Abstract
Background
Curative parathyroidectomy for primary hyperparathyroidism (PHPT) resolves various nonspecific symptoms related to the disease. Between 8 to 40% of patients with normocalcemia after parathyroidectomy have persistently elevated parathyroid hormone levels (ePTH) at follow-up. We investigated whether ePTH in the early post-operative period was associated with the timing of symptom improvement.
Materials and Methods
This prospective study included adult patients with PHPT who underwent curative parathyroidectomy from November 2011 to September 2012. Biochemical testing 2 weeks post-operatively identified ePTH (defined as PTH > 72 pg/mL) versus normal PTH (nPTH). A questionnaire administered pre- and post-operatively at 6 weeks and 6 months asked patients to rate the frequency of 18 symptoms of PHPT on a 5-point Likert scale. Student’s T-tests were used to compare pre- to post-operative changes in scores for individual symptoms.
Results
Of 194 patients that underwent parathyroidectomy, 129 (66%) participated in the study. Pre-operatively, all patients were symptomatic, with a mean of 13±4 symptoms. Two weeks post-operatively, 20 patients (16%) had ePTH. The percentage of patients with post-operative improvement for individual symptoms was compared between groups. At the early time point (6 weeks), the ePTH group showed less improvement in 14 of 18 symptoms. This difference reached statistical significance for four symptoms: anxiety, constipation, thirst, and polyuria. By the 6 month time point, these differences had resolved and symptom improvement was similar between groups.
Conclusions
Elevated PTH after curative parathyroidectomy may result in a delay in symptom improvement 6 weeks post-operatively, however, this difference resolves by 6 months.
Keywords: Primary hyperparathyroidism, parathyroidectomy, prognosis, timing, symptom improvement, elevated parathyroid hormone
Introduction
Primary hyperparathyroidism (PHPT) is one of the most common endocrine disorders in the United States, with approximately 100,000 new cases diagnosed each year1,2. Parathyroidectomy is the definitive treatment. It restores normocalcemia – the criteria by which cure is defined – and also generally alleviates the numerous typical and nonspecific symptoms of PHPT. Nontraditional symptoms associated with PHPT include musculoskeletal pain and fatigue, insomnia, gastrointestinal and urinary problems, and neuropsychiatric complaints such as depression, anxiety, and irritability1,3–12.
Interestingly, between 8 to 40% of patients with normocalcemia after parathyroidectomy have persistently elevated parathyroid hormone (ePTH) levels at follow-up, ranging anywhere from 1–2 weeks to 5 years post-operatively2,13–15. The pathophysiology and significance of this phenomenon is unclear, though several studies have investigated possible etiologies, which include impaired renal function, bone remineralization, and vitamin D deficiency14,16–18. Factors associated with ePTH are varied and inconsistent across studies but include: high pre-operative PTH, low pre-operative vitamin D, advanced age, and higher adenoma volume2,14,18. Studies investigating whether ePTH confers a higher risk of persistent or recurrent PHPT also have inconsistent conclusions. Evidence supports that a great majority of ePTH patients do not develop recurrent disease, however, comparatively, their risk of developing recurrent disease may be higher than patients with normal PTH (nPTH) levels2,15,19. Despite the research focusing on ePTH and the risk of recurrence of PHPT, no studies have investigated the association between post-operative ePTH and symptom improvement after curative parathyroidectomy for PHPT. A better understanding of the relationship of ePTH and symptom frequency and improvement would aid clinicians in more effectively counseling patients in the post-operative period, as well as determining an appropriate follow-up strategy. Therefore, the objectives of this study were to: 1) determine the incidence of post-operative ePTH in patients with normocalcemia after curative parathyroidectomy for PHPT; 2) investigate whether ePTH in the early post-operative period was associated with changes in the extent or timing of symptom improvement; and 3) determine if ePTH affects overall symptom improvement.
Materials and Methods
Patients
This is a prospective study of patients with PHPT who underwent parathyroidectomy between November 2011 and October 2012 at a large academic tertiary care center in the Midwest. Identification of patients with PHPT was made by biochemical diagnosis, which is defined as hypercalcemia (serum calcium >10.2 mg/dL) with an elevated or inappropriately normal PTH level. Patients were excluded if their operation was not curative, which was defined as patients with continued hypercalcemia (serum calcium level >10.2 mg/dL) at 6 months post-parathyroidectomy. Additional exclusion criteria included patients <18 years old, having undergone a previous parathyroidectomy, unable to read or understand English, or those who declined to participate in post-operative follow-up questionnaires. There were no significant differences in gender, age, or parathyroid pathology between study participants and non-participants (Table 1). Data including patient age and gender, biochemical profile, operative procedure, and histologic information was collected at the pre-operative visit and two follow-up appointments at approximately 2 weeks and 6 months after surgery. Consent was obtained from patients for study participation during the initial surgical consultation, and specifically, all patients consented to receiving phone calls from our research team intermittently during the post-operative period.
Table 1.
Comparison of demographic and pathologic profile of study participants and non-participants showed no significant differences.
| Study Participants (n=129) |
Study Non-participants (n=65) |
P value | |
|---|---|---|---|
| Sex | 0.59 | ||
| M | 26 (20%) | 11 (17%) | |
| F | 103 (80%) | 54 (83%) | |
| Age (y) | 59.7 | 59.7 | 0.99 |
| Pathology | 0.24 | ||
| Single adenoma | 101 (78%) | 43 (68%) | |
| Double adenoma | 14 (11%) | 9 (14%) | |
| Four-gland hyperplasia | 14 (11%) | 12 (18%) | |
Questionnaire
The questionnaire (Appendix) is a disease-specific tool previously developed and applied by this institution11 and was used to assess the extent of 18 varied non-specific symptoms associated with PHPT. Patients reported the frequency of symptom occurrence according to a 5-point Likert scale (0 = never, 1 = rarely, 2 = occasionally, 3 = frequently, 4 = very frequently). The questionnaire was administered during the initial surgical consultation pre-operatively and again at the two follow-up appointments 2 weeks and 6 months after surgery. In addition, patients were contacted by telephone by one of two trained research assistants 6 weeks post-operatively and asked to complete the questionnaire over the phone. For ease of presentation the post-operative time points will herein be referred to as ‘6 week’ and ‘6 month’, although the median questionnaire completion times were 7.1 weeks (Interquartile Range = IQR, 6.0 to 7.8 weeks) and 6.9 months (IQR, 6.0 to 7.3 months). Of note, the 6 month questionnaire was typically completed at the post-operative appointment, however, in a few instances it was collected over the telephone if the patient did not return to clinic.
Statistical Analysis
Statistical analysis was performed by using the SPSS packages (SPSS version 12.0 for Microsoft Windows; SPSS Inc., Chicago, Illinois). Data are expressed either as mean with standard deviation for continuous, normally distributed variables, or as the median with IQR for non-normally distributed variables. Frequency distributions were calculated for each symptom pre-operatively. Rather than imputing missing responses, individual unreported values were excluded from the analyses.
Student’s T-Test, Fischer’s Exact Test, and chi square analysis were used to identify possible factors associated with ePTH or nPTH status. Likert scale data was dichotomized for each symptom into patients showing improvement post-operatively (i.e. a decrease in the frequency of symptoms by one or more increments), versus those who did not. For each symptom, the percentage of patients showing improvement was determined for each time point. Likert sum scores were also compared with Student’s T-Test. The institutional review board from the University of Wisconsin approved this study.
Results
A total of 194 patients who underwent a parathyroidectomy were eligible for the study, and 129 (66%) participated. All patients completed the questionnaire pre-operatively, and 91% and 88% of patients completed the post-operative questionnaires at 6 weeks and 6 months after surgery, respectively. In total, 103 patients completed the questionnaire at all time points.
The mean age of the cohort was 59.7 ± 12.8 years and 80% (n=103) were female. The majority of patients had a single parathyroid adenoma excised (n=101, 78%), whereas 14 patients had double adenomas, and the remaining 14 patients had four-gland hyperplasia. Two patients experienced transient hypocalcemia post-operatively, one patient had transient hoarseness, and one had bone hunger. There were no occurrences of permanent complications.
Pre-operative mean serum calcium and PTH levels were characteristically elevated (10.8 ± 0.7 mg/dL, 107 ± 58 pg/mL) and normalized after parathyroidectomy (9.2 ± 0.77 mg/dL, 46 ± 37 pg/mL). Vitamin D (D-25-OH), measured pre-operatively, had a mean of 31.5 ± 15.0 ng/mL (optimal range 30–80 ng/mL). Post-operatively, 108 patients (84%) had nPTH at the 2 week follow-up appointment, whereas 20 patients (16%) had ePTH.
Overall Symptom Frequency and Severity
Pre-operatively, patients reported a mean of 13 ± 4 symptoms, and no patients were truly asymptomatic. Preliminary analysis on the entire set of patients showed improvement for each symptom at 6 weeks and at 6 months as compared to pre-operative scores, with 6 week improvement generally greater than 6 month improvement11. The mean pre-operative Likert sum score for all patients was 30.7 ± 14.1, which improved to 16.1 ± 10.0 at 6 weeks, and slightly increased to 18.4 ± 10.7 at 6 months.
Comparison of nPTH to ePTH patients
The 20 (16%) patients with an ePTH post-operatively were compared to the 108 patients (84%) that had nPTH at the 2 week follow-up appointment (Table 2). There was no difference between genders, and patients with ePTH tended to be older than those with nPTH (65.7 ± 11.9 vs. 58.5 ± 12.8 years old, p=0.02). Pre-operative PTH was higher for the ePTH group (p < 0.001), and pre-operative vitamin D levels were slightly lower for ePTH patients although this did not reach statistical significance.
Table 2.
Potential factors associated with PTH elevation at two weeks
| nPTH (n=108) |
ePTH (n=20) |
P value | |
|---|---|---|---|
| Sex | 0.76 | ||
| M | 22 (20%) | 3 (15%) | |
| F | 86 (80%) | 17 (85%) | |
| Age (y) | 58.5 | 65.7 | 0.02 |
| Pre-Operative | |||
| Calcium (mg/dL) | 10.9 | 10.3 | 0.01 |
| PTH (pg/mL) | 99.0 | 147.2 | < 0.001 |
| Vitamin D (D-25-OH, ng/mL) | 32.6 | 26.9 | 0.13 |
| 2 week Post-Operative | |||
| Calcium (mg/dL) | 9.3 | 8.9 | 0.03 |
| PTH (pg/mL) | 34.4 | 113.0 | < 0.001 |
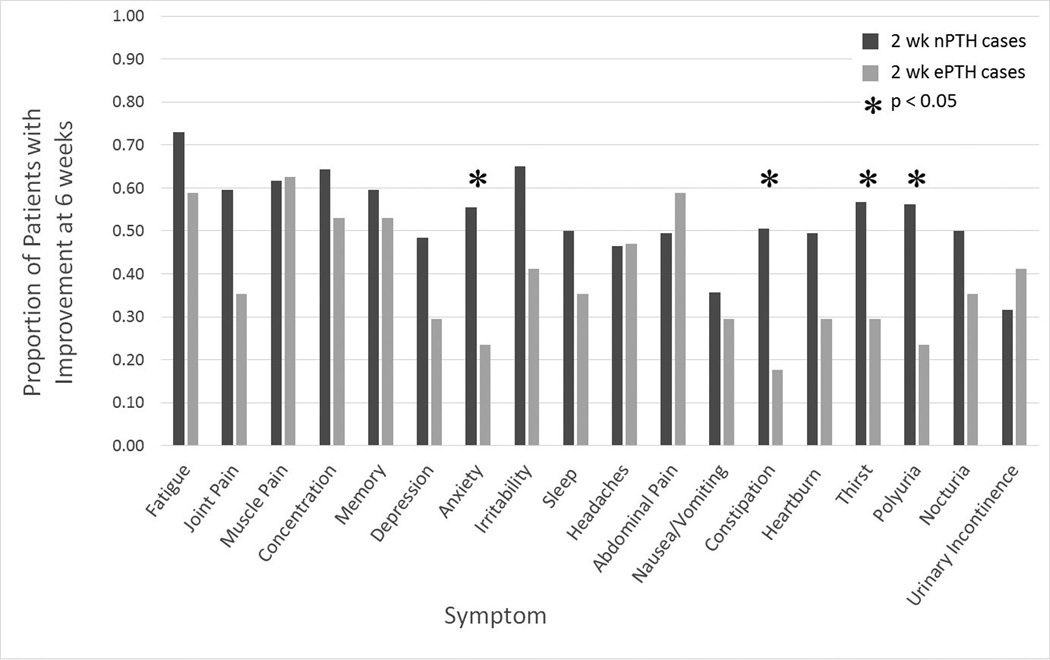
Next, for each individual symptom, improvement at both 6 weeks and 6 months was compared between patients who had ePTH versus nPTH as measured at 2 weeks. At 6 weeks, the percentage of patients who showed improvement was higher in the nPTH group for fourteen out of eighteen symptoms (Figure 1). This difference reached statistical significance for four symptoms: anxiety, thirst, constipation, and polyuria. Differences for joint pain and irritability nearly reached statistical significance (p=0.06). These differences had decreased by the 6 month time point. Although the 2 week nPTH group still had a higher percentage of patients with improvement in fifteen out of eighteen symptoms than the ePTH patients, the magnitude of the difference was less (data not shown, p=NS). There was no statistically significant difference between groups in the percentage of patients that reported improvement at 6 months.
Figure 1.
Individual symptom improvement at 6 weeks compared between patients with nPTH and ePTH as determined by 2 week biochemistry
While there were differences in individual symptom scores for the patients with nPTH and ePTH, when we calculated the mean Likert sum scores for patients with 2 week nPTH and ePTH they were not statistically different pre-operatively, at 6 weeks, or at 6 months (Table 3).
Table 3.
Likert Sum Scores in patients with nPTH and ePTH based on 2 week biochemistry
| Timepoint | Likert Sum for Patients with nPTH |
Likert Sum for Patients with ePTH |
P Value |
|---|---|---|---|
| Pre-Operative | 31.5 ± 14.3 | 26.8 ± 12.8 | 0.18 |
| 6 Week | 16.2 ± 10.0 | 15.9 ± 10.7 | 0.92 |
| 6 Month | 18.6 ± 11.0 | 17.8 ± 9.0 | 0.80 |
All of the above analyses compared ePTH and nPTH patients based on 2 week biochemical profile. PTH was also measured for these patients at 6 month follow-up. Of patients for whom both 2 week and 6 month PTH was available (n= 113), 85 (75%) had nPTH at both time points, and seven (6%) had ePTH at both time points (Table 4).
Table 4.
Number of patients in each nPTH and ePTH category
| PTH at 6 months | ||||
|---|---|---|---|---|
| nPTH | ePTH | Total | ||
| PTH at 2 weeks | nPTH | 85 | 12 | 97 |
| ePTH | 9 | 7 | 16 | |
| Total | 94 | 19 | 113 | |
Factors associated with symptom improvement
Patients were categorized into “Responders” vs. “Non-responders” based on Likert sum scores at both 6 weeks and 6 months as compared to their pre-operative scores. “Responders” were defined as patients whose improvement was above the 75th percentile. The 75th percentile at 6 weeks corresponded to an improvement in symptom sum of 23 points or higher than the pre-operative score. For 6 month data, the 75th percentile corresponded to an improvement of 20 points or higher than the pre-operative score. Though the findings were not statistically significant, at 6 weeks, responders had higher mean pre-operative vitamin D, and lower means for age, pre-operative PTH, and 2 week PTH (Table 5). At 6 weeks, only 4% of responders were male, while 29% of non-responders were male (p=0.01). Observed trends in age and PTH levels also held true for 6 month data, but the magnitude of the differences was lower, and none of the variables showed significant differences between 6 month responders and non-responders (data not shown).
Table 5.
Differences between Responders and Non-Responders based on Likert Sums of symptoms at 6 weeks
| Responders (n= 26) |
Non-Responders (n= 70) |
P value | |
|---|---|---|---|
| Sex | 0.01 | ||
| M | 1 (4%) | 20 (29%) | |
| F | 25 (96%) | 50 (71%) | |
| Age (y) | 58.3 | 60.8 | 0.40 |
| Pre-Operative | |||
| Calcium (mg/dL) | 10.7 | 10.8 | 0.86 |
| PTH (pg/mL) | 91.0 | 112.0 | 0.15 |
| Vitamin D (D-25-OH, ng/mL) | 33.3 | 30.7 | 0.45 |
| 2 week Post-Operative | |||
| Calcium (mg/dL) | 9.4 | 9.2 | 0.33 |
| PTH (pg/mL) | 43.1 | 50.1 | 0.43 |
Vitamin D levels and symptom improvement
All patients were categorized with respect to pre-operative vitamin D levels into ‘inadequate’ (≤ 20 ng/mL) and ‘adequate’ (> 20 ng/mL) levels. Around a fifth (21%) of patients had inadequate levels, having a mean level of 12.8 ± 6.7 ng/mL. The majority of patients (79%) had adequate vitamin D with a mean of 36.5 ± 12.5 ng/mL. Vitamin D inadequacy and PTH elevation was compared through chi-square analysis separately for 2 week and 6 month data, and no significant relationships were found. Likert sum scores were also examined with respect to these vitamin D categories, and showed that pre-operative vitamin D levels did not significantly affect overall symptom improvement.
Discussion
This study evaluated the occurrence of ePTH in patients with PHPT after curative resection, and the extent of post-operative symptom improvement as compared to patients with nPTH. In accordance with prior studies, we found that 16% of patients had ePTH at an early post-operative time point2,13,21. Age, pre-operative PTH, and serum calcium levels were correlated with ePTH at 2 weeks, however, there was no significant association with vitamin D level. Regarding symptom improvement in ePTH patients, several individual symptoms showed less improvement than for nPTH patients at 6 weeks, although by 6 months, rates of improvement were similar in both groups.
Previous studies have examined elevated PTH at time points ranging from 1 day to 5 years after curative surgery14–22. In this study, at 2 weeks and 6 months, a similar proportion of patients had ePTH (16% and 17%, respectively). However, the cohorts of patients with ePTH at 2 weeks and 6 months were different, as only 6% of patients had ePTH at both time points. This finding raises the possibility that patients with short term and longer term ePTH may have different etiologies. Other authors have found considerable fluctuations in patients’ PTH elevation over time as well, though the significance of this phenomenon still remains unclear14,15,16,20. Nordenstrom et al. examined ePTH with a follow-up of 5 years and categorized patients into “Normal”, “Normalized”, and “Variable” groups based on the stability of their ePTH levels over time, and found significant differences in biochemistry between the groups15. Furthermore, whether post-surgical ePTH at any time point is an indicator for recurrent hyperparathyroidism is highly controversial, having contradicting findings in current research2,15–17,19.
This study adds to the available knowledge regarding predictors of ePTH, another topic with no clear consensus. High pre-operative and early post-operative levels of PTH have consistently been shown to correlate with ePTH2,13–15,18,19,21, and we confirmed this relationship as well. A subset of studies have also found advanced age to be a predictor20,21, as was seen in our data. Prior research has shown that ePTH patients have lower pre-operative D-25-OH levels13,17,20, and though our univariate analysis showed the same trend, it was not statistically significant. Furthermore, in this study, patients classified as having inadequate vitamin D were no more likely to have ePTH at either 2 weeks or 6 months. Mizrachi et al. found no difference in post-operative D-25-OH levels between ePTH and nPTH patients, though evidence was found for etiology related to cortical bone mineralization14. Studies that did not systematically measure vitamin D have also found evidence for etiology other than vitamin D deficiency2,19. To further investigate whether vitamin D deficiency is correlated with ePTH or symptom improvement, we suggest that future studies monitor D-25-OH levels at various time points both pre- and post-operatively, which we were unable to do in this analysis. Though our design did not examine specific etiologies, the findings support that etiology for ePTH extends beyond vitamin D deficiency alone.
The presence of pre-operative nonspecific symptoms in patients with ePTH has been documented in multiple studies, and these, in contrast to ours, have not typically investigated symptom improvement. Westerdahl et al. divided patients into ePTH and nPTH groups based on 8-week biochemistry and found that the two groups did not differ in their pre-operative symptoms18. Mitterndorf et al. found the presence of neuromuscular symptoms to be positively associated with elevated PTH 10 to 14 days after surgery16. The present study tracked symptom frequency over time, and examined improvement in frequency from pre-operative baseline. Interestingly, we found that males were less likely to be in the top quartile of overall symptom improvement at 6 weeks. As gender is not commonly found to be associated with symptom improvement in other studies1,3–10, further investigation into this finding would benefit from a larger sample of patients with more male participants. More notable was the finding that at 6 weeks, patients with early post-operative ePTH showed significantly lower proportions of improvement for four individual symptoms, with a trend towards lesser improvement for ten other symptoms. This indicates that ePTH status affects post-surgical recovery for nonspecific symptoms of PHPT. Our study suggests that the delay in recovery is short term, as symptoms improved for ePTH patients between 6 weeks and 6 months, reaching rates similar to those for nPTH patients by 6 months.
The definition for surgical cure for PHPT has come under closer examination recently, with some suggesting that ePTH indicates “incomplete” parathyroidectomy14,21. Taking nonspecific symptoms of PHPT into account, we suggest that optimal recovery includes normalization of PTH levels. This research has implications for follow-up and monitoring for patients post-parathyroidectomy. For patients with ePTH in the early post-operative period, it may be beneficial to monitor PTH levels at further follow-up along with symptom improvement. In order to avoid delays in symptom improvement patients may benefit from more aggressive management of calcium or vitamin D to mitigate ePTH, perhaps especially for older patients, though this is subject to further study. The knowledge that ePTH may lead to delay in symptom recovery can also be useful to clinicians in counseling patients as to timing of symptom improvement post-surgery.
There are several limitations to this study. Firstly, it did not utilize a true non-parathyroid control group and we cannot prove that the symptoms that patients had are related only to their parathyroid disease. Pre-operative questionnaires served as a control in comparing the extent and timing of symptom improvement for an individual patient and our main comparison was amongst surgically treated patients whom underwent curative parathyroidectomy, comparing groups based on the presence or absence of an elevated PTH post-operatively. Secondly, the analysis did not include adjustment for patient sociodemographics or co-morbidities. It is not known how these factors may potentially affect ePTH status or timing of symptom improvement. Thirdly, since all data came from a single university hospital, it may be subject to institutional or referral bias. As responders to the survey made up only 66% of those who underwent parathyroidectomy, there may also be a non-responder bias. However, in this regard, there were no significant differences in parathyroid pathology, age, or gender between responders and non-responders (Table 1), which supports the likelihood that this study sample is generalizable.
In conclusion, ePTH within two weeks of curative parathyroidectomy affects 16% of patients and is associated with higher pre-operative PTH, serum calcium, and advanced age. Early post-operative ePTH is associated with a delay in symptom improvement at 6 weeks, which resolves by 6 months. Although further research is necessary, clinicians should be aware that ePTH may be relevant to post-surgical prognosis of patients with PHPT.
Acknowledgments
Funding for this research was provided by the University of Wisconsin, Physician Scientist Training in Career Medicine grant (National Institutes of Health T32 CA009614-22)
Appendix
Symptom Questionnaire
Footnotes
Summary of Author Contributions:
Pathak- Conception/design, Data collection, Analysis/interpretation, Writing
Murray- Conception/design, Data collection, Analysis/interpretation, Critical revision
Schaefer- Data collection, Critical revision
Leverson- Analysis/interpretation, Critical revision
Chen- Critical revision, Funding
Sippel- Conception/design, Analysis/interpretation, Critical revision, Funding
References
- 1.Eigelberger MS, Cheah WK, Ituarte PH, Streja L, Duh QY, Clark OH. The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited? Ann Surg. 2004;239:528. doi: 10.1097/01.sla.0000120072.85692.a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ning L, Sippel R, Schaefer S, Chen H. What is the clinical significance of an elevated parathyroid hormone level after curative surgery for primary hyperparathyroidism? Ann Surg. 2009;249:469. doi: 10.1097/SLA.0b013e31819a6ded. [DOI] [PubMed] [Google Scholar]
- 3.Burney RE, Jones KR, Coon JW, Blewitt DK, Herm AM. Assessment of patient outcomes after operation for primary hyperparathyroidism. Surgery. 1996;120:1013. doi: 10.1016/s0039-6060(96)80048-1. [DOI] [PubMed] [Google Scholar]
- 4.Khan AA, Bilezikian JP, Potts JT. Asymptomatic primary hyperparathyroidism: a commentary on the revised guidelines. Endocr Pract. 2009;15:494. doi: 10.4158/EP09162.CO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan AK, Duh QY, Katz MH, Siperstein AE, Clark OH. Clinical manifestations of primary hyperparathyroidism before and after parathyroidectomy. A case-control study. Ann Surg. 1995;222:402. doi: 10.1097/00000658-199509000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mittendorf EA, Wefel JS, Meyers CA, Doherty D, Shapiro SE, Lee JE, Evans DB, Perrier ND. Improvement of sleep disturbance and neurocognitive function after parathyroidectomy in patients with primary hyperparathyroidism. Endocr Pract. 2007;13:338. doi: 10.4158/EP.13.4.338. [DOI] [PubMed] [Google Scholar]
- 7.Gopinath P, Sadler GP, Mihai R. Persistent symptomatic improvement in the majority of patients undergoing parathyroidectomy for primary hyperparathyroidism. Langenbeck Arch Surg. 2010;395:941. doi: 10.1007/s00423-010-0689-z. [DOI] [PubMed] [Google Scholar]
- 8.Perrier ND, Balachandran D, Wefel JS, Jimenez C, Busaidy N, Morris GS, Dong W, Jackson E, Weaver S, Gantela S. Prospective, randomized, controlled trial of parathyroidectomy versus observation in patients with “asymptomatic” primary hyperparathyroidism. Surgery. 2009;146:1116. doi: 10.1016/j.surg.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 9.Adler JT, Sippel RS, Schaefer S, Chen H. Surgery improves quality of life in patients with “mild” hyperparathyroidism. Am J Surg. 2009;197:284. doi: 10.1016/j.amjsurg.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Silverberg SJ, Bilezikian JP. The diagnosis and management of asymptomatic primary hyperparathyroidism. Nat Clin Pract Endocrinol Metab. 2006;2:494. doi: 10.1038/ncpendmet0265. [DOI] [PubMed] [Google Scholar]
- 11.Murray S, Pathak P, Pontes D, Schneider D, Schaefer S, Chen H, Sippel RS. Timing of symptom improvement after parathyroidectomy for primary hyperparathyroidism. Surgery. 2013;154:1463. doi: 10.1016/j.surg.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray S, Pathak P, Schaefer S, Chen H, Sippel R. Improvement of Sleep Disturbance and Insomnia Following Parathyroidectomy for Primary Hyperparathyroidism. World J Surg. 2013 doi: 10.1007/s00268-013-2285-1. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Biskobing DM. Significance of elevated parathyroid hormone after parathyroidectomy. Endocr Pract. 2010;16:112. doi: 10.4158/EP09122.RA. [DOI] [PubMed] [Google Scholar]
- 14.Mizrachi A, Gilat H, Bachar G, Feinmesser R, Shpitzer T. Elevated parathyroid hormone levels after parathyroidectomy for primary hyperparathyroidism. Head Neck. 2009;31:1456. doi: 10.1002/hed.21119. [DOI] [PubMed] [Google Scholar]
- 15.Nordenstrom E, Westerdahl J, Isaksson A, Lindblom P, Bergenfelz A. Patients with elevated serum parathyroid hormone levels after parathyroidectomy: Showing signs of decreased peripheral parathyroid hormone sensitivity. World J Surg. 2003;27:212. doi: 10.1007/s00268-002-6600-5. [DOI] [PubMed] [Google Scholar]
- 16.Mittendorf EA, McHenry CR. Persistent parathyroid hormone elevation following curative parathyroidectomy for primary hyperparathyroidism. Arch Otolaryngol Head Neck Surg. 2002;128:275. doi: 10.1001/archotol.128.3.275. [DOI] [PubMed] [Google Scholar]
- 17.Oltmann SC, Maalouf NM, Holt S. Significance of elevated parathyroid hormone after parathyroidectomy for primary hyperparathyroidism. Endocr Pract. 2011;17:57. doi: 10.4158/EP10324.RA. [DOI] [PubMed] [Google Scholar]
- 18.Westerdahl J, Valdemarsson S, Lindblom P, Bergenfelz A. Postoperative elevated serum levels of intact parathyroid hormone after surgery for parathyroid adenoma: sign of bone remineralization and decreased calcium absorption. World J Surg. 2000;24:1323. doi: 10.1007/s002680010219. [DOI] [PubMed] [Google Scholar]
- 19.Carty SE, Roberts MM, Virji MA, Haywood L, Yim JH. Elevated serum parathormone level after “concise parathyroidectomy” for primary sporadic hyperparathyroidism. Surgery. 2002;132:1086. doi: 10.1067/msy.2002.128479. [DOI] [PubMed] [Google Scholar]
- 20.Lang BH, Wong IY, Wong KP, Lo C. Eucalcemic Parathyroid Elevation After Parathyroidectomy for Primary Sporadic Hyperparathyroidism: Risk Factors, Trend, and Outcome. Ann Surg Oncol. 2012;19:584. doi: 10.1245/s10434-011-1846-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang TS, Ostrower ST, Heller KS. Persistently elevated parathyroid hormone levels after parathyroid surgery. Surgery. 2005;138:1130. doi: 10.1016/j.surg.2005.08.026. [DOI] [PubMed] [Google Scholar]