Abstract
Objectives
Using population-based data, we document the comorbidities (medical, neurologic and psychiatric) and consequences for daily functioning of excessive quantity of sleep (EQS), defined as a main sleep period or 24-hour sleep duration ≥9 hours accompanied by complaints of impaired functioning or distress due to excessive sleep, and its links to excessive sleepiness.
Methods
A cross-sectional telephone study using a representative sample of 19,136 non-institutionalized individuals living in the United States, aged ≥18 (participation rate: 83.2%). The Sleep-EVAL expert system administered questions on life and sleeping habits; health; and sleep, mental and organic disorders (DSM-IV-TR, ICSD-II, ICD-10).
Results
Sleeping at least 9 hours per 24-hour period was reported by 8.4% (95% confidence intervals: 8.0%-8.8%) of participants; EQS (prolonged sleep episode with distress/impairment) was observed in 1.6% (1.4% to 1.8%) of the sample. The likelihood of EQS was 3-12 times higher among individuals with a mood disorder. EQS individuals were 2-4 times more likely to report poor quality of life than non-EQS individuals as well as interference with socio-professional activities and relationships. Although between 33% and 66% of individuals with prolonged sleep perceived it as a major problem, only 6.3% to 27.5% of them reported having sought medical attention.
Interpretation
Excessive Quantity of Sleep is widespread in the general population, co-occurring with a broad spectrum of sleep, medical, neurologic and psychiatric disorders. Therefore, physicians must recognize EQS as a mixed clinical entity indicating careful assessment and specific treatment planning.
Introduction
Excessive Sleepiness can be 1) an essential feature for Hypersomnia Disorders and Narcolepsy; 2) an associated feature of Obstructive Sleep Apnea Syndrome, Circadian Rhythm Sleep Disorder; 3) a consequence of insomnia disorder or sleep deprivation, or 4) a side effect of treatment. 1,2 Therefore, trying to disentangle the role of each disease or disorder is complex yet critical for both epidemiologic and clinical purposes.
In 20083, Excessive Sleepiness was defined as constituted by two main symptoms: 1) an Excessive Quantity of Sleep (EQS), defined as a prolonged main sleep period or the presence of napping, and 2) a Deteriorated Quality of Wakefulness (DQW), defined as episodes of excessive somnolence at inappropriate times. Consequently, to better understand excessive sleepiness, it is necessary to evaluate the impact and consequences of these two main symptoms.
Epidemiological studies assessing EQS were based on a subjective evaluation that asked participants if they were “getting too much sleep” or “sleeping too much” without correlating the answer with a reported sleep duration. The studies also omitted critical and clinically relevant information about symptom severity and duration. Consequently, it is not surprising to observe conflicting results with respect to estimates of prevalence, co-morbid conditions and functional consequences of EQS.3 On the other hand, some studies have examined the effects of long sleep on mortality and various organic conditions and reported higher mortality risks among long sleepers.4 Whether long sleep increases the risk of developing some organic conditions is unclear, since conflicting results have been reported for the most commonly studied diseases such as cardiovascular diseases, diabetes and hypercholesterolemia.5-8
The distinction between EQS and long sleep is subtle but critical: Long sleep is a duration category defined by the clinician or researcher with the cutoff point varying from greater than 8 hours to greater than 10 hours. EQS is defined as a long sleep, which bothers or distresses an individual in his/her daily life.
The DSM-5 Task Force is currently working on a new version of its manual. Substantial changes are being made to improve the definition and diagnostic identification of Hypersomnia Disorders, which will be renamed Hypersomnolence Disorders.
Therefore, this study aims to document 1) the prevalence of excessive quantity of sleep in a large representative sample of the adult U.S. general population using the criteria proposed for the DSM-5 9; 2) the medical and neurologic diseases, sleep and mental disorders co-occurring with excessive quantity of sleep; 3) the daytime consequences of excessive quantity of sleep and 4) the link between EQS and DQW.
Methods
Sample
Fifteen states were selected to represent the U.S. population based on the number of inhabitants and the geographical area: Arizona, California, Colorado, Florida, Idaho, Missouri, New York, North Carolina, North Dakota, Oregon, Pennsylvania, South Dakota, Texas, Washington and Wyoming. The final sample included 19,136 individuals representative of the general population of these states (138 million of inhabitants). Of 19,136 eligible adults, 15,929 completed interviews, thus providing an 83.2% cooperation rate, which is considered excellent by CASRO (Council of American Survey Research Organizations) standards.
Procedures
We first retrieved telephone numbers in proportion to the population size of each county in the represented states. Telephone numbers were randomly selected within each state using a computerized residential phone book. Second, during the telephone contact, the Kish method 10 was used to select one respondent per household. This method allowed for the selection of a respondent based on age and gender to maintain a sample representative of these two parameters.
Interviewers explained the goals of the study to potential participants and requested verbal consent before conducting the interview. The participants had the option of calling the principal investigator if they wanted further information. The study was approved by the Stanford University Institutional Review Board (IRB).
Subjects who declined to participate or who gave up before completing half the interview were classified as refusals. Excluded from the study were subjects who were not fluent in English or Spanish, who suffered from a hearing or speech impairment, or who had an illness (such as dementia or Alzheimer's disease, terminal disease) that precluded being interviewed. The interviews lasted on average 62.1 (±32.2) minutes. An interview could be completed with more than one telephone call when it exceeded 60 minutes or at the request of the participant. As a follow-up, the project manager or team leaders telephoned nearly all the participants who completed the interview to ask, during a span of 6-8 min, a series of random questions related to the interview and satisfaction with the interviewer.
It was required that all the interviewers had no specific background in medicine and related sciences or in psychology. The interviewers were college students or had some college education. The training consisted of five 3-hour sessions that covered the study objectives, ethics in research, use of the Sleep-EVAL software and role-playing for interview situations. Interviewers were supervised by 2 or 3 team leaders with a ratio of 1 team leader for 6 interviewers.
Instrument
We used the Sleep-EVAL knowledge-based expert system to conduct the interviews. 11,12 This computer software and its questionnaire were specially designed by one of the authors (MMO) to conduct epidemiological studies in the general population.
The system is composed of a non-monotonic, level-2 inference engine, two neural networks, a mathematical processor, the knowledge base and the base of facts. Simply put, the interview begins with a series of questions asked of all the participants. Questions are read aloud by the interviewer as they appear on the screen. These questions are either closed-ended (e.g., yes/no, five-point scale, multiple choice) or open-ended (e.g., duration of symptom, description of illness).
Once this information was collected, the system began the diagnostic exploration of mental disorders. On the basis of responses provided by a subject to this questionnaire, the system formulated an initial diagnostic hypothesis that it attempted to confirm or reject by asking supplemental questions or by deductions. Concurrent diagnoses are allowed in accordance with the DSM-IV-TR 1 and the Classification of Sleep Disorders or ICSD-II. 2 The system terminated the interview once all diagnostic possibilities were exhausted.
The differential process is based on a series of key rules allowing or prohibiting the co-occurrence of two diagnoses. The questionnaire of the expert system is designed such that the decision about the presence of a symptom is based upon the interviewee's responses rather than on the interviewer's judgment. This approach has proved to yield better agreement between lay interviewers and psychiatrists on the diagnosis of minor psychiatric disorders.13 The system has been tested in various contexts, in clinical psychiatry and sleep disorders clinics. 14-17 In psychiatry, overall kappa between psychiatrists and the system was 0.71;15 kappas have ranged from 0.44 (schizophrenia disorders) to 0.78 (major depressive disorder). Agreement for insomnia diagnoses was obtained in 96.9% of cases (kappa 0.78). Overall agreement on any breathing-related sleep disorder was 96.9% (kappa 0.94). For excessive sleepiness as a symptom, Kappa between Sleep-EVAL and three sleep specialists ranged from 0.62 to 0.70 with an overall sensitivity of 98.3% and a specificity of 62.5%. For narcolepsy with cataplexy, kappas between sleep specialists on the presence of narcolepsy ranged from 0.83 to 0.93 while kappas between Sleep-EVAL and each sleep specialist were 0.89, 0.93 and 1.0.17
Variables
- Excessive quantity of sleep:
- Subjective estimation of sleeping too much
- Napping: frequency, duration
- Nighttime sleep duration; and total sleep time during a 24-hour period (nighttime sleep + naps)
- Quality of wakefulness:
- Falling easily asleep, period(s) of sudden and uncontrollable sleep
- Duration, severity, frequency in a week and in a day
- Epworth Sleepiness Scale
Medical consultations and impact of excessive quantity of sleep and sleepiness on social and occupational functioning.
- Other variables:
- Sleep/wake schedule: bedtime, wake-up time, sleep latency and extra sleep on weekends and days off
- Pharmacological treatment (name, indication, dose)
- Diagnosed physical diseases as reported by the participants
- Use of drugs, alcohol, tobacco and caffeine
- Health-related quality of life
- DSM-IV-TR psychiatric disorders, ICSD sleep disorders, ICD-10 disorders
- Self-reported race and ethnicity.
-
Criterion A for Hypersomnolence Disorder in the forthcoming DSM-5: 9
The predominant characteristic is a complaint of excessive sleepiness associated with at least one of the following symptoms:- Recurrent periods of irrepressible need to sleep within the same day
- Recurrent naps within the same day
- A non-restorative (unrefreshing) main sleep episode of more than 9 hours per day
- Sleep inertia with difficulty being fully awake
Analyses
A weighting procedure to correct for disparities in geographical, age and sex distributions between the sample and the populations of different states. Results were based on weighted n values and percentages. Using logistic regressions, we computed the odds ratios (OR) associated with excessive quantity of sleep. Reported differences were significant at the 0.01 level or less (determined using the Holm-Bonferroni method for multiple comparisons). 18 SPSS version 19 was used to perform statistical analyses.
Results
From 19,136 solicited individuals, data from 15,929 participants, aged from 18 to 102 years, were included in the analyses. Fifty-nine percent were living in areas with a population density >200 inhabitants per square mile. Women represented 51.3% of the sample.
Nearly 40% of the sample was working on a daytime schedule. Shift work (i.e., working outside regular daytime hours) represented about 20% of the sample.
Distribution of sleep quantity
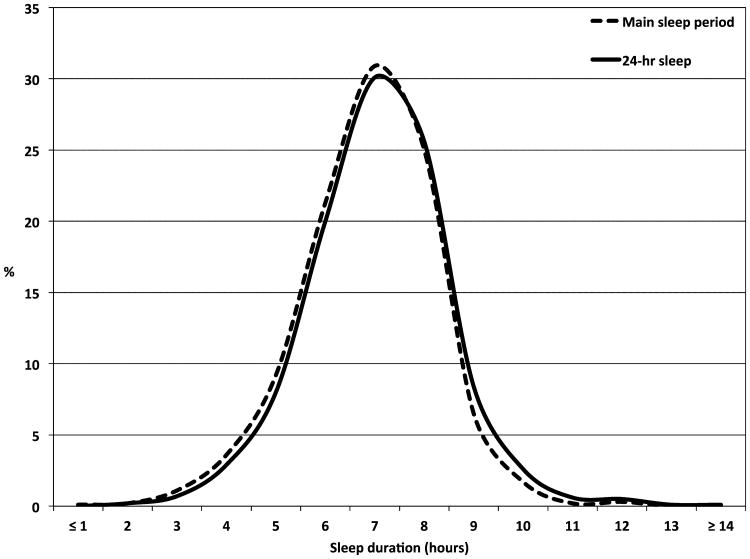
Figure 1 presents the distribution of reported sleep duration for the main sleep episode and for a 24-hour period. As seen, both reported sleep durations are normally distributed with about 75% of the sample sleeping between 6 and 8 hours. The mean sleep duration for the main sleep episode was 6 h 48 min (+/- 1h 23 min). It was 6 h 58 min (+/- 1h 26 min) for the 24-hour sleep duration.
Figure 1. Normal distribution of sleep in the sample.
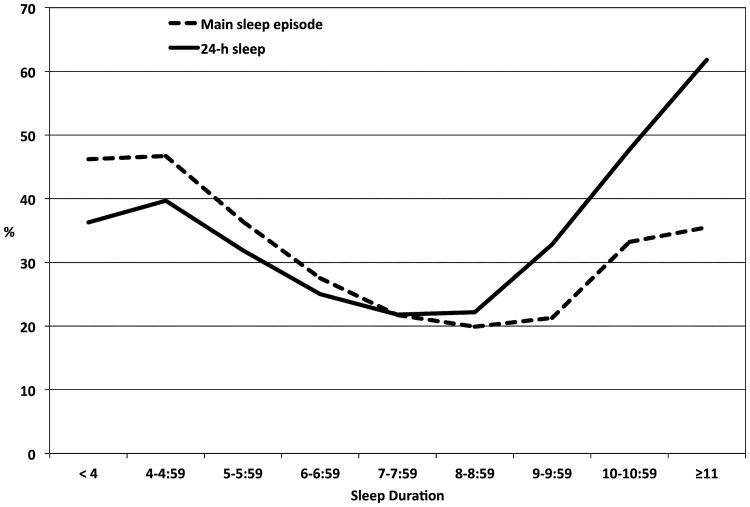
Figure 2 illustrates how the main sleep episode and 24-hour sleep duration were associated with impairment and distress related to deteriorated quality of wakefulness. The curves for both sleep durations have a U-shape, showing that both short and long sleep have repercussions on the functioning of the individuals. As seen, the proportion of impaired individuals markedly increased with both sleep durations of 9 hours or greater (main period of sleep or 24 hours period).
Figure 2. Proportion of individuals with impairment or distress related to deteriorated quality of wakefulness.
A total of 6.3% (5.9%-6.7%) of the sample had a reported sleep duration of 9 hours or greater during the main sleep episode. The prevalence was comparable between men and women (Table 1).
Table 1. Prevalence of excessive quantity of sleep by sociodemographic characteristics.
| Main sleep episode ≥ 9 hours (n= 1,004) | 24 hrssleep ≥ 9 hours (n=1,338) | Sleep impairme ≥ 9 hours with nt/distress (n=255) | |||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| N | % (s.e.) | OR | % (s.e.) | OR | % (s.e.) | OR | |
| Sex | |||||||
| Male | 7755 | 5.9 (0.03) | 1.00 | 7.6 (0.03) | 1.00 | 1.3 (0.01) | 1.00 |
| Female | 8174 | 6.7 (0.03) | 1.10 [0.95-1.28] | 9.2 (0.03) | 1.24 [1.11-1.39]† | 2.0 (0.02) | 1.58 [1.22-2.06]† |
| Age groups | |||||||
| 18-24 | 1980 | 10.5 (0.07) | 1.15 [0.91-1.45] | 13.3 (0.08) | 0.90 [0.74-1.10] | 2.1 (0.03) | 0.94 [0.58-1.54] |
| 25-34 | 2997 | 5.5 (0.04) | 0.64 [0.50-0.81]† | 6.8 (0.05) | 0.46 [0.38-0.57]† | 1.5 (0.02) | 0.69 [0.43-1.11] |
| 35-44 | 3333 | 3.7 (0.03) | 0.38 [0.29-0.49]† | 5.1 (0.04) | 0.33 [0.27-0.41]† | 1.4 (0.02) | 0.68 [0.43-1.07] |
| 45-54 | 2926 | 4.5 (0.04) | 0.47 [0.36-0.60]† | 5.6 (0.04) | 0.37 [0.30-0.46]† | 1.4 (0.02) | 0.81 [0.52-1.27] |
| 55-64 | 1971 | 5.3 (0.06) | 0.53 [0.41-0.70]† | 7.2 (0.06) | 0.48 [0.38-0.60]† | 1.6 (0.03) | 0.83 [0.51-1.36] |
| ≥ 65 | 2721 | 10.1 (0.06) | 1.00 | 14.6 (0.07) | 1.00 | 1.0 (0.03) | 1.00 |
| Race | |||||||
| White | 12361 | 6.3 (0.02) | 1.00 | 8.3 (0.03) | 1.00 | 1.6 (0.01) | 1.00 |
| Black | 1163 | 5.9 (0.08) | 0.91 [0.68-1.23] | 9.0 (0.10) | 1.10 [0.86-140] | 0.9 (0.03) | 0.59 [0.30-1.20] |
| American Indian | 175 | 8.1 (0.24) | 1.35 [0.72-2.52] | 8.9 (0.25) | 1.08 [0.59-1.96] | 3.1 (0.15) | 1.99 [0.74-5.35] |
| Hispanic | 1179 | 5.9 (0.08) | 0.87 [0.65-1.17] | 8.4 (0.09) | 1.01 [0.79-1.29] | 2.2 (0.06) | 1.42 [0.88-2.27] |
| Asian/Pacific | 398 | 3.4 (0.10) | 0.52 [0.28-0.96] | 7.2 (0.15) | 0.85 [0.55-1.33] | 1.7 (0.07) | 1.07 [0.44-2.60] |
| Other race | 653 | 5.2 (0.09) | 0.74 [0.49-1.13] | 8.2 (0.12) | 0.98 [0.72-2.37] | 2.1 (0.06) | 1.30 [0.69-2.48] |
| Occupation* | |||||||
| Daytime worker | 6321 | 4.2 (0.03) | 1.00 | 5.3 (0.03) | 1.00 | 0.9 (0.01) | 1.00 |
| Shift worker | 3168 | 4.7 (0.04) | 1.10 [0.87-1.39] | 5.7 (0.04) | 1.10 [0.89-1.36] | 0.9 (0.02) | 1.21 [0.71-2.06] |
| Unemployed | 634 | 11.8 (0.13) | 2.67 [1.96-3.67]† | 15.9 (0.15) | 3.09 [2.34-4.08]† | 5.1 (0.09) | 8.22 [4.97-13.6]† |
| Homemaker | 2095 | 8.8 (0.06) | 1.97 [1.55-2.51]† | 11.7 (0.07) | 2.24 [1.82-2.76]† | 3.8 (0.05) | 4.68 [3.05-7.18]† |
| Student | 1017 | 7.1 (0.08) | 0.74 [0.51-1.07] | 9.2 (0.09) | 0.81 [0.58-1.12] | 1.4 (0.06) | 1.46 [0.65-3.32] |
| Retired | 2694 | 9.7 (0.06) | 1.98 [1.46-2.70]† | 14.5 (0.07) | 2.24 [1.72-2.91]† | 2.0 (0.03) | 2.82 [1.56-5.08]† |
p<0.001;
p<0.01
OR: Odds ratio
OR adjusted for age and sex
As many as 8.4% (8.0%-8.8%) of participants reported sleeping at least 9 hours per 24-hour period. Women were more likely than men to sleep at least 9 hours per day (Table 1).
Both sleep duration reports, sleeping ≥9 hours per main sleep episode or 24-hour period, were more frequent among the youngest (18-24 years old) and the oldest participants (≥ 65 years old) and were more frequently reported by unemployed persons, homemakers and retired individuals but were unrelated to race.
EQS, defined as a main sleep period or 24-hour sleep duration ≥9 hours accompanied by complaints of impaired functioning or distress due to excessive sleep, was observed in 1.6% (1.4% to 1.8%) of the sample. Significantly more women than men reported a long sleep with consequences but the prevalence did not significantly change with age. After adjusting for age and sex, unemployed persons, homemakers and retired individuals were more likely to have long sleep with consequences than workers.
The prevalence of DSM-IV Hypersomnia Disorder was 0.5% (0.4%-0.6%). Narcolepsy with cataplexy was very rare with a prevalence of 0.038% (six cases).
Association with medical, neurologic and mental disorders
Using logistic regressions to adjust for age and sex, we observed that reported 24-hour sleep duration of 9 hours or more was more prevalent in 5 of 18 organic disorders examined: Cerebrovascular Diseases, Diabetes Mellitus, Disease of the Central Nervous System, Heart Diseases and Diseases of the Musculoskeletal System. Only Heart Diseases were significantly associated with a main sleep episode ≥ 9 hours (Table 2).
Table 2. Associations between excessive quantity of sleep and organic diseases.
| Main sleep episode ≥ 9 hours (n= 1,004) | 24 hrs sleep ≥ 9 hours (n=1,338) | Sleep ≥ 9 hours with impairment/distress (n=255) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| % | AOR [95% CI] | % | AOR [95% CI] | % | AOR [95% CI] | |
| Cerebrovascular diseases | ||||||
| Absent (n=15,579) | 6.1 | 1.00 | 8.2 | 1.00 | 1.6 | 1.00 |
| Present (n=350) | 9.1 | 1.30 [0.85-1.98] | 16.2 | 1.63 [1.16-2.29]f | 4.3 | 2.64 [1.40-4.98]f |
| Diabetes mellitus | ||||||
| Absent (n=15,196) | 6.0 | 1.00 | 8.1 | 1.00 | 1.5 | 1.00 |
| Present (n=733) | 7.8 | 0.80 [0.58-1.10] | 14.2 | 1.64 [1.28-2.11]† | 4.5 | 0.35 [0.22-0.55]† |
| Diseases of the central nervous system | ||||||
| Absent (n=15,754) | 6.1 | 1.00 | 8.3 | 1.00 | 1.6 | 1.00 |
| Present (n=175) | 9.6 | 1.72 [1.00-2.99] | 13.4 | 1.81 [1.12-2.92]f | 1.9 | 2.06 [0.83-5.12] |
| Diseases of the musculoskeletal system & connective tissue | ||||||
| Absent (n=14,241) | 6.0 | 1.00 | 8.0 | 1.00 | 1.4 | 1.00 |
| Present (n=1,688) | 7.1 | 1.28 [1.02-1.60] | 11.0 | 1.46 [1.21-1.76]† | 4.2 | 3.57 [2.60-4.90]† |
| Heart diseases (Diseases of the circulatory system) | ||||||
| Absent (n=15,212) | 5.9 | 1.00 | 7.9 | 1.00 | 1.6 | 1.00 |
| Present (n=717) | 10.2 | 1.50 [1.12-2.02]f | 16.9 | 1.83 [1.43-2.34]† | 3.6 | 2.76 [1.69-4.49]† |
p<0.001;
p<0.01
Non-significant for the three groups: Hypercholesterolaemia; Hypertension; Cerebrovascular Diseases; Diseases of the blood & blood-forming organs; Diseases of the eye & adnexa; Disorders of kidney & ureter; Diseases of the urinary system; Disorders of genital tract; Diseases of the skin & subcutaneous tissue; Upper respiratory tract diseases; Obesity.
AOR: Adjusted Odds Ratios for age and sex
In addition, EQS was more prevalent in Diseases of the Digestive System (Adjusted Odds Ratio (AOR): 1.94 [1.19-3.18]; p< 0.01); Lower Respiratory Tract Diseases (AOR: 3.25 [1.54-6.87]; p< 0.01), Disorders of the Thyroid Gland (AOR: 2.49 [1.59-3.89]; p< 0.001), Hypertension (AOR: 1.79 [1.25-2.56]; p< 0.001) and Malignant Neoplasm (AOR: 4.10 [1.84-9.13]; p<0.001).
Using the same analytic strategies for determining association with mental disorders, prevalence rates of the two sleep durations were significantly higher in Major Depressive Disorder after adjusting for age and sex. Individuals with Bipolar Disorders were two times more likely to report at least 9 hours per main sleep episode and three times more likely to have EQS. Dysthymic Disorder was associated with sleeping at least 9 hours per 24-hour period and EQS (Table 3). Anxiety Disorders, Psychotic Disorders and Eating Disorders were unrelated to prolonged sleep duration.
Table 3.
Associations between excessive quantity of sleep and mental disorders
| Main sleep episode ≥ 9 hours (n= 1,004) | 24 hrs sleep ≥ 9 hours (n=1,338) | Sleep ≥ 9 hours with impairment/distress (n=255) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| % | AOR [95% CI] | % | AOR [95% CI] | % | AOR [95% CI] | |
| Dysthymic Disorder | ||||||
| Absent (n=15,754) | 6.2 | 1.00 | 8.2 | 1.00 | 1.5 | 1.00 |
| Present (n=175) | 8.7 | 1.97 [1.08-3.60] | 17.4 | 3.13 [1.98-4.94]† | 14.6 | 12.69 [7.63-21.1]† |
| Major Depressive | ||||||
| Disorder | ||||||
| Absent (n=15,021) | 6.1 | 1.00 | 8.0 | 1.00 | 1.3 | 1.0 |
| Present (n=908) | 8.3 | 1.56 [1.17-2.07]f | 13.4 | 2.01 [1.60-2.54]† | 7.4 | 6.27 [4.50-8.74]† |
| Bipolar disorders | ||||||
| Absent (n=15,706) | 6.1 | 1.00 | 8.3 | 1.00 | 1.6 | 1.00 |
| Present (n=223) | 12.1 | 2.16 [1.34-3.47]f | 12.4 | 1.59 [0.99-2.57] | 4.6 | 3.31 [1.62-6.76]† |
p<0.001;
p<0.01
Non-significant for the three groups: Psychotic disorders, Cyclothymic disorder; Adjustment disorders; Eating disorders; Obsessive-Compulsive Disorder; Specific phobia; Agoraphobia; Social Anxiety Disorder.
AOR: Adjusted Odds Ratios for age and sex
However, EQS was more prevalent in Generalized Anxiety Disorder (AOR: 4.82 [2.67-8.72]; p < 0.001); Panic Disorder (AOR: 3.62 [2.29-5.73]; p < 0.001); Posttraumatic Stress Disorder (AOR: 3.46 [2.21-5.40]; p<0.001); and Alcohol Abuse/Dependence (AOR: 3.77 [2.35-6.06]; p<0.001).
Finally, individuals with cognitive difficulties (attention, concentration and memory) were more likely to report sleeping at least 9 hours per 24-hour period and EQS, but cognitive difficulties were unrelated to the prolonged duration of the main sleep episode. The adjusted odds ratio for ≥ 9 hours of sleep per 24 hours was 1.26 (95%CI: 1.07-1.47; p=0.005). The adjusted odds ratio for EQS was 4.63 (3.47-6.19; p<0.0001).
Quality of life, social and professional impacts
Among participants who drove a motor vehicle (n=13,376), individuals with EQS more often reported having been involved in a road accident in the previous year when they were the driver than did the rest of the drivers (9.2% vs. 5.5%; AOR: 1.86 [1.06-3.25] p=0.003). Prolonged sleep episode without impairment/distress was not associated with road accident.
Overall, the following three groups were more likely to report poor quality of life (i.e., limitations in accomplishing occupational and/or social activities) compared to the rest of the sample after adjusting for age, sex and the presence of a physical disease: sleeping at least 9 hours per main sleep episode (AOR: 1.23 [1.04-1.45]; p=0.01); sleeping at least 9 hours per 24-hour period (AOR: 1.58 [1.37-1.82]; p<0.0001) and EQS (AOR: 11.03 [8.07-15.08]; p<0.0001). Respectively, 23.3% and 29.9% of individuals sleeping at least 9 hours per main sleep period or 24-hours period reported that sleepiness interfered, at least moderately, with social activities; 13.3% and 19.4% reported interference with professional activities; 16.7% and 28.4% endorsed interference with daily activities; and 13.3% and 20.9% reported disturbances in family relationships.
Finally, as many as 25.1% of individuals sleeping ≥9 hours per main sleep episode and 40.1% of individuals sleeping ≥9 hours per 24-hour period also experienced excessive sleepiness. As seen in Figure 3, individuals sleeping at least 11 hours per 24-hour period were the most affected, even more than individuals with short sleep duration.
Figure 3. Association between sleep duration and complaint of deteriorated quality of wakefulness.
Medical consultations
The percentage of respondents reporting medical consultations for sleepiness was low: 5.2% of individuals sleeping ≥9 hours per main sleep episode; 7.6% for those sleeping ≥ 9 hours per 24 hours and 27.5% for participants with EQS. These rates were low in the context of our other observations that respectively 37.0%, 32.8% and 66% of these participants reported excessive sleep as a problem.
Discussion
This study breaks new ground in examining reports of excessive quantity of sleep in the general population and its pathological associations. In the group of subjects with 9 hours by 24 hours, we have identified three distinct groups:
A first group, sleeping at least 9 hours per main sleep period. They had little association with organic or psychiatric pathologies.
A second group, sleeping at least 9 hours per main period but who regularly nap during the daytime for a total of 9 hours or greater per 24 hours. As seen, this group had a greater number of associated organic and psychiatric pathologies.
Finally, the third group included individuals with a total sleep time of at least 9 hours accompanied WITH distress/impairment related to their sleep. This group had the highest rate of comorbid organic and psychiatric pathologies and a more deteriorated quality of life.
Our major finding is that report of excessive quantity of sleep usually does not occur in isolation but rather coexists with other medical, neurologic, mental or sleep disorders.
We also observed that having a long sleep period (≥ 9 hours per 24-hour period: 1) was reported more frequently by women than men. The difference between men and women had not been uniformly reported in previous epidemiological studies. 2) Excessive quantity of sleep also appeared to be related to age: prolonged sleep duration (9 hours or greater) was more prevalent in both age extremities: the youngest (≤ 24 years old) and the oldest (≥ 65 years old). 3) When reported sleep duration was examined in association with complaints of excessive sleepiness; the distribution had a U-shape that was high among short sleepers (<6 hours) and decreasing with a plateau between 7 and 9 hours of sleep duration. At 9 hours of sleep, the proportion of complaint of excessive sleepiness considerably increased. A similar U-shape distribution was observed for the presence of impairment or distress, organic conditions and psychiatric disorders. The results clearly point to a 9-hour sleep duration as a threshold for increased risk of organic conditions and psychiatric disorders especially mood disorders and also for associated daytime consequences.
Excessive quantity of sleep has a dual significance in sleep-wake disorders classification, representing both the possibility of a specific Hypersomnia Disorder and a consequence of other sleep disorders. As our results show, diagnoses for which excessive quantity of sleep is an essential feature are not so frequent in the general population: 0.5% for DSM-IV-TR Hypersomnia Disorders and 0.038% for narcolepsy with cataplexy. In contrast, other sleep disorders such as Insomnia Disorders, Breathing-Related Sleep Disorders, Circadian Rhythm Sleep Disorders and Dyssomnia Not Otherwise Specified (Restless Legs Syndrome) altogether totaled 20.1% of our sample. Sleep disorders for which deteriorated quality of wakefulness is an associated feature represented about 8% of the sample. For the other cases, the deteriorated quality of wakefulness is part of the impairment/consequences associated with the sleep disorder (for example, insomnia and Restless Legs Syndrome).
The association between excessive quantity of sleep and mood disorders is interesting: Its specificity in mood disorders is difficult to substantiate in the literature.21 While the definitions were all related to the excessive quantity of sleep; for example “sleeping too much,” “sleeping more than 10 hours/day” or “sleeping at least one or two hours more than usual,” they can hardly be compared: depending on the definition, prevalence ranged from 5.5% to 75.8% in individuals with a Major Depressive Disorder.22,23 Nonetheless, our results clearly show that excessive quantity of sleep is highly associated with Dysthymic Disorder and Major Depressive Disorder. Still, excessive quantity of sleep accounts for a small portion of individuals with mood disorders. While sleeping at least 9 hours per day was unrelated to Bipolar Disorders; prolonged sleep episodes accompanied by consequences/distress were significantly related. Also noteworthy, excessive quantity of sleep was seldom associated with other types of mental disorders. Our results show however, that many Anxiety Disorders are associated with prolonged sleep episodes accompanied by consequences/distress.
We also observed that cognitive difficulties were significantly associated with excessive quantity of sleep. Some studies with elderly people have shown that cognitive decline and napping were associated with a greater mortality risk24. Excessive sleepiness was also found to be a predictor of cognitive decline in older individuals. 25,26
Several diseases associated with excessive quantity of sleep were accompanied by consequences/distress. Associations persisted even when adjusting for medication intakes that could be responsible for the increased quantity of sleep.
Consequences associated with excessive quantity of sleep have rarely been investigated in the general population. Our results show that consequences affect many aspects of an individual's life: In addition to its quality, social and professional activities were impaired in about half of the individuals. They were also at greater risk of road accidents. However, direct causality between excessive quantity of sleep and accidents cannot be ascertained.
It should be kept in mind, however, that our results are based on subjective reports. Since ours is an epidemiological study, we did not conduct laboratory testing with respondents to confirm diagnoses. In some cases, such as for insomnia disorder, such measures are not indicated, but for disorders like Obstructive Sleep Apnea Syndrome, polysomnographic recording (PSG) is needed to confirm the diagnosis. Similarly, the use of the daytime Multiple Sleep Latency Test (MSLT) accompanied by nocturnal PSG is useful to confirm a diagnosis of Narcolepsy Without Cataplexy. Therefore, in our study these disorders were diagnosed based on a series of questions addressing the clinical descriptions of the symptoms but without PSG and/or MSLT confirmations. It should be also kept in mind that this study is cross-sectional. Consequently, no causal relationship can be inferred; we can only witness that some associations exist.
The implication for the forthcoming DSM-5 classification of sleep wake disorders is that coexisting medical, neurological, mental and sleep disorders need to be specified when clinicians make a differential diagnosis of Hypersomnolence Disorder. While Hypersomnia Disorders may exist in isolation of other disorders, co-occurring organic and psychiatric disorders are clearly the rule and not the exception. By requiring the clinician to list coexisting disorders, the importance of independent clinical attention to co-morbid conditions is underscored.
Acknowledgments
The three authors have participated sufficiently in the work to take public responsibility for the content. More specifically, the three authors were involved in the conception OR design OR analysis and interpretation of data; have contributed to the drafting and revisions of the manuscript; and have approved the submitted version.
This study was supported by the National Institutes of Health grant R01NS044199, the Arrillaga Foundation and the Bing Foundation (MMO). The authors have no other financial relationships with commercial interests with the sponsors.
MMO was the PI of this study and was doing the data collection. He had access to all data from the study, both what is reported and what is unreported, and he also had complete freedom to direct his analysis and his reporting, without influence from the sponsors. The sponsors had no role in the design and conduct of the study, nor the collection, management, analysis and interpretation of the data. There was no editorial direction or censorship from the sponsors. The sponsors have not seen the manuscript and had no role in the decision to submit the paper for publication.
Contributor Information
Maurice M. Ohayon, Stanford Sleep Epidemiology Research Center, Stanford University, School of Medicine, Palo Alto, CA 94303
Charles F. Reynolds, III, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA 15213
Yves Dauvilliers, Centre de Référence Nationale Maladie Rare – Narcolepsie et Hypersomnie Idiopathique, Service de Neurologie, Hôpital Gui-de-Chauliac, Inserm U1061 Montpellier, France
References
- 1.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR) Washington: The American Psychiatric Association; 2000. [Google Scholar]
- 2.American Academy of Sleep Medicine. The International Classification of Sleep Disorders- Revised: Diagnostic and Coding Manual. Rochester Minnesota: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 3.Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12:129–141. doi: 10.1016/j.smrv.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 5.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 6.Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34:1487–1492. doi: 10.5665/sleep.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sabanayagam C, Shankar A. Sleep duration and hypercholesterolaemia: Results from the National Health Interview Survey 2008. Sleep Med. 2012;13:145–150. doi: 10.1016/j.sleep.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zizi F, Pandey A, Murrray-Bachmann R, Vincent M, McFarlane S, Ogedegbe G, Jean-Louis G. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the National Health Interview Survey. Am J Med. 2012;125:162–167. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ohayon MM, Dauvilliers Y, Reynolds CF. Operational Definitions and Algorithms for Excessive Sleepiness in the General Population: Implications for DSM-5 Nosology. Arch Gen Psychiatry. 2012;69:71–79. doi: 10.1001/archgenpsychiatry.2011.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kish L. Survey Sampling. New York: John Wiley & Sons Inc.; 1965. [Google Scholar]
- 11.Ohayon MM. Sleep-EVAL Knowledge Based System for the Diagnosis of Sleep and Mental Disorders Copyright Office, Canadian Intellectual Property Office. Ottawa: Industry Canada; 1994. [Google Scholar]
- 12.Ohayon MM. Improving decision-making processes with the fuzzy logic approach in the epidemiology of sleep disorders. J Psychosom Res. 1999;47:297–311. doi: 10.1016/s0022-3999(99)00010-0. [DOI] [PubMed] [Google Scholar]
- 13.Lewis G, Pelosi AJ, Araya RC, et al. Measuring psychiatric disorder in the community, a standardized assessment for use by lay interviewers. Psychol Med. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 14.Ohayon MM, Guilleminault C, Zulley J, et al. Validation of the Sleep-EVAL system against clinical assessments of sleep disorders and polysomnographic data. Sleep. 1999;22:925–930. doi: 10.1093/sleep/22.7.925. [DOI] [PubMed] [Google Scholar]
- 15.Ohayon M. Validation of expert systems: Examples and considerations. Medinfo. 1995;8(Pt 2):1071–1075. [PubMed] [Google Scholar]
- 16.Hosn R, Shapiro CM, Ohayon MM. Diagnostic concordance between sleep specialists and the Sleep-EVAL system in routine clinical evaluations. J Sleep Res. 2000;9(suppl 1):86. [Google Scholar]
- 17.Black J, Ohayon MM, Okun M, et al. The narcolepsy diagnosis: comparison between the Sleep-EVAL system and clinicians. Sleep. 2001;24(Abst Suppl):A328. [Google Scholar]
- 18.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 19.Hays JC, Blazer DG, Foley DJ. Risk of napping: excessive daytime sleepiness and mortality in an older community population. J Am Geriatr Soc. 1996;44:693–698. doi: 10.1111/j.1532-5415.1996.tb01834.x. [DOI] [PubMed] [Google Scholar]
- 20.Quera-Salva MA, Orluc A, Goldenberg F, et al. Insomnia and use of hypnotics: study of a French population. Sleep. 1991;14:386–391. doi: 10.1093/sleep/14.5.386. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan KA, Harvey AG. Hypersomnia across mood disorders: a review and synthesis. Sleep Med Rev. 2009;13:275–285. doi: 10.1016/j.smrv.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Roberts RE, Shema SJ, Kaplan GA, et al. Sleep complaints and depression in an aging cohort: A prospective perspective. Am J Psychiatry. 2000;157:81–88. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- 23.Parker G, Malhi G, Hadzi-Pavlovic D, et al. Sleeping in? The impact of age and depressive sub-type on hypersomnia. J Affect Disord. 2006;90:73–76. doi: 10.1016/j.jad.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Hays JC, Blazer DG, Foley DJ. Risk of napping: Excessive daytime sleepiness and mortality in an older community population. J Am Geriatr Soc. 1996;44:693–698. doi: 10.1111/j.1532-5415.1996.tb01834.x. [DOI] [PubMed] [Google Scholar]
- 25.Foley D, Monjan A, Masaki K, et al. Daytime sleepiness is associated with 3-year incident dementia and cognitive decline in older Japanese-American men. J Am Geriatr Soc. 2001;49:1628–1632. doi: 10.1046/j.1532-5415.2001.t01-1-49271.x. [DOI] [PubMed] [Google Scholar]
- 26.Ohayon MM, Vechierrini MF. Daytime sleepiness is an independent predictive factor for cognitive impairment in the elderly population. Arch Intern Med. 2002;162:201–208. doi: 10.1001/archinte.162.2.201. [DOI] [PubMed] [Google Scholar]