Abstract
The establishment of the Meaningful Use criteria has created a critical need for robust interoperability of health records. A universal definition of a personal health record (PHR) has not been agreed upon. Standardized code sets have been built for specific entities, but integration between them has not been supported. The purpose of this research study was to explore the hindrance and promotion of interoperability standards in relationship to PHRs to describe interoperability progress in this area. The study was conducted following the basic principles of a systematic review, with 61 articles used in the study. Lagging interoperability has stemmed from slow adoption by patients, creation of disparate systems due to rapid development to meet requirements for the Meaningful Use stages, and rapid early development of PHRs prior to the mandate for integration among multiple systems. Findings of this study suggest that deadlines for implementation to capture Meaningful Use incentive payments are supporting the creation of PHR data silos, thereby hindering the goal of high-level interoperability.
Key words: personal health record, interoperability, meaningful use, regional health information organization (RHIO)
Introduction
Personal Health Records
The concept of personal health records (PHRs) is not a new one.1 Patients have long kept health information in paper format. Archer et al. (2011) reported that among the 47 percent of patients who maintained health records, 87 percent stated that the information was on paper. The difference is that health information technology (HIT) now provides individuals the ability to keep their health information electronically, thus having the PHR accessible at all times.2
The functionality of PHRs varies, but they have one basic goal, which is to allow people greater access to healthcare data and permit them to engage in their own health management.3 This study used the definition of a PHR according to the Markle Foundation, which states that a PHR is “an electronic application through which individuals can access, manage and share their health information, and that of others for whom they are authorized, in a private, secure, and confidential environment.”4
Different types of electronic PHRs have been previously discussed in the literature. Standalone and tethered PHR systems are the most common. Standalone PHRs require individuals to enter health information exclusively; alternatively, third parties, such as insurance companies, can feed the record. Patients can add information to data provided by third parties and in some instances can modify information.5 Although information can be downloaded to an external storage device, stand-alone PHRs are not sharable with healthcare institutions.6 Tethered PHRs connect to a specific healthcare institution or provider but not to other systems. These types of PHRs are read-only to patients and are not editable. Tethered PHRs contain such information as laboratory results, immunization records, radiology images, and other data.7 The third PHR type is integrated, in which patient information is integrated with the electronic health record (EHR), allowing patients to share personal information and view the entire medical record as documented by the institution or provider.8
A need for a strong, integrated PHR system with interoperability has been paramount in the healthcare environment. The Office of the National Coordinator for Health Information Technology (ONC) was formed in 2004 to facilitate collaboration between the private and public sectors of healthcare to define a national infrastructure to support interoperability.9 Interoperability is the enabling of electronic health information exchange through two or more systems and the ability for that information to be used by the recipients of the healthcare data.10
Interoperability
Three types of interoperability can be identified. Foundational interoperability exchanges data from one HIT system to another without the ability of the recipient system to interpret the data. An example of this type of interoperability occurs when a staff member at a physician's office prints a clinical summary report and gives it to the patient to take to a referral physician. The referral physician's office staff reads the document and enters information into their own system, the recipient system. Structural interoperability is a midlevel type of interoperability that defines a structure for data information exchange. Data exchanged between systems can be read and understood by the receiving system at a granular data level. An example of structural interoperability would be a hospital sending a Health Level Seven (HL7) interface message containing a patient's social history to a home health service. The home health service, or recipient system, could read the incoming message and translate it so that the information becomes part of the home health service's electronic record. Semantic interoperability is the highest-level type of interoperability, in which data exchange standards and data coding allow recipient systems to interpret the data.11 An example of this type of interoperability may occur when a patient interacts with several different providers and healthcare systems. In a true semantic interoperability world, all of these systems would be able to pull data from and search the other systems so that a provider at any one healthcare entity could have all of the patient's most current information. Additionally, the recipient system would take the data gathered from the various other systems and trigger clinical decision support, offering the provider suggestions for care actions.12
The need for interoperability is urgent. Patients, informed through the Internet regarding healthcare, have begun demanding more from healthcare institutions and providers.13 An increased focus on quality healthcare began in 2001 with the release of the Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century.14 In 2012, the gross domestic product (GDP) of the United States reached $2.7 trillion, growing to a staggering equivalent of $8,680 per person.15 As a share of the nation's GDP, healthcare spending accounted for 17.2 percent.16 With the enactment of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009, financial incentives and penalties through Meaningful Use criteria have spurred wider interest in higher-quality and cost-efficient care by healthcare institutions and providers.17, 18 Stages of Meaningful Use progressively have required engagement of patients in their personal health management, strengthening the case for highly functioning PHRs.19
The purpose of this research study was to explore the promotion factors and barriers related to the development of PHRs to determine interoperability challenges and progress in this area.
Methodology
This research study followed the basic principles of a systematic review in examining PHR and healthcare information interoperability. Full-text articles were utilized using the PubMed, EBSCOhost, ProQuest, Academic Premier, PsycINFO, CINAHL, MEDLINE, and LexisNexis databases, along with information from the Agency for Healthcare Research and Quality (AHRQ), Centers for Medicare and Medicaid Services (CMS), CommonWell Health Alliance Organization, Project HealthDesign, American Health Lawyers Association, Healthcare Information and Management Systems Society (HIMMS), Forbes, Markle Foundation, US Department of Health and Human Services (HHS), National eHealth Collaborative (NeHC), Nationwide Health Information Network (NHIN), ONC, Robert Wood Johnson Foundation (RWJF), and TELUS health space websites. Google was used when different articles were not located within the above databases. Abstracts were reviewed to see how articles were relevant to this research. Keywords used throughout the search included PHR OR standalone PHR OR tethered PHR AND interoperability OR Meaningful Use OR healthcare OR barriers OR integrated. The literature search was constrained to articles published after 2000 to limit the material reviewed to recent and relevant information. All articles were limited to the English language. Original articles presented primary and secondary data, including reviews and research studies. Articles were selected after the review of all abstracts was completed. References were determined to have satisfied the inclusion criteria if the material provided accurate information about PHRs with a particular consideration on promotion and hindrance of their implementation. The literature search was conducted by the first author and was validated by the second author, who determined if references met the research study inclusion criteria. From a total of 188 initial references, only 61 sources were deemed suitable for use in this research study.
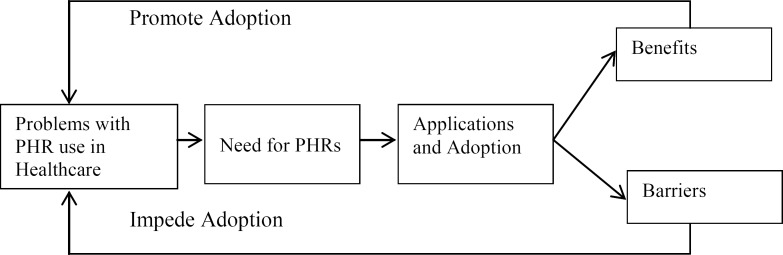
The research approach for the examination of the promotion factors and barriers to adoption of PHRs followed the systematic steps and conceptual framework utilized by Yao, Chu, and Li.20 The use of this conceptual framework in the current study is appropriate because the focus of both studies is to show how new technologies can be applied to healthcare settings to enhance the care of patients; in addition, this approach has been successfully replicated in previous studies, increasing its internal validity.21, 22, 23 Figure 1 depicts the process of PHR adoption in healthcare. To research how PHRs can help to improve healthcare practices, it is first necessary to recognize the existing problems of PHRs and the factors that drive and impede their adoption within the healthcare industry. Different applications can then be identified to solve or partially unravel these challenges. As a final result of analyzing the literature, promotion factors and barriers to PHR utilization in healthcare can be identified.
Figure 1.
Process of Personal Health Record (PHR) Adoption in Healthcare
Finally, the results were structured using two major categories, Promotion Factors and Barriers for Adoption of PHRs, following the conceptual framework.
Results
Promotion Factors for PHR Interoperability
Healthcare Legislation Affecting PHR Development
Through the American Recovery and Reinvestment Act of 2009 (ARRA), and the enactment of the HITECH Act, the Meaningful Use criteria have been fueling a critical need for robust interoperability between the systems used by patients, providers, and healthcare institutions.24, 25 The Meaningful Use stages progressively demand compliance within the Patient Engagement Framework (PEF). Stage 2 of Meaningful Use, the “Engage Me” phase of the PEF, promotes interactive patient forms for scheduling appointments and refilling prescriptions.26 The rate of reported PHR use in New York increased from 11 percent in 2012 to 17 percent in 2013. The proportion of these PHRs that were provided by doctors or healthcare organizations also increased sharply from 50 percent in 2012 to 73 percent in 2013.27 These researchers also reported that the mean age of PHR users was 47.2 years, 51 percent were female, and 80 percent had a physician who used EHRs. PHR and EHR integration has been mandated, as have interoperable health records through health information exchanges (HIEs) and regional health information organizations (RHIOs) at Meaningful Use Stage 3 and the PEF's “Empower Me” phase. Electronic referrals between providers, images, laboratory results, medication lists, and inpatient/outpatient records are also included in Stage 3.28
Potential Financial Impact
A positive force for interoperability of PHRs has been the potential financial impact. Medicare and Medicaid eligible hospitals have received from $2 million up to $6.37 million in incentives for meeting Meaningful Use criteria, which included the implementation of PHRs.29 (See Table 1.) The Center for Information Technology Leadership has suggested that the United States could reap savings greater than $21 billion a year, assuming that 80 percent of healthcare consumers were actively engaged in using a PHR by 2018.30 However, critical technical and policy issues have remained. Management of privacy and access authorization has demanded efficiency and trusted agreements for secure data exchange between health organizations, and third-party data integration has needed further refinement.31 Fabozzi (2013) estimated a market increase in PHR adoption of 221 percent from 2012 to 2017.32 (See Table 1.)
Table 1.
Promotion of Personal Health Record (PHR) Interoperability
| Source | Promotion |
|---|---|
| US Department of Health and Human Services (2001) | • Standard codes such as LOINC, ICD-9, SNOMED, HL7 |
| Bock et al. (2005) | • Interoperability among health information technology systems estimated to save $77.8 billion every year |
| US Department of Health and Human Services (2006) | • Nationwide health information network functional requirements defined |
| Kaelber et al. (2008) | • $21 billion potential savings |
| Hufnagel (2009, “National”) |
|
| Hufnagel (2009, “Interoperability”) |
|
| Robert Wood Johnson Foundation (2009) | • Increased value of patient information |
| Brennan et al. (2010) | • Common software platform |
| Jones et al. (2010) | • PHR certification |
| Kim et al. (2011) | • PHR certification |
| National eHealth Collaborative (2012) |
|
| Rogoski (2012) | • Meaningful Use monetary incentives |
| Centers for Medicare and Medicaid Services (2013) | • Medicare/Medicaid eligible hospitals receive $2 million to $6.37 million in Meaningful Use incentive payments |
| Fabozzi (2013) | • Market increase of 221 percent between 2012 to 2017 |
| Sujansky & Associates, LLC (2013) |
|
Sources:
Bock, C., L. Carnahan, S. Fenves, M. Gruninger, V. Kashyap, B. Lide, J. Nell, R. Raman, and R. D. Sriram. Healthcare Strategic Focus Area: Clinical Informatics. National Institute of Standards and Technology Report No. 7263. Gaithersburg, MD: Technology Administration, US Department of Commerce, 2005.
Brennan, P. F., S. Downs, and G. Casper. “Project HealthDesign: Rethinking the Power and Potential of Personal Health Records.” Journal of Biomedical Informatics 43, no. 5, suppl. (2010): S3–S5.
Centers for Medicare and Medicaid Services. “EHR Incentive Programs.” 2013. Available at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/ (accessed January 11, 2014).
Fabozzi, N. “U.S. Patient Portal Market for Hospitals and Physicians: Overview and Outlook, 2012–2017.” Frost & Sullivan. 2013. Available at http://www.frost.com/prod/servlet/frost-home.pag (accessed January 11, 2014).
Hufnagel, S. P. “Interoperability.” Military Medicine 174, no. 5 (2009): 43–50.
Hufnagel, S. P. “National Electronic Health Record Interoperability Chronology.” Military Medicine 174, no. 5 (2009): 35–42.
Jones, D. A., J. P. Shipman, D. A. Plaut, and C. R. Seiden. “Characteristics of Personal Health Records: Findings of the Medical Library Association/National Library of Medicine Joint Electronic Personal Health Record Task Force.” Journal of the Medical Library Association 98, no. 3 (2010): 243–49.
Kaelber, D. C., S. Shah, A. Vincent, E. Pan, J. M. Hook, D. Johnston, D. W. Bates, and B. Middleton. The Value of Personal Health Records. Charlestown, MA: Center for Information Technology Leadership, 2008. Available at http://www.partners.org/cird/pdfs/CITL_PHR_Report.pdf (accessed November 4, 2013).
Kim, J., H. Jung, and D. Bates. “History and Trends of ‘Personal Health Record’ Research in PubMed.” Healthcare Informatics Research 17, no. 1 (2011): 3–17.
National eHealth Collaborative. “The Patient Engagement Framework.” 2012. http://www.nationalehealth.org/patient-engagement-framework (accessed September 16, 2013).
Robert Wood Johnson Foundation. “Personal Health Records 101.” October 1, 2009. Available at http://www.rwjf.org/en/research-publications/find-rwjf-research/2010/01/feature-the-power-and-potential-of-personal-health-records/chapter-1-personal-health-records-101.html (accessed October 15, 2013).
Rogoski, R. R. “Bridging the EHR Divide: Hospitals, Physician Practices Work toward True Interoperability.” Healthcare Informatics 29, no. 10 (2012): 8–12.
Sujansky & Associates, LLC, on behalf of Project HealthDesign. A Standards-based Model for the Sharing of Patient-generated Health Information with Electronic Health Records. 2013. Available at http://www.projecthealthdesign.org/media/file/Standard-Model-For-Collecting-And-Reporting-PGHI_Sujansky_Assoc_2013-07-18.pdf (accessed October 26, 2013).
US Department of Health and Human Services. Information for Health: A Strategy for Building the National Health Information Infrastructure. 2001. Available at http://www.ncvhs.hhs.gov/nhiilayo.pdf (accessed October 1, 2013).
US Department of Health and Human Services. Report to the Secretary of the U.S. Department of Health and Human Services on Functional Requirements Needed for the Initial Definition of a Nationwide Health Information Network (NHIN). 2006. Available at http://www.ncvhs.hhs.gov/061030lt.pdf (accessed September 18, 2013).
Use of Existing Standards
A report by Sujansky & Associates, LLC, prepared for Project HealthDesign in 2013, proposed specific standards for sharing of patient-generated health information using currently available industry standards.33 The Continua Alliance identified 29 data collection devices certified as agents and 45 gateways devices certified as managers.34 (See Table 1.) The report further noted the development of the IEEE 11073 domain model, the HL7 v. 2.6 message standard, and the Direct Project for secure messaging as strong promoting components for interoperability progress.
Additional supporting factors for interoperability have included patient safety enhancement, increase in speed of delivery of care, and improved quality of care.35, 36 Federated architecture adds minimal or no additional cost to a connected system.37 (See Table 1.)
Barriers to PHR Interoperability
Difficulty of Interoperability of PHRs
Interoperability can be achieved at different levels. At the lowest level, a certain amount of interoperability is present with paper records in that the record can be handed to a provider, who then interprets the data and makes a medical decision.38 At the most sophisticated level of interoperability, EHR systems share the data and can compile information into a type of knowledge that can assist a provider in decision making.39 To achieve semantic interoperability, a consensus much be reached in regard to uniform standards according to which all PHRs are built.40
Standardized code sets have been developed to support interoperability. Laboratory results use Logical Observation Identifiers Names and Codes (LOINC).41 Health information billing specialists use International Classification of Diseases (ICD) codes for medical diagnoses.42 Medications are coded by National Drug Code (NDC) standards.43 Systematized Nomenclature of Medicine–Clinical Terms (SNOMED CT) defines clinical terms.44 Clinical and administrative terms are managed with HL7 code sets.45 These standards have been built for specific entities, and while the standards can pass from one electronic system to another, integration among them has not been supported.46
In 2006, the National Committee on Vital and Health Statistics (NCVHS) issued a summary report outlining functional requirements needed for the definition of a NHIN. This report outlined the need for complete health information interoperability.47 Emergency services, hospitals, individual patients, schools, public health organizations, and providers all needed appropriate access to an individual's health record.48 Functionally high levels of the NHIN have included certification, authentication, authorization, person identification, location of health information, transport and content standards, data transactions, auditing and logging, time-sensitive data access, communications, and data storage.49 Functional categories have been further defined to include confidentiality, credentialing, data access and update, data filtering, data mapping and translation, data quality and integrity, data retrieval, data routing, data source, data transmission, and data usage.50 Overall, 977 data elements and functionality have been specifically spelled out in a 150-page spreadsheet and a 20-page appendix of architecture variations identified by the ONC.51
Lagging interoperability has been stemmed from slow adoption rates by patients, creation of disparate systems as a result of rapid development to meet the Meaningful Use stages of patient engagement, and rapid early development of PHRs prior to the mandate for integration among multiple systems.52 Fragmentation of the PHR environment has been fostered by the disparate nature of the federal government agencies that are responsible for development of a national health information infrastructure.53
Hindrances faced by project teams trying to create interoperability are illustrated in the lessons learned from Project HealthDesign. Issues experienced by the team with a third-party platform, HealthVault, included lack of support for incorporating the observations of daily living (ODL) data type from patient input. The data type did not conform to established data models.54 Trying to upload ODL data required complex interfaces, and the cost of integration outweighed the benefits.55 Project HealthDesign faced many challenges in moving interoperability forward, including the need for a trusted third-party data repository that would provide complete data ownership to patients and the need for providers to be informed of the direct origin of patient-entered data.56 (See Table 2.)
Table 2.
Barriers to Personal Health Record (PHR) Interoperability
| Source | Barriers |
|---|---|
| US Department of Health and Human Services (2001) |
|
| US Department of Health and Human Services (2006) |
|
| Kaelber et al. (2008) |
|
| Robert Wood Johnson Foundation (2009) |
|
| Brennan et al. (2010) |
|
| Gosfield et al. (2010) |
|
| Jones et al. (2010) |
|
| Witry et al. (2010) |
|
| Kim et al. (2011) |
|
| Bipartisan Policy Center (2012) |
|
| National eHealth Collaborative (2012) |
|
| Rogoski (2012) |
|
| Nazi et al. (2013) |
|
| Sujansky & Associates, LLC (2013) |
|
Sources:
Bipartisan Policy Center. Accelerating Electronic Information Sharing to Improve Quality and Reduce Costs of Health Care. October 2012. Available at http://bipartisanpolicy.org/sites/default/files/BPC%20Accelerating%20Health%20Information%20Exchang_e_format.pdf (accessed January 11, 2014).
Brennan, P. F., S. Downs, and G. Casper. “Project HealthDesign: Rethinking the Power and Potential of Personal Health Records.” Journal of Biomedical Informatics 43, no. 5, suppl. (2010): S3–S5.
Gosfield, A. G., and J. L. Reinertsen. Achieving Clinical Integration with Highly Engaged Physicians. 2010. Available at http://www.reinertsengroup.com/publications/documents/True%20Clinical%20Integration%20Gosfield%20Reinertsen%202010.pdf (accessed May 28, 2014).
Jones, D. A., J. P. Shipman, D. A. Plaut, and C. R. Seiden. “Characteristics of Personal Health Records: Findings of the Medical Library Association/National Library of Medicine Joint Electronic Personal Health Record Task Force.” Journal of the Medical Library Association 98, no. 3 (2010): 243–49.
Kaelber, D. C., S. Shah, A. Vincent, E. Pan, J. M. Hook, D. Johnston, D. W. Bates, and B. Middleton. The Value of Personal Health Records. Charlestown, MA: Center for Information Technology Leadership, 2008. Available at http://www.partners.org/cird/pdfs/CITL_PHR_Report.pdf (accessed November 4, 2013).
Kim, J., H. Jung, and D. Bates. “History and Trends of ‘Personal Health Record’ Research in PubMed.” Healthcare Informatics Research 17, no. 1 (2011): 3–17.
National eHealth Collaborative. “The Patient Engagement Framework.” 2012. http://www.nationalehealth.org/patient-engagement-framework (accessed September 16, 2013).
Nazi, K., T. Hogan, D. McInnes, S. Woods, and G. Graham. “Evaluating Patient Access to Electronic Health Records: Results from a Survey of Veterans.” Medical Care 51, no. 3, suppl. 1 (2013): S52–S56.
Robert Wood Johnson Foundation. “Personal Health Records 101.” October 1, 2009. Available at http://www.rwjf.org/en/research-publications/find-rwjf-research/2010/01/feature-the-power-and-potential-of-personal-health-records/chapter-1-personal-health-records-101.html (accessed October 15, 2013).
Rogoski, R. R. “Bridging the EHR Divide: Hospitals, Physician Practices Work toward True Interoperability.” Healthcare Informatics 29, no. 10 (2012): 8–12.
Sujansky & Associates, LLC, on behalf of Project HealthDesign. A Standards-based Model for the Sharing of Patient-generated Health Information with Electronic Health Records. 2013. Available at http://www.projecthealthdesign.org/media/file/Standard-Model-For-Collecting-And-Reporting-PGHI_Sujansky_Assoc_2013-07-18.pdf (accessed October 26, 2013).
US Department of Health and Human Services. Information for Health: A Strategy for Building the National Health Information Infrastructure. 2001. Available at http://www.ncvhs.hhs.gov/nhiilayo.pdf (accessed October 1, 2013).
US Department of Health and Human Services. Report to the Secretary of the U.S. Department of Health and Human Services on Functional Requirements Needed for the Initial Definition of a Nationwide Health Information Network (NHIN). 2006. Available at http://www.ncvhs.hhs.gov/061030lt.pdf (accessed September 18, 2013).
Witry, M., W. Doucette, J. Daly, B. Levy, and E. Chrischilles. “Family Physician Perceptions of Personal Health Records.” Perspectives in Health Information Management (2010).
The sustainability of PHRs has brought forward the issue of patients being able to move their stored health information to another PHR. Google discontinued Google Health in January 2012, leaving users with a quandary regarding how and where to move their stored data.57 In Canada, however, TELUS has formed a collaborative effort with HealthVault and has established interoperability with clinics through TELUS Health Space, which has given Canadian healthcare consumers a national PHR.58
In addition, a universal definition of a PHR has not been agreed upon.59, 60, 61 Wynia and Dunn identified six different definitions from seven different agencies; these definitions have further confounded the drive toward interoperability.62 The sheer volume of PHRs has been documented in the literature as well. Jones, Shipman, Plaut, and Seiden reported identifying 117 PHRs with varying degrees of functionality.63 As of October 2013, the American Health Information Management Association (AHIMA) patient resource website, www.myphr.com, listed 91 PHRs, 10 of which were paper based, and contained nine links to mobile-based PHR websites. Sixty-three percent of the PHRs that AHIMA cited were available to be purchased by the consumer.64
Provider Concerns Regarding PHR Information
Concerns from providers in enhancing the interoperability of PHRs and EHRs have included issues of privacy and the accuracy of the information entered by patients. In addition, questions have risen as to whether the information entered by patients should be used to make medical decisions.65
Physicians and other providers have demonstrated reluctance to use PHR information provided by patients. With increased interoperability populating the patient's EHR with patient-provided information, some providers have expressed concern about legal liability. The fear of being held accountable for using information provided by the patient has hindered interoperability progress between PHRs and EHRs (See Table 2).66
Discussion
The findings of this study suggest that the deadlines for incentive payments for meeting Meaningful Use criteria have stimulated an environment encouraging development and adoption of PHRs, which has resulted in the creation of silos of personal health information that cannot be seamlessly shared with EHRs and other PHRs. With a national goal of seamlessly integrated healthcare, the rush to implement PHRs has perpetuated roadblocks to interoperability, thus hindering progress.
Although PHRs vary in their features, the records all strive to contain common elements. No plan has been defined for the creation of a universal PHR; however, defining common data sets has been an essential starting point.67 Interoperability not only can help to reduce costs and improve quality of care but also can permit regulatory compliance and enhance access to healthcare for millions.68 The urgency of developing interoperable PHR systems has been defined and has created strong promotion of these systems. In the rush to create PHRs to meet Meaningful Use patient engagement standards, little thought has been given at the forefront to the need for a national PHR system to which all healthcare entities can contribute. Healthcare consumers have multiple PHRs that contain duplicate information, are not interoperable, and contain standardized codes rather than nonprofessional medical terms for easy comprehension.
The results of this study also suggest that PHRs have been available from a wide variety of sources and have continued to multiply as the Meaningful Use stages evolve. Hospitals, insurance companies, and physician practices have been striving to rapidly engage consumers. With the multitude of third-party vendors involved in PHR development, oversight from legal and regulatory bodies has been a paramount concern as interoperability has moved forward.69 Interoperability supports accurate exchange of information with other healthcare entities, structured data collection, and access to additional knowledge bases by being standard driven. Common data elements have been established for use.70
In 2006, the NCVHS reported that interoperability was hindered because most PHRs integrated with one EHR exclusively.71 Although this integration supported the patient-provider relationship, the relationship existed in a silo because the EHRs were not interoperable with each other. Because of the lack of EHR interoperability, patient information from other healthcare entities and providers does not populate the patient's PHR. PHRs that have been exclusively maintained by the patient may include information from many EHRs, but interoperability standards for transmission of data from the PHR to EHRs are still lacking.72 According to the authors’ findings, the lack of interoperability has not diminished significantly as of 2013. In the effort to facilitate and support interoperability of PHRs with EHRs, silos of data have been created amid already disparate information systems.
Limitations
In conducting this research study, the authors uncovered a vast number of work groups, grant recipients, proposed methodologies, PHR sites, and opinion blogs that have tackled the difficult undertaking of developing a PHR that is fully interoperable with all EHRs. Despite a common thread, the paths being taken have been widely diverse. Additional limitations of this research study are that no universally accepted definition of a PHR and no single methodology for implementation of standards existed as of 2013. Facilitators and impediments of interoperability represent the authors’ interpretation of the literature reviewed, and thus researchers’ bias cannot be ruled out. Further research limitations included the number and quality of the databases searched, the research strategy used, and publication bias.
Practical Implications and Future Research
As of the writing of this article, some practical applications have moved toward furthering unified healthcare interoperability. Continued widespread adoption of the Blue Button icon, promoted by the Department of Veterans Affairs (VA), by other PHR entities will give consumers a consistent, familiar method for downloading personal information for clinicians. The movement toward establishing a universal patient identifier is gaining ground and will promote further advances in interoperability. In addition, further research is needed to determine the demand by type of patients requiring PHRs, such as seniors or parents, as well as other issues of patient engagement.
However, consumer frustration in trying to maintain multiple PHRs and sharing them with multiple providers and healthcare institutions will foster disengagement of patients, rather than engagement. The overall goal of an integrated healthcare system nationally could suffer from self-sabotage. Additional research is needed to ascertain if the numbers of organizations involved in interoperability work will confound interoperability further or will lead to success in the stated efforts.
Perhaps a highly interoperable PHR solution lies with HIEs and RHIOs taking the lead in organizing the mass of work that has been completed toward efforts of true interoperability. RHIOs will need the financial means to maintain operations once grant funding has ended. Having a standard PHR within HIEs that allows other PHRs to export and import data will offer a standard methodology for sharing of information. Memberships to RHIO PHR systems could be offered for a price and provide monetary support needed for continued sustainability of HIEs and RHIOs.
Conclusion
Promotion of interoperability between PHRs and EHRs has been strongly supported through development of standard coding language, work groups, and federal legislation. Foundational interoperability has been fairly well integrated into physician offices by the provision of a printed clinical summary to the patient. The rapid development of PHRs driven by financial incentives, however, has slowed semantic interoperability. Although much progress has been made toward interoperability in the PHR arena, the rush to implement PHRs has perpetuated roadblocks to interoperability, thus hindering progress.
Contributor Information
Jana Studeny, Jana Studeny, RN-BC, MSHI, is a graduate of the Healthcare Informatics Program at Marshall University in Huntington, WV..
Alberto Coustasse, Alberto Coustasse, DrPH, MD, MBA, MPH, is an associate professor of the healthcare administration program in the College of Business at Marshall University in South Charleston, WV..
Notes
- 1.Archer N., Fevrier-Thomas U., Lokker C., McKibbon K. A., Straus S. E. Personal Health Records: A Scoping Review. Journal of the American Medical Informatics Association. 2011;18(4):515–22. doi: 10.1136/amiajnl-2011-000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coffield R. L., Ishee J., Kapp J. L., Lyles K. D., Williams R. L. Personal Health Records: History, Evolution, and the Implications of ARRA. American Health Lawyers Association; 2011. Available at http://www.healthlawyers.org/Events/Programs/Materials/Documents/AM11/AHLAResources/practicegroups/Briefing_PHRs.pdf (accessed October 2, 2013). [Google Scholar]
- 3.Halamka J. D., Mandl K. D., Tang P. C. Early Experiences with Personal Health Records. Journal of the American Medical Informatics Association. 2006;13(2):121–26. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markle Foundation. Connecting Americans to Their Health Care: A Common Framework for Networked Personal Health Information. 2006. Available at. http://www.markle.org/sites/default/files/CF-Consumers-Full.pdf (accessed September 26, 2013).
- 5.Maloney F. L., Wright A. USB-based Personal Health Records: An Analysis of Features and Functionality. International Journal of Medical Informatics. 2010;79(2):97–111. doi: 10.1016/j.ijmedinf.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Tang P. H. Your Doctor's Office or the Internet? Two Paths to Personal Health Records. New England Journal of Medicine. 2009;360(13):1276–78. doi: 10.1056/NEJMp0810264. [DOI] [PubMed] [Google Scholar]
- 7.Nazi K., Hogan T., McInnes D., Woods S., Graham G. Evaluating Patient Access to Electronic Health Records: Results from a Survey of Veterans. Medical Care. 2013;51(3 suppl. 1):S52–S56. doi: 10.1097/MLR.0b013e31827808db. [DOI] [PubMed] [Google Scholar]
- 8.Detmer D., Bloomrosen M., Raymond B., Tang P. Integrated Personal Health Records: Transformative Tools for Consumer-centric Care. BMC Medical Informatics and Decision Making. 2008;8(1):45–58. doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hufnagel S. P. National Electronic Health Record Interoperability Chronology. Military Medicine. 2009;174(5):35–42. doi: 10.7205/milmed-d-03-9708. [DOI] [PubMed] [Google Scholar]
- 10.Office of the National Coordinator for Health Information Technology (ONC) Certification Guidance for EHR Technology Developers Serving Health Care Providers Ineligible for Medicare and Medicaid EHR Incentive Program. 2013. http://www.healthit.gov/policy-researchers-implementers/meaningful-use-stage-2 (accessed September 13, 2013).
- 11.Healthcare Information and Management Systems Society (HIMSS) What Is Interoperability? 2013. Available at http://www.himss.org/library/interoperability-standards/what-is?navItemNumber=17333 (accessed September 26, 2013).
- 12.Stratis Health. Interoperability for EHR and HIE. 2013. Available at http://www.stratishealth.org/documents/healthit/homehealth/1.Assess/1-interoperability-for-EHR-and-HIE.doc (accessed November 14, 2013).
- 13.Dwyer D., Liu H. The Impact of Consumer Health Information on the Demand for Health Services. Quarterly Review of Economics and Finance. 2013;53(1):1–11. [Google Scholar]
- 14.Institute of Medicine, Committee on Quality of Health Care in America. Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. Crossing the Quality. [Google Scholar]
- 15.Center for Medicare and Medicaid Services. National Health Expenditure Data: Historical. 2014. Available at http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html (accessed March 3, 2014).
- 16.Hartman M., Martin A. B., Benson J., Catlin A. National Health Expenditure Accounts Team. National Health Spending in 2011: Overall Growth Remains Low, But Some Payers and Services Show Signs of Acceleration. Health Affairs. 2013;32(1):87–99. doi: 10.1377/hlthaff.2012.1206. [DOI] [PubMed] [Google Scholar]
- 17.Health Information Technology for Economic and Clinical Health (HITECH) Act. Pub. L. 111-5, 123 Stat. 226. 2009. Available at http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf (accessed September 26, 2013).
- 18.Pipersburgh J. The Push to Increase the Use of EHR Technology by Hospitals and Physicians in the United States through the HITECH Act and the Medicare Incentive Program. Journal of Health Care Finance. 2011;38(2):54–78. [PubMed] [Google Scholar]
- 19.Centers for Medicare and Medicaid Services. Electronic Health Records (EHR) Incentive Program. 2010. http://www.cms.gov/Regulations-andGuidance/Legislation/EHRIncentivePrograms/Stage_2.html (accessed September 26, 2013).
- 20.Yao W., Chu C. H., Li Z. The Use of RFID in Healthcare: Benefits and Barriers. Proceedings of the 2010 IEEE International Conference on RFID–Technology and Applications. 2010. pp. 128–34.
- 21.Coustasse A., Tomblin S., Slack C. Impact of Radio-Frequency Identification (RFID) Technologies on the Hospital Supply Chain: A Literature Review. Perspectives in Health Information Management. 2013. ). [PMC free article] [PubMed]
- 22.Deslich S., Coustasse A. Expanding Technology in the ICU. Telemedicine and e-Health. 2014;20(5):485–92. doi: 10.1089/tmj.2013.0102. [DOI] [PubMed] [Google Scholar]
- 23.Porterfield A., Engelbert K., Coustasse A. Electronic Prescribing: Improving the Efficiency and Accuracy of Prescribing in the Ambulatory Care Setting. Perspectives in Health Information Management. 2014. ). [PMC free article] [PubMed]
- 24.American Recovery and Reinvestment Act (ARRA) Pub. L. 111-5, 123 Stat. 115, 516. 2009. http://www.gpo.gov/fdsys/pkg/PLAW-111publ5/pdf/PLAW_111publ5.pdf19 (accessed October 1, 2013).
- 25.Rogoski R. R. Bridging the EHR Divide: Hospitals, Physician Practices Work toward True Interoperability. Healthcare Informatics. 2012;29(10):8–12. [PubMed] [Google Scholar]
- 26.National eHealth Collaborative. The Patient Engagement Framework. 2012. http://www.nationalehealth.org/patient-engagement-framework (accessed September 16, 2013).
- 27.Anker J., Silver M., Kaushal R. Rapid Growth in Use of Personal Health Records in New York, 2012–2013. Journal of General Internal Medicine. 2014;29(6):850–54. doi: 10.1007/s11606-014-2792-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National eHealth Collaborative. The Patient Engagement Framework.
- 29.Centers for Medicare and Medicaid Services. EHR Incentive Programs. 2013. Available at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/ (accessed January 11, 2014).
- 30.Kaelber D. C., Shah S., Vincent A., Pan E., Hook J. M., Johnston D., Bates D. W., Middleton B. The Value of Personal Health Records. Charlestown, MA: Center for Information Technology Leadership; 2008. Available at http://www.partners.org/cird/pdfs/CITL_PHR_Report.pdf (accessed November 4, 2013). [Google Scholar]
- 31.Brennan P. F., Downs S., Casper G. Project HealthDesign: Rethinking the Power and Potential of Personal Health Records. Journal of Biomedical Informatics. 2010;43(5 (suppl.)):S3–S5. doi: 10.1016/j.jbi.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 32.Fabozzi N. U.S. Patient Portal Market for Hospitals and Physicians: Overview and Outlook, 2012–2017. Frost & Sullivan; 2013. Available at http://www.frost.com/prod/servlet/frost-home.pag (accessed January 11, 2014). [Google Scholar]
- 33.Sujansky & Associates, LLC, on behalf of Project HealthDesign. A Standards-based Model for the Sharing of Patient-generated Health Information with Electronic Health Records. 2013. Available at http://www.projecthealthdesign.org/media/file/Standard-Model-For-Collecting-And-Reporting-PGHI_Sujansky_Assoc_2013-07-18.pdf (accessed October 26, 2013).
- 34. Ibid.
- 35.Hufnagel S. P. Interoperability. Military Medicine. 2009;174(5):43–50. doi: 10.7205/milmed-d-03-9808. [DOI] [PubMed] [Google Scholar]
- 36.Pan E., Johnston J., Walker J., Adler-Milstein J., Bates D. W., Middleton B. The Value of Healthcare Information Exchange and Interoperability. Wellesley, MA: Center for Information Technology Leadership; 2004. [Google Scholar]
- 37.Hufnagel S. P. Interoperability. [DOI] [PubMed]
- 38.Kim J., Jung H., Bates D. History and Trends of ‘Personal Health Record’ Research in PubMed. Healthcare Informatics Research. 2011;17(1):3–17. doi: 10.4258/hir.2011.17.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hufnagel S. P. National Electronic Health Record Interoperability Chronology. [DOI] [PubMed]
- 40. Ibid.
- 41.Center for Biomedical Informatics. Reference Standards. Regenstrief Institute, Inc.; 2013. Available at http://www.regenstrief.org/cbmi/areas-excellence/reference-standards/ (accessed November 5, 2013). [Google Scholar]
- 42.World Health Organization. International Classification of Diseases (ICD). 2013. Available at http://www.who.int/classifications/icd/en/ (accessed November 5, 2013).
- 43.US Food and Drug Administration. National Drug Code Directory. 2013. Available at http://www.fda.gov/Drugs/InformationOnDrugs/ucm142438.htm (accessed November 5, 2013).
- 44.International Health Terminology Standards Development Organization. SNOMED CT. 2013. Available at http://www.ihtsdo.org/snomed-ct/ (accessed November 5, 2013).
- 45.Health Level Seven International. Introduction to HL7 Standards. 2013. Available at http://www.hl7.org/implement/standards/index.cfm?ref=nav (accessed November 5, 2013).
- 46.US Department of Health and Human Services. Information for Health: A Strategy for Building the National Health Information Infrastructure. 2001. Available at http://www.ncvhs.hhs.gov/nhiilayo.pdf (accessed October 1, 2013).
- 47.US Department of Health and Human Services. Report to the Secretary of the U.S. Department of Health and Human Services on Functional Requirements Needed for the Initial Definition of a Nationwide Health Information Network (NHIN) 2006. Available at http://www.ncvhs.hhs.gov/061030lt.pdf (accessed September 18, 2013).
- 48.US Department of Health and Human Services, Agency for Healthcare Research and Quality. Technology Is Improving Patients’ Access to Their Health Information. Available at http://www.innovations.ahrq.gov/content.aspx?id=3732 (accessed October 27, 2013).
- 49.HealthIT.gov. Interoperability Portfolio: Nationwide Health Information Network (NwHIN). 2013. Available at http://www.healthit.gov/policy-researchers-implementers/nationwide-health-information-network-nwhin (accessed October 27, 2013).
- 50. Ibid.
- 51.US Department of Health and Human Services. Report to the Secretary of the U.S. Department of Health and Human Services on Functional Requirements Needed for the Initial Definition of a Nationwide Health Information Network (NHIN)
- 52.Rogoski R. R. Bridging the EHR Divide: Hospitals, Physician Practices Work toward True Interoperability. [PubMed]
- 53.US Department of Health and Human Services. Information for Health: A Strategy for Building the National Health Information Infrastructure.
- 54.Sujansky & Associates, LLC, on behalf of Project HealthDesign. Project HealthDesign—Phase II: Grantee Technical Architectures and Implementations. Robert Wood Johnson Foundation; 2011. Available at http://www.rwjf.org/content/dam/farm/reports/reports/2011/rwjf71294 (accessed May 28, 2014). [Google Scholar]
- 55. Ibid.
- 56.Sujansky & Associates, LLC, on behalf of Project HealthDesign. A Standards-based Model for the Sharing of Patient-generated Health Information with Electronic Health Records.
- 57.Google. Google Health Has Been Discontinued. 2011. Available at http://www.google.com/intl/en_us/health/about/ (accessed October 27, 2013).
- 58.TELUS Health Solutions. What Is TELUS Health Space. 2013. Available at http://telushealthspace.com/en/telushealthspace (accessed October 27, 2013).
- 59.Robert Wood Johnson Foundation. Personal Health Records 101. October 1, 2009. Available at http://www.rwjf.org/en/research-publications/find-rwjf-research/2010/01/feature-the-power-and-potential-of-personal-health-records/chapter-1-personal-health-records-101.html (accessed October 15, 2013).
- 60.US Department of Health and Human Services, Commission on Systemic Interoperability. The Problem and the Solution. Ending the Document Game: Connecting and Transforming Your Healthcare through Information Technology. 2013. Available at http://endingthedocumentgame.gov/PDFs/ProblemSolution.pdf (accessed March 4, 2014). [PubMed]
- 61.Iroju O., Soriyan A., Gambo I., Olaleke J. Interoperability in Healthcare: Benefits, Challenges and Resolutions. International Journal of Innovation and Applied Studies. 2013;3(1):262–70. [Google Scholar]
- 62.Wynia M., Dunn K. Dreams and Nightmares: Practical and Ethical Issues for Patients and Physicians Using Personal Health Records. Journal of Law, Medicine & Ethics. 2010;38(1):64–73. doi: 10.1111/j.1748-720X.2010.00467.x. [DOI] [PubMed] [Google Scholar]
- 63.Jones D. A., Shipman J. P., Plaut D. A., Seiden C. R. Characteristics of Personal Health Records: Findings of the Medical Library Association/National Library of Medicine Joint Electronic Personal Health Record Task Force. Journal of the Medical Library Association. 2010;98(3):243–49. doi: 10.3163/1536-5050.98.3.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.American Health Information Management Association (AHIMA) Choose a PHR. MyPHR. 2013. Available at http://www.myphr.com/resources/choose.aspx (accessed October 26, 2013).
- 65.Witry M., Doucette W., Daly J., Levy B., Chrischilles E. Family Physician Perceptions of Personal Health Records. Perspectives in Health Information Management. 2010. ). [PMC free article] [PubMed]
- 66. Ibid.
- 67.AHIMA e-HIM Personal Health Record Work Group. Defining the Personal Health Record. Journal of AHIMA. 2005;76(6):24–25. [PubMed] [Google Scholar]
- 68.CommonWell Health Alliance. About CommonWell Health Alliance. 2013. Available at http://www.commonwellalliance.org/about (accessed October 27, 2013).
- 69.Cushman R. Primer: Data Protection and the Personal Health Record. Project Health Design ELSI Team; 2007. Available at http://www.projecthealthdesign.org/media/file/primer_data_protection.pdf (accessed October 23, 2013). [Google Scholar]
- 70.AHIMA e-HIM Personal Health Record Work Group. Defining the Personal Health Record.
- 71.US Department of Health and Human Services. Personal Health Records and Personal Health Record Systems: A Report Recommendation from the National Committee on Vital and Health Statistics. 2006. Available at http://www.ncvhs.hhs.gov/0602nhiirpt.pdf (accessed November 4, 2013).
- 72. Ibid.