Abstract
Burkholderia pseudomallei (Bps)is the causative agent of melioidosis and is endemic in regions of northern Australia and Southeast Asia. Bps is inherently resistant to multiple antibiotics and is considered a potential biological warfare agent by the U.S. DHHS. Therefore, effective vaccines are necessary to prevent natural infection and to safeguard against biological attack with this organism. In our previous work we have shown that immunization with naturally derived outer membrane vesicles (OMVs) from Bps provides significant protection against lethal aerosol and systemic infection in BALB/c mice. In this work, we evaluated the safety and immunogenicity of escalating doses of OMV vaccine in rhesus macaques. We show that immunization of rhesus macaques with Bps OMVs generates humoral immuneresponses to protective protein and polysaccharide antigens without any associated toxicity or reactogenicity. These results lay the groundwork for evaluation of protective efficacy of the OMV vaccine in the nonhuman primate model of melioidosis.
Keywords: Burkholderia pseudomallei, Outer membrane vesicle, vaccine, melioidosis, primate
1. Background
Bps is a Gram-negative, facultative-intracellular bacterium and the causative agent of melioidosis. Infection with Bps can manifest as acute septicemia, pneumonia and/or chronic disease and is associated with significant morbidity and mortality. Bps is naturally resistant to multiple antibiotics and there is currently no approved vaccine against the organism.Vaccine strategies against Bps includeinactivated whole cell preparations, live-attenuated strains, purified polysaccharides, glycoconjugates, and protein subunits, amongst others, but none have demonstratedlong term protection and sterilizing immunity in animal models.Outer membrane vesicles (OMVs) are non-replicating particles secreted by Gram-negative bacteria, such as Bps, that range between 50-250 nm in diameter. OMVs are enriched in protein, polysaccharide, and lipid microbial components, including potential immunogens, andcanfacilitate antigen presentation to both B and T cells. OMVsthus represent a multivalent, acellular vaccine platform with a potential forincreased safety and enhanced protection against melioidosis.Our previous studies have shown that Bps OMVs provide protection in an inhalational model of melioidosis in mice.1 We evaluated the safety and immunogenicity of escalating doses of OMV vaccine in rhesus macaques in order to advance the OMV vaccine for testing in a large animal model. We show that immunization of rhesus macaques with Bps OMVs generateshumoralimmune responseswithout any associated toxicity or reactogenicity.
2. Materials and Methods
Preparation of OMV vaccine. B. pseudomallei strain 1026b (BEI Resources) was grown in LB broth at 37°C until late log phase (16–18 hr). The intact bacteria were pelleted by centrifugation at 6,000×g for 10 min at 4°C, and the supernatant was removed and filtered through a 0.22 μm polyethersulfone (PES) filter (Millipore) in order to remove any remaining bacteria or large bacterial fragments. To ensure the supernatant was free of viable bacteria, 1 mL of supernatant was streaked onto PIA agar and incubated 48–72 hrs at 37°C. OMVs were harvested by slowly adding 1.5 M solid ammonium sulfate (Fisher Scientific) while stirring gently and incubated overnight at 4°C. The OMVs were harvested by centrifugation at 11,000×g for 20 min at 4°C. The resulting pellet, consisting of crude vesicles, was resuspended in 60% sucrose (Fisher Scientific) in 30 mM Tris-HCl pH 8.0, filter sterilized through a 0.22 μm PES filter and layered at the bottom of a centrifuge tube. A sucrose gradient was prepared by slowly layering 55%, 50%, 45%, 40%, and 35% sucrose in 30 mM Tris-HCl pH 8.0(w/v) over the crude OMV preparation. Membrane vesicles were collected by ultracentrifugation at 165,000×g for 3 hr at 4°C. Equal fractions were removed sequentially from the top and stored at 4°C. To determine the purity of the fractions, 500 μl of each was precipitated with 20% (w/v) Tri-chloroacetic acid (TCA). The resulting pellet was resuspended in 10 μl phosphate buffered saline (PBS) and 10 μl Laemmli loading buffer (Bio-Rad), boiled for 10 min and loaded onto an SDS-PAGE polyacrylamide gel (4–20% Mini Protean, Bio-Rad) run at 200 V. The working OMV preparation was recovered by pooling the peak fractions (those containing the least amount of insoluble fragments and contaminants) in 30 mM Tris-HCl pH 8.0followed by centrifugation at 165,000×g for 3 hr at 4°C. The resulting pellet, containing OMVs, was then washed and resuspended in LPS-free water. OMVs were quantified with a Bradford Protein Assay (Bio-Rad).
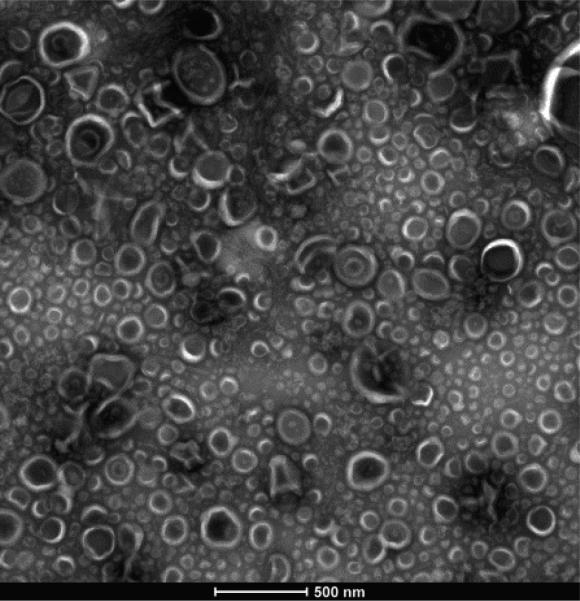
Purified Bps OMVs are negatively stained with 1% uranyl acetate and were imaged by transmission electron microscopy (TEM)to visually confirm their presence and purity. Purified Bps OMVs range in size from 50-250 nm in diameter and are spherical, double membrane structures with an electron dense center.Purified OMV preparations are free of extracellular debris and flagella (Figure 1).
Figure 1. Purified Bps outer membrane vesicles.
Final preparations of OMVs were negatively stained with1% uranyl acetate, and then visualized using TEM. Bar indicates500nm.
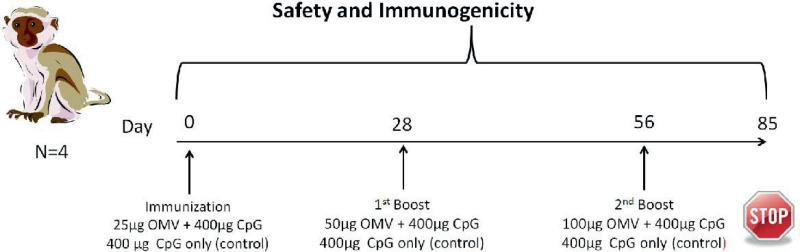
OMV immunization of nonhuman primates.Four male, age- and weight-matched, Indian rhesus macaques (Macacamulatta) were usedinthis study. Two animals (IN71 and II81) were immunizedsubcutaneously (SC) with Bps OMVs admixed with 400 μg CpG oligodeoxynucleotides (ODN)2395 (InvivoGen). Two animals (HM73 and DJ17) were immunized with CpG ODN only and served as controls. Immunizations were performed on days 0, 28, and 56.OMV immunizations were administered using a dose escalation regimen with the first dose containing 25μg, the second dose 50μg, and the third dose 100 μg of OMV. The experimental design in shown in Figure 2.
Figure 2. Experimental design to evaluate BpsOMV vaccine safety and immunogenicity in rhesus macaques.
Animals were immunized with escalating doses of Bps OMVs admixed with CpG ODN (n=2) or CpG ODN alone (n=2).
Blood was obtained prior to immunization (pre-immune) and 4 weeks after each immunization to measure humoral immune responses to OMV vaccination. OMV-, lipopolysaccharide (LPS)-, and capsular polysaccharide (CPS)-specificplasmaIgG were measured by ELISA usingmicrotiter plates coated with purified preparations of OMV, LPS, or CPS. Safety and toxicity of the OMV vaccine was monitored by complete blood chemistry and by daily health examinations.
3. Results
3.1 Assessment of OMV vaccine safety in rhesus macaques
To assess safety of the OMV vaccine formulation, blood chemistry measurements were obtained in OMV-immunized and control macaques. Blood was obtained pre-vaccination and at24, 48, and 72 hr after the first immunization and prior to each booster dose.An increase in blood neutrophil numbers was noted 24 hr after OMV immunization, but neutrophil counts returned to normal range by 72 hr post- immunization. Clinical measurements indicated no changes in liver or kidney function throughout the study(Table 1). The vaccine injection site was also closely examined over the course of immunizations and no erythema, swelling, or necrosis was observed at any time.
Table 1.
Blood chemistry measurements in OMV-immunized and control-immunized macaques. Blood was collected from animals at indicated time points and analyzed using a CBC chemistry panel.IN71, II81 – OMV-immunized; HM73, DJ17 – controls.
| IN71 | Pre-vaccination | Prime 25μg | Boost 50 μg +28 | 2nd Boost 100μg +56 | End Point +85 | II81 | Pre-vaccination | Prime 25μg | Boost 50 μg +28 | 2nd Boost 100μg +56 | End Point +85 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| +1 | +2 | +3 | +1 +2 +3 | ||||||||||||
| ALT (20-126 U/L) | 17 | 36 | 39 | 43 | 17 | 15 | 27 | ALT (20-126 U/L) | 32 | 37 | 47 | 50 | 39 | 39 | 44 |
| AST (25-120 U/L) | 25 | 48 | 50 | 52 | 23 | 22 | 32 | AST (25-120 U/L) | 67 | 33 | 36 | 40 | 36 | 25 | 46 |
| Albumin (3-5.9 g/dL) | 4.3 | 4.0 | 3.9 | 4.2 | 4.2 | 4.3 | 3.7 | Albumin (3-5.9 g/dL) | 4.0 | 4.0 | 3.7 | 4.0 | 4.3 | 4.3 | 3.3 |
| BUN (13-27 mg/dL) | 21 | 18 | 17 | 20 | 19 | 19 | 14 | BUN (13-27 mg/dL) | 14 | 15 | 19 | 19 | 20 | 23 | 21 |
| WBC (6.6-15.5 × 103/UL) | 11.74 | 14.26 | 7.65 | 7.14 | 7.71 | 10.28 | 9.00 | WBC (6.6-15.5 × 103/UL) | 12.49 | 13.96 | 16.01 | 11.89 | 6.7 | 10.84 | 11.10 |
| Neutrophil # (1.4-7.3.0× 103/UL) | 6.71 | 10.14 | 3.51 | 3.25 | 2.65 | 5.03 | 3.10 | Neutrophil # (1.4-7.3.0× 103/UL) | 8.13 | 10.22 | 11.96 | 7.76 | 2.11 | 6.32 | 4.80 |
| Lymphocyte # (2.3-13× 103/UL) | 4.06 | 3.15 | 2.96 | 3.17 | 4.07 | 4.28 | 4.60 | Lymphocyte # (2.3-13× 103/UL) | 3.63 | 3.12 | 3.39 | 3.62 | 4.07 | 3.88 | 4.40 |
| Monocyte # (0.1-1.5× 103/UL) | 0.44 | 0.58 | 0.50 | 0.37 | 0.51 | 0.59 | 1.30 | Monocyte # (0.1-1.5× 103/UL) | 0.37 | 0.43 | 0.32 | 0.32 | 0.28 | 0.35 | 1.90 |
| HM73 | Pre-vaccination | Prime 25μg | Boost 50 μg +28 | 2nd Boost 100μg +56 | End Point +85 | DJ17 | Pre-vaccination | Prime 25μg | Boost 50 μg +28 | 2nd Boost 100μg +56 | End Point +85 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| +1 | +2 | +3 | +1 +2 +3 | ||||||||||||
| ALT (20-126 U/L) | 23 | 22 | 29 | 34 | 26 | 24 | 30 | ALT (20-126 U/L) | 29 | 38 | 29 | 69 | 32 | 31 | 42 |
| AST (25-120 U/L) | 26 | 20 | 31 | 38 | 30 | 27 | 26 | AST (25-120 U/L) | 25 | 43 | 31 | 54 | 22 | 28 | 29 |
| Albumin (3-5.9 g/dL) | 4.2 | 4.2 | 4.1 | 4.3 | 4.4 | 4.5 | 3.5 | Albumin (3-5.9 g/dL) | 4.1 | 4.1 | 4.1 | 4.1 | 4.2 | 4.4 | 3.3 |
| BUN (13-27 mg/dL) | 15 | 20 | 20 | 18 | 18 | 21 | 15 | BUN (13-27 mg/dL) | 19 | 19 | 20 | 15 | 14 | 17 | 15 |
| WBC (6.6-15.5 × 103/UL) | 13.34 | 9.31 | 10.50 | 11.11 | 10.18 | 14.92 | 8.60 | WBC (6.6-15.5 × 103/UL) | 9.13 | 9.13 | 10.50 | 7.50 | 8.52 | 9.48 | 8.40 |
| Neutrophil # (1.4-7.3.0× 103/UL) | 9.21 | 4.66 | 5.63 | 6.16 | 4.50 | 8.11 | 2.40 | Neutrophil # (1.4-7.3.0× 103/UL) | 5.33 | 5.33 | 4.86 | 5.01 | 5.70 | 6.18 | 2.09 |
| Lymphocyte # (2.3-13× 103/UL) | 3.10 | 3.53 | 3.54 | 4.08 | 4.95 | 5.30 | 5.00 | Lymphocyte # (2.3-13× 103/UL) | 3.00 | 3.00 | 2.40 | 1.77 | 2.02 | 2.77 | 2.30 |
| Monocyte # (0.1-1.5× 103/UL) | 0.66 | 0.61 | 0.55 | 0.38 | 0.46 | 0.66 | 1.20 | Monocyte # (0.1-1.5× 103/UL) | 0.29 | 0.29 | 0.30 | 0.21 | 0.37 | 0.25 | 3.20 |
3.2 Assessment of humoral immune responses elicited by OMV immunization of rhesus macaques
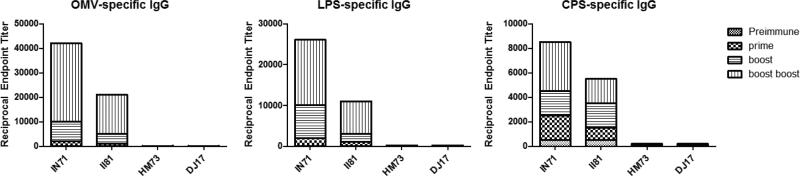
Antibody responses were examinedover the course of the OMV prime-boost-boost immunization. NHPs immunized withBps OMVs produced significantly higher titers of OMV-specific IgG compared to pre-immune sera and sera obtained from control-immunized animals after three immunizations.LPS-and CPS-specific IgG were also measured to determine if humoral immune responses were generated against these known protective antigens. LPS-and CPS-specific serum IgG titers were significantly elevated in OMV-immunized verses controls animals. The LPS-specific IgG response accounted for nearly half of the overall OMV-specific IgG response, while the CPS-specific antibody accounted for approximately 1/5 of the OMV-specific IgG. Taken together, these data demonstrate that Bps OMVs are highly immunogenic and stimulate humoral immunity in immunized rhesus macaques.
4. Conclusion
This work demonstrates the safety and immunogenicity of a Bps OMV vaccine in nonhuman primates.No adverse reactions or toxicity were observed in any macaque that received up to 100 μg OMV indicating that the vaccine is safe at doses equivalent or higher to that previously used in humans2. OMV immunization produced high titers of OMV-, LPS-, and CPS-specific plasmaIgG.The data generated here are encouraging because antibodies directed against OMV, LPS, and CPS are protective in small animal models of melioidosis3. This suggests that the protein and polysaccharide-specific antibody observed in OMV-immunized macaques may confer protectionduringexperimental infection with Bps.Future studies are warranted to evaluate the protective efficacy of the OMV vaccine in a nonhuman primate model of melioidosis.
Figure 3. Bps OMV-specific IgG in plasma of immunized NHPs.
OMV-, LPS-, and CPS-specific plasma IgG isshown for pre-immune samples as well as samples obtained after a primary immunization with 25μg, a boost with 50μg, and a second boost with 100μg of OMV vaccine admixed with CpG. Control animals received 400µg of CpG only at each immunization point. IN71, II81 – OMV-immunized; HM73, DJ17 – controls.
Acknowledgements
This work was supported by a pilot grant from Tulane National Primate Research Center. This work was supported in part through the NIH/OD grant OD-011104-51 (Tulane National Primate Research Center Base grant).
References
- 1.Nieves W, Asakrah S, Qazi O, Brown KA, Kurtz J, Aucoin DP, et al. A naturally derived outer-membrane vesicle vaccine protects against lethal pulmonary Burkholderia pseudomallei infection. Vaccine. 2011;29(46):8381–9. doi: 10.1016/j.vaccine.2011.08.058. PMCID: 3195868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naess LM, Oftung F, Aase A, Wetzler LM, Sandin R, Michaelsen TE. Human T-cell responses after vaccination with the Norwegian group B meningococcal outer membrane vesicle vaccine. Infect Immun. 1998;66(3):959–65. doi: 10.1128/iai.66.3.959-965.1998. PMCID: 108002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones SM, Ellis JF, Russell P, Griffin KF, Oyston PC. Passive protection against Burkholderia pseudomallei infection in mice by monoclonal antibodies against capsular polysaccharide, lipopolysaccharide or proteins. J Med Microbiol. 51(12):1055–62. doi: 10.1099/0022-1317-51-12-1055. 002. [DOI] [PubMed] [Google Scholar]