Abstract
Theoretical approaches traditionally applied in mental health and criminal justice interventions fail to address the historical and structural context that partially explains health disparities. Community Wise was developed to address this gap. It is a 12 week group intervention informed by Critical Consciousness Theory and designed to prevent substance abuse, related health risk behaviors, psychological distress, and reoffending among individuals with a history of incarceration and substance abuse. This paper reports findings from the first implementation and pilot evaluation of Community Wise in two community-based organizations. This pre-posttest evaluation pilot-tested Community Wise and used findings to improve the intervention. Twenty-six participants completed a phone and clinical screening, baseline, 6- and 12-week follow-ups, and a focus group at the end of the intervention. Measures assessed participants’ demographic information, psychological distress, substance use, criminal offending, HIV risk behaviors, community cohesion, community support, civic engagement, critical consciousness, ethnic identification, group cohesion, client satisfaction, and acquired treatment skills. Research methods were found to be feasible and useful in assessing the intervention. Results indicated that while Community Wise is a promising intervention, several changes need to be made in order to enhance the intervention. Community Wise is a new approach where oppressed individuals join in critical dialogue, tap into existing community resources, and devise, implement and evaluate their own community solutions to structural barriers.
Keywords: substance abuse, mental health, health disparities, community based participatory research, health intervention, critical consciousness theory
1. Introduction
During the past several decades, scientific advancements in biomedical research have improved public health (National Institute on Drug Abuse, 2007). However, despite these advancements and overall improvement in the health of Americans in previous years, numerous reports and studies have clearly demonstrated that racial and ethnic disparities exist in healthcare access, delivery and outcomes in the U.S. (Braveman et al., 2011; LaVeist, Pollack, Fesahazion, & Gaskin, 2011; Smedley, Stith, & Nelson, 2002; U.S. Department of Health and Human Services & Services, 2010). According to Healthy People 2020, health disparities are differences in health closely associated with social, economic, and/or environmental disadvantage. Moreover, health disparities negatively affect groups of people who “have systematically experienced greater obstacles to health based on their racial or ethnic group or for a number of other characteristics historically linked to discrimination or exclusion” (U.S. Department of Health and Human Services & Services, 2000).
Racial minorities and members of low socio-economic status (SES) groups tend to face a multitude of health disparities, including shorter life expectancy and higher rates of diabetes, cancer, heart disease, stroke and substance abuse (Centers for Disease Control, 2011; U.S. Department of Health and Human Services & Services, 2010). Moreover, some studies have found that differential exposure to stress and social adversity in the forms of racial/ethnic bias, discrimination and unfair treatment experienced by non-White and/or low SES groups is associated with a variety of health conditions, risk behaviors, and negative outcomes, including, for example, poor mental health (Williams, Neighbors, & Jackson, 2003), and problematic substance and tobacco use (Chae et al., 2008; Gee, Delva, & Takeuchi, 2007; Martin, Tuch, & Roman, 2003; Mulia, Ye, Zemore, & Greenfield, 2008). Thus, chronic stress exposure and risky coping responses may be a potential mechanism in the creation and perpetuation of health disparities.
Disparities related to race and SES are especially obvious when examining the consequences linked to drug use and addiction which include altered judgment and engagement in impulsive and/or unsafe behaviors (e.g., risky sex). Despite relatively uniform rates of abuse across race/ethnic groups (Substance Abuse and Mental Health Services Administration, 2011), African Americans followed by Hispanics suffer harsher consequences (e.g., higher rates of HIV/HCV and incarceration) for drug use than other groups (National Institute on Drug Abuse, 2005, 2012). For instance, in 2009, African Americans comprised 14% of the U.S. population but accounted for 44% of all new HIV infections (Centers for Disease Control, 2011).
Racial disparities in incarceration rates resulting from differential treatment of Whites and non-Whites by the criminal justice system also have a lasting impact on health functioning (Moore & Elkavich, 2008). Prison inmates are exposed to unhealthy conditions and suffer from high rates of mental illness, substance use, and infectious diseases (Moore & Elkavich, 2008). Because poor non-Whites are more likely than their counterparts to be exposed to the penal system and its negative effects – including deviant social peers, reduced labor market opportunities, and high levels of infectious diseases – the penal system contributes to racial health disparities (Centers for Disease Control, 2011; Hallfors, Iritani, Miller, & Bauer, 2007; Rubin, Colen, & Link, 2010; Windsor & Negi, 2009). Once released, previously incarcerated individuals with special needs (e.g., housing, employment, mental health and substance use treatment) return to marginalized, low-income, predominantly non-White communities that have many social and economic barriers (e.g., high rates of crime, poverty and unemployment) and limited or overwhelmed social resources (Blitz, Wolff, Pan, & Pogorzelski, 2005; Braveman et al., 2011; LaVeist et al., 2011; LaVeist, 2005). This formula of returning previously incarcerated individuals with complex needs to communities with inadequate supports harms the individual and the community, and perpetuates the cycle of racial disparities in incarceration and health disparities for non-White and/or low SES populations (Caetano, 2003; Windsor & Dunlap, 2010).
Negative health effects (HIV, cancer, diabetes) and social consequences (incarceration, violence, school dropouts) disproportionately experienced by drug using racial/ethnic minorities may be exacerbated by prevention and treatment challenges. Researchers have reported difficulties with recruitment, engagement, and retention of minority populations in substance use research and treatment (Robinson & Trochim, 2007; Sheikh, 2006). Also, as suggested by the literature, racial minority populations may experience barriers to substance abuse intervention access and engagement (LaVeist, 2005; New Jersey Department of Health and Human Services, 2007; Schmidt, Greenfield, & Mulia, 2006). These barriers include lack of trust of clinical research initiatives (McKay et al., 2007); cost of treatment; fear and shame; belief they can recover without help; lack of knowledge about available services, as well as structural environmental stressors, such as lack of transportation or child care (Caetano & Clark, 2003; Esser-Stuart & Lyons, 2002; Fuller et al., 2004; Longshore, 1999).
These treatment difficulties are reflected in the treatment statistics. Although similar percentages of Blacks, Hispanics, and Whites use substances, 59.8% of White users were admitted to publicly funded substance abuse treatment programs in 2008, whereas only 20.9% of African Americans and 13.7% of Latinos or persons of Hispanic origin were admitted (National Institute on Drug Abuse, 2011). Similar to the drug use statistics across race, the Surgeon General’s report on Mental Health: Culture, Race, and Ethnicity (U.S. Department of Health and Human Services & Services, 2001) highlighted the finding that non-White populations experience mental disorders at a rate that is similar to or higher than their White counterparts; yet, research suggests that racial minorities have low rates of service utilization. The report notes that a collection of barriers impede service utilization, such as a lack of availability of services, mistrust and fear of treatment, and language barriers (U.S. Department of Health and Human Services & Services, 2001). The Surgeon General also concluded that a high proportion of non-Whites have unmet mental health needs due to racial/ethnic discrimination. As a result, the Surgeon General noted that when targeting minorities the research and practice communities should create and use culturally congruent interventions by incorporating historical, political, and cultural factors.
The interaction between disparities in drug abuse and its consequences, the associated stigma (National Institute on Drug Abuse, 2003) and prevention and treatment challenges creates a precarious situation that has led the Department of Health and Human Services and the National Institute on Drug Abuse to seek innovative ways to eliminate health disparities in the U.S. (National Institute on Drug Abuse, 2008). This paper addresses the need for culturally congruent interventions designed to address the historical and structural context that partially explains health disparities experienced by individuals with a history of substance abuse and incarceration residing in low-income and predominantly African American communities, by presenting the data from a pilot evaluation of Community Wise. An important method used to ensure cultural congruency was the application of Community Based Participatory Research (CBPR). CBPR is an approach that encourages researchers to involve the community in all phases of the research process, from question development to dissemination of results (Israel et al., 1998; Pinto, Spector, & Valera, 2011). As an approach, CBPR incorporates experiential and scientific knowledge by having researchers collaborate with community partners (Pinto, Spector, et al., 2011). Through the community partners that represent the voice of the community, researchers are afforded access to information that can improve the applicability of the study for the target population (Pinto, Spector, et al., 2011). CBPR provided the guiding principles that informed the development, implementation and evaluation of Community Wise, a new health intervention developed by a team of researchers, consumers, and service providers to improve substance use and related health among individuals with a history of incarceration and substance abuse residing in distressed communities (Windsor, 2013).
1.1 Community Wise
In 2010, the Newark Community Collaborative Board (NCCB) was created to apply CBPR principles in the development of Community Wise: a manualized, culturally-tailored, 12-week group intervention informed by Critical Consciousness Theory and designed to prevent substance abuse, related health risk behaviors, psychological distress, and reoffending among individuals transitioning from incarceration into a low-income and predominantly African American community struggling with violence, high HIV/HCV incidence, substance abuse, and poverty (Windsor, 2013). The use of CBPR methods allowed the Community Wise intervention to incorporate an understanding of the particular needs, worldviews, strengths, and challenges of the population such that the intervention is meaningful to the participants, which should improve recruitment, engagement and retention (Israel et al., 1998; “Liberia,” 2008; Pinto, Campbell, Hien, Yu, & Gorroochurn, 2011). Community Wise aims to empower participants to combat structural and internalized oppression by developing critical analysis skills and implementing social change projects. Specifically, the historical context and structural barriers impacting individuals with histories of substance abuse and incarceration residing in distressed communities are discussed in group meetings and in homework assigned for participants to complete every week. Critical thinking skills are used to assist participants in achieving a deeper level of analysis regarding how the historical context and structural barriers impact individual behaviors. Individual goals setting, community engagement, and social change projects are then used to address internalized and structural oppression.
1.2 Theoretical Framework
Theoretical approaches traditionally applied in mental health, substance abuse, HIV/HCV and criminal justice interventions (e.g. cognitive behavioral therapy, pharmacotherapy, incarceration) fail to address the historical and structural contexts that partially explain health disparities experienced in low-income and predominantly African-American communities. Community Wise is grounded in Paulo Freire’s critical consciousness theory, which has been used worldwide in conjunction with a myriad of social and medical interventions aimed at empowering distressed populations to become agents of change in their own lives (Freire, 2000). Critical consciousness theory argues that oppressed groups, such as individuals residing in predominantly low-income and African-American neighborhoods with a history of substance abuse and incarceration, are disempowered and dehumanized within society through objectification and silencing. Yet these individuals carry within themselves a great deal of knowledge and skills. By drawing from these strengths and joining other oppressed individuals in dialogue, critical consciousness is developed and entire groups of people become empowered to create individual and community change (Freire, 2000; Mullaly, 2002).
Critical consciousness was defined by Freire (2000) as the ability to “perceive social, political, and economic contradictions, and to take action against the oppressive elements of reality” (p. 19). Community Wise was inspired by the application of critical consciousness theory in the structural social work literature (Mullaly, 2002; Sakamoto & Pitner, 2005). Structural social work argues that traditional social work unwittingly acts as a tool in the enforcement of the status quo. Thus, instead of fostering critical consciousness to create innovative structural solutions to social problems, traditional social work merely assists oppressed individuals in conforming with mainstream acceptable behaviors (Mullaly, 2002). Structural social workers call for critical consciousness-raising, which seeks to help clients understand how and in what ways they have internalized oppression and been impacted by structural oppression. Oppression, in its many forms and manifestations (e.g., racism, discrimination), has been identified as a chronic stressor that can greatly compromise psychological and physical health wellbeing (Brown-Reid & Harrell, 2002; Clark, Anderson, Clark, & Williams, 1999; Jackson et al., 1996) contributing to psychological distress, crime, substance use, and related health risk behaviors (Boyd-Franklin, 1993; Franklin, Boyd-Franklin, & Kelly, 2006; Franklin, 2004). These unique experiences with oppression-related stress and its consequences impact the growing disparity in health. Moreover, the societal and institutional racism that exists within the medical field, leading to the consistent inferior treatment of people of color, also contributes to health disparities (Allen, 1996). The goal of critical consciousness development is to draw from clients’ experiences to build critical consciousness through a dialogue and empowerment process (Mullaly, 2002; Sakamoto & Pitner, 2005). The link between critical consciousness and oppression is the perspective that oppression exists and is perpetuated within a culture with limited capacity for analysis and action (Wallerstein & Sanchez-Merki, 1994; Watts, Griffith, & Abdul-Adil, 1999). As people gain awareness of internal and external oppressive conditions and then collaborate to address oppression, the collaborative efforts increase the community’s capacity to overcome oppression. Consequently, critical consciousness has been identified as an antidote to oppression (e.g., racism, classism, sexism), its consequences (e.g., health disparities, crime), as well as a key ingredient in the fight for social justice (Diemer & Blustein, 2006; Watts, Diemer, & Voight, 2011; Watts et al., 1999). Community Wise was designed to foster critical consciousness in addressing health disparities. A detailed discussion of the theoretical framework, manual development, and description of Community Wise can be found in Windsor, Pinto, Benoit, Jessell, & Jemal (2013 - under review).
2. Methods
The current pilot evaluation applied Community Based Participatory Research (CBPR) principles to test the feasibility of delivering Community Wise at two community-based agencies and to further develop the manual. Following the model developed by Pinto (2009), the NCCB was developed to create and pilot test Community Wise. The NCCB is composed of fifteen consumers, community residents, service providers, and researchers who oversee the program and rotate collaborating and participating in all stages of the research process (Windsor, 2013). The NCCB was also responsible for ensuring that the protocol approved by the Rutgers Institutional Review Board was being followed accordingly.
2.1. Staff and NCCB Training and Monitoring
The NCCB hired four students (1 undergraduate and 3 graduate students) to manage the research and three licensed social workers to facilitate the Community Wise groups. Clinicians and research support staff were directly supervised by the project’s Principal Investigator (PI). All students became members of the NCCB. The project’s staff received training on measurement, data collection, and the manual by the PI and one consultant. Members of the NCCB received specific research training on the research areas they participated in. For instance, those involved in data collection received training on interviewing procedures while those involved in writing/presenting received training on dissemination. All NCCB members received training on research ethics, grant writing, and CBPR. The NCCB met monthly to review and approve the research procedures, resolve any challenges, and make decisions on how to proceed.
Intervention
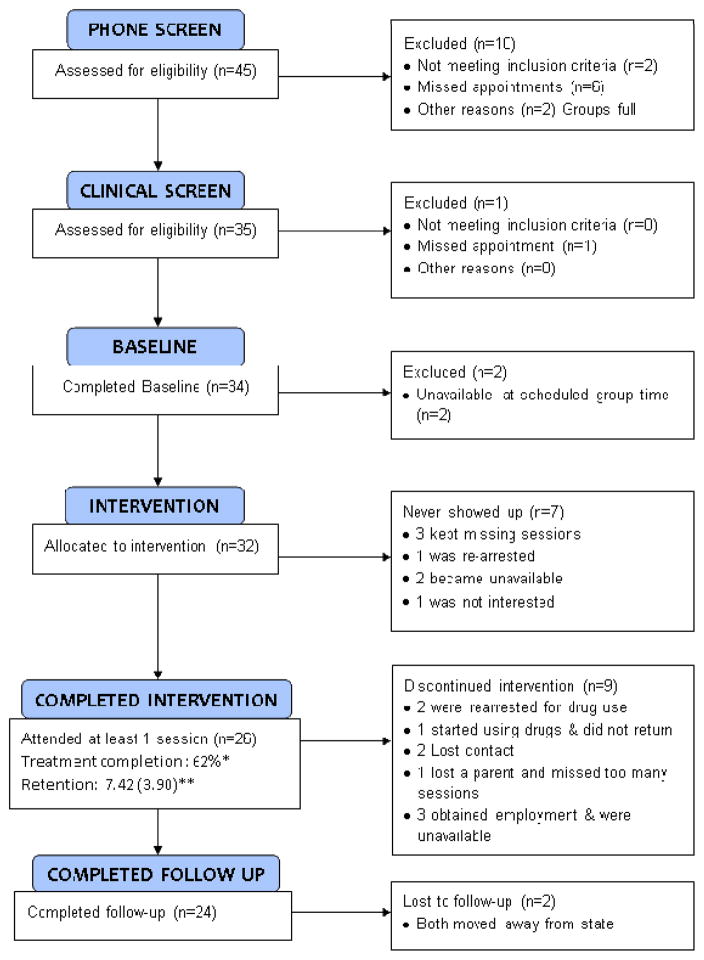
Community Wise is a 12-week, community-based group intervention designed to empower formerly incarcerated individuals to join others in building a safer and healthier community. Community Wise draws on individual- and community-level strengths (e.g. community-based organizations, individual experience) as the basis for addressing oppression, a root cause of problems that concern Community Wise. Community Wise was developed to mobilize formerly incarcerated people to recreate their communities through individual and collective actions that seek to reduce psychological distress, substance abuse, related health risk behaviors, and criminal offending, through critical consciousness raising and community engagement. The Community Wise process of change is shown in Figure 1.
Figure 1.
Community Wise model
The active ingredients of Community Wise include critical dialogue, personal goal development, and social change projects. The dialogue takes place during phase I and it consists of participants’ reactions to illustrations depicting the oppression that individuals with a history of substance abuse and incarceration face in the United States. During phase II, social change projects and personal goals are developed, implemented, and continuously evaluated. Social change projects are strategies that participants develop and implement to address challenges they identify in their community. They may include writing letters to elected officials, participating in fund raising events, and volunteering to clean a park, among other civic activities.
2.2. Recruitment
Snowball and purposive sampling (Rubin & Babbie, 2001) were used to recruit participants from the community. Specifically, flyers were distributed to community-based agencies and NCCB members reached out to potential participants. Participants who were interested called the study’s phone number and completed a pre-screen which included the following: Participant’s name, contact information, age (above 18), date of release (after January 2008), and whether they had a history of substance use. Those who met the phone screen eligibility criteria were invited to complete an in-person clinical screen. Participants received $10 to complete the 30 minute clinical assessment. Those who met eligibility criteria were invited to participate in the study and signed a written consent form. A certificate of confidentiality was obtained from the federal government to prohibit court-ordered violations of participant confidentiality.
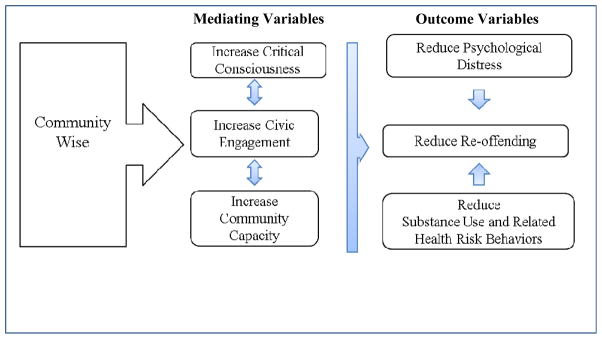
A total of 26 individuals attended at least one session of the intervention and were included in the analysis. Inclusion criteria were: residence in Essex County; having been released in the past 4 years; being over 18 year of age; having a lifetime history of substance abuse; agreeing to be video/voice recorded during the intervention; being able to give informed consent to participate; and speaking English. Exclusion criteria were: gross cognitive impairment; severe unstabilized mental illness such as psychotic disorders; and suicidality. Eligibility was established by an in-person interview with a trained master or doctoral level social worker using the Mini Mental State Exam (Folstein, Folstein, McHugh, & Fanjiang, 2001), MINI International Neuropsychiatric Interview 6, psychoticism and suicidality modules (Sheehan et al., 1998) and a question about whether the person experienced a substance abuse problem in the past. Figure 2 displays the participant recruitment process.
Figure 2.
CONSORT 2010 Flow Diagram. Treatment completion (*) indicates consistent session attendance, clinical improvement (determined by consensus at clinical supervision), and engagement in social change project. Retention (**) is defined as the average number of sessions attended (mean and standard deviation).
2.3. Design and Measures
Mixed methods were used to pilot test Community Wise. For the quantitative evaluation, participants completed questionnaires on laptop computers using Questionnaire Development System (QDS) software technology (Pluhar et al., 2007). Groups of up to five clients were scheduled to come into the laboratory and complete the questionnaire. A research assistant taught participants how to use the computer, answer questions as needed, and monitored the data collection process. Assessments are described below:
Baseline (up to 1.5 hours)
Ethnic identity was measured by the Consideration of Ethnic Culture in Therapy Scale (CECTS) (Donohue et al., 2006) and the Scale of Ethnic Experiences (SEE) (Malcarne, Chavira, Liu, & Fernandez, 2006). Critical Consciousness was measured by a 12 item scale developed and pilot tested by the NCCB with 47 individuals including substance abuse providers, consumers, and community residents (Jessell, Jemal, Blom, & Windsor, 2012). The scale has face validity, however, construct validity is yet to be tested (e.g. items: “Feelings of worthlessness impact how people in my community deal with health-related issues”, “I attend meetings where we discuss issues about my community”- α=.82,). Reoffending was measured by the Criminal History Risk Assessment (Simpson, 2008), the Buss-Perry Aggression Scale (BPAS) (Diamond & Magaletta, 2006), and a question developed by the NCCB: “Since you were released into the community have you engaged in any of the activities below” (e.g.: violent, sexual, property, drug related offences). Health related risk behaviors were measured with the Risk Assessment Battery (RAB) (Metzger, Navaline, & Woody, 2001) and the Risk Behavior Assessment (RBA) (National Insitute on Drug Abuse, 1993). Substance use was measured by the Timeline Follow Back (TLFB) (Sobell & Sobell, 1992), the Short Inventory of Problems – Alcohol and Drugs (SIP-AD) (Blanchard, Morgenstern, Morgan, Labouvie, & Bux, 2003), and hair and saliva drug screens. Mental health symptoms were measured by the Brief Symptom Inventory (BSI) (Derogatis, 1993) and the Post-Traumatic Stress Questionnaire (PTSQ) (Leahy & Holland, 2000). Social support, community cohesion, and civic engagement were measured by the Community Assessment Inventory (CAI) (Brown, O’Grady, Battjes, & Katz, 2004), and the Parker Scale (Goodman et al., 1998). Participants received $15 to complete the baseline.
Follow-up 1 (mid-treatment assessment collected 6 weeks post baseline, up to 20 minutes)
Included selected questions from the mental health, community cohesion, civic engagement, and critical consciousness measures to test its feasibility in being used as part of weekly assessments in a future evaluation. Group process measures included the Working Alliance Inventory (WAI) (Horvath & Greenberg, 1989), the Group Climate Questionnaire (GCQ) (MacKenzie, 1983), the Cohesiveness subscale of the Therapeutic Factors Inventory (TFI) (Lese & MacNair-Semands, 2000), and the Yalom Curative Factors (Yalom, 1995). Moreover, the NCCB developed questions about participants’ use of learned skills (e.g. “I try to reach out and connect with a social network that is supportive to me”). Participants received $10 to complete the mid treatment assessment.
Follow-up 2 (12 weeks post baseline, up to 1.5 hour)
Included baseline measures; monthly assessment measures, and the Treatment Services Review (TSR) (McLellan, Alterman, Cacciola, Metzger, & O’Brien, 1992) in order to assess what other treatments participants received while attending Community Wise group meetings. Participants received $15 to complete the follow-up.
The qualitative evaluation included three focus groups at the end of the intervention, weekly clinical supervisions, and review of group session videos. Focus groups were conducted by a doctoral level NCCB member and one of the research assistants. The purpose of the focus group was to obtain feedback about the intervention from clients. Everyone who attended at least one Community Wise session was invited to participate. Participants received $15 to provide their feedback.
Clinical supervisions were attended by the project PI and all group facilitators on a weekly basis. During supervision the PI provided facilitators with feedback from the sessions’ videos, discussed what was working and what was not working, addressed challenges with non-responsive clients, and ensured the manual was being followed and implemented accurately. The PI and two NCCB members watched all session videos and independently rated the implementation of the manual using a treatment fidelity scale developed by the NCCB for Community Wise. This scale included items such as “Group facilitator posed critical questions that allowed participants to reach the take home message”; “Group facilitator allowed sufficient time to process social change projects” that were rated in a scale from 1 (Not at all) to 5 (Definitely).
2.4 Analysis
Quantitative analyses was descriptive in nature, and thus, it examined pre/post-intervention percentages and mean increases in critical consciousness and decreases in substance use, related health risk behaviors, psychological distress, and reoffending. Preliminary analyses included examining missing data, dropout rates, distributional properties of measures, and correlations among outcome measures. Moreover, baseline demographic characteristics and outcomes were compared between: those who never attended a Community Wise session and those who attended at least one session; intervention groups; and, males and females.
Data analysis was then conducted to answer the primary outcome questions across the groups and for the entire sample. Only the intention to treat group with complete 12 weeks follow-up data was included in the analysis (N=24). As a measure of the magnitude of change in substance use, related health risk behavior, and reoffending outcomes, standardized indices of effect size (Cohen’s d) were calculated for the pre-intervention (baseline) and post-intervention (week 12) assessments. Simple paired sample t-tests were also conducted to examine mean differences between pre-and posttest data.
All focus group sessions were transcribed into Word files. The transcripts were coded and analyzed manually by one of the authors. Both processes were guided by the aims of the study. The thematic analysis (Braun & Clarke, 2006) was influenced by phenomenology and grounded theory, which allow conceptual frameworks to emerge from lived experiences related in participants’ own language (Charmaz, 2006). The process involves reading the focus group transcripts several times, coding and recoding through a process of constant comparison until themes and categories become clear. The focus groups complemented quantitative measures of participant feedback. Such triangulation helps to ensure completeness of data and can reveal convergence or dissonance in key themes developed in our analyses (Farmer, Robinson, Elliott, & Eyles, 2006).
3. Results
3.1. Participants
The study sample included 26 individuals who attended at least one Community Wise session. Table 1 displays the sample characteristics at baseline. Most participants were African American, unemployed, and reported annual incomes below $10,000. The majority were on parole, probation, or in drug court. They were arrested for a variety of crimes including violent, property, and drug crimes. Most participants reported that they were currently smoking cigarettes but had stopped illicit drug and alcohol use prior to enrolling in Community Wise. The majority reported being HIV negative and 4 out of 9 reported using a condom less than half the time when having sex.
Table 1.
Participants’ Characteristics at Baseline (N=26)
| Characteristic | N (%) or Mean (SD) |
|---|---|
| Male | 16 (62%) |
| Heterosexual | 23 (89%) |
| Age | 47.07 (9.59) |
| Race | |
| Black/African American | 22 (85%) |
| White | 3 (11%) |
| Native American | 1 (4%) |
| Hispanic | 2 (8%) |
| Income less than $10K/year | 21 (84%) |
| At least high school education | 25 (81%) |
| Marital Status | |
| Single/never married | 19 (73%) |
| Unemployed | 23 (89%) |
| Has a Driver’s License | 26 (12%) |
| Arrest History | |
| Probation or parolea | |
| Parole | 13 (50%) |
| Probation | 3 (12%) |
| Drug court | 5 (19%) |
| No supervision | 5 (19%) |
| Average number of years since release | 1.6 (1.38) |
| Offense Type | |
| Violent crime (assault, homicide, carjacking, robbery) | 21% |
| Property crime (burglary, fraud, shoplifting) | 21% |
| Possession | 8% |
| Drug dealing | 34% |
| Prostitution | 16% |
| Substance abuse | |
| Any alcohol use past 30 days | 6 (23.1%) |
| Number of drinking days (past 90-days) | 8.11 days (21.59) |
| Drinks/drinking day (past 90-days) | 1.8 (5.37) |
| Smoking ever | 24 (92.3%) |
| Daily Smoking | 16 (66.7%) |
| Reported illicit drug use past 30 days | 4 (15%) |
| Number of days any illicit drug use past 30 days (crack/cocaine, heroin, marijuana) | 4.42 (13.89) |
| Testing positive for drug use | 3 (13%) |
| Substance use related health risk | % (n) or mean (SD) |
| HIV + | 3 (11%) |
| Engaged in sex for drugs | 6 (23%) |
| Average number of times tested for HIV | 5.7 (2.53) |
| Had oral/vaginal sex in past 30 days | 9 (35%) |
| Used a condom less than half the times when having sex | 4 (44%) |
| IDU Risk Behaviors | 0b |
| Psychological Distress | |
| PTSD (responding yes to having had a near death experience) | 13 (50%) |
| PTSQ (PTSD Symptom Severity) | .82 (.92)c |
| Obsession-Compulsion | .72 (.76)d |
| Somatization | .61 (.55)d |
| Interpersonal Sensitivity | .61 (.77)d |
| Depression | .70 (.83)d |
| Anxiety | .57 (.66)d |
| Hostility | .44 (.49)d |
| Phobic Anxiety | .36 (.71)d |
| Paranoid Ideation | .63 (.60)d |
| BSI 18 Total Score | .62 (.61)d |
| Substance use problems | 4.07 (6.88) |
| Reoffending | |
| Buss Perry Aggression | 2.25 (1.26)e |
| Critical Consciousness | 54.33 (6.37) |
Men less likely to be on parole and more likely to be in drug court compared to women, 2 =10.25, p < .05)
No one in the sample reported using drugs intravenously
Ranges from 0 to 3 (higher scores mean higher PTSD symptom severity)
Ranges from 0 to 4 (higher scores mean higher psychological distress)
Ranges from 1 to 7 (higher scores mean higher aggression)
Results from the psychological distress measures showed a high number of participants reporting that they have had near-death experiences; however, symptom severity scores were not high. Unexpected low levels of depression, anxiety, hostility, substance abuse problems, and aggression were found in this sample. This was likely due to the broad inclusion criteria regarding substance use (lifetime use as opposed to recent or current use) and the high level of participants’ involvement in other interventions such as medication, Drug Court, and outpatient substance abuse. Accordingly, our sample grossly violated assumptions of normality on main outcomes, with very few individuals reporting substance use, criminal behavior, or psychological distress. Transforming skewed outcome variables did little to improve normality. Thus, we violated assumptions of normality in the data analysis. Results of outcome analysis must be interpreted with caution.
3.2. Baseline Group Comparisons
Of those who completed the baseline, 9 (26%) did not attend any treatment sessions. There were no differences on demographic characteristics (race, gender, education, income, and employment) or substance use behavior between those who attended at least one Community Wise session versus those who did not attend. Those who attended at least one session had higher BPAS Hostility scores (M = 9.52) than those who did not attend any session (M = 3.78), F(1,32) = 8.26.
Participants were divided into three Community Wise groups after completing baseline according to their gender and availability. Two groups were gender specific: Group 1 with seven men and Group 3 with eight women. Group 2 was mixed with two women and nine men. Groups differed on number of lifetime arrests, F(2, 24) = 4.65, p < .05, with Group 1 having the greatest mean number of arrests (n = 3) relative to Groups 2 and 3 (n = 2 each). Groups were equivalent on all other demographic, substance use, and baseline factors (see table 3).
Table 3.
Changes on psychological distress, substance use, related health risk behaviors, and reoffending
| Variable | Baseline Mean (SD) |
12 Weeks Follow-up | Effect Size Cohen’s d |
|---|---|---|---|
| Psychological Distress (BSI-18) | |||
| Group 1 | .28 (.29) | .47 (.74) | −.37 |
| Group 2 | .78 (.79) | .79 (.62) | .01 |
| Group 3 | .86 (.48) | .62 (.56) | .46 |
| Combined | .66 (.63) | .64 (.63) | .03 |
| PTSD Symptom Severity (PTSQ) | |||
| Group 1 | .20 (.29) | 0 (0) | 1.38 |
| Group 2 | .46 (.86) | .12 (.37) | .55 |
| Group 3 | .74 (1.08) | 0(0)* | 1.37 |
| Combined | .48 (.82) | .05 (.24)** | .81 |
| Reoffending: BPAS | |||
| Group 1 | 18.14 (7.29) | 15.0 (6.22) | .46 |
| Group 2 | 32.7 (20.90) | 27.6 (18.25)* | .26 |
| Group 3 | 29.14 (9.01) | 29.14 (24.04) | 0 |
| Combined | 27.41(15.66) | 24.37 (18.15) | .30 |
| Criminal reoffending questions | .06 (.23) | .06 (.23) | 0 |
| Substance Use | |||
| # days using drugs (past 3 months) | 42.5 (34.64) | 4 (1.4) | 2.13 |
| Average # of drinks per drinking day | 8.99 (9.99) | 3.2 (2.16) | .95 |
| Positive Drug Test | 1.09 (.30) | 1.24 (.44)* | −.40 |
| Short Inventory of Problems- Drugs and Alcohol | 6.4 (8.8) | 4 (6.16) | .32 |
| Substance Use Related Health Risk | |||
| RAB (risky sex) | |||
| Group 1 | 1 (1.70) | 0 | 1.18 |
| Group 2 | 0.33 (.70) | 1.11 (2.26) | −.53 |
| Group 3 | 0.57 (1.51) | 0.57 (0.97) | 0 |
| Combined | 0.58 (1.28) | 0.58 (1.50) | 0 |
Note. Many outcome measures were very skewed (see large standard deviations), thus analysis violated assumption of normality and these results should be interpreted with caution.
p < .05
p < .01
Women had the poorest scores on outcome measures at baseline when compared to men. Specifically, women scored significantly higher on PTSD symptom severity (22.80(13.64) versus 5.87 (6.17), p < .01), BSI Anxiety (.96(.86) versus .36(.43), p < .05), and BPAS Physical Aggression (3.17(1.90) versus 1.56(.77), p < .05). There were no significant differences on other demographic or outcome measures.
3.3. Outcome Measures
Outcome measures included changes in critical consciousness, civic engagement, community capacity, psychological distress, reoffending, substance use, and related health risk behaviors (See Figure 1). No significant differences were found in civic engagement and community capacity between baseline and follow-up among all participants. Critical consciousness increased significantly for the women’s group from baseline to 12 weeks follow-up, and decreased significantly for the mixed gender group from baseline to 6 weeks follow-up. In the overall sample, no significant differences in critical consciousness were found between baseline and 12 weeks follow-up. The women’s group significantly increased their belief that if needed, their neighbors would intervene on their behalf at 12 weeks follow-up. Overall, participants significantly increased their perceptions of ethnic/cultural importance and problems indicating that at 12 weeks follow-up, participants increased their belief that culture and ethnicity are important and that there are problems associated with their ethnic/cultural group. Table 2 displays changes in critical consciousness, ethnic/cultural importance and problems, and social support at one and 12 weeks follow-up.
Table 2.
Changes on Critical Consciousness, social support, ethnic/cultural problems/importance
| Variable | Baseline Mean (SD) |
6 Weeks Follow-up Mean (SD) |
12 Weeks Follow-up Mean (SD) |
Effect Size Cohen’s d |
|---|---|---|---|---|
| Critical Consciousness | ||||
| Group 1 | 49.40 (5.81) | 51.60 (7.76) | 53.43 (7.60) | .60 |
| Group 2 | 58.57 (5.56) | 55.28 (4.61)* | 52.67 (8.91) | −.81 |
| Group 3 | 53.50 (4.84) | 57.83 (5.78)** | 55.57 (3.26) | .51 |
| Combined | 54.33 (6.37) | 55.11 (6.14) | 53.83 (6.86) | .07 |
| Ethnic/cultural problems (CECTS) | N/A | |||
| Group 1 | 8.28 (3.09) | 9.57 (3.64) | .38 | |
| Group 2 | 8.33 (3.40) | 10.89 (1.96)* | .95 | |
| Group 3 | 9.71 (3.25) | 11.00 (2.31)* | .46 | |
| Combined | 8.54 (3.25) | 10.50 (2.57)** | .67 | |
| Ethnic/cultural importance (CECTS) | N/A | |||
| Group 1 | 20.85 (3.67) | 21.43 (3.20) | .16 | |
| Group 2 | 21.37 (3.42) | 24.25 (2.18)** | 1.03 | |
| Group 3 | 22.28 (3.30) | 22.43 (4.07) | .04 | |
| Combined | 21.30 (3.40) | 22.74 (3.21)* | .4 | |
| Social support (CAI) | N/A | |||
| Group 1 | 67 (5.48) | 54.14 (5.49) | −2.34 | |
| Group 2 | 64.4 (5.64) | 66.4 (4.68) | .28 | |
| Group 3 | 65.57 (6.13) | 66.28 (7.63) | .13 | |
| Combined | 65.50 (5.59) | 65.71 (5.62) | .03 | |
| Neighborhood Control (Parker) | N/A | |||
| Group 1 | 17.14 (3.89) | 17.71 (3.59) | .15 | |
| Group 2 | 15.6 (5.84) | 16.8 (4.21) | .23 | |
| Group 3 | 16 (4.51) | 17.7 (3.10) | 1.13 | |
| Combined | 16.17 (4.8) | 17.33 (3.61) | .27 | |
| Neighborhood Participation (Parker) | N/A | |||
| Group 1 | 11.85 (3.89) | 12 (.00) | .08 | |
| Group 2 | 10.5 (4.45) | 11.4 (4.22) | .20 | |
| Group 3 | 13.28 (2.75) | 14.86 (2.11) | .65 | |
| Combined | 11.71 (3.88) | 12.58 (3.23) | .24 | |
| Neighbors Intervening (Parker) | N/A | |||
| Group 1 | 13 (3) | 13.86 (4.81) | .22 | |
| Group 2 | 12.2 (4.49) | 12.7 (5.77) | .09 | |
| Group 3 | 12.28 (2.93) | 14.57 (2.93)* | .78 | |
| Combined | 12.46 (3.55) | 13.58 (4.69) | .27 | |
p < .05
p < .01
Sample distribution on psychological distress, reoffending, substance use, and related health risk behaviors were very skewed and therefore they should only be interpreted descriptively. Overall, psychological distress, PTSD symptom severity, and substance use means were reduced at 12 weeks follow-up. The proxy measure for reoffending was also reduced, while the questions about criminal offending developed by the NCCB and the measure of sexual risky behaviors remained the same. We were unable to assess Community Wise’s impact on intravenous drug use (IDU) risk behaviors as there were no IDUs in the sample. Table 3 displays comparisons between baseline and 12 weeks follow-up.
3.4. Process Measures
Findings indicated high rates of successful treatment completion, retention, and follow-up. Participants who attended at least one Community Wise session completed an average of 8 out of 12 sessions. A total of 62% successfully completed the intervention. Successful treatment completion was established by engagement in social change projects (developing and implementing a project), attending at least 50% of the sessions, and showing clinical improvement as determined by group facilitator discussions (e.g. using critical thinking skills, engaging with family, showing improvement in mental health symptoms, etc…). Follow-up completion rate was 92% at the 3 months post baseline follow-up. Figure 2 displays details on the evaluation’s CONSORT flowchart. Of participants who attended at least one Community Wise session, 62% developed a social change project idea, but only half of them (31%) completed the project. Overall, 79% of participants reported that Community Wise was greatly helpful. Scores from the WAI scale indicated high levels of working alliance. Scores from the GCQ scale revealed a high level of engagement and low levels of conflict and avoidance in the groups. Scores from the TFI cohesiveness scale indicated a great deal of cohesion among groups. Table 4 displays results for process measures.
Table 4.
Process Measures
| Characteristic | % or Mean(SD) |
|---|---|
| 6 Weeks Follow-up Measure | |
| WAI Bond | 69.67 (14.19) |
| WAI Task | 66.39 (8.42) |
| WAI Goal | 66.89 (12.33) |
| WAI Total | 202.94 (32.57) |
| GCQ Engagement | 19.06 (7.14) |
| GCQ Conflict | 1.61 (2.14) |
| GCQ Avoidance | 7.89 (3.10) |
| TFI Cohesiveness | 52.71 (10.43) |
| 12 Weeks Follow-up Measures | |
| Social Change Project | |
| Did not develop a project | 38% |
| Engaged in project | 31% |
| Completed the project | 31% |
| End of Treatment Questionnaire | |
| How long did it take you to feel comfortable with CW? | 2.5 (2.45) weeks |
| How much will use learned skills (from 0 to 100%)? | 84 (18.72) |
| To what extend would you recommend CW (from 0 not recommending to 100% recommending)? | 84 (27.04) |
| How easy was it to understand CW? (from 0% = difficult to 100% = easy) | 76 (22.41) |
| Yalom, Altruism | 1.96 (.82) |
| Yalom, Instilling Hope | 2.32 (.67) |
| Yalom, Existential Factors | 1.99 (.82) |
| Use of treatment skills | 3.22 (.52) |
Qualitative analysis of video data and facilitator assessments of the Community Wise sessions revealed the spectrum of critical thinking skills as well as the progress participants made over the course of the intervention. Group 3, in particular, demonstrated significant improvement in critical thinking by reflecting on learned ways of thinking and unquestioned acceptance of ideas. However, for the most part, participants argued their beliefs rather than exploring the origins of their beliefs, evaluating the evidence and assumptions underlying their beliefs, or analyzing the consequences of subscribing to one belief versus another. Often, the discussions focused on whether a belief (e.g. the American Dream is attainable by all) is true or not true, and thus, conversations rarely reached a deeper level of critically analyzing the formation of that idea or the consequences of accepting a belief as an absolute truth. For example, when viewing the family illustration which depicted a white suburban, middle class “family” including a mother, father, two children and a dog in front of a nice house with a black maid and Latino gardener in the background, a participant stated, “That’s the right environment to raise kids.” A discussion demonstrating critical analysis would include questions pertaining to who is represented and who is excluded as well as who benefits from different interpretations of the image. Participants who improved critical thinking skills began to question their own assumptions and the assumptions of others. One participant demonstrated critical thinking by making connections between history, lessons learned and risky action. She stated, “Some of us think that we can’t do anything in life productive because of past history, so what we do, we turn to the risky behavior – as far as risky sex, shooting drugs, and [being] abusive with our family members because we think we can’t become better people and it stems from what we were taught and what was experienced in the past. It got a lot to do with society.” A facilitator noted, “One unique direction the session took was the exploration of how the women contribute to oppression themselves. It was nice to see them owning their own prejudices and talking about ways to change that. Women were talking about perspectives, changing their minds, and challenging their own assumptions.”
Focus groups with participants after treatment indicated that the intervention was perceived to be beneficial overall, but that key aspects of its implementation were not successful. Many participants credited Community Wise with making them aware of oppression, motivating them to set goals and enabling them to feel more optimistic about the future. They valued the opportunity to exchange ideas with and learn from others who had had life experiences similar to theirs, and they were enthusiastic about the idea of engaging in social change. Yet the participants were also more critical of the social change projects than of any other aspect of Community Wise. Several recalled frustration at trying to actually execute a project, most often citing inadequate time, because the social change project did not start until midway through the intervention. Participants also expressed mixed feelings toward the images used to prompt critical dialogue. Several described them as upsetting but ultimately helpful, but others suggested using photographs instead of the paintings that were used, particularly photos depicting evidence of oppression in Newark, which they argued would be more relevant to their experiences. Participants offered several constructive suggestions for improving Community Wise, including an earlier start to the social change projects, and either meeting more frequently than once a week or meeting for more than 12 weeks.
4. Discussion
Findings from this preliminary study showed that Community Wise was acceptable to individuals with a history of substance abuse and incarceration residing in a low income and predominantly African American community. Participants found the treatment useful and process measures revealed strong alliance and a high retention rate in the intervention. Overall, these results suggest that participants were able to engage in treatment and viewed treatment as beneficial, despite the multiple challenges they face (e.g. homelessness, unemployment, poverty).
Outcome measures indicated that Community Wise has the potential to be helpful as indicated by many favorable outcome changes in the expected direction. For instance, small to moderate positive effect sizes were found for the overall sample in all of the outcomes. However, most of these indicators failed to reach the statistical level of significance. Studies with larger sample sizes are needed to further test these relationships. Participants reported significant improvements in critical consciousness from baseline to 6 weeks follow-up and significant reduction on PTSD symptom severity from baseline to 12 weeks follow-up. While promising, outcome measures such as PTSD symptom severity were very skewed (as seen in the large standard deviations). Despite our attempt to transform these variables, we were unable to obtain normal distributions. The small sample size and broad inclusion criteria may have contributed to many important outcomes variables being skewed (e.g. substance abuse, psychological distress, health risk behaviors), making statistical analysis challenging.
Despite promising findings, data revealed several areas in which Community Wise needed improvement. Data from clinical supervision with therapists and video recordings of sessions indicated that the small overall change in psychological distress may be due to problems in the first version of the manual. Community Wise was designed to increase anger through group dialogue and channel this anger toward motivation to engage in community change action. However, the intervention placed too much emphasis on the dialogue about oppression and not enough support for participants to engage in social change. Consequently, we decided to change the order of the sessions. Instead of having phase I focus on critical dialogues and phase II focus on social change, we alternated the sessions so that the critical dialogue is intertwined with the social change projects. We also added a single session on empowerment to give participants a wide range of tools they can use to engage in their communities, develop a feasible social change project, and systematically implement and evaluate projects. We will encourage participants to start working on the social change projects in the first session as opposed to waiting for phase II to start. A partnership program will be developed to help connect participants with community residents who are willing to help them work on the social change projects.
We found that participants struggled with grasping the concept of critical thinking. The critical dialogues often felt more like a battle on whose belief was true and whose belief was false instead of a true critical analysis of the origins of these beliefs and their consequences on different groups of individuals. Thus, we added a critical thinking session where we gave participants and facilitators the tools to challenge each other’s thinking in such a way that does not elicit defensiveness. We also added qualitative empirical articles that describe the experiences of oppressed groups who struggle with drug addiction and the criminal justice system as tools to elicit critical dialogue and a way to keep participants engaged in Community Wise between weekly sessions.
Quantitative data clearly showed that the mixed gender group had the poorest outcomes when compared to gender specific groups. While the research design does not allow us to conclusively assess whether it was in fact the mixed gender that caused these differences, data from qualitative analysis indicated that discussions about gender specific issues were richer in the gender specific groups. Existing literature also supports the use of gender specific groups in psychotherapy (Ashley, Marsden, & Brady, 2003; Greenfield et al., 2007). Therefore, we will adapt the manual to be delivered to gender specific groups.
Findings from the pilot study showed QDS (Pluhar et al., 2007) was acceptable to participants and that it was useful in collecting high quality data. We were able to streamline the measures by selecting more specific subscales or short versions that reduce the time needed for data collection. While participants did not have any issues with saliva tests, hair tests were an issue. Most of our participants had short hair or hairstyles that made it impossible to collect head hair. We also found that self-report was more accurate than the saliva test. For instance, a couple of participants reported having used drugs that were not reflected in the saliva test. They had used in the past month and the saliva test only picks up use in the past 3 days (Dolan, Rouen, & Kimber, 2004). Thus, we decided to no longer use drug testing in the research. Qualitative data indicated that many participants seemed to be making lifestyle changes (e.g. trying to eat healthier foods and increasing their exercise). As a result, we will add a lifestyle scale in the next pilot to see if in fact this is another important outcome in Community Wise. Finally, we will restrict the inclusion criteria to individuals with a past year history of substance abuse in order to improve the normal distribution of our sample.
4.1 Limitations
While the current form of Community Wise appears promising in reducing psychological distress, substance use, related health risk behaviors, and reoffending among individuals with a history of substance abuse and incarceration, the findings of our pilot study have several limitations. Without a control group to show that any gains occurred at a significantly higher rate among those who received Community Wise, results remain tentative. The improvement in the outcomes may have been a function of time, engagement on other treatment services, or the natural course of the challenges this population faces. Additionally, it is difficult to interpret findings related to substance use, related health risk behaviors, psychological distress, and reoffending due to the violations of normality in the data. The small sample limits any generalizability of the findings to anyone outside our sample. Other considerations are that Community Wise was not delivered in the same way across different groups. The women’s group received an improved version of the manual (e.g. they received a session on critical thinking). Thus, we cannot know what caused the differences across groups. Finally, the Critical Consciousness Scale has not been systematically validated. We are currently developing a standardized measure of critical consciousness which will be used in future studies to replicate these findings and further examine this important concept.
5. Conclusion
Theoretical approaches traditionally applied in mental health and criminal justice interventions fail to address the historical and structural context that partially explains health disparities experienced in low-income and predominantly African-American communities. Community Wise was developed to address this gap by applying critical consciousness theory to intervene on individual thinking and behaviors that can eventually culminate in community and structural changes. This pilot study was the first step in assessing whether such an approach would be feasible. Findings helped us better conceptualize critical consciousness and explore its potential relationships with psychological distress, substance abuse, related health risk behaviors, and reoffending. For instance, we view these outcomes as manifestations of internalized oppression in reaction to structural oppression. By engaging in dialogue with participants we engage them in a new way of understanding their behavior and the structural powers around them. We then focus on community engagement and community action as a way to utilize existing strengths and resources to address community challenges.
Future research will continue to pilot test the revised version of Community Wise until the manual’s efficacy is optimized. We will continue to explore the role that gender may play in the critical dialogue and as a moderating variable. We must continue to explore creative ways to engage the community with this stigmatized population so that we can break stereotypes not only among participants, but also in the community at large. A better understanding about the way that social change projects are developed, implemented, and evaluated is needed. Such an understanding can improve the manual and make this process more effective for participants. Finally, we must develop ways to measure the community impact that Community Wise may have. Currently, behavioral interventions focus on individual-level measures of thinking and behaviors. We need measures that can capture actual changes that occur at the community and at the structural level as a result of changes in individual behavior.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen IM. PTSD among African Americans. In: Marsella AJ, Friedman MJ, Gerrity ET, Scurfield RM, editors. Ethnocultural aspects of post-traumatic stress disorder: Issues, research, and clinical practice. Washington, DC: American Psychological Association; 1996. pp. 209–238. [Google Scholar]
- Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: A review. The American Journal of Drug and Alcohol Abuse. 2003;29(1):19–53. doi: 10.1081/ada-120018838. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Labouvie EW, Bux DA. Assessing consequences of substance use: Psychometric properties of the Inventory of Drug Use Consequences. Psychology of Addictive Behaviors. 2003;17(4):328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Blitz CL, Wolff N, Pan KY, Pogorzelski W. Gender-Specific Behavioral Health and Community Release Patterns Among New Jersey Prison Inmates: Implications for Treatment and Community Reentry. American Journal of Public Health. 2005;95(10):1741–1746. doi: 10.2105/AJPH.2004.059733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd-Franklin N. In: Racism, secret-keeping, and African-American families. Imber-Black E, editor. W. W. Norton & Co, Inc; 1993. pp. 331–354. [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Braveman PA, Kumanyika S, Fielding J, LaVeist T, Borrell LN, Manderscheid R, Troutman A. Health Disparities and Health Equity: The Issue Is Justice. American Journal of Public Health. 2011;101:S149–S155. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BS, O’Grady KE, Battjes RJ, Katz EC. The Community Assessment Inventory—Client views of supports to drug abuse treatment. Journal of substance abuse treatment. 2004;27(3):241–251. doi: 10.1016/j.jsat.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Brown-Reid TL, Harrell JP. Racist experiences and health outcomes: An examination of spirituality as a buffer. Journal of Black Psychology. 2002;28:18–36. [Google Scholar]
- Caetano R. Alcohol related health disparities and treatment- related epidemiological findings among Whites, Blacks, and Hispanics in the United States. Alcoholism: Clinical and experimental research. 2003;27(8):1337–1339. doi: 10.1097/01.ALC.0000080342.05229.86. [DOI] [PubMed] [Google Scholar]
- Caetano R, Clark CL. In: Acculturation, alcohol consumption, smoking, and drug use among Hispanics. Chun KM, Organista PB, Marin G, editors. Washington, D.C: American Psychological Association; 2003. pp. 223–239. [Google Scholar]
- Centers for Disease Control. HIV Among African Americans. 2011. [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal Of Public Health. 2008;18(8):407. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London: Sage Publications Limited; 2006. [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Community Research Branch, N. I. on D. A. Risk Behavior Assessment. 1993. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual. 3. Minneapolis, MN: NCS Pearson; 1993. [Google Scholar]
- Diamond PM, Magaletta PR. The short-form Buss-Perry Aggression Questionnaire (BPAQ-SF): a validation study with federal offenders. Assessment. 2006;13:227–240. doi: 10.1177/1073191106287666. [DOI] [PubMed] [Google Scholar]
- Diemer MA, Blustein DL. Critical consciousness and career development among urban youth. Journal of Vocational Behavior. 2006;68:220–232. [Google Scholar]
- Dolan K, Rouen D, Kimber J. An overview of the use of urine, hair, sweat and saliva to detect drug use. Drug and Alcohol Review. 2004;23(2):213–217. doi: 10.1080/09595230410001704208. [DOI] [PubMed] [Google Scholar]
- Donohue B, Strada MJ, Rosales R, Taylor-Caldwell A, Hise D, Ahman S, Lefforge NL, et al. The Semistructured Interview for Consideration of Ethnic Culture in Therapy Scale: Initial Psychometric and Outcome Support. Behavior modification. 2006;30(6):867–891. doi: 10.1177/0145445505276096. [DOI] [PubMed] [Google Scholar]
- Esser-Stuart JE, Lyons MA. Barriers and influences in seeking health care among lower income minority women. Social Work in Health Care. 2002;35(3):85–99. doi: 10.1300/J010v35n03_06. [DOI] [PubMed] [Google Scholar]
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qualitative health research. 2006;16(3):377–394. doi: 10.1177/1049732305285708. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, McHugh P, Fanjiang G. Mini-Mental State Examination user’s guide. Odessa, FL: Psychological Assessment Resources; 2001. [Google Scholar]
- Franklin AJ. From brotherhood to manhood: How Black men rescue their relationships and dreams from the invisibility syndrome. New Jersey: John Wiley; 2004. [Google Scholar]
- Franklin AJ, Boyd-Franklin N, Kelly S. Racism and Invisibility: Race-related stress, emotional abuse and psychological trauma for people of color. In: Blitz LV, Greene MP, editors. Racism and Racial Identity: Reflections on Urban Practice in Mental Health and Social Services. New York: The Haworth Press, Inc; 2006. pp. 9–30. [Google Scholar]
- Freire P. Pedagogy of the oppressed. New York, NY: The Continuum Publishing Company; 2000. p. 164. [Google Scholar]
- Fuller CM, Galea S, Blaney S, Ompad DC, Deren S, Des Jarlais D, Vlahov D. Explaining the relationship between race/ethnicity and pharmacy purchased syringes among injection drug users in New York City. Ethnicity & Disease. 2004;14(4):589–596. (Print) [PubMed] [Google Scholar]
- Gee GC, Delva J, Takeuchi DT. Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. American Journal of Public Health. 2007;97:933. doi: 10.2105/AJPH.2005.075739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman RM, Speers MA, McLeroy K, Fawcett S, Kegler M, Parker E, Smith SR, et al. Identifying and Defining the Dimensions of Community Capacity to Provide a Basis for Measurement. 1998;25(3):258–278. doi: 10.1177/109019819802500303. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, et al. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and alcohol dependence. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and Drug Behavior Patterns and HIV and STD Racial Disparities: The Need for New Directions. American Journal of Public Health. 2007;97(1):125–132. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Israel B, Schultz A, Parker E, Becker A, Allen A, Guzman R. In: Critical issues in developing and following community based participatory research principles. Minkler M, Wallwestein N, Hall B, editors. New York: Thousand Oaks; 1998. [Google Scholar]
- Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health of African Americans: A thirteen year national panel study. Ethnicity & Disease. 1996;6(1, 2):132–147. [PubMed] [Google Scholar]
- Jessell L, Jemal A, Blom V, Windsor L. Operationalizing critical consciousness: Community Based Participatory Research and scale development. National Association of Social Workers Conference; Atlantic City, NJ.. 2012. [Google Scholar]
- LaVeist T. Minority populations and health: An introduction to health disparities in the United States. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- LaVeist T, Pollack K, Jr, RT, Fesahazion R, Gaskin D. Place, Not Race: Disparities Dissipate In Southwest Baltimore When Blacks And Whites Live Under Similar Conditions. Health affairs. 2011;30(10):1880–1887. doi: 10.1377/hlthaff.2011.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy R, Holland S. Treatment Plans and Interventions for Depression and Anxiety Disorders. New York: The Guilford Press; 2000. [Google Scholar]
- Lese KP, MacNair-Semands RR. The Therapeutic Factors Inventory: Development of a Scale. Group. 2000;24:303–317. [Google Scholar]
- Liberia. Africa Research Bulletin: Political, Social & Cultural Series. 2008;45(7):17611–17612. [Google Scholar]
- Longshore D. Help seeking by African American drug users: A prospective analysis. Addictive Behaviors. 1999;24(5):683–686. doi: 10.1016/s0306-4603(98)00111-7. [DOI] [PubMed] [Google Scholar]
- MacKenzie KR. In: The clinical application of a Group Climate measure. RRD, MacKenzie KR, editors. New York: International Universities Press; 1983. pp. 159–170. [Google Scholar]
- Malcarne VL, Chavira PJ, Liu DA, Fernandez S. The Scale of Ethnic Experience: A Measure for use across ethnic groups. Journal of Personality Assessment. 2006;86:150–161. doi: 10.1207/s15327752jpa8602_04. [DOI] [PubMed] [Google Scholar]
- Martin JK, Tuch SA, Roman PM. Problem drinking patterns among African Americans: The impacts of reports of discrimination, perceptions of prejudice, and “risky” coping strategies. Journal of Health and Social Behavior. 2003;44:408. [PubMed] [Google Scholar]
- McKay M, Hibbert R, Lawrence R, Miranda A, Paikoff R, Bell CC, Madison-Boyd S, et al. In: Creating mechanisms for meaningful collaboration between members of urban communities and university-based HIV prevention researchers. Mckay MM, Roberta P, editors. Binghamton, NY: The Haworth Press, Inc; 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment: initial studies of the treatment service review. Journal of Nervous and Mental Disease. 1992;180:101–210. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- Metzger D, Navaline H, Woody G. 2001 Assessment of Substance Abuse: HIV Risk Assessment Battery (RAB) The Gale Group Inc; 2001. [Google Scholar]
- Moore LD, Elkavich A. Who’s using and who’s doing time: Incarceration, the war on drugs, and public health. American Journal of Public Health. 2008;98(5):782. doi: 10.2105/AJPH.2007.126284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among black, Hispanic, and white Americans: Findings from the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs. 2008;69:824. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullaly B. Challenging oppression: A critical social work approach. Don Mills, Ontario: Oxford University Press; 2002. p. 232. [Google Scholar]
- National Institute on Drug Abuse. Minority report on racial minorities. 2003:159. [Google Scholar]
- National Institute on Drug Abuse. Report of the racial/ethnic health disparities work group of the National Advisory Council on Drug Abuse. 2005. [Google Scholar]
- National Institute on Drug Abuse. Drugs, brains, and behavior: The science of addiction. 2007;2007 [Google Scholar]
- National Institute on Drug Abuse. Strategic Plan on Reducing and Ultimately Eliminating Health Disparities 2008 [Google Scholar]
- National Institute on Drug Abuse. Drug facts: Treatment statistics 2011 [Google Scholar]
- National Institute on Drug Abuse. Drug use among racial/ethnic minorities 2012 [Google Scholar]
- New Jersey Department of Health and Human Services. Strategic Plan to Eliminate Health Disparities in NJ. Vol. 2010. Trenton, NJ: 2007. [Google Scholar]
- Pinto RM. Community perspectives on factors that influence collaboration in public health research. Health Behavior and Education. 2009;36:930–947. doi: 10.1177/1090198108328328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto RM, Campbell ANC, Hien DA, Yu G, Gorroochurn P. Retention in the National Institute on Drug Abuse Clinical Trials Network Women and Trauma Study: Implications for Posttrial Implementation. American Journal of Orthopsychiatry. 2011;81(2):211–217. doi: 10.1111/j.1939-0025.2011.01090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto RM, Spector AY, Valera PA. Exploring group dynamics for integrating scientific and experiential knowledge in community advisory boards for HIV research. AIDS Care. 2011:1–8. doi: 10.1080/09540121.2010.542126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pluhar E, Yeager KA, Corkran C, McCarty F, Holstad MMD, Denzmore-Nwagbara P, Fielder B, et al. Implementation of audio computer-assisted interviewing software in HIV/AIDS research. The Journal of the Association of Nurses in AIDS Care: JANAC. 2007;18(4):51. doi: 10.1016/j.jana.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JM, Trochim WMK. An Examination of Community Members’, Researchers’ and Health Professionals’ Perceptions of Barriers to Minority Participation in Medical Research: An Application of Concept Mapping. Ethnicity & Health. 2007;12(5):521–539. doi: 10.1080/13557850701616987. [DOI] [PubMed] [Google Scholar]
- Rubin A, Babbie E. Research methods for social work. 4. Belmont, CA: Wadsworth; 2001. [Google Scholar]
- Rubin MS, Colen CG, Link BG. Examination of Inequalities in HIV/AIDS Mortality in the United States From a Fundamental Cause Perspective. American Journal of Public Health. 2010;100(6):1053–1059. doi: 10.2105/AJPH.2009.170241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto I, Pitner RO. Use of critical consciousness in anti-oppressive social work practice: Disentagling power dynamics at personal and structural levels. British Journal of Social Work. 2005;35:435–452. [Google Scholar]
- Schmidt L, Greenfield T, Mulia N. Unequal treatment: Racial and ethnic disparities in alcoholism treatment services. Alcohol Research & Health. 2006;29(1):49–54. [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, et al. The M.I.N.I. International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview. Journal of Clinical Psychiatry. 1998;59(suppl):22–33. [PubMed] [Google Scholar]
- Sheikh A. Why Are Ethnic Minorities Under-Represented in US Research Studies? PLoS Medicine. 2006 doi: 10.1371/journal.pmed.0030049. Retrieved from https://search.ebscohost.com/login.aspx?direct=true&db=aph&AN=23694475&site=ehost-live. [DOI] [PMC free article] [PubMed]
- Simpson D. TCU Treatment Assessment Forms. Institutes of Behavioral Research, Texas Christian University; 2008. Retrieved from http://www.ibr.tcu.edu/pubs/datacoll/tcutreatment.html. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. In: Unequal treatment: What healthcare providers need to know about racial and ethnic disparities in healthcare. Henderson GE, Estroff S, Churchill LR, King NM, Oberlander J, Strauss R, editors. Durham: Duke University Press; 2002. [Google Scholar]
- Sobell LC, SMB . In: Timeline followback: A technique for assessing self-reported alcohol consumption. RZL, Allen J, editors. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Leading Change: A plan for SAMHSA’s roles & actions 2011–1014. 2011. [Google Scholar]
- U.S. Department of Health and Human Services, & Services, H. Healthy People 2010. 2nd Ed. With understanding and improving health and objectives health. 2 vol. 2000 Retrieved from http://www.healthypeople.gov.
- U.S. Department of Health and Human Services, & Services, H. Mental health: Culture, race, and ethnicity. A supplement to mental health: A report of the Surgeon General. 2001. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, & Services, H. Healthy People 2020. 2010 Retrieved from http://www.healthypeople.gov/2020/about/default.aspx.
- Wallerstein N, Sanchez-Merki V. Freirian praxis in health education: Research results from an adolescent prevention program. Health Education Research. 1994;9:105–118. doi: 10.1093/her/9.1.105. [DOI] [PubMed] [Google Scholar]
- Watts RJ, Diemer MA, Voight AM. Critical consciousness: Current status and future directions. In: Flanagan CA, Christens BD, editors. Youth civic development: Work at the cutting edge. New Directions for Child and Adolescent Development. Vol. 134. Wiley; 2011. pp. 43–57. [DOI] [PubMed] [Google Scholar]
- Watts RJ, Griffith DM, Abdul-Adil J. Sociopolitical development as an antidote for oppression - Theory and action. American Journal of Community Psychology. 1999;27(2):255–271. [Google Scholar]
- Windsor L. Using concept mapping for Community-Based Participatory Research: Paving the way for community-based health interventions for oppressed populations. Journal of Mixed Methods Research. 2013 doi: 10.1177/1558689813479175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windsor L, Dunlap E. What is substance use all about? Assumptions in New York’s drug policies and the perceptions of drug using low-income African-Americans. Journal of Ethnicity in Substance Abuse. 2010;9(1):64–87. doi: 10.1080/15332640903539260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windsor L, Negi N. Substance abuse and dependence among low income African Americans: Using data from the National Survey on Drug Use & Health to demystify assumptions. Journal of Addictive Diseases. 2009;28(3):258–268. doi: 10.1080/10550880903028510. [DOI] [PubMed] [Google Scholar]
- Windsor L, Pinto RM, Benoit E, Jessell L, Jemal A. Community Wise: Addressing oppression to promote individual and community health. Journal of Ethnicity & Cultural Diversity in Social Work. 2013 doi: 10.1080/1533256X.2014.962141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalom ID. The Theory and Practice of Group Psychotherapy. 4. New York: Basic Books; 1995. [Google Scholar]