Abstract
Background:
Spinal bracing is widely utilized in patients with moderate severity adolescent idiopathic scoliosis with the goal of preventing curve progression and therefore preventing the need for surgical correction. Bracing is typically initiated in patients with a primary curve angle between 25 and 40 degrees, who are Risser sign 0 to 2 and <1-year postmenarchal. The purpose of this study is to determine whether nighttime bracing using a Charleston bending brace is effective in preventing progression of smaller curves (15 to 25 degrees) in skeletally immature, premenarchal female patients relative to current standard of care (observation for curves <25 degrees).
Methods:
Premenarchal, Risser 0 female patients presenting to 2 pediatric orthopaedic specialty practices for evaluation of idiopathic scoliosis with Cobb angle measurements between 15 and 25 degrees were selected. They were randomized by location to receive nighttime bending brace treatment or observation. Patients in the observation group were converted to fulltime TLSO wear if they progressed to >25 degrees primary curve Cobb angle. Curve progression was monitored with minimum 2-year follow-up.
Results:
Sixteen patients in the observation group and 21 patients in the bracing group completed 2-year follow-up. All patients in the observation group progressed to fulltime bracing threshold. In the nighttime bracing group, 29% of the patients did not progress to 25 degrees primary curve magnitude. Rate of progression to surgical magnitude was similar in the 2 groups.
Conclusions:
Risser 0 patients presenting with mild idiopathic scoliosis are at high risk for progression to >25 degrees primary curve magnitude. Treatment with the Charleston nighttime bending brace may reduce progression to full-time bracing threshold. No difference in progression to surgical intervention was shown between nighttime bracing and observation for small curves.
Level of Evidence:
Level II—therapeutic study (prospective comparative study).
Key Words: scoliosis, bracing, Charleston Brace, early idiopathic scoliosis
This is a prospective cohort controlled study of nighttime bracing versus no treatment for adolescent idiopathic scoliosis (AIS) in young girls with mild curves. In 1 institution, premenarchal, Risser 0 girls with primary scoliotic curves between 15 and 25 degrees were treated with nighttime Charleston bending brace until skeletal maturity and in another center were observed until progression to standard bracing criteria. We hypothesize that (a) this patient population is at high risk for curve progression and (b) that nighttime bracing using a Charleston bending brace is effective in preventing progression of smaller curves (15 to 25 degrees) in skeletally immature, premenarchal female patients relative to current standard of care (observation for curves <25 degrees) to prevent the need for fulltime bracing.
Spinal bracing is widely utilized in patients with moderate severity AIS with the goal of preventing curve progression and therefore preventing the need for surgical correction.1 The generally accepted parameters for initiation of brace treatment in AIS coincide with the Scoliosis Research Society criteria for standardization of bracing studies. These criteria are: primary curve angle between 25 and 40 degrees, age over 10 when brace is prescribed, Risser sign 0 to 2, <1-year postmenarchal, and no prior treatment.2 Despite the presence of these criteria for the last 15 years, there remains a significant debate with regard to the efficacy of bracing and a paucity of high-quality studies to show efficacy.3 Furthermore, many different brace designs exist with conflicting evidence on their relative efficacy.1,4–9
AIS is well documented to progress most rapidly during the pubertal growth spurt, and if bracing is to be effective in preventing progression than it must be prescribed during this period of rapid growth. This serves as the basis for the SRS guidelines to target the patient population with the most potential benefit. However, peak growth velocity occurs during menarche, before radiographic appearance of the iliac apophysis. Although including recently postmenarchal Risser 1 and 2 patients allows for larger study size, there is concern that progression rates may be highest in the premenarchal, Risser 0 population and these patients may benefit from early intervention even with small curves at presentation.
The Charleston brace is a nighttime-only bending brace that has been shown to be effective in controlling curve progression in multiple studies.8–12 Biomechanical analysis has shown that significant compressive stress relayed to the spine on the convexity of the scoliotic curve tensile stress on the concavity.13 This may allow for growth modulation during spinal growth and contribute to efficacy. Furthermore, the psychosocial effects of bracing on the AIS population are significant and nighttime-only brace wear may improve patient acceptance and compliance with treatment, although this has not been definitively shown.14,15
METHODS
Premenarchal, Risser 0 female patients presenting to 2 pediatric orthopaedic specialty practices for evaluation of idiopathic scoliosis with Cobb angle measurements between 15 and 25 degrees were identified for inclusion in the study. Informed consent was obtained. Patients were excluded for prior treatment (bracing or surgery), nonidiopathic etiology, or unwillingness to participate in the study. Assignment to treatment versus control arms was determined by location of presentation. All patients from the treatment group site were assigned to nighttime bracing with the Charleston bending brace at the time of presentation and all patients from the control site were assigned to observation at initial presentation. Patients were followed up at approximately 6-month intervals with full-standing posteroanterior scoliosis radiographs taken at each visit. An additional visit shortly after initiation of brace treatment (if braced) was performed to check brace fit and curve correction with in-brace radiographs. Curve magnitude, Risser sign, menarchal status, and self-reported percentage of brace wear compliance (if braced) were recorded at each visit. The treating physician recorded the measurements and was unaware of whether the patient was enrolled in the study. All radiographs were reviewed by a research fellow and any discrepancy >3 degrees was submitted to a reviewer who made the final determination. In the control group, fulltime TLSO bracing was instituted if progression to 25 degrees Cobb angle or over 5 degrees was observed and this was continued until skeletal maturity. In the treatment group, nighttime Charleston bracing was continued through skeletal maturity. Addition of daytime TLSO brace wear was recommended for curves progressing past 25 degrees despite nighttime bracing. They were maintained in the Charleston brace at night with or without daytime TLSO wear. Surgical intervention was offered in both groups at the discretion of the treating surgeon if the curve progressed to surgical magnitude (>50 degrees). Patients were followed up to skeletal maturity and minimum follow-up was 2 years. All patients were analyzed regardless of compliance (intent-to-treat). Data were analyzed for comparability of treatment groups, progression to fulltime bracing threshold (25 degrees), progression over 5 and 10 degrees of primary curve Cobb angle magnitude during the treatment period, and progression to surgical intervention. Two-sample t test was used to analyze for difference between groups for continuous variables and the 1-tail Fisher exact test was used for binary variables. Curve type was not analyzed due to insufficient sample size. Compliance data were not analyzed due to the proven unreliability of self-reported compliance data.
RESULTS
Twenty-three patients were enrolled in the control group and 23 in the treatment group. Of these, 9 failed to complete 2-year follow-up and were therefore excluded, leaving 16 in the control group and 21 in the treatment group for data analysis. The groups were similar at presentation (Table 1). Average curve magnitude was 19 degrees in both groups. In the control group, all patients progressed to fulltime bracing threshold (Fig. 1). Eight patients (50%) progressed >5 degrees but <10 degrees and the remaining 8 patients (50%) progressed >10 degrees. In the treatment group, 6 patients (29%) did not progress and were continued in nighttime bracing through skeletal maturity (Fig. 2). This was statistically significant (P=0.023). Four patients (19%) progressed >5 degrees but <10 degrees and the remaining 11 patients (52%) progressed >10 degrees. Two patients in the control group (12%) and 4 in the treatment group (19%) progressed to surgical intervention despite bracing. This was not statistically significant (P=0.472).
TABLE 1.
Group Demographics Show No Difference Between Groups at Time of Inclusion
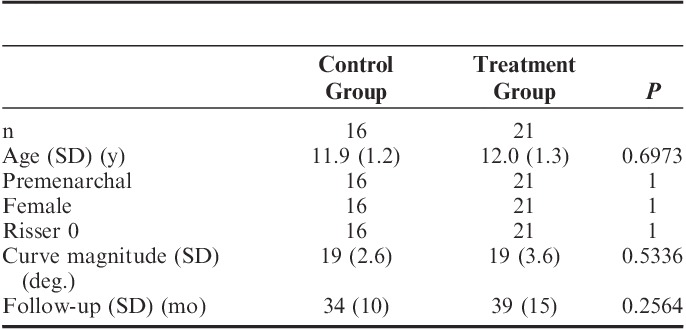
FIGURE 1.
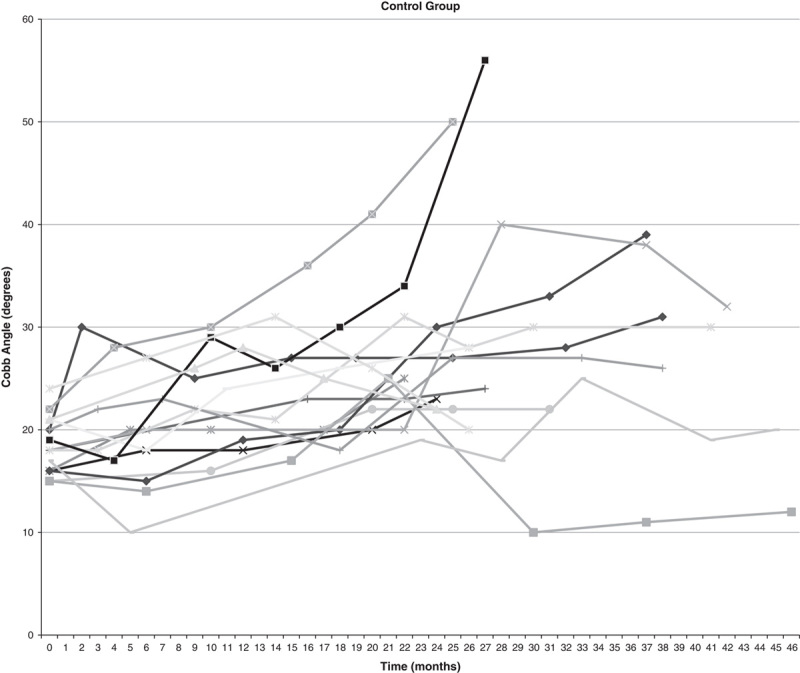
Curve progression for each patient in control group.
FIGURE 2.
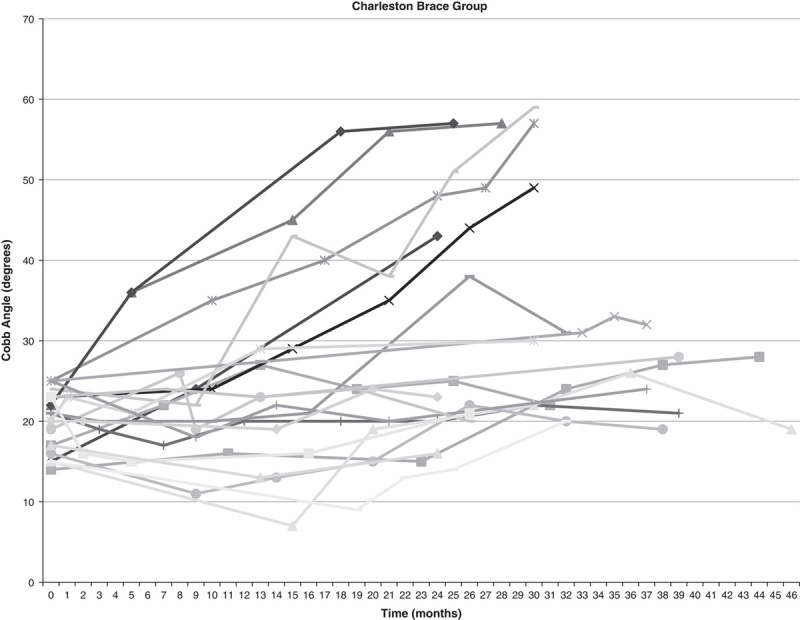
Curve progression for each patient in treatment group.
DISCUSSION
This study highlights a particular subset of patients with idiopathic scoliosis that have not been well studied in an independent manner. We show a significant rate of curve progression in these Risser 0, premenarchal girls despite presenting with small magnitude curves (>15 degrees but <25 degrees). With observation, 100% of these patients progressed to standard criteria for fulltime bracing. With nighttime Charleston brace use, 29% were maintained without progression. Although the majority of patients progressed despite bracing, this still represents a significant decrease in progression. The hypothesis that nighttime Charleston bracing would reduce the need for fulltime bracing was confirmed. Rate of progression to surgical intervention was not statistically significant; however, this study did not include enough patients to make a difference in observed surgical rate meaningful. We also did not have electronically monitored braces for accurate compliance data. Although brace wear compliance is an important factor and would be helpful for determining true efficacy, we feel that the intention-to-treat model with a non–brace-wearing control group provides the most accurate assessment of the efficacy of this treatment model.
This study purposefully does not meet the SRS criteria for brace studies. Although we agree that the SRS criteria are valuable for generating a body of literature that is relevant and helpful to elucidate the value of bracing in the typically presenting AIS patient, it is our opinion that the patient population represented in this study is at particular risk for progression and should be singled out for analysis. The high rate of progression in the control group confirms this opinion, and the inclusion of a prospective control group strengthens the study. All Risser 0, premenarchal girls presenting with curve angles from 15 to 25 degrees progressed to >25 degrees with observation alone. The high rate of progression in this specific subset of girls between 15 and 25 degrees has not been previously identified, perhaps because the previous natural history studies have included more mature patients, or immature patients with curves <15 degrees.
Both fulltime and nighttime bracing present psychosocial challenges to acceptance of treatment and compliance that were not addressed in this study. It is our opinion that nighttime bracing is better accepted by patients, as there is no stigma associated with wearing the brace to school and they are able to participate in all social and athletic activities without encumbrance. Acceptance of treatment is particularly important in this population as they are skeletally younger at the time of presentation and will require a longer period of treatment to reach skeletal maturity.
It remains to be proven whether bracing will influence the need for surgery relative to natural history. In this study we had similar number of patients progress to surgical intervention regardless of treatment. On the basis of the results of this study, it is our conclusion that nighttime bracing with the Charleston brace should be considered for Risser 0, premenarchal girls with scoliosis of 15 to 25 degrees due to the high risk for progression without treatment.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Sponseller PD. Bracing for adolescent idiopathic scoliosis in practice today. J Pediatr Orthop. 2011;31supplS53–S60. [DOI] [PubMed] [Google Scholar]
- 2.Richards BS, Bernstein RM, D’Amato CR, et al. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976). 2005;30:2068–2075discussion 76-7. [DOI] [PubMed] [Google Scholar]
- 3.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2010;1:CD006850. [DOI] [PubMed] [Google Scholar]
- 4.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Spine (Phila Pa 1976). 2010;35:1285–1293. [DOI] [PubMed] [Google Scholar]
- 5.Negrini S, Atanasio S, Fusco C, et al. Effectiveness of complete conservative treatment for adolescent idiopathic scoliosis (bracing and exercises) based on SOSORT management criteria: results according to the SRS criteria for bracing studies—SOSORT Award 2009 Winner. Scoliosis. 2009;4:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janicki JA, Poe-Kochert C, Armstrong DG, et al. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27:369–374. [DOI] [PubMed] [Google Scholar]
- 7.Yrjonen T, Ylikoski M, Schlenzka D, et al. Effectiveness of the Providence nighttime bracing in adolescent idiopathic scoliosis: a comparative study of 36 female patients. Eur Spine J. 2006;15:1139–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gepstein R, Leitner Y, Zohar E, et al. Effectiveness of the Charleston bending brace in the treatment of single-curve idiopathic scoliosis. J Pediatr Orthop. 2002;22:84–87. [PubMed] [Google Scholar]
- 9.Trivedi JM, Thomson JD. Results of Charleston bracing in skeletally immature patients with idiopathic scoliosis. J Pediatr Orthop. 2001;21:277–280. [PubMed] [Google Scholar]
- 10.Howard A, Wright JG, Hedden D. A comparative study of TLSO, Charleston, and Milwaukee braces for idiopathic scoliosis. Spine (Phila Pa 1976). 1998;23:2404–2411. [DOI] [PubMed] [Google Scholar]
- 11.Price CT, Scott DS, Reed FR, Jr, et al. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston Bending Brace: long-term follow-up. J Pediatr Orthop. 1997;17:703–707. [PubMed] [Google Scholar]
- 12.Price CT, Scott DS, Reed FE, Jr, et al. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace. Preliminary report. Spine (Phila Pa 1976). 1990;15:1294–1299. [DOI] [PubMed] [Google Scholar]
- 13.Clin J, Aubin CE, Parent S, et al. A biomechanical study of the Charleston brace for the treatment of scoliosis. Spine (Phila Pa 1976). 2010;35:E940–E947. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, He D, Gao J, et al. Changes in life satisfaction and self-esteem in patients with adolescent idiopathic scoliosis with and without surgical intervention. Spine (Phila Pa 1976). 2011;36:741–745. [DOI] [PubMed] [Google Scholar]
- 15.Climent JM, Sanchez J. Impact of the type of brace on the quality of life of adolescents with spine deformities. Spine (Phila Pa 1976). 1999;24:1903–1908. [DOI] [PubMed] [Google Scholar]


