Abstract
Introduction
While pain in multiple sclerosis (MS) is common, in many cases the precise mechanisms are unclear. Neuroimaging studies could have a valuable role in investigating the aetiology of pain syndromes. The aim of this review was to synthesise and appraise the current literature on neuroimaging studies of pain syndromes in MS.
Methods
We systematically searched PubMed and Scopus from their inception dates to the 2nd of April 2013. Studies were selected by predefined inclusion and exclusion criteria. Methodological quality was appraised. Descriptive statistical analysis was conducted.
Results
We identified 38 studies of variable methodology and quality. All studies but one used conventional structural magnetic resonance imaging, and the majority reported a positive association between location of demyelinating lesions and specific neuropathic pain syndromes. Most investigated headache and facial pain, with more common pain syndromes such as limb pain being relatively understudied. We identified a number of methodological concerns, which along with variable study design and reporting limit our ability to synthesise data. Higher quality studies were however less likely to report positive associations of lesion distribution to pain syndromes.
Conclusions
Further high quality hypothesis-driven neuroimaging studies of pain syndromes in MS are required to clarify pain mechanisms, particularly for the commonest pain syndromes.
Keywords: Pain, Multiple sclerosis, Magnetic resonance imaging, Review, Headache
Highlights
-
•
We reviewed neuroimaging studies of pain syndromes in multiple sclerosis (MS).
-
•
All studies investigated neuropathic pain or headache, mainly using structural MRI.
-
•
Most reported associations between location of demyelinating lesions and pain.
-
•
Culprit lesions were most commonly reported in the brainstem.
-
•
High quality hypothesis-driven neuroimaging studies of pain in MS are still needed.
1. Introduction
Multiple sclerosis (MS) is an inflammatory disease of the central nervous system (CNS), which is associated with demyelination and neurodegeneration (Compston and Coles, 2008). Pain has been recognised as a symptom of MS since the first descriptions of the disease (Charcot, 1872) and can broadly be classified as nociceptive or neuropathic (O'Connor et al., 2008). It is common – the overall point prevalence of pain in MS is around 50% (O'Connor et al., 2008) – and it is often ranked by patients as one of the most distressing symptoms of the disease (Kalia and O'Connor, 2005). In spite of the prevalence and clinical importance of pain in MS, its mechanisms remain poorly understood.
Magnetic resonance imaging (MRI) plays a crucial role both in the diagnosis of MS (Polman et al., 2011) and in clinical research applications. It is widely used to study both inflammatory lesions and non-lesional tissue changes in vivo (Bakshi et al., 2008). MRI is also an important tool in the study of pain mechanisms, and it is likely to play an increasing clinical role in the future (Wise and Tracey, 2006). Positron-emission tomography (PET) and single-photon emission-computed tomography (SPECT) have, in addition, proved invaluable in the study of neurotransmitter systems involved in pain.
While neuroimaging is separately established as a mainstay in the investigation of both MS and pain, the study of pain syndromes in MS by neuroimaging remains a developing field. Improved understanding of neuroradiological findings in MS pain could improve our understanding of its mechanisms, and in turn contribute to development of therapies. In order to identify gaps in knowledge, and highlight future research priorities, our review summarises and appraises existing studies of neuroimaging correlates of MS pain (using MRI, PET or SPECT) and assesses the neuroradiological evidence for aetiology of MS-related pain syndromes.
2. Materials and methods
Our primary outcome of interest was the radiological evidence for the aetiology of any pain syndrome in MS. We analysed findings of available studies in light of detailed methodological assessment and emphasised results of high quality hypothesis-driven studies. We anticipated a low number of available studies, and therefore included any pain syndrome described as associated with MS.
We searched PubMed and Scopus from their inception dates (1977 and 1960, respectively) to the 2nd of April 2013. Keywords used for the PubMed search included the medical subject heading (MeSH) terms “pain” and “multiple sclerosis” along with “magnetic resonance imaging” or “positron-emission tomography” or “tomography, emission-computed, single-photon”. Keywords used for the Scopus search included all entry terms of each MeSH term in PubMed and the MeSH terms themselves, combined in the same manner. We also hand-searched reference lists and consulted experts in the field to identify additional material.
We included all original English language studies examining neuroimaging correlates of pain in MS – using MRI, PET or SPECT imaging – in human adults. Three studies were excluded by the language criterion. We also excluded paediatric studies, studies of other demyelinating disorders, re-published data, and review articles.
We reviewed the titles and abstracts of identified studies and excluded duplicate references. Two reviewers (DS, PF) independently reviewed potentially relevant articles. Disagreements were resolved by consensus.
We then assessed quality of studies using the following 12 criteria relevant to our review objectives (adapted from Campbell et al., 2011): clearly stated research objective, recruitment procedure, and inclusion/exclusion criteria; description of sample demographics, participation rates, imaging protocol, and pain measurement instruments; image interpretation carried out without knowledge of subjects' pain status; participation rate above 70%; use of multivariate analysis; reporting of strength of effect, and acknowledgment of study limitations. Given the low number of identified studies, we did not exclude any studies on the basis of quality assessment. We also assessed the reporting of imaging methodology, clinical diagnostic criteria used, reported imaging findings, and methods used to investigate links between radiological findings and occurrence of pain syndromes. We conducted descriptive statistical analysis. We identified studies as case reports, case series, or investigational studies (defined here by any study with hypothesis-driven experimental design). This work was not submitted to an ethics committee because it is a systematic review of the literature.
3. Results
We found 902 candidate publications (Fig. 1). Thirty-eight met the inclusion criteria (Alstadhaug et al., 2008; Andrade et al., 2012; Athanasiou et al., 2005; Balasa and Bajko, 2010; Bentley et al., 2002; Broggi et al., 2004; Burkey and Abla-Yao, 2010; Carrieri et al., 2009; Cordella et al., 2009; Cruccu et al., 2009; da Silva et al., 2005; Davey and Al-Din, 2004; Deppe et al., 2013; de Santi et al., 2009; Donat, 2012; Eldridge et al., 2003; Fragoso and Brooks, 2007; Gass et al., 1997; Gee et al., 2005; Gentile et al., 2007; González-Quintanilla et al., 2012; Haas et al., 1993; Hellwig et al., 2006; Kister et al., 2010; Leandri et al., 1999; Liu et al., 2008; Marchettini et al., 2006; Meaney et al., 1995; Minagar and Sheremata, 2000; Nakashima et al., 2001; Pichiecchio et al., 2007; Ramirez-Lassepas et al., 1992; Svendsen et al., 2011; Tanei et al., 2010; Tortorella et al., 2006; Tosi et al., 1998; Vilisaar and Constantinescu, 2006; Yetimalar et al., 2008). Of these, 16 were case reports (Alstadhaug et al., 2008; Andrade et al., 2012; Bentley et al., 2002; Burkey and Abla-Yao, 2010; Carrieri et al., 2009; Davey and Al-Din, 2004; Donat, 2012; Gentile et al., 2007; González-Quintanilla et al., 2012; Haas et al., 1993; Leandri et al., 1999; Liu et al., 2008; Pichiecchio et al., 2007; Tanei et al., 2010; Tosi et al., 1998; Vilisaar and Constantinescu, 2006), nine were case series (Athanasiou et al., 2005; Cordella et al., 2009; de Santi et al., 2009; Fragoso and Brooks, 2007; Hellwig et al., 2006; Marchettini et al., 2006; Meaney et al., 1995; Minagar and Sheremata, 2000; Nakashima et al., 2001), and 13 were investigational studies (Balasa and Bajko, 2010; Broggi et al., 2004; Cruccu et al., 2009; da Silva et al., 2005; Deppe et al., 2013; Eldridge et al., 2003; Gass et al., 1997; Gee et al., 2005; Kister et al., 2010; Ramirez-Lassepas et al., 1992; Svendsen et al., 2011; Tortorella et al., 2006; Yetimalar et al., 2008). Characteristics of included investigational studies are detailed in Table 1. On quality assessment, the mean number of criteria fulfilled by the included investigational studies (n = 13) was six (range 3–12). Only Kister et al. (2010) fulfilled all the criteria. Four studies (Gee et al., 2005; Kister et al., 2010; Svendsen et al., 2011; Tortorella et al., 2006) fulfilled seven or more of the twelve criteria (Table 2).
Fig. 1.
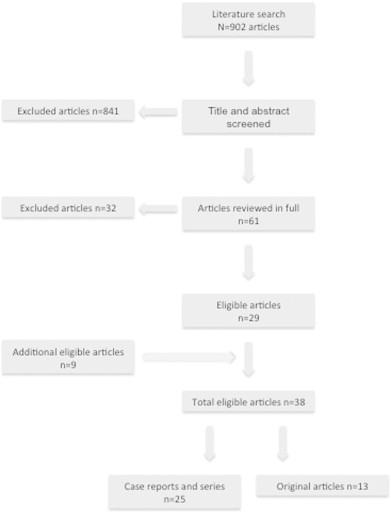
Flow diagram of the review procedure.
Table 1.
Characteristics of included investigational studies.
| Author (year) |
Country | Type of study | Study population (n=) | Main study focus | Assessment of pain | Imaging | Main findings |
|---|---|---|---|---|---|---|---|
| Balasa (2010) | Romania |
Retrospective, cross-sectional | 20 patients with TN (10 with MS and 10 without MS) | Evaluation of clinical differences in TN presentation and pharmacological treatment response in patients with and without MS | International Headache Society Classification (2004), Barrow Neurological Institute score of clinical pain intensity | MRI (1 T), no image acquisition or reading protocols defined |
MS patients had earlier onset TN, probably secondary to lesions in the trigeminal pathways, with overlapping characteristics and treatment response when compared to non-MS TN |
| Cruccu (2009) | Italy | Retrospective, cross-sectional | 130 MS patients (50 with TN, 30 with sensory trigeminal disturbances, and 50 controls) | Causes and mechanisms of MS-related TN | International Headache Society Classification (2004), neurological examination including sensory and trigeminal reflex testing | MRI, dedicated image acquisition protocol (although not specified), voxel-based brainstem analysis, read by neuroradiologists | The onset ages of MS and trigeminal symptoms were older in the TN group, and most patients in the TN and non-TN groups had abnormal trigeminal reflexes. In the TN group the highest probability of brainstem lesion was in the pontine trigeminal primary afferents |
| Deppe (2013) | Germany | Retrospective | 1 MS patient and 100 healthy controls | Investigate diffusion tensor imaging abnormalities in the thalamus related to a central pain syndrome comparing with controls | Describes the pain syndrome only as “episode of central pain and abnormal somatosensory and thermal sensations on the right hand side of the body” | MRI (3 T), well described imaging protocol and post-processing, data was obtained from a pilot study for a clinical trial, ROI analysis of the thalami | Temporary increase of the fractional anisotropy in the thalamus contralateral to the pain; a causative role is suggested |
| Gee (2005) | United States of America | Retrospective, cross-sectional | 277 MS patients | To determine if the prevalence of migraine-like headache in MS patients was associated with plaques in the brainstem or other locations |
International Headache Society Classification (1988), tailored questionnaire | MRI, contradictory information regarding image acquisition protocol, field strength and scanners; predefined reading protocol |
The presence of a midbrain plaque was associated with an increased likelihood of headache with migraine characteristics; lesions in other locations and lesion load were not associated with headache prevalence |
| Kister (2010) | United States of America | Cross-sectional | 204 MS patients | To assess the relative frequency of migraine in MS and to compare clinical and radiographic characteristics in MS patients with and without migraine | International Headache Society Classification (2004), tailored questionnaire to characterise headache and comorbidities adapted from the American Migraine Prevalence and Prevention Study, migraine severity assessed with Migraine Disability Assessment tool |
MRI (0.6, 1.5 and 3 T), image acquisition protocol defined (T2-w and pre- and post-contrast T1-w), images read by a neurologist and an expert in MS neuroradiology | Migraine frequency was threefold higher in MS patients than in controls, and was more symptomatic; no difference in number or distribution of plaques, or enhancing lesions between migraine and no-migraine groups |
| Ramirez-Lassepas (1992) | United States of America | Retrospective, cross-sectional | 11 MS patients | To study radicular pain as presenting MS symptom | – |
Myelography, computed tomography or MRI; no image acquisition or reading protocols defined | Acute radicular pain in the absence of demonstrable root compression may not be an uncommon presenting symptom in MS and may be associated with trauma; in two patients plaques in the spinal cord explained the symptoms |
| Svendsen (2011) | Denmark | Cross-sectional | 25 MS patients with sensory disturbances (13 with pain and 12 without pain) | To study location of plaques in MS patients with sensory disturbances with and without pain, and to ascertain if deafferentiation of spinothalamic tract was more common in the patients with pain | Structured pain interview, pain location in body map, neurological examination including bedside sensory examination | MRI (1.5 T), image acquisition protocol defined (brain — sagittal T1-w and T2-w and axial FLAIR, spine — sagittal T1-w and STIR axial T2-w), read by a neuroradiologist according to defined reading protocol |
No association between central pain and site of demyelination was found; central pain was associated with allodynia, suggesting central hyperexcitability |
| Tortorella (2006) | Italy | Retrospective | 58 patients with migraine and 79 MS patients (37 with and 42 without migraine) | Evaluate if red nucleus, substantia nigra and periaqueductal grey matter were involved by MRI-detectable structural abnormalities in migraine patients, and to investigate their frequency and extent in MS patients with migraine |
International Headache Society Classification (2004) | MRI (1.5 T), defined image acquisition protocol (axial PD/T2-w), read by two observers using a defined reading protocol | Brainstem lesions were frequent in non-MS migraine, but did not seem associated with aura; demyelinating lesions in the red nucleus, substantia nigra and periaqueductal grey matter might be among the factors responsible for migraine in MS |
| Broggi (2004) | Italy | Cross-sectional, prospective | 35 MS patients who underwent MVD for TN | To clarify the role of MVD in the treatment of TN in MS | Post-operative presence and intensity of residual facial pain and subsequent treatment for TN | MRI (0.5 or 1.5 T), defined image acquisition protocol (axial PD/T2-w, axial or coronal FLAIR; in 23 patients additional axial T2-w or coronal T2-w thin slices, coronal T1-w post-contrast, and 3D TOF angiography) |
Results of MVD in TN in MS seemed to be less satisfactory than in the idiopathic group, suggesting a central mechanism in MS TN |
| da Silva (2005) | Brazil | Retrospective, cross-sectional | 275 MS patients | Review of incidence of trigeminal involvement on MRI, as well as clinical correlation in patients with MS | Search for trigeminal symptoms in medical records and medical attendances | MRI (1 T), defined image acquisition protocol (axial FLAIR, PD/T2-w, and T1-w before and after contrast) | High clinically silent incidence of trigeminal involvement in MS, including simultaneous central and peripheral demyelination |
| Gass (1997) | UK and Germany | Cross-sectional? | 6 MS patients with TN | Lesion localisation in MS patients with TN | Neurological examination | MRI (1.5 T), defined image acquisition protocol (including axial PD/T2-w) | Brainstem lesions involving the trigeminal fibres were demonstrated, without neurovascular contacts |
| Yetimalar (2008) | Turkey | Retrospective, cross-sectional | 21 MS patients (11 with pain syndromes including headache, brachalgia and throat pain) | Description of patients with unusual symptoms that were primary manifestations of MS | International Headache Society Classification (2004), neurological examination | MRI (1.5 T), use of contrast | Possible correlations between clinical disturbances and neuroradiological abnormalities of some unusual primary manifestations of MS |
| Eldridge (2003) | UK | Retrospective | 9 MS patients with TN | To assess whether MVD was a safe and efficacious treatment for patients with TN and MS | Review of medical records | MRI (1.5 T), protocol defined (conventional MRI and angiography, with and without contrast) | MVD provided good initial pain relief, but recurrence rate was higher than in idiopathic TN |
MS — multiple sclerosis; TN — trigeminal neuralgia; MRI — magnetic resonance imaging; MVD — microvascular decompression; T — tesla; T1-w — T1-weighted; T2-w — T2-weighted; PD — proton density; FLAIR — fluid attenuation inversion recovery; STIR — short T1 inversion recovery; TOF — time-of-flight.
Table 2.
The quality assessment criteria used in the systematic review of the literature.
| Original studies | Quality assessment criteria |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Research objective | Recruitment procedure | Inclusion/exclusion criteria | Population demographics | Participation rates | Pain measures | Imaging protocol | Strength of effect | Multivariate analysis | Limitations discussed | Participation over 70% | |
| Balasa (2010) | Yes | Yes | No | No | No | Yes | No | No | No | No | No |
| Broggi (2004) | Yes | Yes | No | Yes | No | Yes | Yes | No | No | No | No |
| Cruccu (2009) | No | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | No |
| Deppe (2013) | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes | No |
| Eldridge (2003) | Yes | Yes | No | Yes | No | No | Yes | No | No | No | No |
| Gass (1997) | Yes | Yes | No | Yes | No | No | Yes | No | No | No | No |
| Gee (2005) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No |
| Kister (2010) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ramirez-Lassepas (1992) | No | Yes | No | Yes | No | No | No | No | No | Yes | No |
| Da Silva (2005) | Yes | Yes | No | Yes | No | No | Yes | No | No | Yes | No |
| Svendsen (2011) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No |
| Tortorella (2006) | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | No |
| Yetimalar (2008) | Yes | Yes | No | Yes | No | No | Yes | No | No | No | No |
3.1. Reporting of image acquisition methods
All identified studies used conventional structural MRI but one, which investigated pain in MS using diffusion tensor imaging (DTI) (Deppe et al., 2013). No studies used functional MRI, SPECT or PET. There were significant deficiencies in the description of imaging methodology in many studies (Table 3 summarises frequency of description of each aspect of imaging acquisition). We found that field strength was specified in 15 studies (39% of all studies). Of these 15 studies, one tesla scanners were used in two studies (Balasa and Bajko, 2010; da Silva et al., 2005), 1.5 T scanners were used in nine studies (Eldridge et al., 2003; Gass et al., 1997; Gee et al., 2005; Meaney et al., 1995; Nakashima et al., 2001; Pichiecchio et al., 2007; Svendsen et al., 2011; Tortorella et al., 2006; Yetimalar et al., 2008), and 3 T scanners were used in two (of the most recent) studies (Andrade et al., 2012; Deppe et al., 2013). Scanners of varying strengths were employed in two studies: 0.6, 1.5 and 3 T (Kister et al., 2010), and 0.5 and 1.5 T (Broggi et al., 2004). Of all the included studies, MRI protocols were stated only in 14 (37%) (Andrade et al., 2012; Athanasiou et al., 2005; Broggi et al., 2004; da Silva et al., 2005; Deppe et al., 2013; Donat, 2012; Eldridge et al., 2003; Gass et al., 1997; González-Quintanilla et al., 2012; Haas et al., 1993; Kister et al., 2010; Meaney et al., 1995; Svendsen et al., 2011; Tortorella et al., 2006). Of the 14 studies that did describe the MRI protocol used, only nine of these described all the sequences (Broggi et al., 2004; da Silva et al., 2005; Deppe et al., 2013; Gass et al., 1997; Haas et al., 1993; Kister et al., 2010; Meaney et al., 1995; Svendsen et al., 2011; Tortorella et al., 2006), and only four described all the sequence parameters of all the sequences (da Silva et al., 2005; Gass et al., 1997; Svendsen et al., 2011; Tortorella et al., 2006). Imaging methodology was relatively better described in the 13 investigational studies, although four did not describe MRI protocols, and reading methods were described in only five studies.
Table 3.
Descriptions of magnetic resonance imaging methodology.
| MRI image acquisition | Papers |
|---|---|
| Scanner | Deppe (2013), Eldridge (2003), Gass (1997), Meaney (1995), Svendsen (2011) |
| Field strength | Andrade (2012), Broggi (2004), da Silva (2005), Deppe (2013), Eldridge (2003), Gass (1997), Kister (2010), Meaney (1995), Svendsen (2011), Tortorella (2006), Yetimalar (2008) |
| Sequences | |
| All the sequences used |
Broggi (2004), da Silva (2005), Deppe (2013), Gass (1997), Haas (1993), Kister (2010), Meaney (1995), Svendsen et al., 2011, Tortorella (2006) |
| Some of the sequences used | Andrade (2012), Athanasiou (2005), Donat (2012), Eldridge (2003), González-Quintanilla (2012) |
| Sequence parameters | |
| All the sequences used and all its parameters | da Silva (2005), Gass (1997), Svendsen (2011), Tortorella (2006) |
| Some of the sequences used and/or some of the parameters | Athanasiou (2005), Broggi (2004), Deppe (2013), Haas (1993), Meaney (1995) |
3.2. Diagnosis of multiple sclerosis
Criteria used to confirm the diagnosis of MS were explicitly stated in only 16 of the 38 studies (2010 revisions to the McDonald criteria — Polman et al., 2011 (Deppe et al., 2013; González-Quintanilla et al., 2012); revised McDonald — Polman et al., 2005 (Andrade et al., 2012; Cruccu et al., 2009; Fragoso and Brooks, 2007; Gentile et al., 2007; Kister et al., 2010); McDonald — McDonald et al., 2001 (Balasa and Bajko, 2010; Carrieri et al., 2009; Hellwig et al., 2006; Yetimalar et al., 2008); Poser — Poser et al., 1983 (Broggi et al., 2004; Hellwig et al., 2006; Leandri et al., 1999; Meaney et al., 1995); Rose — Rose et al., 1976 (Ramirez-Lassepas et al., 1992)). The type of MS in subjects was not fully described in 14 studies (Athanasiou et al., 2005; Balasa and Bajko 2010; Burkey and Abla-Yao, 2010; Cruccu et al., 2009; Donat, 2012; Eldridge et al., 2003; Fragoso and Brooks, 2007; González-Quintanilla et al., 2012; Kister et al., 2010; Marchettini et al., 2006; Meaney et al., 1995; Minagar and Sheremata, 2000; Ramirez-Lassepas et al., 1992; Yetimalar et al., 2008). It was relapsing–remitting in 16 ((Alstadhaug et al., 2008; Andrade et al., 2012; Bentley et al., 2002; Carrieri et al., 2009; Deppe et al., 2013; de Santi et al., 2009; Gentile et al., 2007; Haas et al., 1993; Hellwig et al., 2006; Leandri et al., 1999; Liu et al., 2008; Nakashima et al., 2001; Pichiecchio et al., 2007; Tanei et al., 2010; Tosi et al., 1998) (Minagar and Sheremata, 2000) – one case). Six studies included patients with various MS subtypes (Broggi et al., 2004; da Silva et al., 2005; Gass et al., 1997; Gee et al., 2005; Svendsen et al., 2011; Tortorella et al., 2006).
3.3. Pain syndromes and lesion localisation
All studies examined either neuropathic pain or headache (studied pain syndromes are detailed in Table 4). We found no studies investigating nociceptive/somatic pain or psychogenic pain. Most studies (n = 28, 74% of total) focused on headache or facial pain syndromes, and the remainder on bodily pain (eight studies, 21% of total), except for two studies (6%), which included both patients with headache/facial pain and those with body pain (Svendsen et al., 2011; Yetimalar et al., 2008).
Table 4.
Types of pain syndromes studied.
| Type of pain syndrome | Study |
|---|---|
| Headache disorders | |
| Migraine | Fragoso (2007), Kister (2010), Tortorella (2006) |
| Cluster headache and other trigeminal autonomic cephalalgias | Cluster headache — Gentile (2007) Cluster-like headache — Donat (2012), Leandri (1999) Cluster-tic syndrome — González-Quintanilla (2012) SUNCT — Davey (2004), Vilisaar (2006) Probable trigeminal autonomic cephalalgia with allodynia — Liu (2008) |
| Cranial neuralgias and central causes of facial pain |
Glossopharyngeal neuralgia — Carrieri (2009), Minagar (2000) Occipital neuralgia — de Santi (2009) (2 cases) Painful third nerve palsy — Bentley (2002) Transverse colli neuralgia — de Santi (2009) (1 case) Trigeminal neuralgia — Athanasiou (2005), Balasa (2010), Broggi (2004), Cordella (2009), Cruccu (2009), da Silva (2005), Eldridge (2003), Gass (1997), Meaney (1995), Nakashima (2001), Pichiecchio (2007) |
| Other headache, cranial neuralgia, central or primary facial pain | Atypical trigeminal neuralgia/facial pain — Tanei (2010) Headache — Alstadhaug et al., 2008, Haas (1993) |
| Body pain | |
| Pseudo-radicular pain | Cervical — Tosi (1998) Sciatica — Marchettini (2006) Various levels — Ramirez-Lassepas (1992) |
| Dysesthetic pain |
Burkey (2010), Deppe (2013), Hellwig (2006) |
| Pain and painful itching |
Hellwig (2006) |
| Painful tonic spasms |
Andrade (2012) |
| Visceral pain |
Marchettini (2006) |
| Various | |
| Svendsen (2011), Yetimalar (2008) |
SUNCT — short-lasting unilateral neuralgiform headache with conjunctival injection and tearing.
All studies detailed the location of lesions thought to be responsible for pain syndromes. Table 5 describes lesion locations in the 25 included case reports and series. Of these, 21 describe demyelinating lesions in areas thought likely to be responsible for a pain syndrome (Table 5) whereas four did not find demyelinating lesions thought likely to be responsible (Athanasiou et al., 2005; Carrieri et al., 2009; Davey and Al-Din, 2004; Minagar and Sheremata, 2000). Most authors assigned lesions as the likely cause of pain syndromes by anatomical location. Relatively few investigators further studied the age or evolution of the lesion in relation to the pain syndrome by use of either serial imaging or intravenous contrast (Table 5). Lesions were identified in the CNS (i.e. central neuropathic pain) in 21 studies; of these, lesions were located in the spinal cord in six studies ((Alstadhaug et al., 2008; Burkey and Abla-Yao, 2010; Tosi et al., 1998) (de Santi et al., 2009) — three cases (Hellwig et al., 2006) — four cases: only two documented with MRI (Marchettini et al., 2006) — five cases), in the brainstem in 13 studies ((Bentley et al., 2002; Donat, 2012; Gentile et al., 2007; González-Quintanilla et al., 2012; Haas et al., 1993; Leandri et al., 1999; Liu et al., 2008; Tanei et al., 2010) (Meaney et al., 1995; Nakashima et al., 2001; Vilisaar and Constantinescu, 2006) — one case (Fragoso and Brooks, 2007) — two cases (Cordella et al., 2009) — five cases), in the thalamus in one study (Deppe et al., 2013) and in multiple locations throughout the pyramidal tract in another study (Andrade et al., 2012).
Table 5.
Location of candidate culprit multiple sclerosis lesions in the origin of pain as detected by magnetic resonance imaging in the case reports/series retrieved.
| Study | Pain syndrome or location | Localisation of the lesions possibly explaining the pain syndrome | Basis of association (A/S/C) |
|---|---|---|---|
| Spinal cord | |||
| Tosi (1998) | Radicular | Cervical (C5–C6) dorsal root entry zone and posterior horn |
A, S |
| Alstadhaug et al., 2008 | Headache (type not defined) | Posterior part of the upper cervical spinal cord |
A, S |
| Burkey (2010) | Upper limb pain | Posterior columns from C2 to C4 | A |
| Hellwig (2006) | Painful dysaesthesia at thoracic level and/or below | Posterior upper thoracic spinal cord; cord lesions at the level of C1, C4/5, Th3 (two cases) |
A, C |
| de Santi (2009) | Occipital neuralgia | Right antero-lateral spinal cord at C2; C1, C2, C3 and D1–D2; C2–C3 lesion (three cases) |
A, S, C |
| Marchettini (2006) | Back, leg, flank or abdominal pain | Spinal cord location of the lesions assumed; MRI was used to exclude other causes of pseudo-radicular or visceral pain (five cases) |
n/a |
| Brain | |||
| Andrade (2012) | Painful stereotyped involuntary posturing movements of the left upper limb | Pyramidal tract lesions (cerebral peduncle, internal capsule and corona Radiata) | A, S, C |
| Bentley (2002) | Painful third nerve palsy (including pupil) | Midbrain adjacent to right third nerve fascicle |
A, S |
| Donat, 2012 | Cluster-like headache | Right dorsal pons | A |
| González-Quintanilla (2012) | Cluster-tic | Left and right trigeminal root inlet and main sensory nucleus in the brainstem | A, S |
| Tanei (2010 | Facial pain (non-TN) | Right dorsal pons and medulla oblongata |
A |
| Haas (1993) | Headache (type not defined) |
Periaqueductal grey |
A, S, C |
| Liu (2008) | Probable TAC with allodynia and other symptoms |
Right lateral tegmentum of the lower pons |
A, S |
| Leandri (1999) | TAC | Root entry zone of the trigeminal nerve on the right |
A |
| Gentile (2007) | Cluster headache/TAC with sensory symptoms |
Left brachium pontis |
A, S |
| Meaney (1995) | TN (unilateral or bilateral) | Root entry zone of both trigeminal nerves (one case out of seven cases described) |
A |
| Nakashima (2001) | TN | Left trigeminal root entry zone (one case out of five cases described) |
A |
| Fragoso (2007) | Migraine without aura | Brainstem (two cases) | A |
| Cordella (2009) | TN | Trigeminal root entry zone (five cases) |
A |
| Pichiecchio (2007) | TN | Trigeminal root entry zone bilaterally and enhancement of trigeminal nerves |
A/C |
| Vilisaar (2006) | SUNCT | Anterior pons, right cerebral peduncle and medulla (one case) | A |
A — anatomically plausible lesion; S — serial imaging demonstrating emergence or disappearance of plaque in line with clinical pain syndrome; C — contrast enhancing plaque; n/a = not applicable; TN — trigeminal neuralgia; TAC — trigeminal autonomic cephalalgia; SUNCT — short-lasting unilateral neuralgiform headache with conjunctival injection and tearing; MRI — magnetic resonance imaging.
3.3.1. Headache and facial pain
The classification of headache disorders used was not specified in four of the 10 investigational studies studying headaches (Broggi et al., 2004; da Silva et al., 2005; Eldridge et al., 2003; Gass et al., 1997), and in the remaining six studies the criteria used were those of the International Headache Society 1988 (Headache Classification Committee of the International Headache Society, 1988) (Gee et al., 2005) or of the International Headache Society 2004 (Headache Classification Subcommittee of the International Headache Society, 2004) (Balasa and Bajko, 2010; Cruccu et al., 2009; Kister et al., 2010; Tortorella et al., 2006; Yetimalar et al., 2008).
All identified brainstem lesions corresponded to headache disorders, except for a lesion in the cerebral peduncle (among other lesions identified in the pyramidal tract) in a case of painful tonic spasms (Andrade et al., 2012). Spinal cord lesions corresponded to headache disorders in two studies (Alstadhaug et al., 2008; de Santi et al., 2009) (Table 5). Lesions including both the peripheral and the CNS were described in one study (brainstem and trigeminal nerve — Pichiecchio et al., 2007). Three studies found incidental structural lesions, which were unrelated to MS but felt to explain headache or facial pain (Athanasiou et al., 2005; Eldridge et al., 2003; Meaney et al., 1995).
3.3.2. Neuropathic body pain
Five different body pain syndromes were identified, all neuropathic: pseudo-radicular pain (Marchettini et al., 2006; Ramirez-Lassepas et al., 1992; Tosi et al., 1998), dysesthetic pain (Burkey et al., 2010; Deppe et al., 2013; Hellwig et al., 2006), painful itching (Hellwig et al., 2006), painful tonic spasms (Andrade et al., 2012) and visceral pain (Marchettini et al., 2006). All lesions thought to explain the body pain syndromes were located in the spinal cord (Table 5), except for the painful tonic spasms where lesions were identified in the pyramidal tract in the brain (Andrade et al., 2012) (Table 5).
3.4. Treatment of pain
In seven of the studies (21% of total), although neuroimaging was used to study pain syndromes in MS, the main focus of the study was an invasive pain treatment. These studies addressed microvascular decompression for trigeminal neuralgia (TN) (Athanasiou et al., 2005; Broggi et al., 2004; Eldridge et al., 2003), CNS stimulation (Burkey and Abla-Yao, 2010; Cordella et al., 2009; Tanei et al., 2010), and intrathecal administration of a steroid (Hellwig et al., 2006).
4. Discussion
Our findings suggest that the number of studies examining neuroradiological correlates of MS pain is low and that methodology and quality of these studies are variable. The majority of included articles are case reports or series, and therefore are of limited value for clinical practice or for research (Vandenbroucke, 2001). Specifically, we found only 13 hypothesis-driven investigational studies. In turn, of these identified investigational studies, only one met all of our quality criteria (Kister et al., 2010), and five (Deppe et al., 2013; Gee et al., 2005; Kister et al., 2010; Svendsen et al., 2011; Tortorella et al., 2006) over half. We identified several aspects of methodology that could be improved in our included studies.
Firstly, we identified that the focus of identified studies on specific pain syndromes did not closely reflect clinical estimates of the prevalence of these pain syndromes in MS. All identified studies investigated neuropathic pain syndromes, despite frequent observations in cross-sectional studies that both nociceptive and neuropathic pains are common in MS (Polman et al., 2011). There was also an emphasis on investigation of headache disorders and facial pain (74% of all studies), in particular TN. This emphasis is at odds with estimates of prevalence of pain syndromes in MS — for example TN is reported in 1–5% of MS patients, as compared to an overall pain prevalence of approximately 50% (Polman et al., 2011). Other cranial pain syndromes examined in included studies (such as occipital or glossopharyngeal neuralgia (Carrieri et al., 2009; de Santi et al., 2009; Minagar and Sheremata, 2000; Vilisaar and Constantinescu, 2006)) are even less common. These observations could suggest that studies identifying neuroradiological correlates of neuropathic pain syndromes in general, and headache or facial pain syndromes in particular, are disproportionately represented by the current literature (Bax and Moons, 2011).
The included headache studies largely aimed to examine neuroradiological correlates of specific headache subtypes. Small studies of migraine and unclassified headache including one to two subjects (Fragoso and Brooks, 2007; Haas et al., 1993) identified abnormalities in relation to the brainstem, in keeping with the putative role of the brainstem in pain transmission pathways. Larger investigational studies including those by Gee and colleagues (n = 277) (Gee et al., 2005) and Tortorella and colleagues (n = 79) (Tortorella et al., 2006) (quality assessments ten and eight, respectively, from a maximum of 12) also suggested that the presence of brainstem demyelination might be associated with the occurrence of migraine. In contrast, Kister and colleagues (n = 204) (quality assessment 12) compared MS groups with and without migraine, and found no differences in the number or distribution of lesions in the brain (including the brainstem) between the two groups (Kister et al., 2010).
Studies characterising TN and trigeminal autonomic cephalalgias (TACs), in contrast, focused on abnormalities related to the trigeminal nucleus and nerve. Interestingly, there appears to be an overlap in radiological findings between TN and TACs, though this observation may not be generalisable to patients without MS. Regarding TN, two of the identified studies (Broggi et al., 2004; Eldridge et al., 2003) focused on treatment. Separate studies supported the roles of both central demyelination (Balasa and Bajko, 2010; Broggi et al., 2004; Cruccu et al., 2009; Gass et al., 1997) and peripheral mechanisms (da Silva et al., 2005; Eldridge et al., 2003). Despite the preponderance of headache and facial pain studies described in our review, differing methodology impairs synthesis of results. Both peripheral and central mechanisms in TN related to MS are described, and the relative importance of each is not easily quantified. Studies of microvascular decompression further suggest that in some cases outcome for patients with demonstrated neurovascular contact is relatively poor than that for patients without MS (Broggi et al., 2004; Eldridge et al., 2003). This has been interpreted as supporting a dual mechanism of TN pain in at least some MS patients.
Neuropathic extremity pain of central origin (typically a chronic “burning” pain affecting the lower limbs) is thought to be one of the most common pain syndromes in MS (O'Connor et al., 2008). Our included studies examined differing types of limb pain, and the hypothesis that spinal lesions may be causative in limb or radicular pain has been proposed in several studies. In particular, in case reports or series (Burkey and Abla-Yao, 2010; Hellwig et al., 2006; Tosi et al., 1998), dorsal cord lesions in the thoracic and/or the cervical cord have been linked to limb pain, perhaps by directly disturbing sensory afferent pathways, or by disrupting descending inhibitory pathways (Svendsen et al., 2011). This hypothesis is further supported by one investigational study that was assessed as relatively poor quality by our criteria (n = 11, quality assessment three, from a maximum of 12) (Ramirez-Lassepas et al., 1992). Svendsen et al., however, using a better study design including spinal and brain MRI (n = 25, quality assessment eight) found no association between the site of demyelination and the presence of chronic central neuropathic pain (Svendsen et al., 2011).
Taking into account all identified studies, culprit demyelinating lesions were most commonly reported in the brainstem, and less commonly in the spinal cord. This may as well be linked to our observations above that the majority of studies investigated headache or facial pain. Notably, among the included investigational studies, Svendsen et al. (2011) investigated corticothalamic involvement and found no statistically significant difference in thalamic or thalamo-cortical projection lesion load in MS patients with or without pain. Deppe and colleagues, using DTI, studied a patient with central pain and abnormal somatosensory and thermal sensations on the right side of the body, comparing with imaging data from 100 healthy volunteers (the subjects and patient were part of a pilot study for a clinical trial) (Deppe et al., 2013). The imaging technique and post-processing methods were well described. However, the authors suggest that the unilateral temporary increase of the fractional anisotropy found in the contralateral thalamus may have played a causative role, though the pain syndrome was poorly characterised. The relative lack of studies of corticothalamic involvement in MS-related pain may relate to a historical emphasis on white matter pathology in MS, despite ample recent evidence of grey matter involvement (Compston and Coles, 2008). Methods used for identification of culprit MS lesions also frequently relied on a priori anatomical hypotheses. This could in theory diminish the likelihood of identifying novel associations with a particular pain syndrome. In only a minority of cases was a temporal association between the lesion and the pain syndrome in question further studied by serial imaging and/or the use of intravenous contrast (Table 5). Furthermore, any possible role of MS-related damage in normal-appearing tissue was not considered, with the one exception of Deppe and colleagues' study (Deppe et al., 2013); no investigators explicitly studied transition from acute to chronic pain states.
In all but one of the studies, MRI was used (most frequently to analyse lesion location, or to investigate structural causes of pain). The description of image acquisition and reading protocols, and investigator blinding in the original studies was, however, in general insufficient. It was also not always clear who read and interpreted the images (Table 1), and only four investigational studies (Gee et al., 2005; Kister et al., 2010; Svendsen et al., 2011; Tortorella et al., 2006) described image interpretation blinded to subject pain status (Table 2). The complexity of imaging techniques such as MRI requires more rigorous methodology and reporting in order to ensure clarity and reproducibility. Poldrack and colleagues published comprehensive guidelines for the reporting of methods and results in fMRI that are relevant as well for structural MRI (Poldrack et al., 2008). Blinded assessment could also help to minimise potential for biased interpretation of images.
We identified no functional or molecular imaging studies of the CNS, despite the potential of these methods in studying pain mechanisms in health and disease (Tracey, 2007), and only one study (Deppe et al., 2013) investigated pain using non-conventional structural MRI (DTI). MRI is important in the diagnosis and investigation of MS due to its sensitivity, non-invasiveness and reproducibility. However, clinical–radiological correlations have not always been the expected, including in the pain research field. This discrepancy may reflect the difficulties of imaging the complete spectrum of MS pathological abnormalities that range from focal and diffuse white matter lesions, normal-appearing white matter damage, grey matter damage and vascular changes, in the brain and in the spinal cord. Several non-conventional MRI techniques are important in resolving non-focal, grey matter and vascular MS pathology. DTI, magnetisation transfer imaging (MTI) and proton spectroscopy can quantify and characterise normal-appearing tissue changes (Filippi et al., 2012). Double inversion recovery has improved the sensitivity of MRI to detect cortical lesions (Geurts et al., 2005), and the use of ultra-high-field scanners is promising (Filippi et al., 2012; Ropele et al., 2011). Brain tissue perfusion can be assessed as well with MRI (Ge et al., 2005; Inglese et al., 2007). Inter-patient variability of clinical manifestations might also be explained with functional CNS reorganisation and plasticity, which can be imaged with fMRI (Filippi and Rocca, 2011).
Our review had several limitations. We have included studies, as discussed above, which do not fully describe diagnostic criteria used in application of the diagnosis of MS. Therefore although all studies described the inclusion of only subjects with MS, the possibility of alternative pathology contributing to pain therefore needs to be remembered. We have, in addition, limited our study to articles published in English, and although only three studies were excluded using this criterion, it is possible that relevant data was not assessed.
5. Conclusion
We have found that neuroradiological studies of pain in MS are relatively low in number, and of variable design and quality. Some common pain syndromes were less frequently studied, and significant methodological issues relating to study design, execution and reporting were identified. We found that investigators using different study methodologies have reached differing conclusions regarding the neuroradiological correlates of specific pain syndromes in MS. Methodologically higher-quality studies were however less likely to report positive associations of lesion location to the presence of headache, or of chronic central neuropathic pain (Kister et al., 2010; Svendsen et al., 2011).
Therefore, despite the prevalence and impact of pain in MS, the insight into pain mechanisms currently afforded by neuroimaging studies remains limited. There is considerable opportunity to advance our mechanistic understanding of MS-associated pain, and thus its therapy, through future research. High quality hypothesis-driven studies, including those investigating the more common pain syndromes, comparison of lesion localisation in MS patients with and without pain, and perhaps using functional and advanced structural MRI techniques, could be well placed to advance this important field.
Conflicts of interest
None to declare.
Funding
This study is supported by the Portuguese Foundation for Science and Technology [SFRH/BD/27411/2006 to D.S.].
Acknowledgements
We gratefully acknowledge Dr. Cathie Sudlow (Division of Clinical Neurosciences, University of Edinburgh, Western General Hospital, Edinburgh, UK) for helpful comments on an earlier version of the manuscript.
References
- Alstadhaug K., Breivik K., Rusic Z. Recurrent headache due to MS plaque. Headache. 2008;48:453–454. doi: 10.1111/j.1526-4610.2007.01003.x. 18081822 [DOI] [PubMed] [Google Scholar]
- Andrade C., Massano J., Guimarães J., Garrett M.C. Stretching the limbs? Tonic spasms in multiple sclerosis. BMJ Case Reports. 2012;30 doi: 10.1136/bcr-2012-007513. 23208828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athanasiou T.C., Patel N.K., Renowden S.A., Coakham H.B. Some patients with multiple sclerosis have neurovascular compression causing their trigeminal neuralgia and can be treated effectively with MVD: report of five cases. British Journal of Neurosurgery. 2005;19:463–468. doi: 10.1080/02688690500495067. 16574557 [DOI] [PubMed] [Google Scholar]
- Bakshi R., Thompson A.J., Rocca M.A., Pelletier D., Dousset V., Barkhof F., Inglese M., Guttmann C.R., Horsfield M.A., Filippi M. MRI in multiple sclerosis: current status and future prospects. Lancet Neurology. 2008;7:615–625. doi: 10.1016/S1474-4422(08)70137-6. 18565455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasa R., Bajko Z. Trigeminal neuralgia in multiple sclerosis patients: a clinical comparison of trigeminal neuralgia in patients with and without underlying multiple sclerosis. Romanian Journal of Neurology. 2010;9:68–73. [Google Scholar]
- Bax L., Moons K.G. Beyond publication bias. Journal of Clinical Epidemiology. 2011;64:459–462. doi: 10.1016/j.jclinepi.2010.09.003. 21194886 [DOI] [PubMed] [Google Scholar]
- Bentley P.I., Kimber T., Schapira A.H. Painful third nerve palsy in MS. Neurology. 2002;58:1532. doi: 10.1212/wnl.58.10.1532. 12034792 [DOI] [PubMed] [Google Scholar]
- Broggi G., Ferroli P., Franzini A., Nazzi V., Farina L., La Mantia L., Milanese C. Operative findings and outcomes of microvascular decompression for trigeminal neuralgia in 35 patients affected by multiple sclerosis. Neurosurgery. 2004;55:830–838. 15458591 [PubMed] [Google Scholar]
- Burkey A.R., Abla-Yao S. Successful treatment of central pain in a multiple sclerosis patient with epidural stimulation of the dorsal root entry zone. Pain Medicine (Malden, Mass.) 2010;11:127–132. doi: 10.1111/j.1526-4637.2009.00764.x. 20447296 [DOI] [PubMed] [Google Scholar]
- Campbell P., Wynne-Jones G., Dunn K.M. The influence of informal social support on risk and prognosis in spinal pain: a systematic review. European Journal of Pain (London, England) 2011;15:444.e1–444.e14. doi: 10.1016/j.ejpain.2010.09.011. 20970363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri P.B., Montella S., Petracca M. Glossopharyngeal neuralgia as onset of multiple sclerosis. Clinical Journal of Pain. 2009;25:737–739. doi: 10.1097/AJP.0b013e3181af133b. 19920727 [DOI] [PubMed] [Google Scholar]
- Charcot J.M. Lecons sur les maladies du systeme nerveux faites a la Salpetriere. Delahaye; Paris: 1872. [Google Scholar]
- Compston A., Coles A. Multiple sclerosis. Lancet. 2008;372:1502–1515. doi: 10.1016/S0140-6736(08)61620-7. 18970977 [DOI] [PubMed] [Google Scholar]
- Cordella R., Franzini A., La Mantia L., Marras C., Erbetta A., Broggi G. Hypothalamic stimulation for trigeminal neuralgia in multiple sclerosis patients: efficacy on the paroxysmal ophthalmic pain. Multiple Sclerosis (Houndmills, Basingstoke, England) 2009;15:1322–1328. doi: 10.1177/1352458509107018. 19812115 [DOI] [PubMed] [Google Scholar]
- Cruccu G., Biasiotta A., Di Rezze S., Fiorelli M., Galeotti F., Innocenti P., Mameli S., Millefiorini E., Truini A. Trigeminal neuralgia and pain related to multiple sclerosis. Pain. 2009;143:186–191. doi: 10.1016/j.pain.2008.12.026. 19171430 [DOI] [PubMed] [Google Scholar]
- Da Silva C.J., da Rocha A.J., Mendes M.F., Maia A.C., Jr., Braga F.T., Tilbery C.P. Trigeminal involvement in multiple sclerosis: magnetic resonance imaging findings with clinical correlation in a series of patients. Multiple Sclerosis (Houndmills, Basingstoke, England) 2005;11:282–285. doi: 10.1191/1352458505ms1186oa. 15957508 [DOI] [PubMed] [Google Scholar]
- Davey R., Al-Din A. Secondary trigeminal autonomic cephalgia associated with multiple sclerosis. Cephalalgia: an International Journal of Headache. 2004;24:605–607. doi: 10.1111/j.1468-2982.2004.00725.x. 15196304 [DOI] [PubMed] [Google Scholar]
- Deppe M., Müller D., Kugel H., Ruck T., Wiendl H., Meuth S.G. DTI detects water diffusion abnormalities in the thalamus that correlate with an extremity pain episode in a patient with multiple sclerosis. NeuroImage: Clinical. 2013;2:258–262. doi: 10.1016/j.nicl.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Santi L., Monti L., Menci E., Bellini M., Annunziata P. Clinical–radiologic heterogeneity of occipital neuralgiform pain as multiple sclerosis relapse. Headache. 2009;49:304–307. doi: 10.1111/j.1526-4610.2008.01209.x. 18647183 [DOI] [PubMed] [Google Scholar]
- Donat J. A patient with cluster headache — due to a brainstem lesion. Headache. 2012;52:1035–1036. doi: 10.1111/j.1526-4610.2011.02044.x. 22077341 [DOI] [PubMed] [Google Scholar]
- Eldridge P.R., Sinha A.K., Javadpour M., Littlechild P., Varma T.R. Microvascular decompression for trigeminal neuralgia in patients with multiple sclerosis. Stereotactic and Functional Neurosurgery. 2003;81:57–64. doi: 10.1159/000075105. 14742965 [DOI] [PubMed] [Google Scholar]
- Filippi M., Rocca M.A. MR imaging of multiple sclerosis. Radiology. 2011;259:659–681. doi: 10.1148/radiol.11101362. 21602503 [DOI] [PubMed] [Google Scholar]
- Filippi M., Rocca M.A., Barkhof F., Brück W., Chen J.T., Comi G., DeLuca G., De Stefano N., Erickson B.J., Evangelou N., Fazekas F., Geurts J.J., Lucchinetti C., Miller D.H., Pelletier D., Popescu B.F., Lassmann H., Attendees of the Correlation Between Pathological MRI Findings in MS Workshop Association between pathological and MRI findings in multiple sclerosis. Lancet Neurology. 2012;11(() doi: 10.1016/S1474-4422(12)70003-0. ) 349–360 [Pubmed: 22441196] [DOI] [PubMed] [Google Scholar]
- Fragoso Y.D., Brooks J.B. Two cases of lesions in brainstem in multiple sclerosis and refractory migraine. Headache. 2007;47:852–854. doi: 10.1111/j.1526-4610.2007.00823.x. 17578534 [DOI] [PubMed] [Google Scholar]
- Gass A., Kitchen N., MacManus D.G., Moseley I.F., Hennerici M.G., Miller D.H. Trigeminal neuralgia in patients with multiple sclerosis: lesion localization with magnetic resonance imaging. Neurology. 1997;49:1142–1144. doi: 10.1212/wnl.49.4.1142. 9339705 [DOI] [PubMed] [Google Scholar]
- Ge Y., Law M., Johnson G., Herbert J., Babb J.S., Mannon L.J., Grossman R.I. Dynamic susceptibility contrast perfusion MR imaging of multiple sclerosis lesions: characterizing hemodynamic impairment and inflammatory activity. AJNR. American Journal of Neuroradiology. 2005;26:1539–1547. 15956527 [PMC free article] [PubMed] [Google Scholar]
- Gee J.R., Chang J., Dublin A.B., Vijayan N. The association of brainstem lesions with migraine-like headache: an imaging study of multiple sclerosis. Headache. 2005;45:670–677. doi: 10.1111/j.1526-4610.2005.05136.x. 15953299 [DOI] [PubMed] [Google Scholar]
- Gentile S., Ferrero M., Vaula G., Rainero I., Pinessi L. Cluster headache attacks and multiple sclerosis. Journal of Headache and Pain. 2007;8:245–247. doi: 10.1007/s10194-007-0405-8. 17901919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurts J.J., Pouwels P.J., Uitdehaag B.M., Polman C.H., Barkhof F., Castelijns J.A. Intracortical lesions in multiple sclerosis: improved detection with 3D double inversion-recovery MR imaging. Radiology. 2005;236:254–260. doi: 10.1148/radiol.2361040450. 15987979 [DOI] [PubMed] [Google Scholar]
- González-Quintanilla V., Oterino A., Toriello M., de Pablos C., Wu Y., de Marco E., Pascual J. Cluster-tic syndrome as the initial manifestation of multiple sclerosis. Journal of Headache and Pain. 2012;13:425–429. doi: 10.1007/s10194-012-0449-2. 22543446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas D.C., Kent P.F., Friedman D.I. Headache caused by a single lesion of multiple sclerosis in the periaqueductal gray area. Headache. 1993;33:452–455. doi: 10.1111/j.1526-4610.1993.hed3308452.x. 8262789 [DOI] [PubMed] [Google Scholar]
- Headache Classification Committee of the International Headache Society Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988;8:1–96. [PubMed] [Google Scholar]
- Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia: an International Journal of Headache. 2004;24:9–160. doi: 10.1111/j.1468-2982.2003.00824.x. 14979299 [DOI] [PubMed] [Google Scholar]
- Hellwig K., Lukas C., Brune N., Schimrigk S., Przuntek H., Müller T. Repeat intrathecal triamcinolone acetonide application reduces acute occurring painful dysesthesia in patients with relapsing remitting multiple sclerosis. TheScientificWorldJournal. 2006;6:460–465. doi: 10.1100/tsw.2006.86. 16604259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglese M., Park S.J., Johnson G., Babb J.S., Miles L., Jaggi H., Herbert J., Grossman R.I. Deep gray matter perfusion in multiple sclerosis: dynamic susceptibility contrast perfusion magnetic resonance imaging at 3 T. Archives of Neurology. 2007;64:196–202. doi: 10.1001/archneur.64.2.196. 17296835 [DOI] [PubMed] [Google Scholar]
- Kalia L.V., O'Connor P.W. Severity of chronic pain and its relationship to quality of life in multiple sclerosis. Multiple Sclerosis (Houndmills, Basingstoke, England) 2005;11:322–327. doi: 10.1191/1352458505ms1168oa. 15957515 [DOI] [PubMed] [Google Scholar]
- Kister I., Caminero A.B., Monteith T.S., Soliman A., Bacon T.E., Bacon J.H., Kalina J.T., Inglese M., Herbert J., Lipton R.B. Migraine is comorbid with multiple sclerosis and associated with a more symptomatic MS course. Journal of Headache and Pain. 2010;11:417–425. doi: 10.1007/s10194-010-0237-9. 20625916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leandri M., Cruccu G., Gottlieb A. Cluster headache-like pain in multiple sclerosis. Cephalalgia: an International Journal of Headache. 1999;19:732–734. doi: 10.1046/j.1468-2982.1999.019008732.x. 10570729 [DOI] [PubMed] [Google Scholar]
- Liu F.C., Fuh J.L., Wang S.J. Symptomatic trigeminal autonomic cephalalgia associated with allodynia in a patient with multiple sclerosis. Journal of the Chinese Medical Association: JCMA. 2008;71:583–586. doi: 10.1016/S1726-4901(08)70174-6. 19015058 [DOI] [PubMed] [Google Scholar]
- Marchettini P., Formaglio F., Lacerenza M. Pain as heralding symptom in multiple sclerosis. Neurological Sciences. 2006;27:s294–s296. [Google Scholar]
- McDonald W.I., Compston A., Edan G., Goodkin D., Hartung H.P., Lublin F.D., McFarland H.F., Paty D.W., Polman C.H., Reingold S.C., Sandberg-Wollheim M., Sibley W., Thompson A., van den Noort S., Weinshenker B.Y., Wolinsky J.S. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Annals of Neurology. 2001;50:121–127. doi: 10.1002/ana.1032. 11456302 [DOI] [PubMed] [Google Scholar]
- Meaney J.F., Watt J.W., Eldridge P.R., Whitehouse G.H., Wells J.C., Miles J.B. Association between trigeminal neuralgia and multiple sclerosis: role of magnetic resonance imaging. Journal of Neurology, Neurosurgery, and Psychiatry. 1995;59:253–259. doi: 10.1136/jnnp.59.3.253. 7673952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minagar A., Sheremata W.A. Glossopharyngeal neuralgia and MS. Neurology. 2000;54:1368–1370. doi: 10.1212/wnl.54.6.1368. 10746612 [DOI] [PubMed] [Google Scholar]
- Nakashima I., Fujihara K., Kimpara T., Okita N., Takase S., Itoyama Y. Linear pontine trigeminal root lesions in multiple sclerosis: clinical and magnetic resonance imaging studies in 5 cases. Archives of Neurology. 2001;58:101–104. doi: 10.1001/archneur.58.1.101. 11176942 [DOI] [PubMed] [Google Scholar]
- O'Connor A.B., Schwid S.R., Herrmann D.N., Markman J.D., Dworkin R.H. Pain associated with multiple sclerosis: systematic review and proposed classification. Pain. 2008;137:96–111. doi: 10.1016/j.pain.2007.08.024. 17928147 [DOI] [PubMed] [Google Scholar]
- Pichiecchio A., Bergamaschi R., Tavazzi E., Romani A., Todeschini A., Bastianello S. Bilateral trigeminal enhancement on magnetic resonance imaging in a patient with multiple sclerosis and trigeminal neuralgia. Multiple Sclerosis (Houndmills, Basingstoke, England) 2007;13:814–816. doi: 10.1177/1352458506075261. 17613612 [DOI] [PubMed] [Google Scholar]
- Poldrack R.A., Fletcher P.C., Henson R.N., Worsley K.J., Brett M., Nichols T.E. Guidelines for reporting an fMRI study. NeuroImage. 2008;40:409–414. doi: 10.1016/j.neuroimage.2007.11.048. 18191585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polman C.H., Reingold S.C., Banwell B., Clanet M., Cohen J.A., Filippi M., Fujihara K., Havrdova E., Hutchinson M., Kappos L., Lublin F.D., Montalban X., O'Connor P., Sandberg-Wollheim M., Thompson A.J., Waubant E., Weinshenker B., Wolinsky J.S. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Annals of Neurology. 2011;69:292–302. doi: 10.1002/ana.22366. 21387374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald W.I., Compston A., Edan G., Goodkin D., Hartung H.P., Lublin F.D., McFarland H.F., Paty D.W., Polman C.H., Reingold S.C., Sandberg-Wollheim M., Sibley W., Thompson A., van den Noort S., Weinshenker B.Y., Wolinsky J.S. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Annals of Neurology. 2001;50:121–127. doi: 10.1002/ana.1032. 11456302 [DOI] [PubMed] [Google Scholar]
- Ramirez-Lassepas M., Tulloch J.W., Quinones M.R., Snyder B.D. Acute radicular pain as a presenting symptom in multiple sclerosis. Archives of Neurology. 1992;49:255–258. doi: 10.1001/archneur.1992.00530270069020. 1536627 [DOI] [PubMed] [Google Scholar]
- Poser C.M., Paty D.W., Scheinberg L., McDonald W.I., Davis F.A., Ebers G.C., Johnson K.P., Sibley W.A., Silberberg D.H., Tourtellotte W.W. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Annals of Neurology. 1983;13:227–231. doi: 10.1002/ana.410130302. 6847134 [DOI] [PubMed] [Google Scholar]
- Ropele S., de Graaf W., Khalil M., Wattjes M.P., Langkammer C., Rocca M.A., Rovira A., Palace J., Barkhof F., Filippi M., Fazekas F. MRI assessment of iron deposition in multiple sclerosis. Journal of Magnetic Resonance Imaging: JMRI. 2011;34:13–21. doi: 10.1002/jmri.22590. 21698703 [DOI] [PubMed] [Google Scholar]
- Rose A.S., Ellison G.W., Myers L.W., Tourtellotte W.W. Criteria for the clinical diagnosis of multiple sclerosis. Neurology. 1976;26:20–22. doi: 10.1212/wnl.26.6_part_2.20. 58393 [DOI] [PubMed] [Google Scholar]
- Svendsen K.B., Sørensen L., Jensen T.S., Hansen H.J., Bach F.W. MRI of the central nervous system in MS patients with and without pain. European Journal of Pain (London, England) 2011;15:395–401. doi: 10.1016/j.ejpain.2010.09.006. 20947397 [DOI] [PubMed] [Google Scholar]
- Tanei T., Kajita Y., Wakabayashi T. Motor cortex stimulation for intractable neuropathic facial pain related to multiple sclerosis. Neurologia Medico-Chirurgica. 2010;50:604–607. doi: 10.2176/nmc.50.604. 20671392 [DOI] [PubMed] [Google Scholar]
- Tortorella P., Rocca M.A., Colombo B., Annovazzi P., Comi G., Filippi M. Assessment of MRI abnormalities of the brainstem from patients with migraine and multiple sclerosis. Journal of the Neurological Sciences. 2006;244:137–141. doi: 10.1016/j.jns.2006.01.015. 16530789 [DOI] [PubMed] [Google Scholar]
- Tosi L., Righetti C.A., Zanette G., Beltramello A. A single focus of multiple sclerosis in the cervical spinal cord mimicking a radiculopathy. Journal of Neurology, Neurosurgery, and Psychiatry. 1998;64:277. doi: 10.1136/jnnp.64.2.277. 9489549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey I. Neuroimaging of pain mechanisms. Current Opinion in Supportive and Palliative Care. 2007;1:109–116. doi: 10.1097/SPC.0b013e3282efc58b. 18685351 [DOI] [PubMed] [Google Scholar]
- Vandenbroucke J.P. In defense of case reports and case series. Annals of Internal Medicine. 2001;134:330–334. doi: 10.7326/0003-4819-134-4-200102200-00017. 11182844 [DOI] [PubMed] [Google Scholar]
- Vilisaar J., Constantinescu C.S. SUNCT in multiple sclerosis. Cephalalgia: an International Journal of Headache. 2006;26:891–893. doi: 10.1111/j.1468-2982.2006.01110.x. 16776709 [DOI] [PubMed] [Google Scholar]
- Wise R.G., Tracey I. The role of fMRI in drug discovery. Journal of Magnetic Resonance Imaging: JMRI. 2006;23:862–876. doi: 10.1002/jmri.20584. 16649197 [DOI] [PubMed] [Google Scholar]
- Yetimalar Y., Seçil Y., Inceoglu A.K., Eren S., Başoğlu M. Unusual primary manifestations of multiple sclerosis. New Zealand Medical Journal. 2008;121:47–59. 18677330 [PubMed] [Google Scholar]


