Abstract
Segmental testicular infarction is a rare cause of acute scrotal pain. The appearances on grey-scale sonography are often indistinguishable from that of a testicular tumour, resulting in unnecessary orchiectomy. We report a case of acute bilateral testicular infarction, of unknown etiology, which was conservatively managed to resolution following a confident diagnosis achieved with the aid of contrast-enhanced ultrasound (CEUS) and real-time tissue elastography (RTE) along with conventional grey-scale and Doppler sonography. The evolving appearances on each of the sonographic modalities are described. We discuss the importance of complementing conventional sonography with CEUS and RTE in order to make a confident diagnosis and avoid unnecessary surgical intervention.
Keywords: Testis, Segmental infarction, Ultrasonography, Contrast-enhanced ultrasound, Tissue elastography
Riassunto
L’infarto testicolare segmentale è una causa rara di dolore scrotale acuto. L’aspetto ecografico, in scala di grigi, è spesso indistinguibile da quello di un tumore testicolare, con conseguenti orchiectomie inutili. Riportiamo un caso di infarto testicolare acuto bilaterale, ad eziologia sconosciuta, gestito in maniera conservativa fino a risoluzione, dopo una diagnosi realizzata con l’ausilio di ecografia con messo di contrasto (CEUS) e elastosonografia tessutale in tempo reale (RTE), ecografia convenzionale in scala di grigi e Doppler. Sono descritti gli aspetti, in ciascuna delle modalità ecografiche, dell’evoluzione delle lesioni. Discutiamo l’importanza della complementarietà dell’ecografia convenzionale con CEUS e RTE per effettuare una diagnosi di certezza ed evitare un inutile intervento chirurgico.
Introduction
Segmental testicular infarction is a rare cause of acute scrotal pain. The sonographic appearances are variable, both wedge-shaped and rounded lesions have been described, and may mimic a primary germ cell tumour of the testis [1]. Distinguishing a segmental infarction from a tumour is of critical importance in order to avoid unnecessary orchiectomy [2]. Newer techniques of contrast-enhanced ultrasound (CEUS) [3] and real-time tissue elastography (RTE) [4] are being used to aid in the differentiation of indeterminate intra-testicular abnormalities [5, 6]. We document the evolving appearances of bilateral testicular infarction on CEUS and RTE, which allowed for conservative management to resolution.
Case report
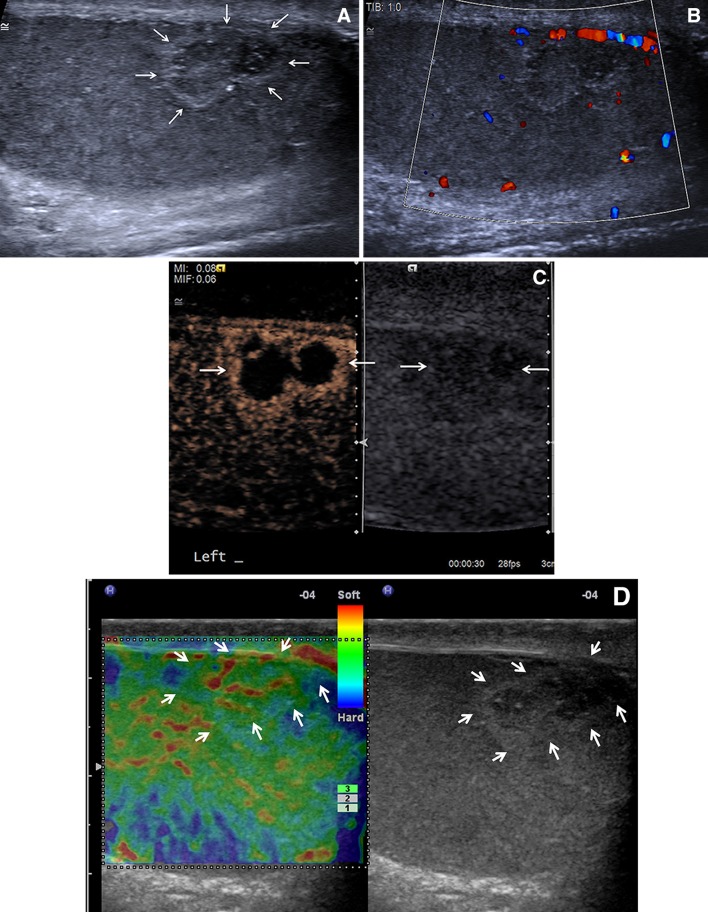
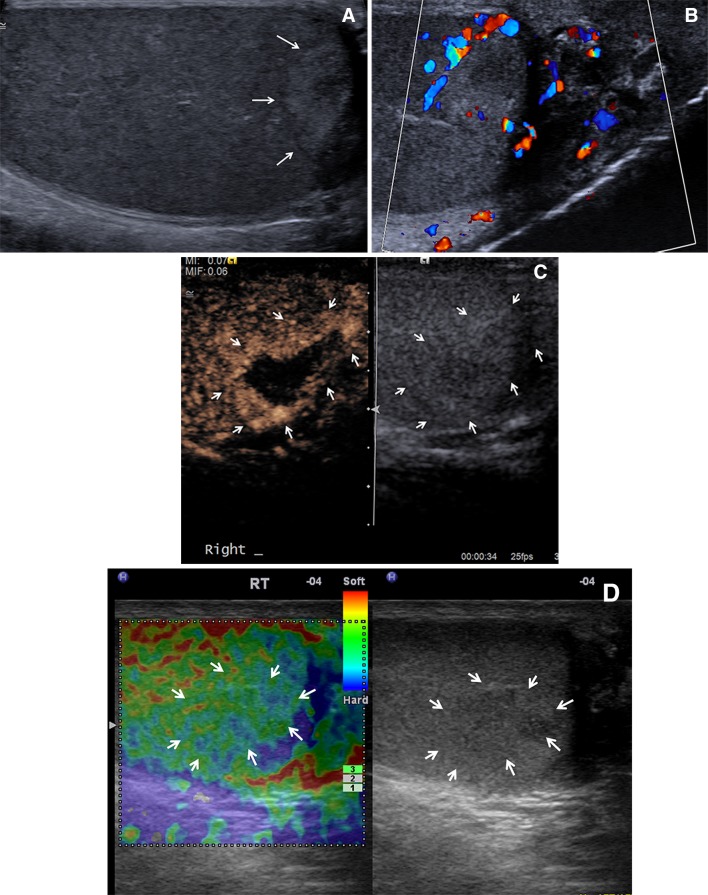
A 33-year-old healthy male presented with a 3-day history of acute onset, left-sided testicular pain. The pain had commenced spontaneously, with no preceding trauma or infection, was variable in nature and with no aggravating factors. The testis was tender to palpation but otherwise clinical examination was normal. All hematological markers including inflammatory and tumour markers were negative. At ultrasonography (14–9 MHz linear array transducers, Siemens S2000, Mountain View, CA) on day three, two rounded, focal areas of mixed reflectivity, with central low reflectivity, in the lower pole of the left testis were identified, measuring 7.8 × 6.7 mm and 9.3 × 6.4 mm (Fig. 1a). There was no colour Doppler flow or flow on CEUS (SonoVue™ 4.8 mLs, Bracco SpA, Milan, CPS™, low mechanical index imaging, Siemens, Mountain View, CA) demonstrable within the lesions, with hyperemia surrounding both lesions on the CEUS examination (Fig. 1b, c). Real-time tissue elastography (Hitachi HV900, Hitachi Medical Corporation, Tokyo, Japan) using a 14–6 MHz linear transducer and using Hitachi real-time tissue elastography (HI-RTE™, Hitachi Medical Corporation, Tokyo, Japan), demonstrated that the lesions were predominantly red/green and labelled “soft”, with a strain ratio estimated at 1.14 (Fig. 1d). At the time of the examination no abnormality was present in the right testis. The patient was assessed by Urology and a provisional diagnosis of focal segmental infarction was suggested. Further hematological investigations for vasculitis, a lipid profile and diabetes mellitus screen were performed all of which were normal. A full rheumatologic and autoimmune screen was normal. No cause was identified and the patient was symptomatically treated with analgesia. Seven days after the onset of symptoms in the left testis, the patient experienced similar pain in the right testis, and underwent a second sonographic examination. The appearances were similar to that originally seen on the left, with a heterogeneous mixed reflective lesion measuring 14.4 × 8.5 mm (Fig. 2a). There was no colour Doppler flow to the central aspect of the lesion and the CEUS examination demonstrated no central vascularity with surrounding hyperemia (Fig. 2b, c). The RTE examination demonstrated a predominantly green lesion with a strain ratio of 1.14 (Fig. 2d). The abnormality in the left testis at this time had regressed in size (combined measurement of 4.5 × 6.7 mm), with the RTE examination showing a predominant green colour, with some blue changes, and a strain ratio of 1.22 (Fig. 3a, b). Fourteen days after the initial presentation, clinical symptoms had subsided, with no pain reported, sonography demonstrated improvement with CEUS rim enhancement seen only on the right, the more recent lesion (Fig. 4a, b). A further follow-up sonographic examination after 50 days of presenting symptoms showed only minimal grey-scale change at the site of the previous abnormalities. The patient was discharged with no follow-up and remains well at 6 months with no repeat symptoms.
Fig. 1.
a A longitudinal grey-scale image of the left testis demonstrating two (arrows) closely located rounded low echogenic lesions, with surrounding high echogenicity. b A longitudinal colour Doppler image of the lesion, with no colour Doppler signal present within the lesion. c A dual view of the two lesions on contrast-enhanced ultrasound (arrows) demonstrating peripheral rim enhancement, and absent enhancement within the central aspects of the lesion. d A longitudinal real-time elastography image of the lesion, (arrows) demonstrating a predominantly green signal, with areas of red consistent with a “soft” lesion. A strain ratio was measured at 1.14 (not shown)
Fig. 2.
a A longitudinal grey-scale image of the right testis demonstrating (arrows) a rounded low echogenic centre with surrounding high echogenicity. b A longitudinal colour Doppler image of the lesion, with no colour Doppler signal present within the lesion. c A dual view of the lesion on contrast-enhanced ultrasound (arrows) demonstrating peripheral rim enhancement, and absent enhancement within the central aspects of the lesion. d A longitudinal real-time elastography image of the lesion, (arrows) demonstrating a predominantly green signal, with areas of blue consistent with a “soft” lesion. A strain ratio was measured at 1.14 (not shown)
Fig. 3.
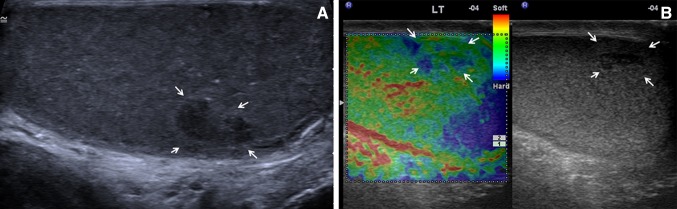
a A longitudinal grey-scale image of the left testis 7 days following the first examination demonstrating reduction in size of the lesion, with continuing central low echogenicity and surrounding increased echogenicity (arrows). b A longitudinal real-time elastography image of the lesion, (arrows) demonstrating a predominantly green signal, with areas of blue consistent with a “soft” lesion. A strain ratio was measured at 1.22 (not shown)
Fig. 4.
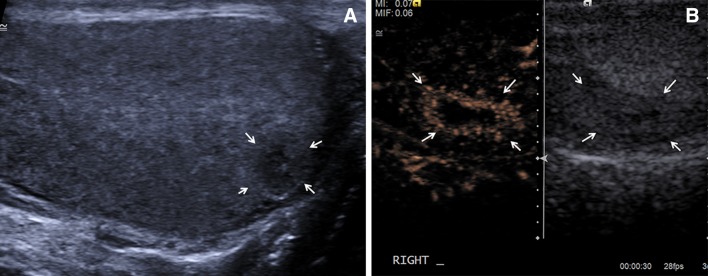
a A longitudinal grey-scale image of the right testis 7 days following the first examination demonstrating reduction in size of the lesion, with continuing central low echogenicity and surrounding increased echogenicity (arrows).b A dual view of the lesion on contrast-enhanced ultrasound (arrows) demonstrating peripheral rim enhancement, and absent enhancement within the central aspects of the lesion, with appearances much less florid than on the previous occasion
Discussion
Segmental testicular infarct is a rare entity that usually presents with an insidious onset of scrotal pain and tenderness with no other findings on clinical or hematological investigations [1, 7, 8]. The etiology is usually idiopathic; however, cases have been associated with hypercoagulability, vasculitis, torsion, trauma, infection and iatrogenic vessel damage [1]. The first line imaging investigation is usually grey-scale sonography with colour Doppler; however, CEUS [7, 8] and RTE [9] are being used to improve characterization of these lesions.
All lesions in our patient had similar early and delayed imaging appearances. Initially the lesions appeared as rounded, focal areas of mixed reflectivity. There was no colour Doppler flow or flow on CEUS demonstrable within the lesions, as expected for an ischemic testicular segment. Peripheral hyperemia was evident in both the lesions on CEUS, the mechanism for this is uncertain; possibly due to mass effect secondary to edema resulting in crowding of perilesional parenchymal vessels or due to an inflammatory process secondary to the ischemia. Both lesions were predominantly green on RTE, indicating that they were equivalent in stiffness to the adjacent normal testicular parenchyma. This would support the concept that an area of infarction represents liquefying tissue which is “soft”. At follow-up examinations the lesion gradually becomes smaller without significant alteration in the RTE appearances and stable strain ratios, perhaps reflecting organization of the hemorrhage and necrosis and the shrinkage in size of the lesion. Over 50 days, both lesions became inconspicuous on ultrasonography and the degree of peripheral hypervascularity on CEUS reduced as symptoms improved.
The sonographic appearances of segmental infarctions have been previously documented with the typical description of a rounded, hypo-echoic, avascular lesion. Variations have been reported in shape (rounded to wedge shaped), echogenicity (hypo-, iso- or hyper-echoic or of mixed echogenicity), vascularity (avascular although hypo-vascular lesions are seen) and degree of perilesional hypervascularity [1, 8]. In addition, the appearances of individual lesions vary as the lesion evolves. Therefore, confidently differentiating segmental infarction from a hypo-vascular tumour using conventional ultrasonography alone is difficult.
Contrast-enhanced ultrasound can improve characterization of segmental testicular infarction by better demonstrating the morphological features of the lesion which are different from those of a hypo-vascular tumour [7, 8]. Two findings in particular on CEUS are important [7, 8, 10–12]; vessels can be seen for a prolonged period after injection of micro bubbles, with the ability to differentiate between the normal centripetal testicular arteries originating from the capsular arteries and tumour neovascularization. Secondly, perilesional rim enhancement which is present for up to 17 days following onset of pain is a much more consistent finding than the perilesional hyperemia observed on Doppler sonographic examination.
A single case report describes the appearances of testicular infarction on RTE, demonstrating within 24 h of the onset of pain, an area of infarction as soft compared to the adjacent normal testicular parenchyma [13]. A 10-day follow-up with RTE demonstrated that the lesion was harder than the normal testicular tissue. We found that the area of infarction in our lesions were similar to the normal testicular tissue but RTE findings may be variable depending in the timing of the follow-up examinations, and in turn a difference in the degree of lesion resolution. There has only been one other case of bilateral segmental testicular infarcts which occurred in a healthy, male physician aged 31 years [14]. The authors reported negative tumour markers and consecutive daily sonographic examinations, with early orchiopexy due to uncertainty of the diagnosis. In the present case, the use of CEUS and RTE meant that we were able to make a confident diagnosis on imaging and tumour markers alone without the need for daily sonographic examinations and surgical intervention.
This report documents the conventional grey-scale sonography, CEUS and RTE appearances of the spontaneous occurrence, progression and resolution of bilateral segmental testicular infarcts. We conclude that multi-parametric imaging is essential in order to make a confident diagnosis and avoid unnecessary repeat imaging and surgery.
Conflict of interest
Ketul V. Patel, Dean Y. Huang, Paul S. Sidhu declare no conflict of interest with this case study. The patient gave informed consent to report the case.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2,000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
References
- 1.Bilagi P, Sriprasad S, Clarke JL, Sellars ME, Muir GH, Sidhu PS. Clinical and ultrasound features of segmental testicular infarction: six-year experience from a single centre. Eur Radiol. 2007;17:2810–2818. doi: 10.1007/s00330-007-0674-2. [DOI] [PubMed] [Google Scholar]
- 2.Sriprasad SI, Kooiman GG, Muir GH, Sidhu PS. Acute segmental testicular infarction: differentiation from tumour using high frequency colour Doppler ultrasound. Br J Radiol. 2001;74:965–967. doi: 10.1259/bjr.74.886.740965. [DOI] [PubMed] [Google Scholar]
- 3.Piscaglia F, Nolsoe C, Dietrich CF, Cosgrove DO, Gilja OH, BAchmann-Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O, Claudon M, Weskott HP, Clevert DA, Correas JM, D’Onofrio M, Drudi FM, Eyding J, Giovannini M, Hocke M, Ignee A, Jung EM, Klauser AS, Saftoiu A, Mathis G, Leen E, Lassau N, Seidel G, Sidhu PS, ter Haar G, Timmerman D. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;32:33–59. doi: 10.1055/s-0031-1281676. [DOI] [PubMed] [Google Scholar]
- 4.Bamber JC, Cosgrove DO, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH, Havre RF, Jenssen C, Klauser AS, Ohlinger R, Saftoiu A, Schaefer F, Sporea I, Piscaglia F. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: basic principles and technology. Ultraschall in Med. 2013;34:169–184. doi: 10.1055/s-0033-1335205. [DOI] [PubMed] [Google Scholar]
- 5.Huang DY, Sidhu PS. Focal testicular lesions: colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br J Radiol. 2012;85:S41–S53. doi: 10.1259/bjr/30029741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah A, Lung PF, Clarke JE, Sellars ME, Sidhu PS. New ultrasound techniques for imaging of the indeterminate testicular lesion may avoid surgery completely. Clin Radiol. 2010;65:496–498. doi: 10.1016/j.crad.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Lung PF, Jaffer OS, Sellars ME, Sriprasad S, Kooiman GG, Sidhu PS. Contrast enhanced ultrasound (CEUS) in the evaluation of focal testicular complications secondary to epidiymitis. AJR Am J Roentgenol. 2012;199:W345–W354. doi: 10.2214/AJR.11.7997. [DOI] [PubMed] [Google Scholar]
- 8.Bertolotto M, Derchi LE, Sidhu PS, Serafini G, Valentino M, Grenier N, Cova MA. Acute segmental testicular infarction at contrast-enhanced ultrasound: early features and changes during follow-up. AJR Am J Roentgenol. 2011;196:834–841. doi: 10.2214/AJR.10.4821. [DOI] [PubMed] [Google Scholar]
- 9.Goddi A, Sacchi A, Magistretti G, Almolla J, Salvadore M. Real-time elastography for testicular lesion assesment. Eur Radiol. 2012;22:721–730. doi: 10.1007/s00330-011-2312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lock G, Schmidt C, Helmich F, Stolle E, Dieckmann K. Early experience with contrast enhanced ultrasound in the diagnosis of testicular masses; a feasibility study. Urology. 2011;77:1049–1053. doi: 10.1016/j.urology.2010.12.035. [DOI] [PubMed] [Google Scholar]
- 11.Jaffer OS, Sidhu PS. Contrast-enhanced ultrasonography of the testes. Ultrasound Clin North Am. 2013;8:509–523. doi: 10.1016/j.cult.2013.06.003. [DOI] [Google Scholar]
- 12.Valentino M, Bertolotto M, Derchi L, Bertaccini A, Pavlica P, Martorana G, Barozzi L. Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol. 2011;21:1831–1840. doi: 10.1007/s00330-010-2039-5. [DOI] [PubMed] [Google Scholar]
- 13.Kantarci M, Olgun DC, Mihmanli I. Shear-wave elastography of segmental infarction of the testis. Korean J Radiol. 2012;13:820–822. doi: 10.3348/kjr.2012.13.6.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayne A, Koslin B, Daneshmand S. Bilateral segmental testicular infarction. TSW. Urology. 2007;2:53–57. doi: 10.1100/tsw.2007.146. [DOI] [PMC free article] [PubMed] [Google Scholar]