Abstract
The resilience construct has received a great deal of attention as a result of the long wars in Iraq and Afghanistan. The discourse about resilience, especially the promise of promoting it and mitigating risk for serious post-traumatic negative outcomes among service members and veterans, is hopeful and encouraging. Remarkably, most service members exposed to horrific war trauma are not incapacitated by the experience. Yet, resilience is elusive and fleeting for many veterans of war. In this paper, I address some of the complexities about resilience in the context of exposure to war stressors and I offer some assumptions and heuristics that stem from my involvement in the dialogue about resilience and from experiences helping prevent post-traumatic stress disorder among active-duty service members with military trauma. My goal is to use my observations and applied experiences as an instructive context to raise critical questions for the field about resilience in the face of traumatic life-events.
Keywords: resilience, military trauma, indicated prevention, post-traumatic stress disorder
1. Introduction
The resilience construct has received a great deal of attention in the stress and trauma fields especially as a result of 9–11, an event that raised the spectre of a future with mass violence, terror and loss in the consciousness of citizens, care-communities, academics and policy-makers. The discourse about resilience has also been shaped and intensified by the long wars in Iraq and Afghanistan—approximately 2.5 million US service members have been deployed to these wars and 1.5 are still deployed overseas 13 years on. In this time frame, it might be said that we have emerged as an uneasy, concerned and weary society arguably looking for comfort and reassurance. The promise of promoting resilience and mitigating risk for serious post-traumatic negative outcomes among those who serve in the military during time of sustained wars is hopeful and encouraging. Remarkably, most service members exposed to severe war trauma are not incapacitated by the experience. However, we need to be cautious; resilience is very complex, multiply determined, and elusive and fleeting for many war veterans.
In this paper, I address some of the complexities about the construct of resilience and I offer some assumptions and heuristics that stem from my involvement in the dialogue about resilience in the face of trauma generally and war trauma specifically. Because of the uniqueness of the military sub-population and the extraordinary demands of war, which includes perpetration of violence and killing, adaptation to traumatic war experiences, in particular, is relatively incomparable to the wide variety of no less important forms of resilience in the face of other acute and chronic stressors, such as poverty, poor living conditions, disease, disability, political violence, occupational demands and so forth. In this effort, I will not be addressing the similarities and differences in the varieties of resilience contexts, nor will I be offering comments about what can be learned about resilience of all kinds from resilience in the context of war trauma. I will also be framing resilience in the war-trauma context in mental health terms, indexed chiefly by the severity of post-traumatic stress disorder (PTSD) symptoms. PTSD is one of the most common mental health outcomes from war among US military personnel (in the UK, the most common mental disorder is alcohol abuse [1]) and the discourse about resilience in the military has underscored the need to prevent or mitigate PTSD. However, it should be emphasized that service members and veterans may have PTSD and manifest other types or forms of resilience, and veterans may have minimal PTSD symptoms, yet have a range of problems in living and wellness deficits that are undeniable signs of a lack of resilience.
My perspective stems from my experience advising, researching and caring for active-duty service members and veterans exposed to various military traumas. My goal is to use my observations as an early interventionist and the extensive cumulative knowledge about the impact of war on service members and veterans as an instructive context to raise critical questions for the field about resilience. In my view, those who promote and study resilience in the face of war-zone stressors fail to sufficiently appreciate that much is unsettled and unknown. There is a lack of specificity or agreement about numerous fundamental questions: how should resilience be operationalized? What is it? Is there only one form? What are people resilient to? When does it manifest and in what context? Most importantly, can it be trained or promoted?
Since 9–11, it appears that at least two factors have motivated the focus on resilience. First, researchers, informed by theory, observation, applied field experiences and epidemiological efforts, were critical about the long-standing tradition in the culture, media and among policy-makers that regardless of role, culture and context, exposure to any traumatic life experience and serious loss is sufficient to convey serious risk for PTSD and other mental and behavioural health problems implicated by exposure to these horrific life experiences [2,3]. This type of thinking about risk had led to a one-size-fits-all thinking about the care needs of trauma and loss victims—the assumption was that everyone needed some kind of crisis intervention or grief counselling to ensure resilience. The equal risk model, for want of a better term, is unfounded and the intervention strategies that flow from it are problematic because they are not evidence-based [4], rather they often stem from heartfelt organizational needs to do something in the face of tragedy. Historically, early interventions for victims of trauma typically entail outsiders intervening with one-off strategies that fall short in several respects [5]. The prevention strategies may be intrusive for some; fail to appreciate and leverage indigenous resources that promote healing and recovery; waste professional support resources on the majority who do not need them; and overemphasize the normality of various signs and symptoms of early reactions. The latter merits a separate explanation and focus.
Because only a small minority of people exposed to trauma develops mental illness as a result, many assume that if a person's immediate response to trauma is not demonstrable incapacitation it is normal. In the military, this assumption often leads care-providers and leaders to foster the expectation among service members that any acute experience will abate and any impairment in functioning will be temporary. In the field, in terms of operational policy, this model stems from concerns about inappropriately pathologizing and over-medicalizing true normal reactions (false positives). The binary expectation of normality or incapacitation can be functional in an operational environment because it may be inappropriate for leaders to suggest to service members after battle, when troops are vulnerable and suggestible, that what is being experienced is disordered, which may foster a putative iatrogenic type of false positive reaction. However, the assumption that, short of mental illness, all reactions to extraordinary stress are normal is not only anachronistic in terms of the study of serious and sustained trauma but it begs the question: if most reactions are normal, what is there to prevent—why provide even one-off counselling of any sort? What I will argue below is that these issues are inextricably bound by the type of traumatic context and the degree and type of exposure. It is one thing to predict positive adaptation after an automobile accident; it is entirely another to think about what people need and to predict what will happen over time after sustained deprivation, torture and sexual violence. Consider for a moment the latter type of experience. If normality is emphasized, what is someone going to think when their invisible wounds, such as being haunted and anguished by the experience, consume them and they are having a hard time functioning ‘normally’? Especially early on, most cases such as these will not have a mental disorder, yet their suffering and impairment is not normal. What will these people think of professionals or leaders if they are dissociating, numb and disorganized while they listen to messages about normality early on in their adaptation? The danger is that carer and leaders will not be trusted and they will lose credibility or, worse yet, those who are understandably abnormally affected will feel stigmatized and ashamed—they will regard their response as due to personal weakness and blame themselves.
In addition to setting in motion innovative research on models of adaptation to trauma, loss and serious life challenges that posit varied response typologies (one of which is resilience; e.g. [6]), the emphasis on resilience, especially in the trauma and PTSD field, stems from the aspiration to determine the modifiable and trainable keys to successful navigation of high-magnitude events and losses. In other words, it is not enough to expect high rates of resilience and let nature run its course. The challenge is to assess individuals over time to help those who need help bouncing back and to collect information about what predicts adaptive outcomes. Knowing what predicts sustained resilience in the face of horrific traumatic events in the military will allow professionals to develop and adopt training and preparation programmes, and policy-makers can shape post-exposure contexts to promote these outcomes and processes.
2. What is resilience?
Resilience, like the constructs stress and trauma, signifies a process and an outcome. As a process, resilience entails a relatively unspecified and under-researched transaction between personal traits and resources (and the group) and the environment. These transactions entail hard-wired, psychological, biological, behavioural, social and spiritual processes that mediate outcomes. In simplistic terms, the first transaction in the context of exposure to traumatic stressors is the person's automatic response to the profound provocation and his or her appraisal of the meaning and implication of the experience. The second entails the complex interplay of the post-traumatic experience and personal coping assets and options (social, occupational, cultural and so forth; e.g. [7]). The outcome of these transactions between lived experience and real and appraised resources to manage and adapt is highly dependent on the degree of exposure, whether maliciousness was involved, the age and development of the person, and social, cultural, and economic resources.
The terms resilient or resilience most often refer to an outcome. That is, a person who manages and reconciles a traumatic experience in the moment and over time is said to have navigated the impact successfully. The key challenges are to define impact and to be clear about what success means, issues I hope to clarify.
Resilience as an outcome is an unfolding process [8]; any given cross section is never sufficient to define resilience. In other words, resilience needs to endure or it is not a characteristic, but a temporary state or stage. Consider delayed trauma-linked adaptation problems (e.g. PTSD, substance abuse, aggression, withdrawal, work problems, etc.) and apparently spontaneous resolution of early incapacitation [9–11]. It is safe to assume that for many service members exposed to sustained and frequent trauma, resilience is a lifelong challenge. Life context and life demands change. Failure experiences and losses can trigger a re-emergence of problems linked to trauma. Alternatively, rewarding relational, occupational and financial experiences improve adaptation to trauma.
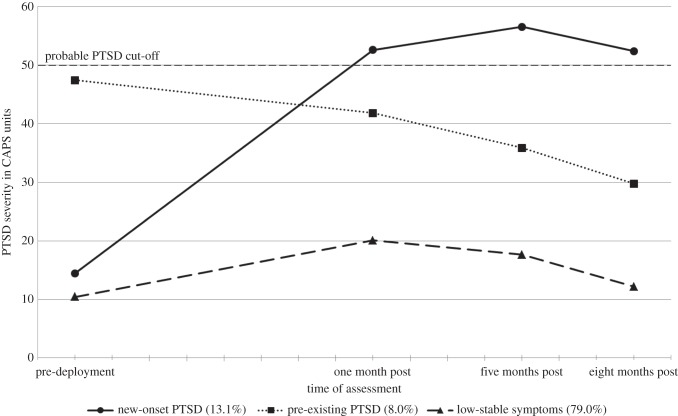
Generally, there are two broad definitions of resilience. One model, depicted in figure 1, posits that resilience entails enduring minimal or no disruption in a person's functions [6]. Another model poses that resilience is the ability to bounce back from immediate understandably disrupted states and from initial pre-clinical responses and impairments. I prefer this second definition for several reasons. The first model conflates resilience with low exposure. Although there is empirical support for the model first proposed by Bonanno et al. [12] and Horton et al. [13], the studies used to validate it have been longitudinal evaluations of populations with highly varying degrees of exposure to a given traumatic context (e.g. 9–11). Consequently, it is understandable that so-called resilience is the most common type of adaptation because the findings are confounded by degree of exposure. In other words, to a large degree, the flat response over time is due to low levels of exposure to traumatic stressors, which is typically the case with large cohort studies. Figure 2 shows a graph that depicts the results from a study conducted by Bonanno [6], which evaluated the course of PTSD among 4394 service members with highly heterogeneous exposure to war-zone stressors in Iraq or Afghanistan. Here, not surprisingly, the modal trajectory entailed virtually no PTSD symptoms (the lowest score possible was 17).
Figure 1.
Hypothetical patterns of disruption following loss or traumatic stressors.
Figure 2.
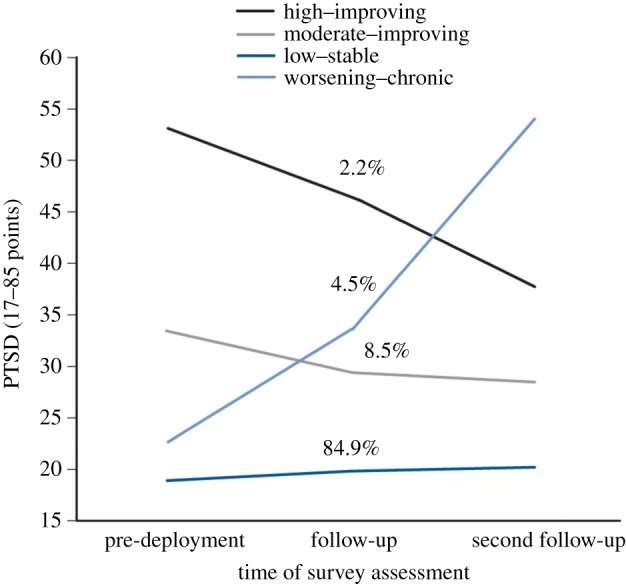
Post-traumatic stress over time among deployed service members. (Online version in colour.)
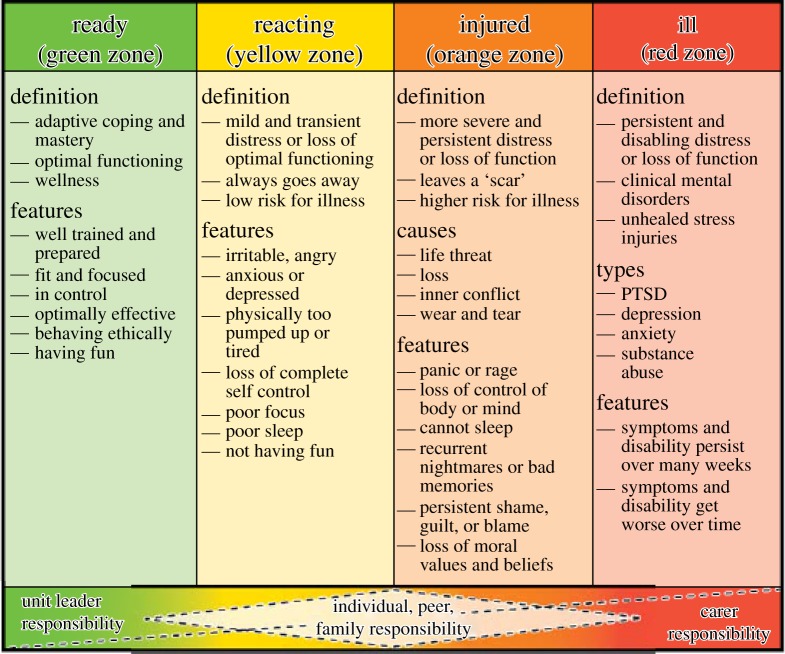
By contrast, cohort studies that evaluate individuals with shared high-magnitude exposure to traumatic stressors confirm this expectation. For example, in a recent longitudinal study of rape victims that my colleagues and I conducted (see figure 3), the modal response over time was what we labelled as recovery, namely high PTSD symptoms within a week of the sexual assault followed by resolution six months later. Of note, the type of reaction we labelled as resilient also entailed significant levels of PTSD soon after the trauma; these women bounced back over time. Figure 4 shows a graph that tracks the course of PTSD symptoms among a cohort of Marines that were highly exposed to war-zone traumatic stressors [14]. In this study, the modal trajectory was low and stable PTSD symptoms but this course was quadratic. This course entailed a significant increase in PTSD symptoms over the deployment cycle, followed by a reduction over time—a bouncing back.
Figure 3.
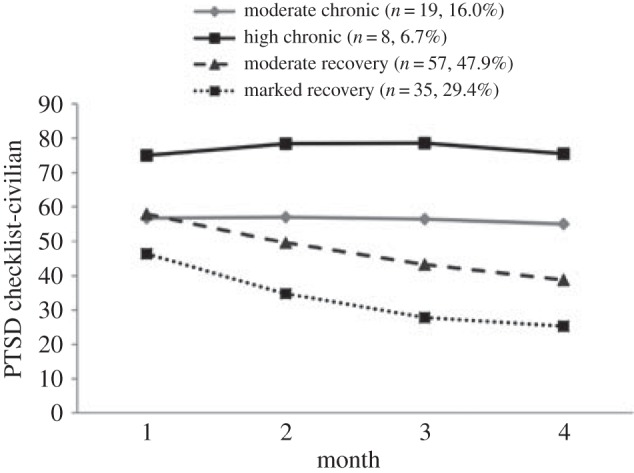
Trajectories of PTSD symptoms among sexual assault survivors.
Figure 4.
PTSD trajectories among Marines with high exposure to war-zone stressors.
Another reason why I believe that the ability to bounce back is the right way to operationalize resilience is that it acknowledges that everyone has a line that can be crossed and which leads to severe initial disruption of normal functions and functioning. For example, even the most mature, healthy, battle-tested, well-trained, well-supported, decorated and hard-nosed senior non-commissioned officer has a breaking point. In my view, the truest test of the capacity for resilience is the ability to bounce back from entirely understandable and human crushing blows (i.e. serious disruptions in biological, psychological, social and spiritual capacities). Moreover, it is unhelpful and misguided to expect people to be uber resistant and unscathed by all experiences. Yet, a great deal of attention and resources have been devoted to training people in the high-risk dangerous occupations in the hope of creating minimally disrupted professionals who can grow positively from stress and exposure to traumatic stressors. Arguably, these initiatives have failed to draw sufficient attention to training leaders, peers and individuals about what to do if understandable psychic injuries occur. Also, few resources have been devoted to studying the causes of bouncing back from high-magnitude impacts and disruptions.
Ideally, there would be a proven way to help people grow and to be minimally affected by serious occupational exposures to traumatic stressors. To be worth the effort, formal prevention programmes have to demonstrate incremental validity. Resilience training efforts need to account for a substantial amount of variance in long-term outcomes above and beyond the critical indigenous sources of occupational resilience, healing and recovery (e.g. training, preparation, leadership, peer and family supports [15–17]). In this regard, it is worth considering how the US Army defined resilience and tackled resilience training with the Comprehensive Soldier Fitness Program (CSF).
3. Defining resilience and promoting it in the US Army
In 2009, the Army implemented CSF, a very well-funded universal prevention initiative designed to train all soldiers and their families in mental fitness and resilience [18–20]. CSF is the largest mental and behavioural health prevention programme ever undertaken, disseminated to well over a million soldiers to date. In CSF, resilience is defined as ‘the maintenance of normal functioning in the face of adversity’ [19, p. 8]. The Army states that CSF aims to ‘…shift the normal psychological performance ‘curve’ of the soldier population to the right, that is, to increase the number of soldiers who derive meaning and personal growth from their combat experience (the rightmost part of the curve), to increase the number of soldiers who complete combat tours without pathology, and to decrease the number of soldiers who develop stress pathologies’ [18, p. 20].
The CSF training that all soldiers are mandated to receive is based on positive psychology. The positive psychology perspective argues that in the context of prevention, positive human traits such as optimism and contentment can buffer against psychopathology in the face of military adversity and traumatic stressors. Accordingly, identifying and amplifying these traits in at-risk individuals prevents mental health problems [20]. The empirical justification for CSF comes from the Penn Resiliency Program which uses positive psychology methods to prevent depression in adolescents. Unfortunately, a meta-analysis of the Penn Resiliency Program's effect on depressive symptoms concluded that there was no evidence that the programme is effective in ‘preventing, delaying or lessening the intensity or duration of future psychological disorders’ [21, p. 1051]. Indeed, my colleagues and I conducted a systematic review of the evidence used to support the efficacy and impact of CSF and we found that there is no evidence that CSF prevents PTSD or that CSF has incremental validity in altering response to daily hassles and adversities [22].
It is not surprising that CSF would be attractive to the Army leaders who fund and promote it because it is focused on putatively trainable positive proactive wellness behaviours that could easily be framed as a form of mental and relational ‘fitness’. The model is strength-based and eschews the equal risk and the medical pathology-based models. Each of these features is understandably attractive and laudable. It makes sense that the military is attracted to a solution that does not require the imposition and intrusion of mental health professionals in-theatre and in-garrison. I also suspect that senior leaders who had been exposed to the hell of war but grew and matured from these experiences resonated with the central thesis of the positive psychology approach, namely that with the right frame of mind, PTSD is not destiny. Rather, service members can be taught ways to ensure minimal impact if not growth.
In my view, at the start of the conversation about the relevance of the positive psychology approach for what was to become CSF someone needed to ask about the core assumptions about resilience that were being considered, particularly whether maintenance of normal functioning in the face of non-combat hassles and adversities is the right framework to consider. In other words, why would cognitive and behavioural wellness strategies, which may help service members adapt to work and relationship conflicts, daily hassles and chronic adversities, be sufficient to help them bounce back from exposure to the serious and grotesque harms of war? Other questions would be: if service members have war experiences that putatively cross their personal threshold, what are they to do—will they know what to do or, more importantly, will peers and leaders know what to do? How will positive psychological strategies be seen by service members in this context? Might the credibility of the programme be in jeopardy? And, worst of all, what about service members who believe that CSF training is sufficient and they look around them and their peers appear to be unharmed yet they are psychically injured by a recent experience? How could this not lead to the unintended iatrogenic consequence of greater stigma, shame and withdrawal?
4. The spectrum of post-traumatic outcomes
If resilience is a process of bouncing back (or as some have suggested, bouncing forward; e.g. [23]), what is the experience that requires a bouncing back from? And, if for some, the state is non-normal, what can be done to facilitate bouncing back? To my mind, Bill Nash, a retired Navy captain, psychiatrist and former head of Navy and Marine Corps combat and operational stress control, was the first to posit a formal conceptual framework that specifically defines a pre-clinical sub-syndromal state of stress injury that entails dyscontrol and disinhibition (the experiential line of dysfunction that can occur post-traumatically; see [24]).
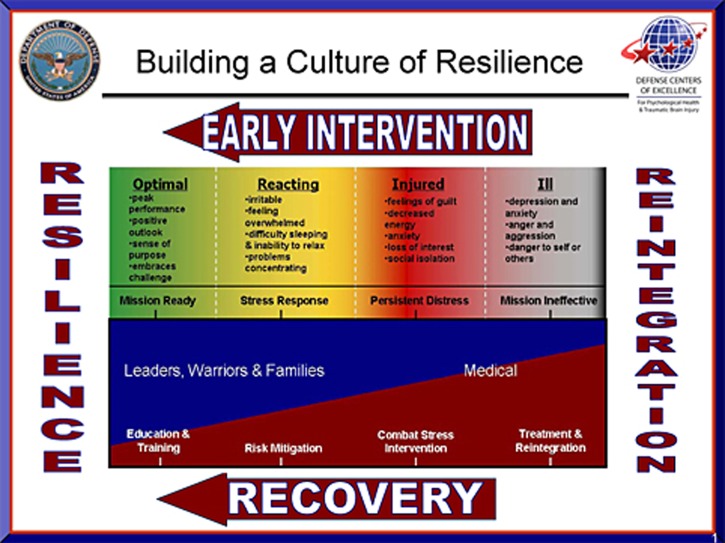
In Nash's model (see figure 5), in the context of the military, service members' adaptation lies along this broad spectrum or continuum, ranging from wellness and thriving to illness and disability [16,25]. In collaboration with military leaders, chaplains and medical and mental health professionals, Nash developed the Combat and Operational Stress Continuum Model, a heuristic that divided the spectrum of possible stress states into four colour-coded zones labelled ‘Ready’ (green zone), ‘Reacting’ (yellow zone), ‘Injured’ (orange zone) and ‘Ill’ (red zone). This model is doctrine in the Navy and Marine Corps and variants have also been employed in the Department of Defense (see figure 6). This model counters the dichotomous thinking about the impact of trauma, particularly in the military, namely that a response is either normal and good-to-go or pathological.
Figure 5.
The Navy and Marine Corps Stress Continuum Model. (Online version in colour.)
Figure 6.
Defense Centers of Excellence resilience continuum. (Online version in colour.)
The stress injury model codifies pre-clinical states of psychological and behavioural health problems that not only cause military personnel and their families to suffer, but can also affect military performance (mission readiness) and increase healthcare costs [26]. Pre-clinical reactions entail states of functional impairment and distress that cannot be diagnosed as a psychiatric illness (red zone), but they are behaviours and states of mind and body that are non-normal and demonstrably impairing. In the mental health field, non-trivial pre-clinical levels of distress and impairment after exposure to traumatic stressors have also been called sub-syndromal, sub-threshold or partial PTSD. Sub-syndromal PTSD increases risk for comorbid disorders, delayed onset PTSD and poor occupational outcomes similar to full PTSD. The prevalence rates for sub-syndromal PTSD among veterans of the Iraq and Afghanistan wars are approximately 22%, and pre-clinical cases have impairment and psychosocial difficulties significant enough to warrant care [27]. Importantly, returning veterans with sub-syndromal PTSD report similar rates of suicidal ideation, hopelessness and aggressive acts such as physical assault and destruction of property, as those with full PTSD [26].
5. The spectrum of prevention in the military
Without the orange stress injury zone between normal and disordered responses, there would be no way to assess service members that may need help to bounce back. A system that is able to identify these injuries and assist service members in the least restrictive, least intrusive and most indigenous manner (leveraging cultural and contextual assets) is arguably manifesting what might be called programmatic resilience. This entails resilient systems that can identify individuals in a way that obviates shame and promotes acceptance and follow-through of recommended courses of action. In the military, it is leaders and peers that are most likely to possess these capacities. To put these prevention efforts in context and to further explain the unique value of the stress injury model, it is worth describing the spectrum of prevention and care that is theoretically possible in the military.
Various military task forces pertaining to mental health, resilience and prevention have underscored that to maintain warfighter readiness, the military needs to expand mental health service resources and prevention strategies across the deployment cycle and to bolster the identification of stress injuries and disorders, and intervention needs to build resilience and promote healing and recovery from combat and operational stressors [28]. In service of these goals, the military has a three-tiered system of care starting with prevention, then identification and treatment of mental disorders, followed by reintegration back into units. The military faces a host of challenges to realize this comprehensive vision. For example, there are numerous acculturated barriers to care and access to care problems.
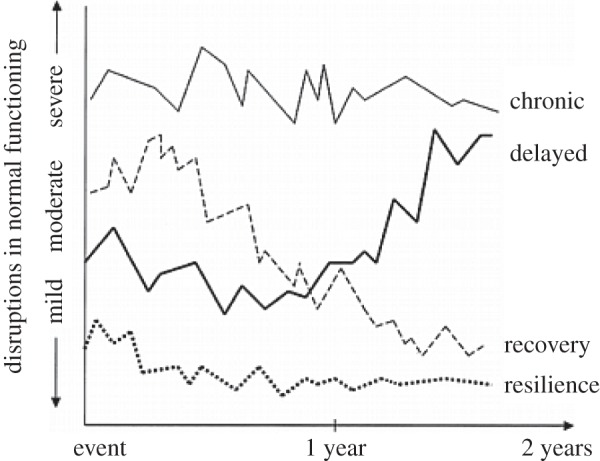
The Institute of Medicine (IOM) prevention scheme [29] (see figure 7) is especially pertinent to understanding and distinguishing the spectrum of prevention and care resources germane to the challenges and responsibilities of the US military. In the IOM framework, mental health prevention entails a continuum of strategies and ways of conceptualizing the needs of individuals at risk, from resilience promotion to after-care and rehabilitation for chronic conditions. Formal prevention interventions are based on who they target: (i) universal prevention targets a whole population (CSF is an example), (ii) selective prevention stems from the equal risk model and targets all members of sub-groups exposed to at least some degree to trauma, and (iii) indicated prevention targets at-risk individuals with stress injuries/pre-clinical symptoms and impairments in functioning.
Figure 7.
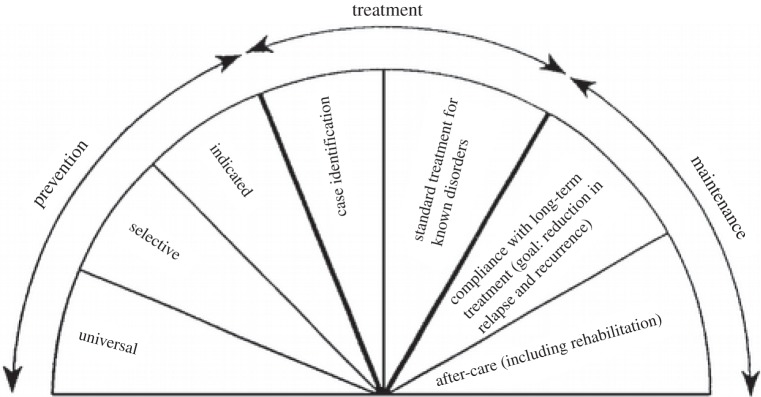
The Institute of Medicine prevention scheme.
Currently, in the military, troops are provided various forms of intrinsic and extrinsic universal prevention programmes (and behavioural health promotions) to prepare for military stressors. Examples of intrinsic forms of universal prevention include tough realistic training, effective leadership and cohesive unit functions. An example of an extrinsic prevention effort is the CSF described above. In addition, in many contexts, all members of units exposed to shared military trauma and loss are provided selective prevention strategies in the form of variants of debriefing for all unit members, regardless of degree of exposure or impairment [4]. In terms of targeting mental disorders such as PTSD, the military has been responsive to the need for case identification and evidence-based treatments of PTSD and other mental health disorders across the deployment cycle. And, much attention has been paid to promoting reintegration of service members back into their units should they require specialty care and respite.
However, indicated prevention programmes and research is relatively underdeveloped, notwithstanding a recent US military Instruction about the Maintenance of Psychological Health in Military Operations [30], which codifies the necessity to address pre-clinical stress injuries and ‘establishes requirements for activities that support psychological health in military operations for the early detection and management of combat and operational stress reactions in order to preserve mission effectiveness and warfighting capabilities and mitigate the adverse physical and psychological consequences of exposure to severe stress’. Indicated prevention entails targeting service members who develop pre-clinical PTSD across the deployment cycle so that they do not develop mental disorders and related disabilities (a form of resilience). The care and research gap that exists in this regard is unfortunate because as stated above, pre-clinical states impair functioning and create risk for clinical disorders and long-term dysfunction. In addition, the best available evidence supports the effectiveness of indicated prevention interventions that target subclinical distress, rather than selective or universal prevention interventions [2,31].
To reiterate, one of the obstacles to developing and testing indicated prevention in the military is the assumption that all pre-clinical stress symptoms and impairment are normal and will naturally abate. Although many service members will bounce back based on non-clinical resources and personal resourcefulness, others will stay sufficiently symptomatic or become clinical cases. Sustained sub-syndromal PTSD is statistically non-normal and confers risk for PTSD and depression [32,33]. For example, among injury survivors, 90% of cases diagnosed with delayed onset PTSD 12 months post-trauma had been diagnosed with sub-syndromal PTSD at three months post-trauma [34]; similarly, 70% of car accident survivors with sub-syndromal acute stress symptoms were diagnosed with PTSD 2 years later [35]. In addition, pre-clinical states interfere with service members' ability and motivation to function effectively in their military roles [36]. However, because some service members with pre-clinical impairment may recover without formal assistance (via a combination of supports, guidance/leadership, and respite and rest) an indicated prevention programme needs to demonstrate incremental validity. That is, it has to be substantially better than the passage of time.
6. Resilience to what?
The prevailing theory about why acute and chronic stress and trauma is harmful is the neo-conditioning fear-systems-based biological model of uncontrollable stress. This model is doctrine in the medical model of PTSD. The sine qua non is exposure to life-threat trauma, which triggers an unconditioned ‘fight-flight-or-freeze’ response, initiating activity in the hypothalamic–pituitary–adrenal axis, the locus coeruleus and noradrenergic systems, and the neuro-circuitry of fear system. This hard-wired response to life-threat is richly encoded in memory and conditioned to a variety of peri- and post-event stimuli. In this framework, PTSD is in effect the manifestation of traumatic Pavlovian conditioning and learning. In life-threat contexts, this model is compelling and valid from a variety of perspectives. For example, it is not surprising that clinical trials of exposure/extinction-based treatments for single incident, adult onset life-threat trauma (motor vehicle accidents and sexual assault) are positive (see [37]). To date, most resilience and prevention models nearly exclusively stem from the life-threat fear-conditioning model.
However, my colleagues and I have argued that in the military in a time of war (and other complex trauma contexts), life-threat trauma is not the only hazard that threatens resilience [15]. Cumulative wear-and-tear, loss and inner conflict from morally injurious experiences, such as killing or failing to prevent unethical behaviour, are co-equal challenges to resilience [24]. Each of these resilience challenges has a different phenomenology, aetiology and course from life-threat experiences. Consequently, each requires a different perspective on resilience but to date the focus has been on stress and fear.
Yet, there are good reasons to assume that there are very high rates of resilience to life-threat trauma in the modern military. Service members are self-selected (and screened) to be able to be trainable in the face of life-threats. The modern military also provides exceptional tough realistic training for various roles and potential high-threat experiences. Because of the warrior ethos and training, high-threat experiences are not likely to elicit the kinds of peri-event responses that define life-threat trauma in other contexts, namely intense fear, helplessness or horror. Performing your duty, assisting your peers and surviving in battle are not laden with internal and social conflicts; it will likely be construed as heroic, a source of pride and resonant with role-, self- and group-identity [24]. For those that develop a danger-based stress injury, arguably the most pressing problem is not high states of fear and arousal but the self-condemnation and guilt that may arise from letting peers and leaders down because of a temporary incapacitation in the field. Moreover, there is reason to assume that most threat-based stress injuries are readily healed by indigenous military rituals and assets. For example, peer and social supports, training and effective leadership are often sufficient to recover from high-threat experiences. The social element is particularly important; there are ritualized opportunities to operationally debrief and to bond by sharing narratives about common high-threat experiences. In addition, in pure learning theory terms, leaders in the theatre of operations typically ensure sufficient exposure to high fear contexts to provide natural extinction of any conditioned fear. Wear-and-tear challenges are also typically handled well; leaders make sure that service personnel get respite after highly charged and sustained operational demands.
By contrast, I would argue that there are far fewer indigenous military resources to support resilience in the face of loss of life (especially the survivor guilt that can ensue [38]), and the lasting impact of perpetrating, failing to prevent or bearing witness to acts that transgress deeply held moral beliefs and expectations, what has been termed moral injury [39]. Furthermore, the conditioning and learning model built on the concept of high threat and fear does not sufficiently explain, predict or address the needs of many who are exposed to the divergent and diverse psychic injuries of war (and many other traumatic contexts). Resilience promotion and prevention efforts need to consider different mechanisms of change, targets and intervention strategies. Recall the senior non-commissioned officer described above; the sufficient provocation, injury or insult to lead to a stress injury is not likely to be personal life-threat, but rather a child's suffering, a moral or ethical transgression in a moment of blind rage, or the grotesque loss of a special and loved member of his or her unit. Do current resilience models sufficiently account for these experiences?
To put these issues in context, consider this thought experiment: what might promote a service member's healing and recovery from a single life-threat incident, such as a sniper attack when no one was hurt (high threat)? Contrast this with a service member who is plagued by the aftermath of an improvised explosive device explosion that killed her best friend who she witnessed die (traumatic loss). Contrast that with a service member who is haunted by an incident where he acted out his rage due to a mortar attack that killed his friend the day before (he was not present when that happened) by killing an unarmed civilian man who was agitated during a house search (moral injury related to perpetration). Compare that with the experience of a service member who is angry and demoralized by a betrayal by a trusted leader whose ruthless and capricious decision led to the unnecessary deaths of civilians. Does the fear-conditioning model fit any case but the first?
7. Different types of resilience in the military
Resilient outcomes are multi-dimensional. For example, people exposed to trauma for various reasons may be able to function within normal limits, but they suffer from significant distress and internal conflict. This might be called functional resilience. Alternatively, others may have facets of their social and behavioural repertoires affected by stress exposure but other aspects are unaffected. This might be termed compartmentalized or system-specific resilience. For example, there may be family strife and conflict, but the person is well connected with peers.
In the military, almost any mission can expose service members to mortal danger, loss and moral compromise with ferocity, intensity and relentlessness hard to imagine in most other settings (see [24]). Both during and after deployment, service members face the challenge of mourning losses, finding meaning in experiences that seem senseless and making peace with enduring memories of death and destruction. Returning from deployment exposes service members to different adaptive challenges, which may include the relatively abrupt transition to civilian contexts, a lost relationship or other family problems, a lost civilian job or serious financial problems. We have argued that resilience challenges for military service members and the organizations that support them entail three broad forms [5]: (i) operational resilience, or the ability to maintain occupational role functioning and psychological performance during operational deployments despite stressor exposures, and perhaps despite internal distress and conflict, (ii) post-deployment resilience, which may be defined as the ability to reacquire and maintain effective role functioning in largely non-military settings after returning from deployment, and thus to again be a productive member of a family and civilian society; and (iii) long-term psychological resilience, which may be defined as the enduring ability to adapt physically, mentally and spiritually to combat or operational exposures without developing a significant mental disorder or behavioural problem.
The traditional view has been that resilience framed as mental health response to traumatic stressors is the same as functional operational resilience, and such features as courage and fortitude can lead to mental resilience. This mind-set has increased the stigma associated with being damaged by the stress of military service, and erected barriers of shame and denial between injury and care [40]. In the military, observable indicators and metrics of performance and functioning may disguise poor levels of psychological resilience because even extreme internal strife and suffering may be invisible to most. Psychological resilience is more than merely meeting minimum standards of behaviour during circumscribed periods of time. To a much greater extent than operational or post-deployment resilience, psychological resilience in particular must be viewed as a process rather than a state or temporally consistent trait and studied longitudinally rather in cross section.
8. Summary
I have tried to describe the unique definitional, conceptual and operational challenges that arise when trying to study and promote resilience in the aftermath of exposure to traumatic stressors. I have used the military as an example of a unique culture and ethos, which no doubt will fail to capture the exigencies and nuances of different types of traumatic contexts. The point is that there really is no universally appropriate definition, model and applied framework for the construct of resilience. Time since event, context, culture, indigenous resources and the feasibility of prevention efforts to promote resilience, all vary and all matter.
Nevertheless, I have raised issues that should be useful for anyone studying resilience to consider. Namely, that in any given context there may be different forms of resilience, which means that resilience needs to be seen as a multi-dimensional construct. I have also underscored that resilience can never be defined or measured by a cross section; things change, adaptation is an unfolding process, a trajectory. Another point I wanted to emphasize is that adaptation to high-magnitude life-events and trauma should be construed along a continuum and especially that there is a response to trauma that is short of mental disorder but also not a normal stress reaction, namely stress injury. Finally, and most importantly, I defined resilience as bouncing back from an understandably human biological, social, psychological and spiritual response to extreme events. Some have argued that this bouncing back should be defined as recovery and resilience should be defined as minimal reactions over the long haul [6]. Because in many respects minimal reaction and impact is a proxy for relatively lower exposures, and especially low exposure to highly toxic losses and moral and ethical challenges, this definition of resilience is not appropriate. In effect, I have argued that resilience is a form of recovery. Each entails adaptation followed by a return of functioning and homeostasis.
References
- 1.Iversen AC. 2009. The prevalence of common mental disorders and PTSD in the UK military: using data from a clinical interview-based study. BMC Psychiatry 9, 68 ( 10.1186/1471-244X-9-68) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Litz BT, Gray MJ, Bryant R, Adler AB. 2002. Early intervention for trauma: current status and future directions. Clin. Psychol. Sci. Pract. 9, 112–134. ( 10.1093/clipsy.9.2.112) [DOI] [Google Scholar]
- 3.McNally RJ, Bryant RA, Ehlers A. 2003. Does early psychological intervention promote recovery from posttraumatic stress? Psychol. Sci. Public Interest 4, 45–79. [DOI] [PubMed] [Google Scholar]
- 4.Adler AB, Litz BT, Castro CA, Suvak M, Thomas JL, Burrell L, McGurk D, Right KW, Bliese PB. 2008. A group randomized trial of critical incident stress debriefing provided to U.S. peacekeepers. J. Traumatic Stress 21, 253–263. ( 10.1002/jts.20342) [DOI] [PubMed] [Google Scholar]
- 5.Nash W, Steenkamp M, Conoscenti L, Litz BT. 2012. The stress continuum model: a military organizational approach to resilience and recovery. In Resiliency in clinical practice (eds Southwick S, Litz BT, Friedman M, Charney D.), pp. 238–252. Cambridge, UK: Cambridge University Press. [Google Scholar]
- 6.Bonanno GA. 2004. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 59, 20–28. ( 10.1037/0003-066X.59.1.20) [DOI] [PubMed] [Google Scholar]
- 7.Lazarus RS, Cohen JB. 1977. Environmental stress. Human Behav. Environ. 2, 89–127. ( 10.1007/978-1-4684-0808-9_3) [DOI] [Google Scholar]
- 8.King DW, Vogt DS, King LA. 2004. Risk and resilience factors in the etiology of chronic posttraumatic stress disorder. In Early intervention for trauma and traumatic loss (ed. Litz BT.), pp. 34–64. New York, NY: Guilford Press. [Google Scholar]
- 9.Andrews B, Brewin C, Philpott R, Stewart L. 2007. Delayed-onset posttraumatic stress disorder: a systematic review of the evidence. Am. J. Psychiatry 164, 1319–1326. ( 10.1176/appi.ajp.2007.06091491) [DOI] [PubMed] [Google Scholar]
- 10.Bryant RA, Harvey AG. 2002. Delayed-onset posttraumatic stress disorder: a prospective evaluation. Aust. NZ J. Psychiatry 36, 205–209. ( 10.1046/j.1440-1614.2002.01009.x) [DOI] [PubMed] [Google Scholar]
- 11.Gray MJ, Bolton EE, Litz BT. 2004. A longitudinal analysis of PTSD symptom course: delayed-onset PTSD in Somalia peacekeepers. J. Consult. Clin. Psychol. 72, 909–913. ( 10.1037/0022-006X.72.5.909) [DOI] [PubMed] [Google Scholar]
- 12.Bonanno GA, et al. 2012. Trajectories of trauma symptoms and resilience in deployed US military service members: prospective cohort study. Br. J. Psychiatry 200, 317–323. ( 10.1192/bjp.bp.111.096552) [DOI] [PubMed] [Google Scholar]
- 13.Horton J, et al. 2010. Mental health trajectories and their predictors: application of latent growth mixture modeling in the millennium cohort study. Ann. Epidemiol. 20, 714–715. ( 10.1016/j.annepidem.2010.07.069) [DOI] [Google Scholar]
- 14.Nash WP, Boasso AM, Steenkamp MM, Larson JL, Litz BT. Submitted Posttraumatic stress in deployed marines: prospective trajectories of early adaptation. [DOI] [PubMed]
- 15.Litz BT, Steenkamp MM, Nash WP. 2014. Resilience and recovery in the military. In Facilitating resilience and recovery following trauma (eds Zoellner LA, Feeny NC.), pp. 113–136. New York, NY: Guilford Press. [Google Scholar]
- 16.Nash W, Krantz L, Stein N, Westphal R, Litz BT. 2011. Comprehensive soldier fitness, battlemind, and the stress continuum model: military organizational approaches to prevention. In Caring for veterans with deployment-related stress disorders: Iraq, Afghanistan, and beyond (eds Ruzek JI, Schnurr PP, Vasterling JJ, Friedman MJ.), pp. 193–214. Washington, DC: American Psychological Association. [Google Scholar]
- 17.Whealin JM, Ruzek JI, Southwick S. 2008. Cognitive behavioral theory and preparation for professionals at risk for trauma exposure. Trauma Violence Abuse 9, 100–113. ( 10.1177/1524838008315869) [DOI] [PubMed] [Google Scholar]
- 18.Cornum R, Matthews MD, Seligman ME. 2011. Comprehensive soldier fitness: building resilience in a challenging institutional context. Am. Psychol. 66, 4–9. ( 10.1037/a0021420) [DOI] [PubMed] [Google Scholar]
- 19.Lester PB, McBride S, Bliese PD, Adler AB. 2011. Bringing science to bear: an empirical assessment of the comprehensive soldier fitness program. Am. Psychol. 66, 77–81. ( 10.1037/a0022083) [DOI] [PubMed] [Google Scholar]
- 20.Seligman ME, Fowler RD. 2011. Comprehensive soldier fitness and the future of psychology. Am. Psychol. 66, 82–86. ( 10.1037/a0021898) [DOI] [PubMed] [Google Scholar]
- 21.Brunwasser SM, Gillham JE, Kim ES. 2009. A meta-analytic review of the Penn Resiliency Program's effect on depressive symptoms. J. Consult. Clin. Psychol. 77, 1042–1054. ( 10.1037/a0017671) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steenkamp MM, Nash WP, Litz BT. 2013. Posttraumatic stress disorder prevention in troops: review of the comprehensive soldier fitness program. Am. J. Prev. Med. 44, 507–512. ( 10.1016/j.amepre.2013.01.013) [DOI] [PubMed] [Google Scholar]
- 23.Walsh F. 2006. Strengthening family resilience, 2nd edn. New York, NY: Guilford Press.
- 24.Nash WP. 2007. Combat/operational stress adaptations and injuries. In Combat stress injuries: theory, research, and management (eds Figley CR, Nash WP.), pp. 33–63. New York, NY: Routledge. [Google Scholar]
- 25.Nash WP, et al. 2010. Consensus recommendations for common data elements for operational stress research and surveillance: report of a federal interagency working group. Arch. Phys. Med. Rehabil. 91, 1673–1683. ( 10.1016/j.apmr.2010.06.035) [DOI] [PubMed] [Google Scholar]
- 26.Jakupcak M, et al. 2007. Anger, hostility, and aggression among Iraq and Afghanistan war veterans reporting PTSD and subthreshold PTSD. J. Traumatic Stress 20, 945–954. ( 10.1002/jts.20258) [DOI] [PubMed] [Google Scholar]
- 27.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. 2009. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from operations Enduring Freedom and Iraqi Freedom. Depress. Anxiety 26, 745–751. ( 10.1002/da.20558) [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine of the National Academies. 2010. Preliminary assessment of readjustment needs of veterans, service members, and their families. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 29.Muñoz RF, Mrazek PJ, Haggerty RJ. 1996. Institute of Medicine report on prevention of mental disorders: summary and commentary. Am. Psychol. 51, 1116–1122. ( 10.1037/0003-066X.51.11.1116) [DOI] [PubMed] [Google Scholar]
- 30.Department of Defense Instruction (DoDI) 6490.05. 2011. Maintenance of Psychological Health in Military Operations.
- 31.Feldner MT, Monson CM, Friedman MJ. 2007. A critical analysis of approaches to targeted PTSD prevention: current status and theoretically derived future directions. Behav. Modif. 31, 80–116. ( 10.1177/0145445506295057) [DOI] [PubMed] [Google Scholar]
- 32.Andrews B, Brewin CR, Stewart L, Philpott R, Hejdenberg J. 2009. Comparison of immediate-onset and delayed-onset posttraumatic stress disorder in military veterans. J. Abnorm. Psychol. 118, 767–777. ( 10.1037/a0017203) [DOI] [PubMed] [Google Scholar]
- 33.Solomon Z, Bleich A, Koslowsky M, Kron S, Lerer B, Waysman M. 1991. Post-traumatic stress disorder: issues of co-morbidity. J. Psychiatr. Res. 25, 89–94. ( 10.1016/0022-3956(91)90002-R) [DOI] [PubMed] [Google Scholar]
- 34.Carty J, O'Donnell ML, Creamer M. 2006. Delayed-onset PTSD: a prospective study of injury survivors. J. Affect. Disord. 90, 257–261. ( 10.1016/j.jad.2005.11.011) [DOI] [PubMed] [Google Scholar]
- 35.Harvey AG, Bryant RA. 1999. The relationship between acute stress disorder and posttraumatic stress disorder: a 2-year prospective evaluation. J. Consult. Clin. Psychol. 67, 985–988. ( 10.1037/0022-006X.67.6.985) [DOI] [PubMed] [Google Scholar]
- 36.Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. 2008. Validation of scales from the deployment risk and resilience inventory in a sample of operation Iraqi Freedom veterans. Assessment 15, 391–403. ( 10.1177/1073191108316030) [DOI] [PubMed] [Google Scholar]
- 37.Steenkamp MM, Litz BT. 2012. Psychotherapy for military-related posttraumatic stress disorder: review of the evidence. Clin. Psychol. Rev. 33, 45–53. ( 10.1016/j.cpr.2012.10.002) [DOI] [PubMed] [Google Scholar]
- 38.Prigerson HG. 2009. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 6, e1000121 ( 10.1371/journal.pmed.1000121) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. 2009. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol. Rev. 29, 695–706. ( 10.1016/j.cpr.2009.07.003) [DOI] [PubMed] [Google Scholar]
- 40.Nash WP, Silva C, Litz B. 2009. The historic origins of military and veteran mental health stigma and the stress injury model as a means to reduce it. Psychiatr. Ann. 39, 789–794. ( 10.3928/00485713-20090728-05) [DOI] [Google Scholar]