Executive Summary
Primary care–related emergency department (PCR-ED) utilization, including for conditions that are preventable or treatable with appropriate primary care, is associated with decreased efficiency of and increased costs to the health system. Many PCR-ED users experience actual or perceived problems accessing appropriate, ongoing sources of medical care. Patient navigation, an intervention used most often in the cancer care continuum, may help to address these barriers among medically underserved populations, such as those who are low income, uninsured, publicly insured, or recent U.S. immigrants.
We examined a patient navigation program designed to promote appropriate primary care utilization and prevent or reduce PCR-ED use at Memorial Hermann Health System in Houston, Texas. The intervention is facilitated by bilingual, state-certified community health workers (CHWs) who are trained in peer-to-peer counseling and connect medically underserved patients with medical homes and related support services. The CHWs provide education about the importance of primary care, assist with appointment scheduling, and follow up with patients to monitor and address additional barriers.
Our study found that the patient navigation intervention was associated with decreased odds of returning to the ED among less frequent PCR-ED users. Among patients who returned to the ED for PCR reasons, the pre/post mean visits declined significantly over a 12-month pre/post-observation period but not over a 24-month period. The savings associated with reduced PCR-ED visits were greater than the cost to implement the navigation program. Our findings suggest that an ED-based patient navigation program led by CHWs should be further evaluated as a tool to help reduce PCR-ED visits among vulnerable populations.
Introduction
An estimated 13% to 27% of emergency department (ED) visits in the United States could be managed in physician offices, clinics, and urgent care centers at a savings of $4.4 billion annually (Weinick, Burns, & Mehrotra, 2010). Many ED visits are made for primary care–related (PCR) reasons by individuals who go to the ED multiple times each year, or “frequent fliers” (Garcia, Bernstein, & Bush, 2010; Hoot & Aronsky, 2008; Schoen et al., 2004; Weinick et al., 2010). PCR-ED patients are defined as those for whom medical care was not required within 12 hours; those who required immediate medical care but could have been treated safely and effectively in a primary care setting; or those who required immediate medical care, but the emergent nature of the condition was potentially preventable or avoidable with timely and appropriate primary care (Begley, Courtney, & Brau, 2012; Billings, Parikh, & Mijanovich, 2000). Users of PCR-ED also are likely to be privately insured, publicly insured, or uninsured (Garcia et al., 2010).
Regardless of insurance status, individuals who do not have a usual source of care (USOC) provider, who are dissatisfied with their USOC provider, or who have experienced disruptions in regular care or perceived barriers to accessing their USOC provider are more likely than individuals who are satisfied with their USOC provider access to utilize the ED for PCR reasons (Petersen, Burstin, O'Neil, Orav, & Brennan, 1998; Petterson, Rabin, Hillips, Bazemore, & Dodoo, 2009; Sarver, Cydulka, & Baker, 2002; Weber, Showstack, Hunt, Colby, & Callaham, 2005).
In November 2008, Houston, Texas–based Memorial Hermann Health System initiated an ED-based patient navigation intervention to reduce or eliminate PCR-ED utilization, improve ED efficiency, and reduce uncompensated care costs in one of the city's busiest EDs, Memorial Hermann Texas Medical Center (MH-TMC). The program uses community health workers (CHWs) to connect Medicaid and uninsured patients with medical homes, promote appropriate preventive and primary care utilization, and reduce unnecessary costs associated with PCR-ED use.
In 2010, nearly 41% of the more than 1.5 million ED visits to Houston/Harris County hospitals were PCR, with uninsured and Medicaid patients accounting for more than 53% of all PCR-ED visits (Begley et al., 2012). These visits contributed to more than $5 billion in uncompensated care (bad debt and charity) provided by Texas hospitals to uninsured and underinsured patients in 2010 (THA, 2012).
In this article, we address three primary research questions:
Were PCR-ED users who received the navigation intervention, compared with those who did not, less likely to return to the ED for PCR reasons?
For all patients who used the ED for PCR reasons, did the organization's ED experience reductions in mean visits and costs in the post-observation period compared with the pre-observation period? If so, were these reductions greater for patients who received the navigation intervention compared with those who did not?
Were any such reductions in PCR-ED costs associated with the intervention greater than the costs incurred by delivering the intervention?
Conceptual Framework
Patient Navigation to Promote appropriate Utilization
Patient navigation for the purpose of eliminating barriers to timely cancer screening, diagnosis, treatment, and supportive care for poor and uninsured people was first introduced in 1990 in Harlem, New York (Paskett, Harrop, & Wells, 2011; Vargas, Ryan, Jackson, Rodriguez, & Freeman, 2008; Wells et al., 2008). More recently, patient navigation has been expanded to include the timely movement of individuals across the entire healthcare continuum—from preventive care, screening, and early diagnosis to treatment and end-of-life care—for cancers and other chronic diseases (Dohan & Schrag, 2005; Freeman & Rodriguez, 2011).
Patient navigators (PNs) bridge the gap between the health system and the patient. They represent their organizations as skilled, culturally competent care coordinators who have the ability to effectively communicate with providers and other stakeholders within and across the institution while serving patients as knowledgeable, caring peers and allies who have an inside track to the health system (Carroll et al., 2010). PNs help patients address barriers ranging from communication related (literacy, culture, and language) to psychological (fear and distrust) to financial (help with applying for public insurance and assistance programs) to health system related (appointment scheduling, referrals, and care coordination) to social support related (transportation and child care) (Freeman & Rodriguez, 2011; Natale-Pereira, Enard, Nevarez, & Jones, 2011). They may work in healthcare or community-based organizations and have qualifications ranging from trained lay navigators to licensed professionals, such as nurses and social workers. Navigators with strong ties to the community, such as CHWs, or promotores de salud, have a unique opportunity to build patient trust by demonstrating their knowledge and respect for cultural and linguistic differences and to extend that trust to the larger health system (Carroll et al., 2010; Han, Lee, Kim, & Kim, 2009; Petereit et al., 2008).
Initial evidence suggests that patient navigation may help remove specific barriers to timely, evidence-based primary care among vulnerable populations, which may, in turn, influence these patients' PCR-ED utilization. For example, some studies demonstrate that repeat ED users have periodic contact with primary care physicians but may return to EDs because they have poor experiences or encounter access problems in other settings (Sarver et al., 2002; Weber et al., 2005; Zuckerman & Shen, 2004). Patient navigation has been shown to be potentially useful in linking vulnerable patients to appropriate medical and support services, reducing disruptions in care, and increasing patient satisfaction (Freeman & Rodriguez, 2011; Solberg, Asche, Fontaine, Flottemesch, & Anderson, 2011). Therefore, a patient navigation program may improve actual and perceived access to care and prevent or reduce PCR-ED utilization.
Other published studies focus on patient navigation as a mechanism to reduce visits among frequent PCR-ED users who have substantial psychosocial challenges and often require comprehensive clinical case management; interventions for these challenges are usually facilitated by nurses or social workers. For example, one intensive case management pilot study, implemented by a psychiatric social worker, was associated with significant reductions in ED and acute inpatient hospital services utilization and with reductions in psychosocial problems among frequent ED users over a 12-month pre/post period (Okin et al., 2000). Another study, which considered patients with chronic or complex medical conditions, demonstrated similar reductions in ED use (Pope, Fernandes, Bouthillette, & Etherington, 2000). A large study by Roby et al. (2010) found that patients who received case management through medical homes were less likely that those who did not receive it to have any ED visits or multiple ED visits over an observation period of 16 to 19 months. In a controlled study comparing case management with usual care among frequent ED users, researchers found that ED utilization decreased over time for all patients (measured at 6-month intervals over a 24-month study period), but intervention patients had fewer ED visits than did nonintervention patients over the observation period (Shumway, Boccellari, O'Brien, & Okin, 2008).
Our study contributes to the literature in three important ways. First, it describes the implementation of an ED-based intervention that employs CHWs to address PCR-ED utilization among culturally and linguistically diverse Medicaid and uninsured patients. As such, it teases out the impact of CHW-facilitated patient navigation from more comprehensive clinical case management. Second, it evaluates the impact of patient navigation using intervention and comparison groups, which enables us to differentiate potentially confounding effects associated with uncontrolled studies. Third, it examines the intervention's impact on the odds of any post-observation PCR-ED visits taking place for the study populations and the changes in pre/post utilization among patients with post-observation visits while stratifying participants by their pre-observation period behavior. We hypothesize that by using CHWs as PNs to effectively connect uninsured and Medicaid patients with medical homes and other support resources, PCR-ED utilization among target populations will decrease.
The Memorial Hermann ED-Based Patient Navigation Program
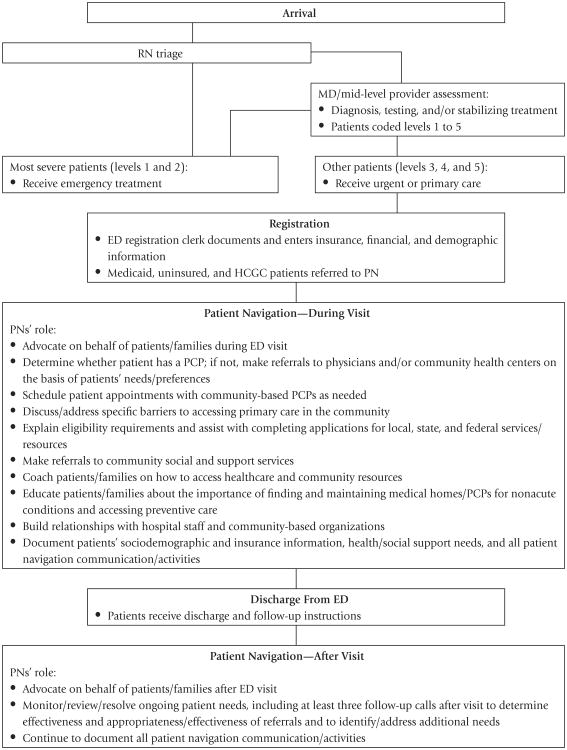
The ED-based patient navigation program under study was developed by the Memorial Hermann Community Benefits Corporation in November 2008 as a performance improvement initiative in its largest hospital, MH-TMC. Prospective patients for the intervention are initially identified during the ED triage process. Arriving patients are coded by ED clinical staff according to acuity level, from 1 to 5, with levels 1 and 2 reflecting the most severe injuries and conditions and levels 4 and 5 reflecting conditions that require medical decisions of minimal to low complexity. Patients coded as level 3 require medical decisions of moderate complexity but may be considered primary care patients as well.
After arriving patients have been triaged and all stabilizing care has been delivered, ED registration clerks meet with patients to record insurance, financial, sociodemographic, and other relevant information. Patients who meet the referral criteria for the navigation program are flagged for intervention. This information, along with the location of the patient, is monitored via the ED tracking board by the PNs, who are bilingual, state-certified CHWs trained in peer-to-peer counseling. The PNs determine the most appropriate time during the visit to initiate navigation.
Using a standard set of questions, the PNs engage the patients or clients to identify and understand the specific barriers to appropriate primary care utilization (e.g., lack of insurance, lack of financial resources) and to begin to determine local, state, and federal resources that can support the clients' needs. For example, the PNs ask the clients if they have a medical home, primary care doctor, or clinic to call or visit for medical reasons. If the clients respond in the negative, the PNs offer to connect them with providers in the clients' neighborhood who accept their insurance or who charge uninsured patients on a sliding fee scale. Initially, the PNs ask about problems the clients may be experiencing related to accessing providers (e.g., office hours or appointment wait times that fail to meet the clients' needs) and about medical conditions for which the clients may need referrals (e.g., pregnancy, diabetes, asthma). Then, the PNs document and tailor the intervention on the basis of the clients' responses. Additionally, the PNs educate the clients about the importance of making and keeping appointments and receiving preventive healthcare, and they provide contact information for future questions and concerns. For quality assurance, the most experienced PN and the designated team leader monitor and coach the PNs as needed to ensure the quality and consistency of the intervention. Program data are aggregated and reviewed during biweekly team meetings to help flag potential problems and identify areas for improvement.
After the clients' discharge from the ED, the PNs follow up with them within 3 to 10 days to monitor the success of the referral, review next steps, and assist with additional support needs. Additionally, the PNs proactively engage with community-based providers, such as federally qualified health centers, to nurture positive referral relationships and maintain updated information about each provider. This continual interaction helps improve the match between clients and prospective medical homes and other resources.
The estimated annual costs for the ED-based patient navigation program at MH-TMC are approximately $45,880 (annual salary and fringe benefits for one full-time CHW). Based on an average cost per PCR-ED visit of $400, an annual reduction of 115 PCR-ED visits is required to cover the costs of the intervention.
Methods
In this study, we used administrative data initially collected to facilitate monitoring and improvement of the patient navigation program. For this reason, the University of Texas MD Anderson Cancer Center Institutional Review Board determined that our evaluation of existing data, deidentified for the purposes of research, was exempt under Category 4 from full committee review, which is the standard process for the approval of research involving human subjects.
The protocol for the intervention is illustrated in Figure 1. Patients eligible for referral to the program are those older than 18 months and younger than 65 years who frequently use the ED for primary care and are publicly insured (Medicaid); uninsured/self-pay; or covered by the Harris County Gold Card (HCGC), a Texas public health benefit that subsidizes medical costs for eligible residents.
Figure 1. Navigation Process for Target Primary Care–Related Emergency Department Patients.
Study design
To examine our research questions, we used a nonequivalent comparison group, quasi-experimental study design (Grembowski, 2001). This design included pretest and posttest (pre/post) observations at 12 and 24 months for the intervention group and a nonrandomized control group with similar characteristics. We abstracted internal administrative data retrospectively for all MH-TMC patients who received navigation during the observation period (intervention group) as well as for patients who were eligible for but did not receive the intervention during the observation period (comparison group). Participant utilization data included visits to any of the nine Memorial Hermann EDs in the Houston area. Eligible participants were contacted in person by the PNs at MH-TMC on Monday through Friday from 11:00 a.m. to 7:00 p.m.
Because the patient navigation program was initiated as a performance improvement project, patients were not formally recruited and few eligible participants refused the intervention. Participants were approached during each PCR-ED visit and may have received the intervention multiple times. The PNs attempted to follow up with eligible participants by phone when the intervention was not delivered in person. We included in the comparison group the eligible participants who were not reached in person or by phone. These patients usually visited the ED when the PNs were not there, when ED volume reached a level that prevented the PNs from seeing all eligible participants, and/or when the patients failed to provide an accurate phone number or respond to messages.
Data analyses
The key outcomes of interest in our study included (1) a dichotomous variable representing the odds ratio (OR) of having any (>0) post-observation PCR-ED visit and, conditional on having any post-observation visit, (2) a continuous measure of mean visits as well as (3) a continuous measure of cost per person. The primary regressor of interest is receipt of the intervention, compared with usual care (no intervention) for the comparison group.
We analyzed basic descriptive statistics for each variable of interest, estimated the unadjusted OR of PCR-ED use during the post-observation period for intervention versus comparison participants, and calculated unadjusted pre/post mean visits and costs at 12 and 24 months among patients with post-observation PCR-ED use. To facilitate cost comparisons across intervention and control groups, we constructed a variable representing the pre/post difference in cost per person by dividing the pre/post difference in total costs by the patient sample size (n) based on pre-observation visit frequency. Finally, we compared differences between pre/post visits and costs within and across intervention and comparison groups. We compared 95% confidence intervals for each outcome to determine if they were significantly different at the p <.05 level. We used Stata 10.1 to facilitate data management and statistical analyses (StataCorp, 2008).
Results
Characteristics of our study sample (N = 13,642), which included participants with complete pre/post data from November 2008 to April 2011, are presented in Table 1. Among participants in the intervention group (n = 1,905), 16.7% were white, 58.0% black, 23.1% Hispanic, and 2.2% another race/ethnicity. More than half (59.9%) of navigated patients were 18–34 years old, while 28.1% were 35–49 years old and 12.0% were 50–64 years old. Females made up the majority (59.5%) of the intervention group. Most navigated patients were uninsured (78.6%); 21.4% of patients in the intervention group were covered by Medicaid. The characteristics of the comparison group (n = 11,737) were similar, except that a small majority of the comparison sample (60.1%) were uninsured.
Table 1. Select Participant Characteristics1.
| Intervention | Comparison | Total | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n = 1,905 | % | n = 11,737 | % | n = 13,642 | % | |
|
|
||||||
| Race/ethnicity | ||||||
| White | 31 9 | 16.7 | 2,092 | 17.9 | 2,411 | 17.7 |
| Black | 1,104 | 58.0 | 6,879 | 58.9 | 7,983 | 58.8 |
| Hispanic | 4 41 | 23.1 | 2,129 | 18.2 | 2,570 | 18.9 |
| Other | 41 | 2.2 | 579 | 5.0 | 620 | 4.6 |
| Age | ||||||
| 18–34 years | 1,141 | 59.9 | 6,816 | 58.4 | 7,957 | 58.6 |
| 35–49 years | 535 | 28.1 | 3,120 | 26.7 | 3,655 | 26.9 |
| 50–64 years | 229 | 12.0 | 1,743 | 14.9 | 1,972 | 14.5 |
| Gender | ||||||
| Male | 772 | 40.5 | 4,284 | 36.7 | 5,056 | 37.2 |
| Female | 1,133 | 59.5 | 7,393 | 63.3 | 8,526 | 62.8 |
| Insurance status | ||||||
| Uninsured | 1,498 | 78.6 | 7,024 | 60.1 | 8,522 | 62.7 |
| Medicaid | 407 | 21.4 | 4,655 | 39.9 | 5,062 | 37.3 |
Includes navigated MH-TMC primary care–related ED patients with complete 12-month pre-observation/post-observation data for the period November 2008 to April 2011.
Given that many ED patients are not repeat or frequent users and may, in fact, have not used PCR-ED services previously, we focused our analyses on five subsets of navigated patients who had 1+, 2+, 3+, 4+, and 5+ PCR-ED visits 12 and 24 months prior to the intervention. These subsets were not mutually exclusive (i.e., the 2+ pre-intervention group was a subset of the 1+ pre-intervention group, the 3+ group was a subset of the 1+ and 2+ groups, and so on).
Among intervention group participants, 46.4% of patients with 1+ PCRED visits and 36.0% of patients with 2+ visits in the 12-month pre-intervention period did not return to a Memorial Hermann ED in the 12-month post-observation period (Table 2). Similar reductions were observed in intervention group patients with more frequent 12- and 24-month pre-intervention visits, but the pre/post percentage changes in the number of patients progressively diminished. This pattern was also observed in the comparison group.
Table 2. Intervention and Comparison Participants, by Pre-intervention Visit Frequency and Unadjusted Odds of returning to Ed during 12- and 24-Month Post-observation Periods.
| Intervention Group | Comparison Group | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Visits, Pre-period | Pre | Post | % Change | Pre | Post | % Change | Odds Ratio |
| 12 Months | |||||||
| 1+ | 6 81 | 365 | −46.4% | 4,625 | 2,686 | −41.9% | 0.83*** (.71, .98) |
| 2+ | 31 7 | 203 | −36.0% | 2,300 | 1,635 | −28.9% | 0.72** (.57, .93) |
| 3+ | 1 61 | 125 | −22.4% | 1,365 | 1,085 | −20.5% | 0.90 (.60, 1.3) |
| 4+ | 86 | 73 | −15.1% | 888 | 756 | −14.9% | 0.98 (.52, 1.8) |
| 5+ | 58 | 52 | −10.3% | 634 | 5 71 | −9.9% | 0.96 (.39, 2.3) |
| 24 Months | |||||||
| 1+ | 850 | 51 4 | −39.5% | 6,355 | 4,683 | −26.3% | 0.55* (.47, .63) |
| 2+ | 470 | 339 | −27.9% | 4,267 | 3,621 | −15.1% | 0.46* (.37, .57) |
| 3+ | 290 | 2 21 | −23.8% | 3,235 | 2,937 | −9.2% | 0.32* (.24, .44) |
| 4+ | 190 | 157 | −17.4% | 2,657 | 2,503 | −5.8% | 0.29* (.19, .44) |
| 5+ | 125 | 10 9 | −12.8% | 2,354 | 2,244 | −4.7% | 0.31* (.17, .54) |
p < .001.
p < .01.
p < .05.
The unadjusted odds associated with having a post-observation visit within 12 or 24 months are also presented in Table 2. At 12 months, the intervention was associated with significantly lower unadjusted odds of having any post-observation PCR-ED visit among patients with the fewest pre-intervention visits. For example, in contrast to the comparison group, intervention group patients with 1+ and 2+ PCR-ED visits in the 12-month pre-observation period had 17% (OR [odds ratio]: 0.83, p < .05) and 28% (OR: 0.72, p < .01) lower odds, respectively, of having a post- observation visit. At 24 months, the intervention was associated with significantly lower unadjusted odds of having any post-observation PCR-ED visit for all patients, regardless of pre- observation visit frequency.
Mean PCR-ED visits, total visits, total costs, cost per person, and pre/post differences for the intervention and comparison groups are presented in Table 3.
Table 3. Visits and Costs at 12 and 24 Months for Participants Returning to ED During Post-period, by Pre-period Visit Frequency.
| Intervention Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Pre-period | Post-period | Pre/Post Differences | |||||||||
|
|
|
|
|||||||||
| Visits, Pre-period | n | Mean Visits (95% CI) | Total Visits | Total Costs | Mean Visits (95% CI) | Total Visits | Total Costs | Mean Visits | Total Visits | Total Costs | Cost per Person |
| 12 Months | |||||||||||
| 1+ | 365 | 3.8 (3.5, 4.1) | 1,377 | $550,800 | 2.9 (2.6, 3.3) | 1,075 | $430,000 | −0.9* | −302 | −120,800 | −$331 |
| 2+ | 203 | 5.2 (4.7, 5.7) | 1,053 | $421,200 | 3.7 (3.1,4.2) | 745 | $298,000 | −1.5* | −308 | −123,200 | −$607 |
| 3+ | 125 | 6.5 (5.9,7.3) | 819 | $327,600 | 4.4 (3.6, 5.2) | 551 | $220,400 | −2.1* | −268 | −107,200 | −$858 |
| 4+ | 73 | 8.4 (7.4, 9.4) | 611 | $244,400 | 5.5 (4.3, 6.7) | 402 | $160,800 | −2.9* | −209 | −83,600 | −$1,145 |
| 5+ | 52 | 9.7 (8.5, 11.0) | 506 | $202,400 | 6.3 (4.8, 7.8) | 328 | $131,200 | −3.4* | −178 | −71,200 | −$1,369 |
| 24 Months | |||||||||||
| 1+ | 514 | 4.4 (4.1,4.8) | 2,280 | $912,000 | 3.9 (3.5, 4.4) | 2,014 | $805,600 | −0.5 | −266 | −$106,400 | −$207 |
| 2+ | 339 | 5.7 (5.3, 6.1) | 1,930 | $772,000 | 4.7 (4.0, 5.3) | 1,581 | $632,400 | −1.0 | −349 | −$139,600 | −$412 |
| 3+ | 221 | 7.1 (6.5,7.7) | 1,576 | $630,400 | 5.6 (4.7, 6.5) | 1,234 | $493,600 | −1.5 | −342 | −$136,800 | −$619 |
| 4+ | 157 | 8.4 (7.7,9.1) | 1,320 | $528,000 | 6.6 (5.4, 7.8) | 1,031 | $412,400 | −1.8 | −289 | −$115,600 | −$736 |
| 5+ | 109 | 9.9 (9.0, 10.8) | 1,080 | $432,000 | 7.6 (6.0, 9.1) | 825 | $330,000 | −2.3 | −255 | −$102,000 | −$936 |
| 12 Months | |||||||||||
| 1+ | 2,686 | 3.5 (3.3, 3.6) | 9,291 | $3,716,400 | 3.5 (3.3, 3.6) | 9,312 | $3,724,800 | 0.0 | +21 | $8,400 | $3 |
| 2+ | 1,635 | 5.0 (4.8, 5.3) | 8,240 | $3,296,000 | 4.4 (4.1,4.6) | 7,127 | $2,850,800 | −0.6* | −1,113 | −$445,200 | −$272 |
| 3+ | 1,085 | 6.6 (6.3, 6.9) | 7,140 | $2,856,000 | 5.3 (5.0, 5.6) | 5,723 | $2,289,200 | −1.3* | −1,417 | −$566,800 | −$522 |
| 4+ | 756 | 8.1 (7.8, 8.5) | 6,153 | $2,461,200 | 6.2 (5.8, 6.6) | 4,714 | $1,885,600 | −1.9* | −1,439 | −$575,600 | −$761 |
| 5+ | 571 | 9.5 (9.1,9.9) | 5,413 | $2,165,200 | 6.9 (6.4, 7.3) | 3,925 | $1,570,000 | −2.6* | −1,488 | −$595,200 | −$1,042 |
| 24 Months | |||||||||||
| 1+ | 3,269 | 4.3 (4.1,4.5) | 13,986 | $5,594,400 | 4.7 (4.5, 5.0) | 15,511 | $6,204,400 | 0.4 | +1,525 | $610,000 | $187 |
| 2+ | 2,207 | 5.9 (5.5, 6.2) | 12,924 | $5,169,600 | 5.8 (5.5, 6.1) | 12,833 | $5,133,200 | −0.1 | −91 | −$36,400 | −$16 |
| 3+ | 1,523 | 7.6 (7.2, 8.0) | 11,556 | $4,622,400 | 7.1 (6.6, 7.5) | 10,760 | $4,304,000 | −0.5 | −796 | −$318,400 | −$209 |
| 4+ | 1,089 | 9.4 (8.9, 10.0) | 10,254 | $4,101,600 | 8.4 (7.8, 8.9) | 9,095 | $3,638,000 | −1.0 | −1,159 | −$463,600 | −$426 |
| 5+ | 830 | 11.1 (10.4, 11.8) | 9,218 | $3,687,200 | 9.5 (8.8, 10.2) | 7,897 | $3,158,800 | −1.6* | −1,321 | −$528,400 | −$637 |
p < .05.
Intervention Group
For all intervention group subsets in the 12-month observation period, mean PCR-ED visits declined significantly in the corresponding post-observation period. Differences in pre/post visits ranged from an average of 0.9 fewer visits when including all patients with 1+ pre-intervention PCRED visits to an average of 3.4 fewer visits when including only patients with 5+ pre-intervention visits. Associated pre/post declines in mean costs per person ranged from −$331 among patients in the 1+ pre-intervention visit subset to −$1,369 in the 5+ pre- intervention visit subset. Estimated values for all subsets indicated pre/post reductions in visits, and associated costs in the intervention group were sufficient to achieve breakeven. Differences in mean visits were not significant in the 24-month subsets.
Comparison Group
Among comparison participants, 12-month pre/post mean PCR-ED visits also declined significantly in the corresponding post-intervention period, with the exception of participants in the 1+ pre-observation visit subset. In this group, differences in pre/post observation visits ranged from zero (when including all patients with 1+ pre-observation PCR-ED visits) to an average of 2.6 fewer visits (when including only patients with 5+ pre-observation visits). Changes in associated cost per person ranged from +$3 in the 1+ to –$1,042 in the 5+ pre-observation visit subsets. In all cases, intervention participants were associated with greater reductions in mean visits and cost per person than the reductions seen with comparison participants.
Discussion
The purpose of this study was to examine differences in PCR-ED visits over time for Medicaid and uninsured patients who received ED-based patient navigation, which was delivered by CHWs and designed to promote appropriate primary care use and reduce PCR-ED utilization. We found that in our target population the patient navigation intervention was associated with significantly lower odds of having any post-observation period visits for less frequent users in the 12-month pre/post period and for all users in the 24-month pre/post period. These results indicate that, over short periods, CHWs may be effective in intervening early with patients who use PCR-ED services less frequently and, over long periods, CHWs may play some role in preventing PCR-ED use.
Additionally, we found that when limiting our analysis to participants with PCR-ED visits during the 12-month post-observation period, mean PCR-ED visits declined significantly among intervention participants (as well as among the comparison group), regardless of pre-intervention visit frequency, with the exception of comparison participants in the 1+ pre-observation visit subset. We observed greater declines in mean visits and associated costs per person among intervention group participants compared to comparison participants during the 12-month pre/post period, but we did not observe similar declines in the 24-month pre/post period. This finding suggests that among repeat users, the impact of the intervention on reducing PCR-ED visits is not sustained over long periods.
Finally, we found that the intervention was associated with reduced PCR-ED costs or cost savings. These cost savings were greater than the costs to implement the program, which demonstrates that an ED-based navigation program led by CHWs is cost-effective for Memorial Hermann. Our study, however, did not control for clinical or psychosocial characteristics of study participants. Many persistent PCR-ED users present with chronic or complex health conditions and behaviors that require intensive case management by licensed nurses, social workers, or other CHW professionals. Therefore, healthcare managers must consider the characteristics of the population being targeted—including patients' clinical, cultural, linguistic, and socioeconomic diversity—as well as the perspectives of clinicians and administrators within their organizations in designing and implementing patient navigation. Further investigation is warranted to better predict which patient populations can most effectively be served by CHW PNs.
Limitations
Several limitations must be considered when interpreting the results of this research. First, while our study included a comparison group (an improvement on pre-experimental research designs), it was not a randomized controlled trial and therefore did not rule out all threats to internal validity (Campbell & Stanley, 1963; Grembowski, 2001). While we believe the intervention participants were similar to those in the comparison group, it is possible that unmeasured, systematic differences in the selection of the groups exist that account for differences in outcomes between the two groups. If present, this selection threat may be magnified by interacting with other threats to internal validity. For example, patients might have discontinued visits to the Memorial Hermann EDs in Houston but continued to seek PCR-ED care at other local EDs, or they might have died during the study period. This factor would affect post-observation results if it occurred more frequently among the intervention group than comparison group participants. Regression to the mean also is a concern when selection threats are present. In this study, however, comparison group participants began with statistically similar pre-observation period mean visits and therefore had equal opportunity to regress to the mean. That pre/post visits decreased more among intervention than comparison participants suggests the intervention had some impact on the outcomes.
Second, challenges in the navigation process may have affected the results. For example, a goal of the ED is efficiency in the triage, treatment, and discharge processes. During peak demand periods, the PNs may have less time to spend with patients prior to discharge, or they may miss the opportunity to navigate some patients altogether. These factors may have affected the overall effectiveness or consistency of the intervention.
Third, MH-TMC serves a high proportion of immigrants, who are fearful of divulging accurate personal information, and other patients do not provide adequate contact information due to billing concerns. These issues persist despite assurances that the information requested is for navigation and follow-up only and therefore negatively affect the PNs' effectiveness both during and after the ED visit. Finally, differences in experiences and competency strengths of the PNs may also lead to variability in the results.
The program's sole focus on Medicaid, uninsured, and HCGC-covered patients aged less than 65 years in a hospital ED setting impedes our ability to generalize the results to other patient populations in other settings. In addition, while Houston is a diverse market reflective of many large urban cities across the United States, health policies and practices vary at the local and state levels. These factors may affect the generalizability of the intervention to other markets inside and outside the United States.
Future research
Since 2008, Memorial Hermann has piloted the patient navigation program in four of its nine EDs in the Houston area. In addition to its implementation at MH-TMC, the program has been implemented at MH–Northwest Hospital and was returned to MH–Southwest Hospital in August 2011. Outcomes at these facilities are similar to those at MH-TMC. The program was also active in MH–Northeast Hospital until it was discontinued due to lack of hospital support.
To continue improving the design and effectiveness of the intervention, we have collected focus group and survey data to investigate individual-and system-level factors that drive PCR-ED use among the target population. These factors include clinical and psychosocial characteristics of frequent PCR-ED users and actual and perceived barriers to medical homes and appropriate primary care utilization. Our findings will aid the refinement of the existing intervention. Additionally, Memorial Hermann is establishing a pilot project with local federally qualified health centers—which have agreed to serve as medical homes for the target population—to increase primary care access and improve the monitoring of frequent PCR-ED users. Our future research will establish collaborations with a wider network of providers to enable us to evaluate the cost- effectiveness of the intervention for the local health system.
Conclusion
The ability to identify effective and sustainable methods to address poorly coordinated care and inappropriate healthcare utilization, particularly for medically underserved populations, will become increasingly critical as the demand for services increases in the era of healthcare reform. The findings from this study, while preliminary, suggest that CHW-led patient navigation should be explored as a potential tool to reduce PCR-ED visits among vulnerable populations.
Acknowledgments
Dr. Kimberly R. Enard was partially supported by the University of Texas School of Public Health Cancer Education and Career Development Program–National Cancer Institute (NCI)/National Institutes of Health (NIH) [Grant 2 R25 CA57712] and the W.K. Kellogg Foundation [Grant P0117943] via the Center for Advancing Health for the Kellogg Health Scholars Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI, NIH, W.K. Kellogg Foundation, or Center for Advancing Health.
Contributor Information
Kimberly R. Enard, University of Texas School of Public Health, Houston, Texas.
Deborah M. Ganelin, Community Benefit Corporation, Memorial Hermann Health System, Houston, Texas.
References
- Begley C, Courtney P, Brau K. Houston hospitals emergency department use study. Houston, TX: University of Texas Health Science Center School of Public Health; 2012. [Google Scholar]
- Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: A substitute for primary care? New York, NY: NYU Center for Health and Public Service Research; 2000. [PubMed] [Google Scholar]
- Campbell D, Stanley J. Experimental and quasi-experimental designs for research. Boston, MA: Houghton Mifflin; 1963. [Google Scholar]
- Carroll JK, Humiston SG, Meldrum SC, Salamone CM, Jean-Pierre P, Epstein RM, Fisella K. Patients' experiences with navigation for cancer care. Patient Education and Counseling. 2010;80(2):241–247. doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohan D, Schrag D. Using navigators to improve care of under-served patients: Current practices and approaches. Cancer. 2005;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(S15):3537–3540. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia T, Bernstein A, Bush M. Emergency department visitors and visits: Who used the emergency room in 2007? Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- Grembowski D. The practice of health program evaluation. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Han H, Lee H, Kim M, Kim K. Tailored lay health worker intervention improves breast cancer screening outcomes in non-adherent Korean-American women. Health Education Research. 2009;24(2):318–329. doi: 10.1093/her/cyn021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: Causes, effects, and solutions. Annals of Emergency Medicine. 2008;52(2):126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natale-Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating health disparities. Cancer. 2011;117(S15):3541–3550. doi: 10.1002/cncr.26264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okin RL, Boccellari A, Azocar F, Shumway M, O'Brien K, Gelb A, et al. Wachsmuth C. The effects of clinical case management on hospital service use among ED frequent users. American Journal of Emergency Medicine. 2000;18(5):603–608. doi: 10.1053/ajem.2000.9292. [DOI] [PubMed] [Google Scholar]
- Paskett ED, Harrop JP, Wells KJ. Patient navigation: An update on the state of the science. CA: A Cancer Journal for Clinicians. 2011;61(4):237–249. doi: 10.3322/caac.20111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petereit DG, Molloy K, Reiner ML, Helbig P, Cina K, Miner R, et al. Roberts CR. Establishing a patient navigator program to reduce cancer disparities in the American Indian communities of western South Dakota: Initial observations and results. Cancer Control. 2008;15(3):254–259. doi: 10.1177/107327480801500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen LA, Burstin HR, O'Neil AC, Orav EJ, Brennan TA. Non-urgent emergency department visits: The effect of having a regular doctor. Medical Care. 1998;36(8):1249–1255. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- Petterson S, Rabin D, Hillips R, Bazemore A, Dodoo M. Having a usual source of care reduces ED visits. American Family Physician. 2009;79(2):94. [PubMed] [Google Scholar]
- Pope D, Fernandes CM, Bouthillette F, Etherington J. Frequent users of the emergency department: A program to improve care and reduce visits. Canadian Medical Association Journal. 2000;162(7):1017–1020. [PMC free article] [PubMed] [Google Scholar]
- Roby DH, Pourat N, Pirritano MJ, Vrungos SM, Dajee H, Castillo D, Kominski GF. Impact of patient-centered medical home assignment on emergency room visits among uninsured patients in a county health system. Medical Care Research and Review. 2010;67(4):412–430. doi: 10.1177/1077558710368682. [DOI] [PubMed] [Google Scholar]
- Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Academic Emergency Medicine. 2002;9(9):916–923. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- Schoen C, Osborn R, Huynh P, Doty M, Davis K, Zapert K, Peugh J. Primary care and health system performance: Adults' experiences in five countries. Health Affairs. 2004:w4-487–w4-503. doi: 10.1377/hlthaff.w4.487. Web Exclusive. [DOI] [PubMed] [Google Scholar]
- Shumway M, Boccellari A, O'Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: Results of a randomized trial. American Journal of Emergency Medicine. 2008;26(2):155–164. doi: 10.1016/j.ajem.2007.04.021. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Asche SE, Fontaine P, Flottemesch TJ, Anderson LH. Trends in quality during medical home transformation. Annals of Family Medicine. 2011;9(6):515–521. doi: 10.1370/afm.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata 10.1. College Station, TX: StataCorp; 2008. [Google Scholar]
- Texas Hospital Association (THA) 2012–2013 fast facts on Texas hospitals. 2012 Retrieved from http://www.tha.org/HealthCareProviders/Advocacy/Hospital%20Facts.pdf.
- Vargas RB, Ryan GW, Jackson CA, Rodriguez R, Freeman HP. Characteristics of the original patient navigation programs to reduce disparities in the diagnosis and treatment of breast cancer. Cancer. 2008;113(2):426–433. doi: 10.1002/cncr.23547. [DOI] [PubMed] [Google Scholar]
- Weber EJ, Showstack JA, Hunt KA, Colby DC, Callaham ML. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Annals of Emergency Medicine. 2005;45(1):4–12. doi: 10.1016/j.annemergmed.2004.06.023. [DOI] [PubMed] [Google Scholar]
- Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Affairs. 2010;29(9):1630–1636. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient Navigation Research Program. Patient navigation: State of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: Do insurance coverage and access to care matter? Medical Care. 2004;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]