine are already interacting on the ground [41].
Complementarity of three systems
The lack of any one definitive pattern of healthcare-seeking behavior among mothers in our study reflected the truly pluralistic healthcare systems of both countries [1], the dynamic process of deciding how to care for children [15], and the fact that mothers see the three African systems of healthcare as largely complementary. Mothers’ general pattern of resort [42] was to self-treat with plants first, seek biomedical care for specific illnesses or as a second source of healthcare and to consult the spiritual realm, including gangas and the nyembe in Gabon, to treat folk illnesses. However, as found in a recent study in South Africa [43], this pattern varied according to illness; each healthcare option was seen to have specific advantages and disadvantages. Biomedicine was perceived to have the advantage of advanced technology and materials, especially for treatments related to blood transfusions. Some mothers in Bénin reported a preference of using self-collected herbal medicine over biomedical care due to the expensive of modern treatment.
Future research can take demographic and socio-economic data into account to further the understanding of preferences for childcare treatment [28]. Additionally, our research did not explore mothers’ attitudes towards the quality of the different healthcare options. Future studies can ask women if a positive experience with one form of treatment would influence future decisions. Infant and child healthcare will be enriched if local knowledge, illness concepts, and medicinal plants fit into a larger framework that studies healthcare from a community perspective [1], including researchers from outside the biomedical field [5]. With the Millennium Development Goals concluding in 2015, and the reality that both countries have not met their targets of reducing infant mortality rates [22], [24], there is a renewed opportunity for infant healthcare initiatives to become more comprehensive.
Supporting Information
Species cited in 43 questionnaires in Bénin: scientific botanical name, vernacular plant name(s), plant part used, preparation, use category and collection number.
(DOCX)
Species cited in 38 questionnaires in Gabon: scientific botanical name, vernacular plant name(s), plant part used, preparation, use category and collection number.
(DOCX)
Acknowledgments
In Bénin, we would like to thank the professors at the University of Abomey-Calavi, especially A. Akoegninou and B. Sinsin, as well as the staff of the National Herbarium of Bénin (BEN), and l’Institut de Développement et d’Echanges Endogènes (IDEE). We are grateful to S. Ruysschaert, K. Ostertag, and L. Atindehou for their assistance in the Bénin fieldwork. The Gabon fieldwork was supported by the research staff at L’Institut de Pharmacopée et de Médecine Traditionnelles (IPHAMETRA), the National Herbarium of Gabon (LBV), HB Bourobou, le Centre National de la Recherche Scientifique et Technologique (CENAREST), and the Agence Nationale des Parcs Nationaux (ANPN) in Gabon. The authors would like to share a special thanks to E. van Vliet E, H. Eyi Ndong, J.P. Ongoda, A. Izouret, and the Grand Kami of Assiami for their assistance with the questionnaires. In the Netherlands, we would like to thank M. Sosef for his logistical support and the expert botanists at Wageningen University for their assistance with plant identification.
Data Availability
The authors confirm that, for approved reasons, there are some access restrictions on the data underlying the findings. The botanical vouchers collected for this study are publically available at the three herbaria involved in this study and online at the on-line Global Biodiversity Information Facility (www.gbif.org). Due to ethical restrictions, the interview data are available upon request to Johan Mols, Naturalis Research and Education sector (johan.mols@naturalis.nl), David Heijkamp, Naturalis ICT sector (david.heijkamp@naturalis.nl), or the corresponding author (alexandra.towns@naturalis.nl).
Funding Statement
This research was funded by the Netherlands Organization for Scientific Research (NWO), Vidi grant nr. 864.09.00 (http://www.nwo.nl/en). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. van der Geest S (1997) Is there a role for traditional medicine in basic health services in Africa? A plea for a community perspective. Trop Med Int Heal 2(9): 903–11. [DOI] [PubMed] [Google Scholar]
- 2. Nyamongo IK (2002) Health care switching behaviour of malaria patients in a Kenyan rural community Soc Sci Med. 54(3): 377–86. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Traditional medicine. Available: http://www.who.int/mediacentre/factsheets/fs134/en/. Accessed 2013 Apr 29.
- 4. Pfeiffer J, Butz R (2005) Assessing cultural and ecological variation in ethnobiological research: the importance of gender. J Ethnobiol 25(2): 240–278. [Google Scholar]
- 5. Vandebroek I (2013) Intercultural health and ethnobotany: How to improve healthcare for underserved and minority communities? J Ethnopharmacol 148(3): 746–754. [DOI] [PubMed] [Google Scholar]
- 6. McDade TW, Reyes-García V, Blackinton P, Tanner S, Huanca T, et al. (2007) Ethnobotanical knowledge is associated with indices of child health in the Bolivian Amazon. Proc Natl Acad Sci USA 104(15): 6134–6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pearce TO (1993) Lay Medical Knowledge in an African Context. In Lindenbaum S, Lock M, editors. Knowledge, Power and Practice: The Anthropology of Medicine and Everyday Life. Berkeley: University of California Press. 150–165. [Google Scholar]
- 8. Geissler PW, Harris SA, Prince RJ, Olsen A, Odhiambo RA, et al. (2002) Medicinal plants used by Luo mothers and children in Bondo district, Kenya. J Ethnopharmacol 83(1–2): 39–54. [DOI] [PubMed] [Google Scholar]
- 9. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, et al. (2010) Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375(9730): 1969–1987. [DOI] [PubMed] [Google Scholar]
- 10. Miller EM (2011) Maternal health and knowledge and infant health outcomes in the Ariaal people of northern Kenya. Soc Sci Med 73(8): 1266–1274. [DOI] [PubMed] [Google Scholar]
- 11. Tanner S, Chuquimia-Choque ME, Huanca T, McDade TW, Leonard WR, et al. (2011) The effects of local medicinal knowledge and hygiene on helminth infections in an Amazonian society. Soc Sci Med 72(5): 701–709. [DOI] [PubMed] [Google Scholar]
- 12. Rutherford M (2010) How access to health care relates to under-five mortality in sub-Saharan Africa: systematic review. Trop Med Int Heal 15(5): 508–519. [DOI] [PubMed] [Google Scholar]
- 13. Beiersmann C, Sanou A (2007) Malaria in rural Burkina Faso: local illness concepts, patterns of traditional treatment and influence on health-seeking behaviour. Malar J 9: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Helman CG (2007) Culture, Health and Illness. London: Hodder Arnold. 266–271. [Google Scholar]
- 15. Colvin CJ, Smith HJ, Swartz A, Ahs JW, de Heer J, et al. (2013) Understanding careseeking for child illness in sub-Saharan Africa: a systematic review and conceptual framework based on qualitative research of household recognition and response to child diarrhoea, pneumonia and malaria. Soc Sci Med 86: 66–78. [DOI] [PubMed] [Google Scholar]
- 16. Nsungwa-Sabiiti J, Källander K, Nsabagasani X, Namusisi K, Pariyo G, et al. (2004) Local fever illness classifications: implications for home management of malaria strategies. Trop Med Int Heal 9(11): 1191–1199. [DOI] [PubMed] [Google Scholar]
- 17. de Zoysa I, Carson D, Feachem R, Kirkwood B, Lindsay-Smith E, et al. (1984) Perceptions of childhood diarrhoea and its treatment in rural Zimbabwe. Soc Sci Med 19(7): 727–734. [DOI] [PubMed] [Google Scholar]
- 18. Green EC (1985) Traditional healers, mothers and childhood diarrheal disease in Swaziland: the interface of anthropology and health education. Soc Sci Med 20(3): 277–285. [DOI] [PubMed] [Google Scholar]
- 19. Straus L, Munguambe K, Bassat Q, Machevo S, Pell C, et al. (2011) Inherent illnesses and attacks: an ethnographic study of interpretations of childhood Acute Respiratory Infections (ARIs) in Manhiça, southern Mozambique. BMC Public Health 11(1): 556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mogensen HO (2000) False teeth and real suffering: the social course of ‘germectomy’ in eastern Uganda. Cult Med Psychiatry 24(3): 331–351. [DOI] [PubMed] [Google Scholar]
- 21.CIA. The World Factbook: Benin 2013. Available: https://www.cia.gov/library/publications/the-world-factbook/geos/bn.html. Accessed 2013 Apr 29.
- 22.UNDP. International Human Development Indicators - UNDP: Benin 2013. Available: http://hdrstats.undp.org/en/countries/profiles/BEN.html. Accessed 2013 Apr 29.
- 23.CIA. The World Factbook: Gabon 2013. Available: https://www.cia.gov/library/publications/the-world-factbook/geos/gb.html. Accessed 2013 Apr 29.
- 24.UNDP. International Human Development Indicators - UNDP: Gabon 2013. Available: http://hdrstats.undp.org/en/countries/profiles/GAB.html. Accessed 2013 Apr 29.
- 25.Martin GJ (2004) Ethnobotany: a methods manual. London: Earthscan. 1–269. [Google Scholar]
- 26.International Society of Ethnobiology (ISE). ISE Code of Ethics (with 2008 additions), Available: http://ethnobiology.net/code-of-ethics/. Accessed 2013 Nov 23.
- 27. Montgomery CM, Mwengee W, Kong’ong’o M, Pool R (2006) To help them is to educate them’: power and pedagogy in the prevention and treatment of malaria in Tanzania. Trop Med Int Heal 11(11): 1661–1669. [DOI] [PubMed] [Google Scholar]
- 28. Bakshi S, McMahon S, George A (2013) The Role of Traditional Treatment on Health Care Seeking by Caregivers for Sick Children in Sierra Leone: Results of a Baseline Survey. Acta Trop 127: 46–52. [DOI] [PubMed] [Google Scholar]
- 29. Towns AM, van Andel TR (2014) Comparing local perspectives on women’s health with statistics on maternal mortality: an ethnobotanical study in Bénin and Gabon. BMC Complement Altern Med 14: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Quinlan MB (2010) Ethnomedicine and ethnobotany of fright, a Caribbean culture-bound psychiatric syndrome. J Ethnobiol Ethnomed 6(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mathez-Stiefel SL, Vandebroek I, Rist S (2012) Can Andean medicine coexist with biomedical healthcare? A comparison of two rural communities in Peru and Bolivia. J Ethnobiol Ethnomed 8(1): 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kay MA (1993) Fallen fontanelle: Culture bound or cross-cultural? Med Anthropol 15(2): 137–156. [DOI] [PubMed] [Google Scholar]
- 33. Kiesler J, Ricer R (2003) The abnormal fontanel. Am Fam Physician 67(12): 2547–2552. [PubMed] [Google Scholar]
- 34. Grosse SD, Odame I, Atrash HK, Amendah DD, Piel FB, et al. (2011) Sickle cell disease in Africa: a neglected cause of early childhood mortality. Am J Prev Med 41(6): S398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Meier E, Miller J (2012) Sickle cell disease in children. Drugs 72(7): 895–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Makani J, Williams TN, Marsh K (2007) Sickle cell disease in Africa: burden and research priorities. Ann Trop Med Parasitol 101(1): 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gottlieb A (2004) The afterlife is where we come from. Chicago: University of Chicago Press. 1–404. [Google Scholar]
- 38. Bland RM, Rollins NC, Van den Broeck J, Coovadia HM (2004) The use of non-prescribed medication in the first 3 months of life in rural South Africa. Trop Med Int Heal 9(1): 118–24. [DOI] [PubMed] [Google Scholar]
- 39.Etkin NL (1998) Cultural constructions of efficacy. In The context of medicines in developing countries. Springer Netherlands. 299–326.
- 40. Reyes-García V (2010) The relevance of traditional knowledge systems for ethnopharmacological research: theoretical and methodological contributions. J Ethnobiol Ethnomed 6(1): 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Langwick S (2008) Articulate(d) bodies: Traditional medicine in a Tanzanian hospital. American Ethnologist 35(3): 428–439. [Google Scholar]
- 42. Ryan GW (1998) What do sequential behavioral patterns suggest about the medical decision-making process?: modeling home case management of acute illnesses in a rural Cameroonian village. Soc Sci Med 46(2): 209–225. [DOI] [PubMed] [Google Scholar]
- 43. Friend-du Preez N, Cameron N, Griffiths P (2013) ‘So they believe that if the baby is sick you must give drugs…’ The importance of medicines in health-seeking behaviour for childhood illnesses in urban South Africa. Soc Sci Med 92: 43–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Species cited in 43 questionnaires in Bénin: scientific botanical name, vernacular plant name(s), plant part used, preparation, use category and collection number.
(DOCX)
Species cited in 38 questionnaires in Gabon: scientific botanical name, vernacular plant name(s), plant part used, preparation, use category and collection number.
(DOCX)
Data Availability Statement
The authors confirm that, for approved reasons, there are some access restrictions on the data underlying the findings. The botanical vouchers collected for this study are publically available at the three herbaria involved in this study and online at the on-line Global Biodiversity Information Facility (www.gbif.org). Due to ethical restrictions, the interview data are available upon request to Johan Mols, Naturalis Research and Education sector (johan.mols@naturalis.nl), David Heijkamp, Naturalis ICT sector (david.heijkamp@naturalis.nl), or the corresponding author (alexandra.towns@naturalis.nl).