Abstract
Objectives
To evaluate associations of cardiac biomarkers with in utero antiretroviral (ARV) drug exposures and cardiac function/structure measured by echocardiograms in HIV-exposed but uninfected (HEU) children.
Design and methods
We analyzed the association of three cardiac biomarkers (cardiac troponin T, cTnT; high sensitivity C-reactive protein, hsCRP; and N-terminal pro-brain natriuretic peptide, NT-proBNP) with prenatal ARV exposures, maternal-child characteristics, and echocardiographic parameters.
Results
Among 338 HEU children (mean age=4.3 years), 51% had at least 1 elevated cardiac biomarker. Maternal tobacco use was associated with elevated NT-proBNP (adjusted odds ratio [aOR]=2.28, P=0.02). Maternal alcohol and abacavir use were associated with elevated cTnT levels (aOR=3.56, P=0.01 and aOR=2.33, P=0.04, respectively). Among 94 children with paired echocardiogram-biomarker measurements, cTnT measurements were correlated with increased left ventricular (LV) thickness-to-dimension ratio (r=0.21, P=0.04); and elevated cTnT was associated with higher mean LV end-diastolic (ED) posterior wall thickness (P=0.04). hsCRP measurements were negatively correlated with septal thickness (r=-0.22, P=0.03) and elevated hsCRP was associated with lower mean LV contractility Z-scores (P=0.04). NT-proBNP measurements were correlated with increased LVED dimension (r=0.20, P=0.05) and elevated NT-proBNP was associated with lower mean end-systolic septal thickness (P=0.03).
Conclusion
Our findings suggest that cardiac biomarkers may help identify HEU children who require further cardiac evaluation including echocardiography. Potential cardiac effects of prenatal abacavir exposure in this population need further investigation.
Keywords: cardiac biomarkers, echocardiography, HIV, antiretroviral drugs, pediatric
Introduction
Nearly 9000 HIV-exposed but uninfected (HEU) infants are born in the US each year, and from 85% to nearly 97% were exposed in utero and/or in early infancy to antiretroviral drugs (ARVs) [1,2]. In utero ARV exposure has been associated with significant changes in echocardiographic parameters of left ventricular (LV) structure and function in HEU children within the first two years of life in the HAART era [3]. ARV-exposed HEU infants need to be followed to monitor the long-term safety of these exposures including cardiac health [4].
Cardiac biomarkers which have proven useful in evaluating cardiac status in children with a variety of conditions may be similarly useful in HIV-infected or HEU children [5,6]. In children, serum measurements of cardiac troponins T (cTnT) and I (cTnI) are sensitive and specific for detecting myocardial injury in a variety of settings [7-12]. Elevated NT-proBNP levels are sensitive markers of asymptomatic LV systolic and diastolic dysfunction, as determined by echocardiography [13,14]. Serum high-sensitivity C-reactive protein (hsCRP) is a general inflammatory marker produced in response to infection or inflammation associated with a variety of cardiovascular conditions [15-17].
Echocardiographic screening and monitoring of the thousands of HEU children born annually in the US is not affordable or practical. Cardiac biomarkers could potentially identify which HEU patients might benefit from a more comprehensive clinical assessment including echocardiography. Using data from a cohort of HEU children, we tested two hypotheses: first, that there would be associations between specific maternal ARV regimens and abnormal cardiac biomarker levels and, second, that there would be a significant association between levels of cardiac biomarkers and echocardiographic measurements.
Methods
Study Population
The Surveillance Monitoring for ART Toxicities Study (SMARTT) of the Pediatric HIV/AIDS Cohort Study (PHACS) is a prospective study of the potential adverse outcomes of maternal ARV use on HEU infants and children using longitudinal demographic, anthropomorphic, clinical and laboratory data collected at 22 U.S. pediatric centers. The study protocol was reviewed and approved by the institutional review boards at all sites. Written informed consent was obtained from the children's parent or legal guardian and assent from child participants as appropriate. Details of the SMARTT study design have been described previously [18].
Children underwent a single echocardiogram and blood draw between the ages of 3 and 5 years. Cardiac biomarker evaluation was initiated prior to performing an echocardiogram on all children, and only a subset of children had biomarker assays performed within 3 months of the echocardiogram. Biomarker assays were performed using the repository specimen closest in time to the echocardiogram for participants who had an echocardiogram; the most recently obtained specimen was used for participants who did not have an echocardiogram.
Cardiac Biomarker Assays
For consistency, all specimens were analyzed for cardiac biomarkers at the Clinical Chemistry Laboratory at Boston Children's Hospital: high sensitivity cTnT, with a detection limit of 3 pg/ml and normal value defined as ≤3 pg/ml; hsCRP, with normal defined as ≤1 mg/L); and NT-proBNP, with normal defined as ≤100 pg/ml [10,19,20]. cTnT and NT-proBNP were measured by a quantitative sandwich enzyme immunoassay technique on the Roche E Modular system (Roche Diagnostics, Indianapolis, IN). The concentration of hsCRP was determined using an immunoturbidimetric assay on the Roche P Modular system (Roche Diagnostics, Indianapolis, IN). These biomarkers are stable in cryopreserved specimens [7,21-25].
Child and Maternal Factors and Maternal Antiretroviral Use
Child demographic, anthropometric factors, and birth characteristics (preterm birth [<37 weeks], and low birth weight [<2500 grams]) were considered. Maternal factors included young age at delivery (<25 years), low household income (<$20,000), less than a high school education, viral load >1000 copies/mL, CD4+ T-lymphocyte (CD4) count <250 cells/mm3, and illicit substance use during pregnancy. Intrauterine exposures to individual ARV drugs, ARV drug classes, and highly active antiretroviral therapy (HAART) were examined overall and by trimester. ARV drug classes included nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), nonnucleoside reverse transcriptase inhibitors (NNRTIs), and protease inhibitors (PIs). HAART was defined as at least 3 ARV drugs from at least 2 ARV classes.
Echocardiographic Assessment of Cardiac Structure and Function
An M-mode echocardiogram including 2-D and tissue Doppler imaging was performed by PHACS trained sonographers. Echocardiographic measures were centrally re-measured at the echocardiographic core lab at Boston Children's Hospital to improve measurement reliability. Using normative data from a reference cohort of healthy children from Boston Children's Hospital Echocardiographic Laboratory, echocardiographic parameter Z-scores were calculated. This population was not known to be HIV-infected or ARV-exposed and was not matched to the study cohort for race, ethnicity, or socioeconomic status [26]. Reporting the data as Z-scores adjusts for the effects of variation in age and body surface area.
Statistical Analysis
We calculated the percent of children with elevated levels of each cardiac biomarker, along with exact 95% confidence intervals (CIs) based on a binomial distribution. Logistic regression models were used to assess the association of maternal and infant characteristics and of in utero ARV exposure with abnormal biomarker levels. Child characteristics considered included age at biomarker measurement, sex, race, ethnicity, prematurity, low birth weight, and body mass index (BMI) Z-score. Maternal characteristics included age at delivery of child, household income, educational level, maternal CD4 count and viral load, and use of illicit drugs, alcohol or tobacco during pregnancy. Univariate logistic regression models were first fit for each covariate and those with P<0.20 were considered for inclusion in a multivariate model. The multivariate model was reduced to those covariates with P<0.15 to develop a separate core model for each biomarker. Adjusted logistic regression models were then fit for intrauterine exposure to HAART and for each drug class overall and by trimester, adjusting for potential confounders. Similar analyses evaluating associations between individual ARV agents and elevated cardiac biomarkers were also conducted, restricting to children with intrauterine exposure to HAART to reduce residual confounding. Because prematurity and/or low birth weight may be on the causal pathway between in utero ARV exposure and abnormalities in cardiac biomarkers, sensitivity analyses were also conducted excluding these birth characteristics from models.
The association between cardiac biomarkers with echocardiographic Z-scores was based on a subset of participants (the echocardiogram group) aged 3-5 years who also had an echocardiogram conducted within 3 months of their blood draw and was evaluated in two ways. First, Spearman rank-based correlation coefficients were calculated between cardiac biomarker measurements and each targeted echocardiographic parameter. Secondly, the mean echocardiographic Z-scores were compared between those with elevated versus those with normal biomarker levels in linear regression models adjusting for potential confounders, including age sex, ethnicity, and BMI Z-score. Two sided P values <0.05 were considered statistically significant. Because SMARTT is a safety study, we did not adjust for multiple comparisons in order to minimize the Type II error rate (e.g., the probability of failing to detect true associations). SAS version 9.2 (SAS Institute, Cary, NC) was used to conduct all analyses, based on data submitted as of October 1, 2010.
Results
Study Group
We evaluated 338 children enrolled between March 2007 and June 2009 who had cardiac biomarker measurements obtained at a mean age of 4.3 years (Table 1). Ninety-four of these patients also had an echocardiogram within 3 months of the biomarker measurements. The group was 50% female, 66% non-White, and 43% Hispanic. Almost all subjects (96%) received neonatal prophylaxis with zidovudine for the first six weeks of life, while a small number (N=10, 3%) received zidovudine in combination with at least one other ARV drug as prophylaxis. There were no significant differences between those with versus those without an echocardiogram for any child or maternal characteristic.
Table 1.
Child and Maternal Characteristics of HIV-Exposed Uninfected Children with and without an Echocardiogram within 3 months of the Biomarker Measurement.
| Echocardiogram within 3 months of biomarker | ||||
|---|---|---|---|---|
| Characteristic | No (n = 244) | Yes (n = 94) | Total (n = 338) | P Value |
| Child Demographic and Birth Characteristics | ||||
| Age at biomarker, Mean (SD) | 4.28 (0.82) | 4.22 (0.85) | 4.26 (0.83) | 0.58 |
| BMI Z-score, Mean (SD) | 0.42 (1.39) | 0.38 (1.34) | 0.40 (1.38) | 0.63 |
| Female sex | 122 (50%) | 47 (50%) | 169 (50%) | 1.00 |
| Non-White | 146 (65%) | 60 (70%) | 206 (66%) | 0.50 |
| Latino/Hispanic | 108 (44%) | 36 (38%) | 144 (43%) | 0.33 |
| Gestational age <37 weeks | 43 (18%) | 21 (22%) | 64 (19%) | 0.44 |
| Low birth weight (<2500 grams) | 46 (19%) | 21 (22%) | 67 (20%) | 0.54 |
| Neonatal ARV prophylaxis with zidovudine only | 235 (96%) | 89 (95%) | 324 (96%) | 0.73 |
| Maternal Factors/Exposures during Pregnancy | ||||
| Age <25 years at birth of child | 76 (32%) | 28 (30%) | 104 (31%) | 0.79 |
| Household income <$20,000 | 162 (70%) | 61 (71%) | 223 (71%) | 1.00 |
| Caregiver <HS education | 85 (36%) | 27 (29%) | 112 (34%) | 0.30 |
| Maternal RNA >1000 copies/mL | 35 (16%) | 19 (22%) | 54 (17%) | 0.24 |
| Maternal CD4 <250 cells/mm3 prior to labor and delivery | 22 (10%) | 9 (11%) | 31 (10%) | 0.83 |
| Maternal Substance Use During Pregnancy | ||||
| Illicit drug use | 19 (9%) | 10 (12%) | 29 (10%) | 0.52 |
| Hard drug use (cocaine/opiate) | 6 (3%) | 2 (2%) | 8 (3%) | 1.00 |
| Alcohol use | 17 (8%) | 7 (8%) | 24 (8%) | 1.00 |
| Tobacco use | 43 (20%) | 18 (21%) | 61 (21%) | 1.00 |
BMI=Body mass index; HS=High school; CD4=CD4+ T-cell count; RNA=HIV-1 RNA copies; SD=standard deviation. Percentages are based on non-missing observations, P value by t-test for continuous covariates and by Fisher's Exact test for categorical measures.
Prevalence of Elevated Cardiac Biomarkers
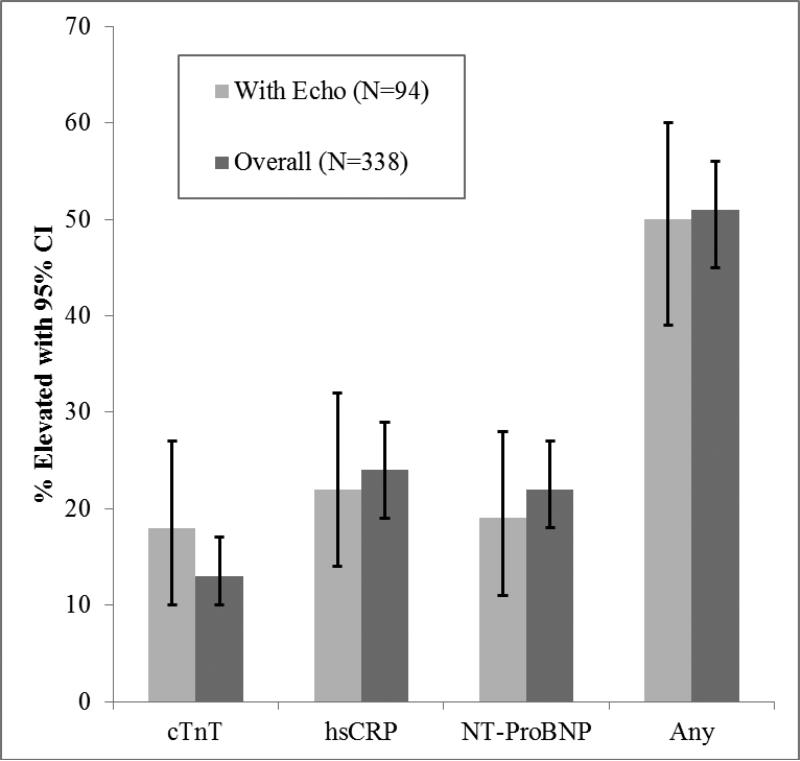
For the 338 children with biomarker measurements, the median level of NT-proBNP was 57.6 pg/ml (IQR=29.8, 94.8), 87% of cTnT results were at or below the limit of detection of 3.0 pg/ml, and the median level of hsCRP was 0.22 mg/L (IQR=0.11, 0.97). No child had an NT-proBNP level in the cardiomyopathy (>100 pg/ml) or heart failure range (>400 pg/ml) [9]. Two children had cTnT measurements which exceeded the 10 pg/ml level (10.9 and 72.4 pg/ml, respectively), the limit of detection of the older, less-sensitive cTnT assay; no child had cTnT measurements in the unstable angina range of 100-200 pg/ml or the acute myocardial infarction range of >200 pg/ml. However, 42/338 children (12%) had a cTnT between 3 and 10 pg/ml, a low-level elevation of unclear clinical significance. Elevated biomarker levels ranged from 13% to 24% (Fig. 1). At least one elevated biomarker value was found in 51% of children.
Figure 1. A comparison of all SMARTT children with elevated biomarkers compared to those with an echocardiogram within 3 months of the biomarker assays.
The percent (%) of study children with elevated cardiac biomarker levels, for those with an accompanying echocardiogram within 3 months of a biomarker assay (n=94) versus the entire study cohort (n=338). cTnT=cardiac troponin T; hsCRP=high-sensitivity C-reactive protein; NT-proBNP=N-terminal pro-brain natriuretic peptide.
Association of Cardiac Biomarkers with Child Demographic and Maternal Factors
Elevated levels of hsCRP were associated with older age at biomarker draw (adjusted Odds Ratio [aOR]=1.42, 95% CI: 1.03, 1.94, P=0.03), while children born prematurely had reduced odds of elevated hsCRP (aOR=0.46, 95% CI: 0.22, 0.97, P=0.04). Elevated NT-proBNP levels were associated with maternal tobacco use (aOR=2.28, 95% CI: 1.13, 4.58, P=0.02); female sex (aOR=1.73, 95% CI: 0.94, 3.18, P=0.08), Hispanic ethnicity (aOR=1.83, 95% CI: 0.99, 3.40, P=0.05), maternal viral load >1000 copies/mL (aOR=2.10, 95% CI: 0.99, 4.46, P=0.05), and marginally with low birth weight (aOR=1.86, 95% CI: 0.92, 3.76, P=0.08). Increased odds of elevated cTnT were associated with younger age of the child (aOR=0.56, 95% CI: 0.38, 0.85, P=0.01), and marginally associated with younger age of the mother at delivery (aOR=0.46, 95% CI: 0.20, 1.07, P=0.07). Maternal alcohol use during pregnancy was associated with more than 3-fold odds of an elevated level of cTnT (aOR=3.56, 95% CI: 1.30, 9.74, P=0.01).
Association of Maternal ARV Exposures and Cardiac Biomarkers
Most (84%) participants had intrauterine exposure to HAART, 97% had exposure to NRTIs (primarily zidovudine and lamivudine), 23% had exposure to NNRTIs (primarily nevirapine), and 69% had exposure to PIs (primarily nelfinavir) (Table 2). With one exception, no significant associations were found between in utero HAART exposures or specific drug classes, either overall or during the 1st trimester, and elevated cardiac biomarkers. Overall exposure to NRTIs was associated with decreased odds of elevated NT-proBNP levels (aOR=0.08, 95% CI: 0.01, 0.85; P=0.04); however, only 3% of participants were unexposed to NRTIs. The only individual ARV drugs for which intrauterine exposure showed associations with elevated cardiac biomarkers after adjustment for maternal and child covariates were abacavir and stavudine. Abacavir exposure was associated with increased odds of elevated cTnT levels (aOR=2.33, 95% CI: 1.03, 5.26; P=0.04). Stavudine was significantly associated with decreased odds of elevated NT-proBNP (aOR=0.13, 95% CI: 0.02, 0.99; P=0.05). In sensitivity analyses excluding birth characteristics (prematurity and low birth weight) from models for NT-proBNP and hsCRP due to the possibility of these measures being part of the causal pathway between in utero ART exposure and elevated cardiac biomarkers, the above findings remained unchanged.
Table 2.
Adjusted Logistic Regression Models for Association of Elevated Biomarker Levels with in utero Antiretroviral Exposure
| Exposure | Percent Exposed | hsCRP* | NT-proBNP† | cTnT‡ | |||
|---|---|---|---|---|---|---|---|
| aOR (95% CI) | P Value | aOR (95% CI) | P Value | aOR (95% CI) | P Value | ||
| Exposure at any time during pregnancy | |||||||
| n = 323 | n = 272 | n = 289 | |||||
| HAART | 84% | 0.91 (0.46, 1.81) | 0.79 | 1.00 (0.43, 2.33) | 0.99 | 1.83 (0.58, 5.70) | 0.30 |
| NRTI | 97% | --- | - | 0.08 (0.01, 0.85) | 0.04 | 0.62 (0.06, 5.91) | 0.67 |
| NNRTI | 23% | 0.73 (0.39, 1.37) | 0.33 | 1.06 (0.53, 2.15) | 0.87 | 1.27 (0.56, 2.87) | 0.57 |
| PI | 69% | 1.09 (0.62, 1.91) | 0.77 | 0.93 (0.48, 1.80) | 0.83 | 1.07 (0.49, 2.32) | 0.87 |
| Exposure During the 1st Trimester of Pregnancy | |||||||
| HAART | 42% | 1.55 (0.93, 2.60) | 0.09 | 0.79 (0.43, 1.46) | 0.45 | 1.22 (0.62, 2.43) | 0.57 |
| NRTI | 50% | 1.44 (0.86, 2.41) | 0.16 | 0.60 (0.33, 1.11) | 0.10 | 0.97 (0.49, 1.93) | 0.93 |
| NNRTI | 13% | 0.93 (0.44, 1.99) | 0.86 | 0.65 (0.25, 1.69) | 0.38 | 1.00 (0.35, 2.83) | 1.00 |
| PI | 32% | 1.57 (0.91, 2.70) | 0.10 | 0.92 (0.48, 1.76) | 0.80 | 1.02 (0.49, 2.09) | 0.97 |
| Exposure to Individual ARV Agents (restricted to children with in utero HAART exposure) | |||||||
| n = 270 | n = 231 | n = 243 | |||||
| Zidovudine | 85% | 1.20 (0.52, 2.80) | 0.67 | 1.39 (0.52, 3.72) | 0.51 | 0.41 (0.17, 1.01) | 0.05 |
| Lamivudine | 59% | 1.27 (0.40, 4.00) | 0.69 | 0.60 (0.21, 1.77) | 0.36 | 0.71 (0.23, 2.15) | 0.54 |
| Abacavir | 25% | 1.08 (0.53, 2.20) | 0.84 | 0.64 (0.26, 1.60) | 0.34 | 2.33 (1.03, 5.26) | 0.04 |
| Didanosine | 7% | 0.54 (0.17, 1.65) | 0.28 | 0.89 (0.24, 3.37) | 0.87 | 0.98 (0.21, 4.64) | 0.98 |
| Stavudine | 8% | 0.45 (0.15, 1.39) | 0.17 | 0.13 (0.02, 0.99) | 0.05 | 0.89 (0.24, 3.31) | 0.86 |
| Tenofovir | 17% | 1.14 (0.56, 2.32) | 0.73 | 1.11 (0.50, 2.46) | 0.79 | 1.37 (0.58, 3.24) | 0.47 |
| Emtricitabine | 4% | 1.22 (0.31, 4.88) | 0.78 | 2.05 (0.55, 7.65) | 0.29 | 0.81 (0.16, 4.10) | 0.79 |
| Efavirenz | 4% | 1.97 (0.53, 7.32) | 0.31 | 1.28 (0.24, 6.78) | 0.77 | 1.51 (0.30, 7.73) | 0.62 |
| Nevirapine | 20% | 0.63 (0.31, 1.29) | 0.21 | 1.06 (0.50, 2.25) | 0.89 | 1.13 (0.46, 2.77) | 0.80 |
| Nelfinavir | 47% | 1.52 (0.85, 2.70) | 0.16 | 0.87 (0.46, 1.68) | 0.69 | 0.56 (0.26, 1.18) | 0.13 |
| Indinavir§ | 3% | --- | - | --- | - | 0.67 (0.07, 6.57) | 0.73 |
| Saquinavir | 4% | 0.49 (0.10, 2.29) | 0.37 | 0.69 (0.13, 3.59) | 0.66 | 0.62 (0.07, 5.09) | 0.65 |
| Lopinavir/Ritonavir | 20% | 0.79 (0.40, 1.55) | 0.49 | 1.10 (0.53, 2.31) | 0.80 | 1.23 (0.56, 2.74) | 0.60 |
aOR=adjusted odds ratio, CI=confidence interval, HAART=highly active antiretroviral therapy, NRTI=nucleoside reverse transcriptase inhibitor, NNRTI=non-nucleoside reverse transcriptase inhibitor, PI=protease inhibitor. NT-proBNP=N-terminal pro-brain natriuretic peptide; hsCRP=high-sensitivity C-reactive protein; cTnT=cardiac troponin T.
Logistic regression models adjusted for:
(hsCRP) - age at biomarker draw and gestational age at birth <37 weeks
(NT-proBNP) - sex, ethnicity, birth weight <2500g, maternal viral load during pregnancy, and maternal tobacco use during pregnancy
(cTnT) - age at biomarker draw, mother's age at delivery, and maternal alcohol use during pregnancy
Unable to estimate odds ratio of elevated biomarker due to small cell counts.
Association between Cardiac Biomarkers and Echocardiographic Parameters
For the 94 children with an echocardiogram within 3 months of a biomarker assay, the mean echocardiographic Z-scores were 0.00 for LV fractional shortening (a load-dependent measure of LV systolic performance), and 0.09 for LV contractility (a load-independent measure of LV systolic performance that reflects the health of the cardiomyocytes), consistent with cardiac functioning in the reference population. However, mean Z-scores for LV thickness-to-dimension ratio (a measure of potential LV remodeling which is LV structural changes of the LV wall thickness and dimension in response to a cardiac injury or insult) (−0.52), and ED septal thickness (a measure of ventricular structure) (−0.23) were significantly below 0 (P<0.0001 and P=0.011, respectively).
Table 3 summarizes the association of cardiac biomarkers with echocardiographic parameter Z-scores, based on both linear regression models comparing mean echocardiographic Z-scores between children with abnormal versus normal biomarker levels and on Spearman correlation coefficients for biomarker levels with echocardiographic Z-scores. The adjusted mean Z-scores for children with abnormal cTnT levels were significantly higher than those for children with normal cTnT levels for LVED posterior wall thickness (a measure of ventricular structure) (mean Z=0.33 versus −0.21, respectively, P=0.04) and LV thickness-to-dimension ratio (mean Z=−0.10 versus -0.61, respectively, P=0.04). Mean end-systolic septal thickness Z-scores were significantly lower in children with elevated NT pro-BNP than children with normal NT pro-BNP (mean Z=−0.89 versus -0.39, P=0.03). In addition, LV contractility Z-scores for children with abnormal hsCRP levels were significantly lower than for those with normal hsCRP (mean Z=−0.37 versus 0.21, P=0.04).
Table 3.
Association of Cardiac Biomarkers with Echocardiographic Z-scores for 94 Children in SMARTT having an Echocardiogram within 3 months of Biomarker Assay
| Comparison of Adjusted* Mean Echocardiographic Z-score between Children with Elevated versus Normal Cardiac Biomarker Levels | Correlation of Z-scores with Continuous Biomarker Level | ||||
|---|---|---|---|---|---|
| Echocardiographic Z-score | Elevated Biomarker Mean (SE) | Normal Biomarker Mean (SE) | P Value | Spearman Correlation Coefficient | P Value |
| hsCRP | |||||
| Contractility | −0.37 (0.24) | 0.21 (0.12) | 0.04 | −0.09 | 0.41 |
| ED Septal Thickness | −0.41 (0.19) | −0.18 (0.10) | 0.30 | −0.22 | 0.03 |
| NT-proBNP | |||||
| LV ED Dimension | 0.29 (0.22) | −0.11 (0.10) | 0.12 | 0.20 | 0.05 |
| ES Septal Thickness | −0.89 (0.20) | −0.39 (0.09) | 0.03 | −0.05 | 0.65 |
| cTnT | |||||
| LV ED Posterior Wall Thickness | 0.33 (0.24) | −0.21 (0.11) | 0.04 | 0.20 | 0.06 |
| LV Thickness-to-Dimension Ratio | −0.10 (0.22) | −0.61 (0.10) | 0.04 | 0.21 | 0.04 |
NT-proBNP=N-terminal pro-brain natriuretic peptide; hsCRP=high-sensitivity C-reactive protein; cTnT=cardiac troponin T, LV=Left ventricular; ED=End-diastolic.
Using continuous measures of biomarker levels, hsCRP was inversely associated with ED septal thickness (correlation coefficient r=−0.22, P=0.03); NT-proBNP was positively associated with LVED dimension (a measure of ventricular structure) (r=0.20, P=0.05); and cTnT was positively associated with LVED thickness-to-dimension ratio (r=0.21, P=0.04).
Discussion
The first study aim was to determine if maternal ARV regimens or specific ARV agents were associated with cardiac biomarkers in HEU infants and children exposed in utero to these agents. No association between elevated cardiac biomarkers and maternal HAART or ARV drug class was found. Analysis of individual ARV agents revealed that abacavir was associated with significantly increased odds of elevated cTnT, suggesting injury or death of cardiomyocytes. Abacavir has been associated with cardiac toxicity, including increased risk of myocardial infarction in HIV-infected adults, although recent reports have challenged this association [27-30]. Although these results are not definitive, they highlight the need for further evaluation of the potential cardiotoxicity of in utero exposure to abacavir. Using cardiac biomarkers, we found no evidence of cardiotoxicity after in utero exposure to other ARVs using observations at a single time point.
We found an association of maternal alcohol use during pregnancy with elevated cTnT levels. Maternal alcohol use during pregnancy has been associated with structural heart defects, long QT syndrome, and heart muscle disease in human, animal, and in vitro studies [31-36]. Maternal tobacco use was associated with significantly increased NT-proBNP levels. Prenatal tobacco exposure is associated with inhibition of cardiac DNA synthesis, impaired vascular smooth muscle structure and function, and structural cardiac defects [36].
The second study aim was to determine if elevated serum cardiac biomarker levels were associated with echocardiographic parameters in HEU infants and children. Higher hsCRP levels were associated with significantly lower ED septal thickness and LV contractility. The NHLBI-funded Cardiovascular Status of HAART Therapy in HIV-Exposed Infants and Children (CHAART-1) study of HEU children found that decreased septal thickness and LV mass were associated with in utero exposure to ARV [4]. The same study found an association between specific cardiac biomarkers and LV echocardiographic parameter changes [37]. The CHAART-1 study found that in utero ARV exposure was associated with increased LV contractility at age 2 years. We found that HEU children in the SMARTT cohort had significantly decreased LV contractility in those with elevated hsCRP who were aged 3-5 years, suggesting the possibility that perhaps HEU children with ongoing generalized inflammation, as indicated by elevated hsCRP, are at risk for decreased LV function as they age. This has implications for recommendations for cardiac screening and follow-up of this group. It has been reported that generalized inflammation in the neonatal period is associated with myocardial injury as measured by cTnT [10]. If such generalized inflammation persists, the expected consequence in later childhood may be decreased septal thickness and perhaps decreased LV contractility. We have previously found that generalized inflammation is associated with echocardiographic abnormalities, myocardial injury, and poorer clinical status in children with heart failure [13, 14]. Ongoing generalized inflammation has been associated with restrictive cardiomyopathy in anthracycline-exposed long-term survivors of childhood cancer [38-40].
Detectable serum cTnT suggests the possibility of active myocardial injury or cardiomyocyte apoptosis [7,41-49]. In this study we found that 12% of SMARTT HEU children had detectable serum cTnT raising concerns that active myocardial injury occurred. We are concerned that these low level cTnT elevations are significantly associated with a higher LV thickness-to-dimension ratio suggesting that low-level cTnT elevations may relate to subclinical changes in LV structure. Although 2 of 338 (0.6%) of SMARTT children had cTnT levels >10 pg/mL, none of them had cTnT levels at the higher levels seen with unstable angina (~100 pg/mL) or myocardial infarction (≥200 pg/mL) in adults. In a previous study of apparently HIV or ART unexposed pediatric outpatients [9], we reported elevated levels of cTnI >0.05 ng/mL in 7.8% of 193 acutely ill children and 4.4% of well children. Four of five children with elevated cTnI, who also had cTnT measured (level of detection=0.01 ng/mL or 10 pg/mL), had highly elevated cTnT levels in the range seen in adults with unstable angina or myocardial infarction. Previously, it had been shown that cTnI accurately shows myocardial injury similar to cTnT [50,51]. Compared to the previous report of cardiac troponin levels in non-HIV or ART exposed children in an outpatient setting [9], the HEU children described in this current report had reassuringly lower rates of active myocardial injury as defined by serum cardiac troponin concentrations. Based on our results, we cannot determine whether elevated cTnT levels in our HEU population are related to HIV or ART exposure, acute febrile illnesses, or other conditions. We do not consider evidence of dead or dying cardiomyocytes, as indicated by measureable cardiac troponin blood concentrations, in healthy children in this age range to be normal.
In active myocardial injury with myocytolysis related to inflammatory heart disease, such as myocarditis, cardiac biopsy specimens often demonstrate a mononuclear intramyocardial infiltrate [52]. This infiltrate is accompanied by interstitial edema with a thicker LV wall by cardiac imaging [53,54]. Therefore, for the subset of children in this study with a measureable cTnT, the association with a thicker LV wall could be consistent with active myocardial inflammation, although similar levels have been reported in 4% of healthy children in one study. Further investigation would be needed to establish the significance of this finding [9].
The association of a greater LV dimension with increased NT-proBNP is consistent with LV neurohormonal activation due to LV stress (cardiomyocyte release of NT-pro BNP in response to increased LV volume or pressure) [55]. The finding of a significant correlation between LV dimension and NT-proBNP, coupled with overall mean decrease in LV thickness-to-dimension ratio and septal thickness for the 94 children with both echocardiographic and biomarker measurements noted above, could be suggestive of early LV remodeling (LV structural changes of the LV wall thickness and dimension in response to a cardiac injury or insult). We have previously reported that in children with heart failure that a 10-fold increase in NT-proBNP serum levels was associated with cardiac symptoms and indices of LV systolic dysfunction and remodeling [13].
Our results suggest that there may be several pathophysiologic processes occurring in some of these patients. An acute and active myocardial injury process may explain the detectable serum cTnT. Acute myocardial hypertrophy may be the results of an inflammatory cardiac process such as myocarditis with an infiltrate and interstitial edema. There also may be a chronic inflammatory process resulting in decreased septal thicknesses and a decrease in the LV thickness-to-dimension ratio consistent with LV remodeling even at 3-5 years of age. The significantly reduced LV thickness-to-dimension ratio overall is consistent with active LV remodeling being present in this population.
Study Limitations
The first limitation of this study is that only a subset (28%) of the children with biomarker measurements had temporally matched cardiac echocardiographic measurements. This affects the power of the study to detect significant associations between these parameters. Secondly, using only a single time point for both cardiac biomarker measurements and echocardiography limits the ability to assess temporal trends and evaluate causal associations. Next, the large number of comparisons between echocardiographic parameters, cardiac biomarker levels, and maternal ARV use means that statistically significant associations could be a result of chance. Analyses were not adjusted for multiple comparisons in order to detect safety signals.
However, the findings of LV structural and functional abnormalities are consistent with other studies and the associations with cardiac biomarkers are biologically plausible. Finally, the clinical significance of these findings is unclear; as is the optimal postnatal time to conduct these measurements to best identify those HEU infants and children who should receive additional longitudinal cardiac follow-up.
Conclusions
We observed no potentially adverse significant associations between specific intrauterine ARV exposures and elevated cardiac biomarkers of abnormal cardiac structure or function, with the exception of a positive association between maternal abacavir use and measureable serum cTnT. Our results highlight the need for further evaluation of the potential for in utero exposure to abacavir to cause adverse cardiac effects in HEU children. HIV strains that are resistant to zidovudine or lamivudine are generally sensitive to abacavir. The largest maternal risk from abacavir use is a hypersensitivity reaction in less than 10% of patients [56]. Hypersensitivity testing has been determined to be cost-effective [57]. The maternal or child health effects of removing abacavir from HAART regimens for pregnant mothers are unknown. The child health cardiac effects of pre-natal abacavir exposures need to be further studied.
We observed associations between elevations of specific biomarkers and echocardiographic parameters consistent with an acute and/or chronic cardiac inflammatory response. The results of this study suggest that there may be a role for cardiac biomarkers to monitor HEU children for increased risk of deleterious cardiac effects that merit echocardiographic evaluation. The cost of these three biomarkers, or a similar panel, is less than $100 while the cost of an echocardiogram is $1000 or more. Future longitudinal studies of these and other, possibly more sensitive and specific, cardiac biomarkers or biomarker combinations in a larger population of HEU infants with echocardiograms could better define the utility of cardiac biomarkers to screen for cardiac changes in this population.
Acknowledgments
J. D. W. designed the study, interpreted the data, and wrote the article. P. L. W. designed the study, analyzed and interpreted the data, and wrote the article. E. L. and B. Z. analyzed the data and wrote the manuscript. W. T. S., S. D. C., G. K. S., L. B. D., G. B. S., and K. C. R. interpreted the data and wrote the manuscript. S. E. L. designed the study, interpreted the data, and wrote the manuscript.
We thank the children and families for their participation in the PHACS protocol “Surveillance Monitoring of ART Toxicities” (SMARTT), and the individuals and institutions involved in the conduct of PHACS SMARTT. The following institutions, clinical site investigators and staff participated in conducting PHACS SMARTT in 2010, in alphabetical order: Baylor College of Medicine: William Shearer, Mary Paul, Norma Cooper, Lynette Harris; Bronx Lebanon Hospital Center: Murli Purswani, Emma Stuard, Anna Cintron; Children's Diagnostic & Treatment Center: Ana Puga, Dia Cooley, Doyle Patton, Deyana Leon; Children's Hospital of Philadelphia: Richard Rutstein, Carol Vincent, Nancy Silverman; Children's Memorial Hospital: Ram Yogev, Margaret Ann Sanders, Kathleen Malee, Scott Hunter; Jacobi Medical Center: Andrew Wiznia, Marlene Burey, Molly Nozyce; New York University School of Medicine: William Borkowsky, Sandra Deygoo, Helen Rozelman; St. Jude Children's Research Hospital: Katherine Knapp, Kim Allison, Megan Wilkins; San Juan Hospital/Department of Pediatrics: Midnela Acevedo-Flores, Lourdes Angeli-Nieves, Vivian Olivera; SUNY Downstate Medical Center: Hermann Mendez, Ava Dennie, Susan Bewley; SUNY Stony Brook: Sharon Nachman, Margaret Oliver, Helen Rozelman; Tulane University Health Sciences Center: Russell Van Dyke, Karen Craig, Patricia Sirois; University of Alabama, Birmingham: Marilyn Crain, Newana Beatty, Dan Marullo; University of California, San Diego: Stephen Spector, Jean Manning, Sharon Nichols; University of Colorado Denver Health Sciences Center: Elizabeth McFarland, Emily Barr, Robin McEvoy; University of Florida/Jacksonville: Mobeen Rathore, Kristi Stowers, Ann Usitalo; University of Illinois, Chicago: Kenneth Rich, Delmyra Turpin, Renee Smith; University of Maryland, Baltimore: Douglas Watson, LaToya Stubbs, Rose Belanger; University of Medicine and Dentistry of New Jersey: Arry Dieudonne, Linda Bettica, Susan Adubato; University of Miami: Gwendolyn Scott, Claudia Florez, Elizabeth Willen; University of Southern California: Toinette Frederick, Mariam Davtyan, Maribel Mejia; University of Puerto Rico Medical Center: Zoe Rodriguez, Ibet Heyer, Nydia Scalley Trifilio. PHACS was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development with co-funding from the National Institute on Drug Abuse, the National Institute on Allergy and Infectious Diseases, the Office of AIDS Research, National Institute of Mental Health, the National Institute of Neurological Diseases and Stoke, the National Institute of Deafness and Other Communication Disorders, the National Heart, Lung, and Blood Institute, the National Institute of Dental and Craniofacial Research, and the National Institute on Alcohol Abuse and Alcoholism, through cooperative agreements with Harvard School of Public Health and Tulane School of Medicine. Data management services were provided by Frontier Science and regulatory services and logistical support by Westat. The conclusions and opinions expressed are those of the authors and do not necessarily reflect those of the NIH or DHHS.
Source of Funding: National Institutes of Health (HD052102; HD052104)
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institutes of Health or the Department of Health and Human Services.
Abbreviation List
- ARV
antiretroviral drugs
- HEU
HIV-exposed, uninfected
- ED
end-diastolic
- LV
left ventricular
- HIV
human immunodeficiency virus
- HAART
highly active antiretroviral therapy
- NRTI
nucleoside reverse transcriptase inhibitor
- NNRTI
non-nucleoside reverse transcriptase inhibitor
- PI
protease inhibitor
Footnotes
Conflicts of Interest: All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
REFERENCES
- 1.Whitmore SK, Zhang X, Taylor AW, Blair JM. Estimated number of infants born to HIV-infected women in the United States and five dependent areas. J Acquir Immune Defic Syndr. 2011;57:218–222. doi: 10.1097/QAI.0b013e3182167dec. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health and Human Services Centers for Disease Control and Disease Prevention HIV Surveillance Supplemental Report: Table 4[serial online] Available at. 2011 http://www.cdc.gov/hiv/surveillance/resources/reports/2010supp_vol16no2/pdf/table4-5.pdf February 17, 2012.
- 3.Lipshultz SE, Shearer WT, Thompson B, Rich KC, Cheng I, Orav EJ, et al. Cardiac effects of antiretroviral therapy in HIV-negative infants born to HIV-positive mothers: NHLBI CHAART-1 (National Heart, Lung, and Blood Institute Cardiovascular Status of HAART Therapy in HIV-Exposed Infants and Children cohort study). J Am Coll Cardiol. 2011;57:76–85. doi: 10.1016/j.jacc.2010.08.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hazra R, Siberry GK, Mofenson LM. Growing up with HIV: children, adolescents, and young adults with perinatally acquired HIV infection. Annu Rev Med. 2010;61:169–185. doi: 10.1146/annurev.med.050108.151127. [DOI] [PubMed] [Google Scholar]
- 5.Lipshultz SE, Fisher SD, Lai WW, Miller TL. Cardiovascular risk factors, monitoring, and therapy for HIV-infected patients. AIDS. 2003;17(Suppl 1):S96–S122. doi: 10.1097/00002030-200304001-00014. [DOI] [PubMed] [Google Scholar]
- 6.Lipshultz SE, Miller TL, Scully RE, Lipsitz SR, Rifai N, Silverman LB, et al. Changes in cardiac biomarkers during doxorubicin treatment of pediatric patients with high-risk acute lymphoblastic leukemia: associations with long-term echocardiographic outcomes. J Clin Oncol. E-pub ahead of print. 2012 Feb 27; doi: 10.1200/JCO.2010.30.3404. doi: 10.1200/JCO.2010.30.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipshultz SE, Rifai N, Sallan SE, Lipsitz SR, Dalton V, Sacks DB, et al. Predictive value of cardiac troponin T in pediatric patients at risk for myocardial injury. Circulation. 1997;96:2641–2648. doi: 10.1161/01.cir.96.8.2641. [DOI] [PubMed] [Google Scholar]
- 8.Lipshultz SE, Somers MJ, Lipsitz SR, Colan SD, Jabs K, Rifai N. Serum cardiac troponin and subclinical cardiac status in pediatric chronic renal failure. Pediatrics. 2003;112:79–86. doi: 10.1542/peds.112.1.79. [DOI] [PubMed] [Google Scholar]
- 9.Lipshultz SE, Wong JC, Lipsitz SR, Simbre VC, 2nd, Zareba KM, Galpechian V, et al. Frequency of clinically unsuspected myocardial injury at a children's hospital. Am Heart J. 2006;151:916–922. doi: 10.1016/j.ahj.2005.06.029. [DOI] [PubMed] [Google Scholar]
- 10.Lipshultz SE, Simbre VC, 2nd, Hart S, Rifai N, Lipsitz SR, Reubens L, et al. Frequency of elevations in markers of cardiomyocyte damage in otherwise healthy newborns. Am J Cardiol. 2008;102:761–766. doi: 10.1016/j.amjcard.2008.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soongswang J, Durongpisitkul K, Nana A, Laohaprasittiporn D, Kangkagate C, Punlee K, et al. Cardiac troponin T: a marker in the diagnosis of acute myocarditis in children. Pediatr Cardiol. 2005;26:45–49. doi: 10.1007/s00246-004-0677-6. [DOI] [PubMed] [Google Scholar]
- 12.Lipshultz SE, Rifai N, Dalton VM, Levy DE, Silverman LB, Lipsitz SR, et al. The effect of dexrazoxane on myocardial injury in doxorubicin-treated children with acute lymphoblastic leukemia. N Engl J Med. 2004;351:145–153. doi: 10.1056/NEJMoa035153. [DOI] [PubMed] [Google Scholar]
- 13.Ratnasamy C, Kinnamon DD, Lipshultz SE, Rusconi P. Associations between neurohormonal and inflammatory activation and heart failure in children. Am Heart J. 2008;155:527–533. doi: 10.1016/j.ahj.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Rusconi PG, Ludwig DA, Ratnasamy C, Mas R, Harmon WG, Colan SD, et al. Serial measurements of serum NT-proBNP as markers of left ventricular systolic function and remodeling in children with heart failure. Am Heart J. 2010;160:776–783. doi: 10.1016/j.ahj.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cesari M, Penninx BW, Newman AB, Kritchevsky SB, Nicklas BJ, Sutton-Tyrrell K, et al. Inflammatory markers and onset of cardiovascular events: results from the Health ABC study. Circulation. 2003;108:2317–2322. doi: 10.1161/01.CIR.0000097109.90783.FC. [DOI] [PubMed] [Google Scholar]
- 16.Kaneko K, Kanda T, Hasegawa A, Suzuki T, Kobayashi I, Nagai R. C-reactive protein as a prognostic marker in lymphocytic myocarditis. Jpn Heart J. 2000;41:41–47. doi: 10.1536/jhj.41.41. [DOI] [PubMed] [Google Scholar]
- 17.Pye M, Rae AP, Cobbe SM. Study of serum C-reactive protein concentration in cardiac failure. Br Heart J. 1990;63:228–230. doi: 10.1136/hrt.63.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams PL, Seage GR, III, Van Dyke RB, Siberry GK, Griner R, Tassiopoulos K, et al. for the Pediatric HIV/AIDS Cohort Study A trigger-based design for evaluating the safety of antiretroviral exposure in uninfected children of HIV-infected mothers. Am J Epidemiol. 2012;175:950–961. doi: 10.1093/aje/kwr401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilkinson JD, Lee DJ, Arheart KL. Secondhand smoke exposure and C-reactive protein levels in youth. Nicotine Tob Res. 2007;9:305–307. doi: 10.1080/14622200601080299. [DOI] [PubMed] [Google Scholar]
- 20.Quest Diagnostics. Congestive Heart Failure (CHF) Risk Testing [serial online] 2011 Available at: http://www.questdiagnostics.com/hcp/topics/bnp/bnp.html July 13, 2011.
- 21.Agarwal SK, Avery CL, Ballantyne CM, Catellier D, Nambi V, Saunders J, et al. Sources of variability in measurements of cardiac troponin T in a community-based sample: the atherosclerosis risk in communities study. Clin Chem. 2011;57:891–897. doi: 10.1373/clinchem.2010.159350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilkins J, Gallimore JR, Moore EG, Pepys MB. Rapid automated high sensitivity enzyme immunoassay of C-reactive protein. Clin Chem. 1998;44:1358–1361. [PubMed] [Google Scholar]
- 23.Ledue TB, Rifai N. Preanalytic and analytic sources of variations in C-reactive protein measurement: implications for cardiovascular disease risk assessment. Clin Chem. 2003;49:1258–1271. doi: 10.1373/49.8.1258. [DOI] [PubMed] [Google Scholar]
- 24.Nowatzke WL, Cole TG. Stability of N-terminal pro-brain natriuretic peptide after storage frozen for one year and after multiple freeze-thaw cycles. Clin Chem. 2003;49:1560–1562. doi: 10.1373/49.9.1560. [DOI] [PubMed] [Google Scholar]
- 25.Cauliez B, Guignery J, Marinier S, Mariau I, Lavoinne A. Two-year stability of NT-proBNP in frozen samples using the Roche Elecsys system. Ann Clin Biochem. 2008;45:318–319. doi: 10.1258/acb.2007.007187. [DOI] [PubMed] [Google Scholar]
- 26.Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. J Appl Physiol. 2005;99:445–457. doi: 10.1152/japplphysiol.01144.2004. [DOI] [PubMed] [Google Scholar]
- 27.D:A:D Study Group. Sabin CA, Worm SW, Weber R, Reiss P, El-Sadr W, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet. 2008;371:1417–1426. doi: 10.1016/S0140-6736(08)60423-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ding X, Andraca-Carrera E, Cooper C, Miele P, Kornegay C, Soukup M, et al. No association of myocardial infarction with ABC use: an FCA meta-analysis.. Abstract presented at: 18th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, MA. February 28, 2011. [Google Scholar]
- 29.Durand M, Sheehy O, Baril JG, Lelorier J, Tremblay CL. Association between HIV infection, antiretroviral therapy and risk of acute myocardial infarction: a cohort and nested case-control study using Quebec's public health insurance database (RAMQ). J Acquir Immune Defic Syndr. 2011;57:245–253. doi: 10.1097/QAI.0b013e31821d33a5. [DOI] [PubMed] [Google Scholar]
- 30.Sax P. Abacavir and cardiovascular risk: still no clarity. Journal Watch HIV/AIDS Clinical Care [serial online] Available at: http://aids-clinical-care.jwatch.org/cgi/content/full/2011/627/1 June 27, 2011.
- 31.Krasemann T. QT prolongation in the newborn and maternal alcoholism. Cardiol Young. 2004;14:565–566. doi: 10.1017/S1047951104005177. [DOI] [PubMed] [Google Scholar]
- 32.Krasemann T, Klingebiel S. Influence of chronic intrauterine exposure to alcohol on structurally normal hearts. Cardiol Young. 2007;17:185–188. doi: 10.1017/S1047951107000224. [DOI] [PubMed] [Google Scholar]
- 33.Löser H, Pfefferkorn JR, Themann H. Alcohol in pregnancy and fetal heart damage. Klin Padiatr. 1992;204:335–339. doi: 10.1055/s-2007-1025368. [DOI] [PubMed] [Google Scholar]
- 34.Adickes ED, Mollner TJ, Makoid MC. Teratogenic effects of ethanol during hyperplastic growth in cardiac myocyte cultures. Alcohol Clin Exp Res. 1993;17:988–992. doi: 10.1111/j.1530-0277.1993.tb05653.x. [DOI] [PubMed] [Google Scholar]
- 35.Wold LE, Norby FL, Hintz KK, Colligan PB, Epstein PN, Ren J. Prenatal ethanol exposure alters ventricular myocyte contractile function in the offspring of rats: influence of maternal Mg2+ supplementation. Cardiovasc Toxicol. 2001;1:215–224. doi: 10.1385/ct:1:3:215. [DOI] [PubMed] [Google Scholar]
- 36.Mone SM, Gillman MW, Miller TL, Herman EH, Lipshultz SE. Effects of environmental exposures on the cardiovascular system: prenatal period through adolescence. Pediatrics. 2004;113:1058–1069. [PubMed] [Google Scholar]
- 37.Wilkinson J, Cheng I, Thompson B, Rifai N, Shearer WT, Rich KC, et al. Are cardiac biomarkers useful in assessing cardiac structure and function in children exposed to the human immunodeficiency virus in utero?. Abstract presented at: Pediatric Academic Societies (PAS); Baltimore, MD.. May 4, 2009. [Google Scholar]
- 38.Lipshultz SE, Lipsitz SR, Sallan SE, Dalton VM, Mone SM, Gelber RD, et al. Chronic progressive cardiac dysfunction years after doxorubicin therapy for childhood acute lymphoblastic leukemia. J Clin Oncol. 2005;23:2629–2636. doi: 10.1200/JCO.2005.12.121. [DOI] [PubMed] [Google Scholar]
- 39.Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP. Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med. 1991;324:808–815. doi: 10.1056/NEJM199103213241205. [DOI] [PubMed] [Google Scholar]
- 40.Lipshultz SE, Lipsitz SR, Mone SM, Goorin AM, Sallan SE, Sanders SP, et al. Female sex and drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Engl J Med. 1995;332:1738–1743. doi: 10.1056/NEJM199506293322602. [DOI] [PubMed] [Google Scholar]
- 41.Newby LK, Rodriguez I, Finkle J, Becker RC, Hicks KA, Hausner E, et al. Troponin measures during drug development-considerations for monitoring and management of potential cardiotoxicity: an educational collaboration among the Cardiac Safety Research Consortium, the Duke Clinical Research Institute, and the US Food and Drug Administration. Am Heart J. 2011;162:64–73. doi: 10.1016/j.ahj.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 42.Herman EH, Lipshultz SE, Rifai N, Zhang J, Papoian T, Yu Z-X, et al. Cardiac troponin T: Elevated serum levels and loss from cardiac myocytes in doxorubicin toxicity. Cancer Research. 1998;58:195–197. [PubMed] [Google Scholar]
- 43.Herman EH, Zhang J, Lipshultz SE, Rifai N, Chadwick D, Takeda, et al. Correlation between serum levels of cardiac troponin–T and the severity of chronic cardiomyopathy induced by doxorubicin. J Clin Oncol. 1999;17:2237–2243. doi: 10.1200/JCO.1999.17.7.2237. [DOI] [PubMed] [Google Scholar]
- 44.Herman EH, Zhang J, Rifai N, Lipshultz SE, Hasinoff BB, Chadwick DP, et al. The use of serum levels of cardiac troponin T to compare the protective activity of dexrazoxane against doxorubicin- and mitoxantrone-induced cardiotoxicity. Cancer Chemother Pharmacol. 2001;48:297–304. doi: 10.1007/s002800100348. [DOI] [PubMed] [Google Scholar]
- 45.Herman E, Zhang J, Knapton A, Lipshultz SE, Rifai N, Sistare F. Serum cardiac troponin T as a biomarker for acute myocardial injury induced by low doses of isoproterenol in rats. Cardiovasc Toxicol. 2006;6:211–221. doi: 10.1385/ct:6:3:211. [DOI] [PubMed] [Google Scholar]
- 46.Zhang J, Knapton A, Lipshultz SE, Weaver JL, Herman EH. Isoproterenol-induced cardiotoxicity in Sprague-Dawley rats: correlation of reversible and irreversible myocardial injury with release of cardiac troponin T and roles of iNOS in myocardial injury. Toxicol Pathol. 2008;36:277–278. doi: 10.1177/0192623307313010. [DOI] [PubMed] [Google Scholar]
- 47.Thompson KL, Rosenzweig BA, Zhang J, Knapton AD, Honchel R, Lipshultz SE, et al. Early alterations in heart gene expression profiles associated with doxorubicin cardiotoxicity in rats. Cancer Chemother Pharmacol. 2010;66:303–314. doi: 10.1007/s00280-009-1164-9. [DOI] [PubMed] [Google Scholar]
- 48.Berridge BR, Pettit S, Walker DB, Jaffe AS, Schultze AE, Herman E, et al. A transformational approach to detecting drug-induced cardiac injury with cardiac troponins: consensus and recommendations from the Cardiac Troponins Biomarker Working Group of the Health and Environmental Sciences Institute. Am Heart J. 2009;158:21–29. doi: 10.1016/j.ahj.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 49.Lipshultz SE. Ventricular dysfunction clinical research in infants, children and adolescents. Prog Ped Cardiol. 2000;12:1–28. doi: 10.1016/s1058-9813(00)00076-x. [DOI] [PubMed] [Google Scholar]
- 50.Herman E, Knapton AD, Rosen E, Zhang J, Estis J, Agee SJ, et al. Baseline serum cardiac troponin I concentrations in Sprague-Dawley, spontaneous hypertensive, Wistar, Wistar-Kyoto, and Fisher rats as determined with an ultrasensitive immunoassay. Toxicol Pathol. 2011;39:653–663. doi: 10.1177/0192623311406931. [DOI] [PubMed] [Google Scholar]
- 51.Dunn ME, Coluccio D, Hirkaler G, Mikaelian I, Nicklaus R, Lipshultz SE, et al. The complete pharmacokinetic profile of serum cardiac troponin I in the rat and the dog. Toxicol Sci. 2011;123:368–373. doi: 10.1093/toxsci/kfr190. [DOI] [PubMed] [Google Scholar]
- 52.Cooper LT., Jr Myocarditis. N Engl J Med. 2009;360:1526–1538. doi: 10.1056/NEJMra0800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schultheiss HP, Kuhl U. Viral myocarditis: diagnosis, aetiology and management. Drugs. 2009;69:1287–1302. doi: 10.2165/00003495-200969100-00001. [DOI] [PubMed] [Google Scholar]
- 54.Cocker M, Friedrich MG. Cardiovascular magnetic resonance of myocarditis. Curr Cardiol Rep. 2010;12:82–89. doi: 10.1007/s11886-009-0077-x. [DOI] [PubMed] [Google Scholar]
- 55.Lim P, Monin JL, Monchi M, Garot J, Pasquet A, Hittinger L, et al. Predictors of outcome in patients with severe aortic stenosis and normal left ventricular function: role of B-type natriuretic peptide. Eur Heart J. 2004;25:2048–2053. doi: 10.1016/j.ehj.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 56.Hetherington S, McGuirk S, Powell G, Cutrell A, Naderer O, Spreen B, et al. Hypersensitivity reactions during therapy with the nucleoside reverse transcriptase inhibitor abacavir. Clin Ther. 2001;23:1603–1614. doi: 10.1016/s0149-2918(01)80132-6. [DOI] [PubMed] [Google Scholar]
- 57.Hughes DA, Vilar FJ, Ward CC, Alfirevic A, Park BK, Pirmohamed M, et al. Cost-effectiveness analysis of HLA B*5701 genotyping in preventing abacavir hypersensitivity. Pharmacogenetics. 2004;14:335–342. doi: 10.1097/00008571-200406000-00002. [DOI] [PubMed] [Google Scholar]