Abstract
Introduction
Few studies have evaluated the frequency or predisposing factors for respiratory involvement in facioscapulohumeral muscular dystrophy type 1 (FSHD1) and type 2 (FSHD2).
Methods
We performed a prospective cross-sectional observational study of 61 genetically confirmed FSHD participants (53 FSHD1 and 8 FSHD2). Participants underwent bedside pulmonary function testing in sitting and supine positions, a standard clinical history and physical assessment, and manual muscle testing.
Results
Restrictive respiratory involvement was suggested in 9.8% (95% confidence interval 2.4 – 17.3): 7.5% FSHD1 and 25.0% FSHD2 (P=0.17). Participants with testing suggestive of restrictive lung involvement (n=6) were more severely affected (P=0.005), had weaker hip flexion (P=0.0007), and were more likely to use a wheelchair (P=0.01).
Conclusion
Restrictive respiratory involvement should be considered in all moderate to severely affected FSHD patients with proximal lower extremity weakness. The higher frequency of restrictive lung disease in FSHD2 seen here requires confirmation in a larger cohort of FSHD2 patients.
Keywords: Muscle Disease, Prevalence Studies, FSHD1, FSHD2, Respiratory disease
Introduction
Facioscapulohumeral muscular dystrophy (FSHD) is one of the most prevalent muscular dystrophies (1:20,000), but few studies have evaluated the frequency or predisposing factors for related respiratory complications in genetically confirmed individuals.1,2 FSHD is an autosomal dominant disorder characterized by descending, often asymmetric, progression of muscle weakness in the face and shoulder girdle, followed by humeral, truncal, and lower extremity muscles.3
The majority of FSHD patients (95%) have deletion of a critical number of macrosatellite repeat units in the D4Z4 region on chromosome 4q35 (termed FSHD1: > 10 repeats in normals, 1-10 in FSHD1). The remaining 5% of patients, termed FSHD2, develop disease through a contraction-independent mechanism. Common to both are epigenetic changes to the D4Z4 region which lead to transcriptional derepression of a retrogene (DUX4) believed to cause disease in a toxic gain-of-function manner.4 Although the 2 groups differ genetically, a study of 33 patients with FSHD2 suggested FSHD1 and FSHD2 were similar clinically.5
Evaluation of respiratory involvement in patients with genetically confirmed FSHD has been limited to 2 studies and to the best of our knowledge there have been no studies of respiratory function in FSHD2 patients.1,2 In a study of 15 FSHD1 patients, none had signs of restrictive lung disease.2 In the second study of 30 patients, 10 of whom were wheelchair dependent, 26.7% had a restrictive respiratory pattern.1 A Dutch study looked at the number of FSHD patients who required ventilatory support at 4 centers that supply all home ventilator support in the Netherlands relative to the prevalence of FSHD in the Dutch population to estimate that 1% of patients with FSHD required ventilator assistance.6 Given the paucity of information on respiratory involvement in FSHD, we set out to examine respiratory involvement in a large prospectively collected cohort of genetically confirmed and clinically characterized participants with FSHD. Additionally, we evaluated respiratory involvement in patients with FSHD2. Knowledge about which patients develop respiratory complications is important for clinical management and surveillance recommendations.
Methods
We performed a prospective cross-sectional observational study of 61 genetically confirmed and clinically affected FSHD participants between ages 18 and 75 years recruited between 2009 and 2012 as part of our Cellular and Molecular Pathophysiology (CAMP) Study at the University of Rochester Medical Center (Rochester, NY). The study was approved by our Institutional Review Board, and written and informed consent was obtained from all participants. We determined genetic mutation by previously published protocols (http://www.urmc.rochester.edu/fields-center/protocols/).5,7
Measurements
Forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) were measured using the Renaissance II Spirometer (model PB-700) by a single trained therapist. Following exhalation and full inhalation, participants exhaled hard and long into the sensor tube, with nose occluded. The best of 3 trials were recorded in both the sitting and supine positions. If facial muscle weakness resulted in a poor seal around the sensor tube, support was provided manually to ensure no air leakage. Results were reported as the percentage predicted according to age, gender, and height.8,9 The American Thoracic Society guideline identifies restrictive lung disease as an FVC below the 5th percentile of a normal population with a normal or increased FEV1/FVC ratio. Normative data have shown that this value is generally equivalent to an FVC below 80% predicted. 10,11 Thus, for screening purposes in a neuromuscular clinic setting we defined restrictive lung disease as an FVC of <80% predicted, with a preserved FEV1/FVC predicted ratio > 80%. Screened patients were confirmed to meet the American Thoracic Society criteria for restrictive lung disease, and their flow volume loop was consistent with a restrictive pattern.
Manual muscle testing (MMT) was performed utilizing a modified 13-point Medical Research Council Scale and standardized positions. The following muscle groups were included: bilateral shoulder abductors and forward flexors, elbow flexors and extensors, wrist extensors, hip flexors, knee flexors and extensors, and ankle dorsiflexors.12 A modified clinical severity score (CSS) was determined based on a scale proposed by Ricci et al, with raw scores multiplied by 2 to create whole numbers (http://www.urmc.rochester.edu/fields-center/protocols/disease-severity-scoring.cfm).13
Statistical analysis
Descriptive statistics including mean and standard deviation were used for demographics and baseline population characteristics. Patients were first grouped into FSHD1 and FSHD2 based on genetic testing and then separated into restrictive and non-restrictive patterns for analysis. FSHD1 and FSHD2 participants were grouped for evaluation of respiratory involvement in order to gain power to detect clinical associations and because a prior study suggested the patterns of weakness in FSHD1 and 2 are similar clinically.5 MMT scores were averaged across muscle groups to create total, lower extremity, and upper extremity scores. For single muscles the average of both sides (right and left) were used. The Student 2-sample t-test was used to compare groups. The Chi-square or Fisher exact test was used for comparisons of frequencies between groups. All testing was 2-sided, with a P-value <0.05 considered to be significant. Frequencies of respiratory involvement are presented with Wald binomial 95% confidence limits. Analysis was performed using Microsoft Excel 2008 (Microsoft Corporation), and STATA version 11.2 (Statacorp, College Station, TX).
Results
61 clinically affected and genetically characterized participants were evaluated between December 2009 and August 2012, including 53 participants with FSHD1 and 8 with FSHD2. The average age of participants was 49.5 years [standard deviation (SD) 13.4], with 31.1% women. FSHD1 participants had a mean D4Z4 contraction size of 23.4 kb (range 12-37 kb), while FSHD2 participants had a mean D4Z4 methylation of 13.2% (SD 5.3). There were no significant differences in baseline clinical characteristics between FSHD1 and FSHD2 (Table 1). Overall, participants reported symptom onset in the 3rd decade and were affected moderately (average age of onset 23.8 years for FSHD1 versus 25.7 years for FSHD2, P=0.76; mean CSS 5.2 for FSHD1 versus 5.3 for FSHD2, P=0.91; mean combined MMT 4.4 for FSHD1 versus 4.6 for FSHD2, P=0.31).
Table 1.
Baseline cohort characteristics
| Characteristic | FSHD1 | FHSD2 | P-value |
|---|---|---|---|
| Number (n) | 53 | 8 | * |
| Age, years (SD) | 50.0 (12.8) | 46.0 (17.7) | 0.42 |
| Women (%) | 16 (30.2%) | 3 (37.5%) | 0.70 |
| Age Symptom Onset, years (SD) | 23.8 (14.4) | 25.7 (19.0) | 0.76 |
| D4Z4 Contraction, kb (SD) | 23.4 (6.5) | * | * |
| Methylation (SD) | * | 13.2 (5.3) | * |
| CSS (SD) | 5.2 (2.3) | 5.3 (1.2) | 0.91 |
| Restrictive Pattern, number (%) | 4 (7.5%) | 2 (25%) | 0.17 |
| FVC Sitting %Predicted (SD) | 101.4 (26.0) | 102.0 (32.7) | 0.95 |
| FVC Supine %Predicted (SD) | 95.8 (26.7) | 98.8 (28.5) | 0.77 |
| FVC supine-sitting (SD) | −5.6 (−13.6) | −3.0 (−5.0) | 0.62 |
| Self-reported breathing problem (%) | 9 (17.0%) | 3 (37.5%) | 0.18 |
| History of asthma (%) | 4 (7.5%) | 1 (12.5%) | 0.51 |
| History of emphysema (%) | 0 | 0 | * |
| History of Smoking (%) | 21 (39.6%) | 3 (37.5%) | >0.99 |
| Use of Wheelchair (%) | 5 (9.4%) | 1 (12.5 %) | >0.99 |
| Nocturnal mechanical ventilation | 0 | 0 | * |
| Combined MMT score (SD) | 4.4 (0.7) | 4.6 (0.6) | 0.31 |
| Shoulder Range of Motion degrees (SD) | 101.2 (51.3) | 81.9 (26.0) | 0.31 |
not applicable
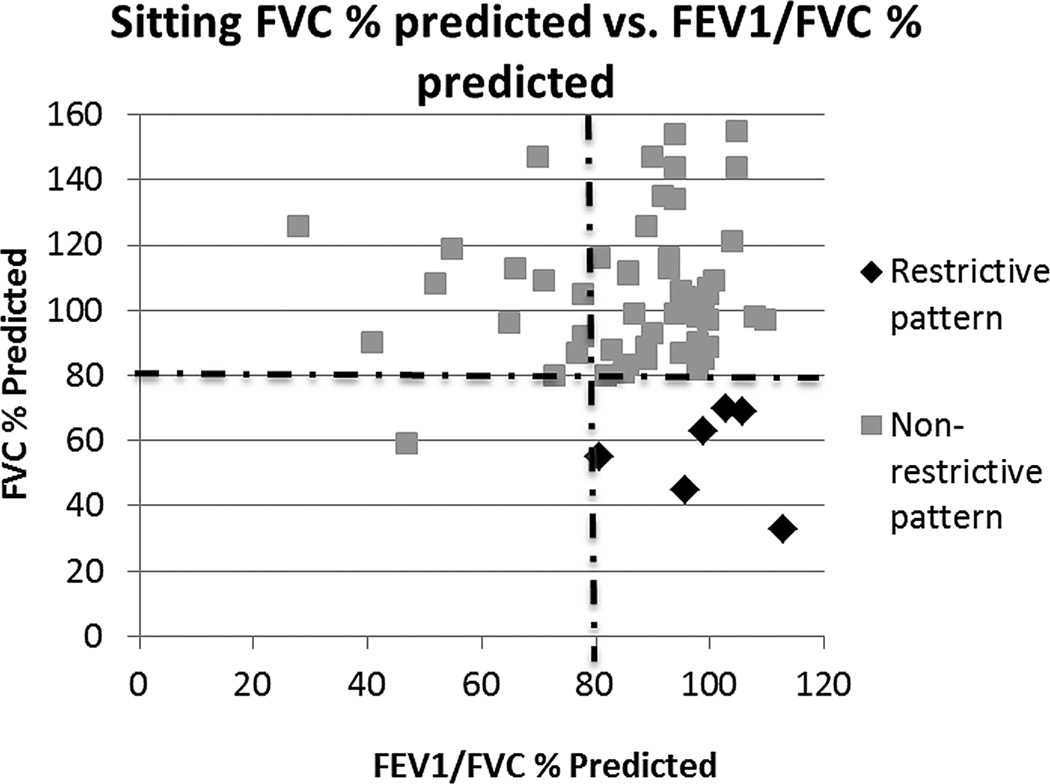
Mean sitting FVC for FSHD1 and FSHD2 was 101.4% predicted and 102.0% predicted, respectively (P=0.95). Overall, for both groups restrictive respiratory involvement was suggested in 9.8% [95% confidence interval (CI) 2.4, 17.3, Figure 1], 7.5% for FSHD1 versus 25.0% for FSHD2 (P=0.17). Mean change from sitting to supine was -5.6% for FSHD1 and -3.0% for FSHD2 (P=0.62). None of the patients in the cohort used non-invasive or invasive nocturnal ventilation. However, non-invasive positive pressure ventilation was offered to all patients with bedside PFTs suggestive of restrictive lung disease and FVC < 50%.
Figure 1.
Plot of FVC versus FEV1/FVC percent predicted. Restrictive pattern was defined as an FVC < 80% predicted, and FVC/FEV1% predicted > 80%.
Clinical characteristics of patients with restrictive pulmonary involvement are shown in Table 2. Participants with restrictive lung involvement were more severely affected; they had higher clinical severity scores (CSS 7.5 versus 4.9, P=0.005), decreased shoulder ROM (55.0 degrees versus 103.5 degrees, P=0.02), and were more likely to use a wheelchair (50.0% versus 5.4%, P=0.01). Participants with restrictive respiratory involvement were weaker in the lower extremity muscles, in particular hip flexors (mean MMT 3.7 versus 4.6, P=0.0007), knee flexors (mean MMT 3.5 versus 4.4, P=0.01), and knee extensors (mean MMT 4.2 versus 4.8, P=0.02). Ankle dorsiflexion, clinically one of the weakest lower extremity muscles (Average MMT of 3.0), was not associated significantly with lung disease (P=0.34). Additionally, the total combined average MMT, history of asthma, and smoking were not different significantly between groups.
Table 2.
Clinical characteristics of participants with restrictive lung involvement (FSHD1 and FSHD2 inclusive)
| Characteristic | Restrictive Pattern | Non-restrictive Pattern | P-value |
|---|---|---|---|
| Number (%) | 6 (9.8%) | 55 (90.2%) | * |
| Age years (SD) | 48.9(13.3) | 54.8 (14.6) | 0.31 |
| Gender female (%) | 3 (50.0%) | 16 (29.0%) | 0.36 |
| Age at symptom onset (SD) | 23.6 (14.5) | 36.3 (11.09) | 0.09 |
| FSHD1 (%) | 4 (66.7%) | 49 (89.0%) | 0.17 |
| CSS (SD) | 7.5 (1.4) | 4.9(2.1) | 0.005 |
| FVC supine-sitting (SD) | −2.3 (7.4) | −4.3 (13.3) | 0.56 |
| Self-reported breathing problem (%) | 4 (66.7%) | 8 (14.5%) | 0.01 |
| History of asthma (%) | 2 (33.3%) | 4 (7.3%) | 0.10 |
| History of Smoking (%) | 4 (66.7%) | 21 (38.2%) | 0.38 |
| Use of Wheelchair (%) | 3 (50.0%) | 3 (5.4%) | 0.01 |
| Composite MMT score (SD) | 4.0 (0.8) | 4.5 (0.6) | 0.12 |
| Hip Flexion (SD) | 3.7 (0.8) | 4.6 (0.5) | 0.0007 |
| Knee Extension (SD) | 4.2 (0.8) | 4.8 (0.5) | 0.02 |
| Knee Flexion (SD) | 3.5 (1.6) | 4.4 (0.7) | 0.01 |
| Ankle Dorsiflexion (SD) | 3.0 (1.5) | 3.7 (1.5) | 0.34 |
| Shoulder ROM degrees (SD) | 55.0 (22.1) | 103.5 (48.8) | 0.02 |
not applicable
Discussion
This is the largest cohort of pulmonary function testing in genetically confirmed FSHD patients and the only study to investigate pulmonary function in FSHD2 patients. Although the mean pulmonary function was normal in both groups, 9.8% of participants had pulmonary function testing that was suggestive of restrictive respiratory involvement. These participants were more severely affected, had increased pelvic girdle weakness, and were more likely to use a wheelchair.
Prior to standardized genetic testing, a study suggested up to 50% of FSHD patients can have respiratory involvement.14 Two smaller subsequent studies of respiratory involvement in genetically confirmed FSHD showed a restrictive pattern between 0 and 26.7%.1,2 One study showed reduced maximal expiratory pressures but normal inspiratory pressures, suggesting respiratory involvement is due to weakness of chest wall musculature, not diaphragmatic weakness.2 A subsequent study analyzed chest wall kinematics using Optoelectronic Plethysmography and suggested significant reduction in the abdominal component in the supine versus sitting position during quiet breathing.1 A Dutch population study identified 10 FSHD patients who required home mechanical ventilation, representing approximately 1% of the total Dutch FSHD population.6 Eight of these patients had symptoms of nocturnal hypoventilation before respiratory insufficiency was diagnosed.6
The restrictive lung involvement seen in our cohort was not explained by history of smoking or other obstructive pulmonary diseases. Although we did not perform chest wall kinematics, the pattern on bedside testing supports intercostal muscle weakness over diaphragmatic, since there was no significant decrease in the FVC from sitting to supine (P=0.56). The average decrease of −5.3% is in line with previously published normative values.15 The suggestion of intercostal muscle weakness supports the concept that weakness of truncal or axial musculature may lead to the restrictive respiratory pattern seen in FSHD and that proximal lower extremity weakness may be an early indicator for patients at risk for pulmonary complication. This also fits with the common conception of descending weakness and lower extremity weakness as a marker of overall disease severity.13
This study evaluated respiratory involvement in patients with FSHD2. The trend towards higher frequency of respiratory involvement in FSHD2 (25%) vs. 7.5% in FSHD1, needs to be evaluated further in a larger cohort, given the small number of FSHD2 participants in this study.
Limitations to this study include possible referral bias. All participants were ambulatory, and although some participants used wheelchairs or other assistive devices during ambulation, none were permanently wheelchair bound. Nevertheless, our cohort is a fair representation of the FSHD population typically encountered in clinic; the age of onset, mean D4Z4 contraction size, and clinical severity were similar to other large FSHD cohorts.16,17,13 Additionally, all patients with bedside screening suggestive of restrictive lung involvement should have formal pulmonary testing including total lung capacity and diffusion capacity to exclude false positive results that can be seen in obesity or obstructive lung disease.
Current FSHD standards of care, based on expert opinion, recommend baseline screening for respiratory involvement in all patients with moderate to severe disease.3 Our data support these recommendations; in addition, based on the association with wheelchair use at any time and increased predominately proximal lower extremity weakness in participants with testing suggestive of restrictive respiratory involvement, we recommend yearly bedside pulmonary function screening in patients with any pelvic girdle weakness or who utilize a wheelchair.6 Since restrictive respiratory involvement appears to be due to axial or truncal weakness versus true diaphragmatic weakness, we also recommend screening individuals with marked kyphoscoliosis. All patients with bedside screening suggestive of a restrictive pattern of lung involvement should be questioned about signs and symptoms associated with hypercarbia, and a multi-disciplinary approach should be taken, with referral to a pulmonologist for formal lung function testing. In the most severely affected patients, those wheelchair bound due to proximal lower extremity weakness, a sleep study with measurements of end-tidal CO2 to look for signs of nocturnal hypoventilation, is warranted.2 Ultimately, a longitudinal cohort is needed to be able to determine the true risk of developing respiratory complications over time in FSHD. However, FSHD is a rare disease, and thus such large international efforts are not practicable or likely forthcoming. Prospectively collected observational studies, like this study, are essential when formulating guidelines for clinical care.
Acknowledgements
This Study has been funded in whole or in part by the National Institutes of Health (grant # 1PO1NS069539-01) and NIH NCRR UL1RR024160. Dr. Statland’s work on this project was supported by the Muscular Dystrophy Association Clinical Research Training Grant. We thank the patients and their family members who were the impetus for this study.
Abbreviations
- CSS
clinical severity score
- FSHD
fascioscapulohumerol musclar dystrophy
- FSHD1
fascioscapulohumerol musclar dystrophy type 1
- FSHD2
fascioscapulohumerol musclar dystrophy type 2
- FEV1
forced expiratory volume
- FVC
forced vital capacity (FVC)
- MMT
manual muscle testing
- ROM
range of motion
References
- 1.D'Angelo MG, Romei M, Lo Mauro A, Marchi E, Gandossini S, Bonato S, et al. Respiratory pattern in an adult population of dystrophic patients. Journal of the neurological sciences. 2011;306((1–2)):54–61. doi: 10.1016/j.jns.2011.03.045. [DOI] [PubMed] [Google Scholar]
- 2.Stubgen JP, Schultz C. Lung and respiratory muscle function in facioscapulohumeral muscular dystrophy. Muscle & nerve. 2009;39(6):729–734. doi: 10.1002/mus.21261. [DOI] [PubMed] [Google Scholar]
- 3.Lemmers RJ, van der Vliet PJ, Klooster R, Sacconi S, Camano P, Dauwerse JG, et al. A unifying genetic model for facioscapulohumeral muscular dystrophy. Science. 2010;329(5999):1650–1653. doi: 10.1126/science.1189044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Maarel SM, Tawil R, Tapscott SJ. Facioscapulohumeral muscular dystrophy and DUX4: breaking the silence. Trends Mol Med. 2011;17(5):252–258. doi: 10.1016/j.molmed.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Greef JC, Lemmers RJ, Camano P, Day JW, Sacconi S, Dunand M, et al. Clinical features of facioscapulohumeral muscular dystrophy 2. Neurology. 2010;75(17):1548–1554. doi: 10.1212/WNL.0b013e3181f96175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wohlgemuth M, van der Kooi EL, van Kesteren RG, van der Maarel SM, Padberg GW. Ventilatory support in facioscapulohumeral muscular dystrophy. Neurology. 2004;63(1):176–178. doi: 10.1212/01.wnl.0000133126.86377.e8. [DOI] [PubMed] [Google Scholar]
- 7.Wijmenga C, Hewitt JE, Sandkuijl LA, Clark LN, Wright TJ, Dauwerse HG, et al. Chromosome 4q DNA rearrangements associated with facioscapulohumeral muscular dystrophy. Nat Genet. 1992;2(1):26–30. doi: 10.1038/ng0992-26. [DOI] [PubMed] [Google Scholar]
- 8.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. American journal of respiratory and critical care medicine. 1999;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 9.Knudson RJ, Slatin RC, Lebowitz MD, Burrows B. The maximal expiratory flow-volume curve. Normal standards, variability, and effects of age. The American review of respiratory disease. 1976;113(5):587–600. doi: 10.1164/arrd.1976.113.5.587. [DOI] [PubMed] [Google Scholar]
- 10.Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis. 1991;144(5):1202–1218. doi: 10.1164/ajrccm/144.5.1202. [DOI] [PubMed] [Google Scholar]
- 11.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. The European respiratory journal. 2005;26(5):948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 12.Personius KE, Pandya S, King WM, Tawil R, McDermott MP. Facioscapulohumeral dystrophy natural history study: standardization of testing procedures and reliability of measurements. The FSH DY Group. Phys Ther. 1994;74(3):253–263. doi: 10.1093/ptj/74.3.253. [DOI] [PubMed] [Google Scholar]
- 13.Ricci E, Galluzzi G, Deidda G, Cacurri S, Colantoni L, Merico B, et al. Progress in the molecular diagnosis of facioscapulohumeral muscular dystrophy and correlation between the number of KpnI repeats at the 4q35 locus and clinical phenotype. Annals of neurology. 1999;45(6):751–757. doi: 10.1002/1531-8249(199906)45:6<751::aid-ana9>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 14.Kilmer DD, Abresch RT, McCrory MA, Carter GT, Fowler WM, Jr, Johnson ER, et al. Profiles of neuromuscular diseases. Facioscapulohumeral muscular dystrophy. Am J Phys Med Rehabil. 1995;74(5 Suppl):S131–S139. doi: 10.1097/00002060-199509001-00007. [DOI] [PubMed] [Google Scholar]
- 15.Vilke GM, Chan TC, Neuman T, Clausen JL. Spirometry in normal subjects in sitting, prone, and supine positions. Respiratory care. 2000;45(4):407–410. [PubMed] [Google Scholar]
- 16.Lunt PW, Jardine PE, Koch MC, Maynard J, Osborn M, Williams M, et al. Correlation between fragment size at D4F104S1 and age at onset or at wheelchair use, with a possible generational effect, accounts for much phenotypic variation in 4q35-facioscapulohumeral muscular dystrophy (FSHD) Hum Mol Genet. 1995;4(5):951–958. doi: 10.1093/hmg/4.5.951. [DOI] [PubMed] [Google Scholar]
- 17.Mostacciuolo ML, Pastorello E, Vazza G, Miorin M, Angelini C, Tomelleri G, et al. Facioscapulohumeral muscular dystrophy: epidemiological and molecular study in a north-east Italian population sample. Clin Genet. 2009;75(6):550–555. doi: 10.1111/j.1399-0004.2009.01158.x. [DOI] [PubMed] [Google Scholar]