Abstract
BACKGROUND
Horizontal strabismus due to a weak rectus muscle can be treated with an augmented Hummelsheim procedure, in which both vertical rectus muscle tendons are split, resected by 4 mm, and reattached to the sclera adjacent to the weak rectus muscle. Compared with vertical rectus transposition, the procedure spares two ciliary vessels and does not require placement of augmentation sutures. In this study, we evaluated binocular alignment and ocular motility in patients with abducens nerve palsy treated with an augmented Hummelsheim procedure.
METHODS
The medical records of consecutive patients with complete abducens nerve palsy who underwent the augmented Hummelsheim procedure, usually combined with medial rectus muscle recession, were retrospectively reviewed. Binocular alignment, ocular motility, and complications were analyzed.
RESULTS
Ten patients (age range, 12–57 years) met inclusion criteria for the study, of whom 9 of 10 had simultaneous medial rectus recession. Follow-up ranged from 1 week to 24 months. The augmented Hummelsheim procedure improved esotropia from 43Δ ± 5Δ preoperatively to 6Δ ± 7Δ postoperatively (P < 0.0001) and reduced abduction deficits from −4 to −3 (P < 0.0001). One patient with coexisting oculomotor nerve palsy developed consecutive exotropia; 2 had induced vertical deviations. There were no cases of anterior segment ischemia.
CONCLUSIONS
The augmented Hummelsheim procedure combined with medial rectus muscle recession reduced mean primary position esotropia and improved abduction in patients with complete abducens nerve palsy.
A variety of surgical approaches are available to address the esotropia and loss of abduction that result from complete abducens nerve palsy. Although a large recession of the medial rectus muscle and resection of the lateral rectus muscle in the involved eye will improve anatomical alignment, in most cases, the esotropia and abduction deficit recur postoperatively. Therefore, transposition procedures (of the ipsilateral superior and inferior rectus muscles to the insertion of the lateral rectus muscle) generally are preferred in cases of complete abducens nerve palsy. In 2000 Brooks and colleagues 1 introduced a modification of the traditional Hummelsheim procedure for use in patients with paralytic strabismus in which a 4–5 mm portion of each vertical rectus muscle was resected before transposition. This technique spares the ciliary vessel in the nontransposed half of each vertical rectus muscle, theoretically reducing the risk of anterior segment ischemia. Simultaneous recession of the ipsilateral medial rectus may therefore be considered. In addition, the procedure may enable a more precise titration of the effects of surgery by altering the amounts of medial rectus recession and half-vertical tendon resection.1 Finally, the augmented Hummelsheim procedure does not require placement of lateral fixation sutures, which may confer the advantage of simplifying subsequent surgery, if needed. We present a series of patients with complete abducens nerve palsy treated with the augmented Hummelsheim procedure.
Subjects and Methods
This study was approved by the Emory University School of Medicine Institutional Review Board and conformed to the requirements of the United States Health Insurance Portability and Accountability Act. We retrospectively reviewed the medical records of consecutive patients who underwent an augmented Hummelsheim procedure to treat complete abducens nerve palsy. These cases were identified by means of a computerized search of billing records for the CPT code 67320 for transposition. Patients were considered to have complete abducens nerve palsy if they were unable to abduct the involved eye to or past the midline. All surgeries were performed by 2 surgeons (AKH and PDL). Data extracted from the medical record and entered into a spreadsheet included sex, age at surgery, operated eye, source of the abducens nerve palsy, preoperative, initial postoperative, and final postoperative deviation in primary position at both distance and near, preoperative, initial postoperative, and final postoperative duction limitation, interval to initial and final postoperative evaluation, and general comments. Ductions were graded on a scale from 0, indicating full ductions, to −5 for an eye that could not reach the midline on attempted abduction.
All patients but one underwent an augmented Hummelsheim procedure combined with a medial rectus muscle recession. The surgical technique used was as follows: forced ductions were performed to confirm medial rectus muscle restriction. Fornix incisions were used in all patients. Accessed via an inferior-nasal incision, the medial rectus muscle was isolated and secured with a 6-0 polyglactin 910 suture, disinserted from the globe, and set aside. The lateral half of the superior and inferior rectus muscles were isolated through superior-temporal and inferior-temporal incisions, respectively (Figure 1A). The nasal half of each vertical rectus muscle was left unoperated, thus leaving the remaining nasal ciliary arteries intact. A 6-0 polyglactin 910 suture was placed 4 mm posterior to the insertion of the muscle, and a 4mmresection of the temporal half of the muscle was performed (Figure 1B). The temporal halves of superior and inferior rectus muscles were sutured to the corresponding border of the lateral rectus muscle (Figure 1C). Then the medial rectus muscle was placed at the natural position at which its restriction was relieved. This resulted in a 5 mm recession of the medial rectus muscle in all but one patient, for whom a 4.5 mm recession was performed.
FIG 1.
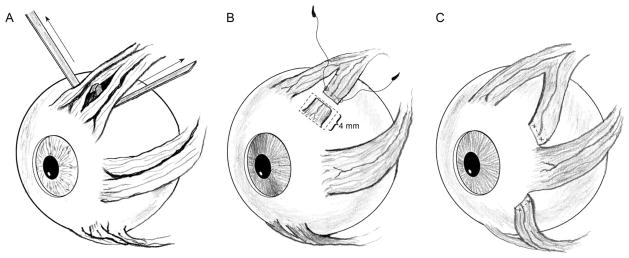
Augmented Hummelsheim procedure. A, small muscle hooks separate the nasal and temporal halves of the vertical rectus muscles, preserving the nasal ciliary vessels. B, a 6-0 polyglactin 910 suture is placed 4 mm posterior to the insertion of the vertical rectus muscle and a 4mmresection of the temporal half of the muscle is performed. C, the temporal halves of superior and inferior rectus muscles are sutured adjacent to the corresponding borders of the lateral rectus muscle along the spiral of Tillaux.
For the purposes of this study, we defined the outcome as successful if the patient had residual horizontal deviation <10Δ with no induced vertical deviation at final follow-up. The paired t test was used to determine whether the procedure resulted in a significant change in ocular alignment and duction limitation. A P value <0.05 was considered statistically significant.
Results
Medical record review identified 12 patients who had undergone an augmented Hummelsheim procedure between July 2008 and January 2011. Of these, 2 did not return for a follow-up examination and were excluded from analysis. The initial postoperative evaluation took place at a mean of 14 days (median, 9 days; range, 6–38 days) after surgery. The final postoperative evaluation took place at a mean of 28 weeks (median, 12 weeks; range, 1–105 weeks) after surgery.
The pre- and postoperative characteristics of the included patients are shown in the e-Supplement 1 (available at jaapos.org). Mean patient age at surgery was 29 years (median, 31 years; range, 12–57 years). Of the 10 patients, 6 had isolated unilateral traumatic abducens nerve palsy, 1 had partial oculomotor nerve and complete abducens nerve palsy caused by an intracavernous sinus carotid artery aneurysm, 1 patient had an isolated abducens nerve palsy caused by a petroclival meningioma, and 2 had multiple cranial nerve palsies caused by intracranial tumor. Patient 2 was the only one in our series who did not undergo a simultaneous medial rectus muscle recession at the time of her augmented Hummelsheim procedure; this patient had bilateral, asymmetric pathology involving multiple cranial nerves and a second surgery was anticipated on the other eye at a later date.
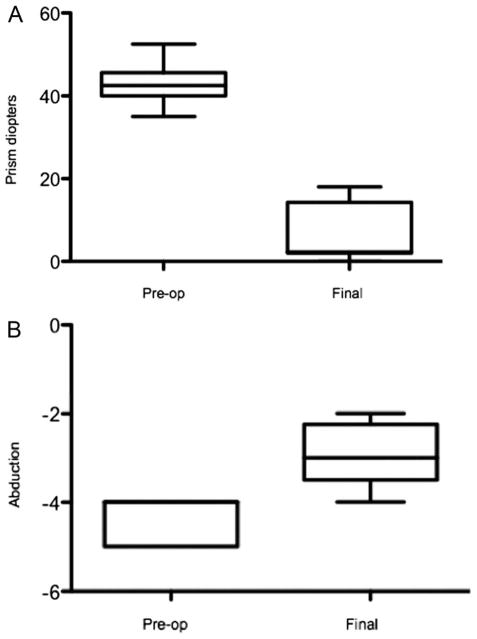
The mean esodeviation at distance in primary position improved from 43Δ ± 5Δ (median, 43Δ) preoperatively to 6Δ ± 7Δ (median, 2Δ) postoperatively (P < 0.0001; Figure 2A). Mean esotropia at near in primary position improved from 43Δ ± 7Δ (median, 43Δ) preoperatively to 9Δ ± 10Δ (median, 4Δ) postoperatively (P < 0.0001). Of note, the initial postoperative deviation was within 10Δ of orthophoria at both distance and near in all but 2 of the patients. Overall, we observed a mean final exoshift of 39Δ (median, 39; range, 29Δ–53Δ). A successful outcome was achieved in 80% of patients.
FIG 2.
A, preoperative versus final angle of primary gaze (paired t test, P < 0.0001): box-and-whiskers diagram showing 25th, 50th, and 75th percentiles; the ends of the whiskers represent the minimum and maximum of the data. Since postoperative measurements were mostly clustered between 0Δ and 2Δ, minimum, 25th percentile, and 50th percentile appear indistinguishable. B, preoperative versus final limitation of abduction (paired t test, P < 0.0001): box-and-whiskers diagram showing 25th, 50th, and 75th percentiles; the ends of the whiskers represent the minimum and maximum of the data. Since all preoperative measurements were either −4 and −5, the median, 75th percentile, and upper limit are superimposed.
Only 2 patients had an increase in their distance or near horizontal deviation >8Δ noted between the initial and final postoperative evaluations. One patient (patient 5) noted a somewhat sudden increase in diplopia within a few weeks of surgery and was found to have an esotropia of 18Δ and a right hypertropia of 8Δ after an initial postoperative measurement of orthophoria. A slipped inferior rectus muscle was suspected, but the patient declined reoperation. Another patient (Patient 1), with an initial postoperative measurement of orthophoria, was found to have variable esotropia measuring 14Δ to 20Δ 13 months postoperatively. The patient with the longest follow-up (patient 3) showed stable alignment in primary position, although he subjectively reported that his field of single binocular vision seemed to have become smaller over time.
Induced vertical deviations were noted at the final follow-up visit in 2 patients: one (patient 9) had a history of multiple cranial nerve palsies, exposure keratopathy, poor vision, and presumably poor fusion and was noted to have a 12Δ hypertropia postoperatively; the second (Patient 5) had an 8Δ hypertropia thought to be attributable to a slipped inferior rectus muscle.
All of our patients had a residual abduction deficit of at least −3 (no more than 25% of full abduction) postoperatively (Figure 2B), although abduction improved according to subjective measurements in 8 patients. There were no cases of anterior segment ischemia, and no other complications were observed.
Discussion
Resection of the affected lateral rectus muscle coupled with recession of the ipsilateral antagonist medial rectus muscle can often restore normal alignment and full or nearly full abduction to patients with abducens nerve palsy who have residual lateral rectus function; however, no known procedure can restore function in cases of complete lateral rectus palsy. In general, in cases of total abducens nerve palsy, a transposition procedure is chosen to restore primary position alignment.2 Some strabismus surgeons prefer to perform a medial rectus recession and lateral rectus resection on the affected eye combined with a contralateral medial rectus recession and posterior fixation suture. The goal of this technique is to create an adduction deficit in the contralateral eye that will “match” the abduction deficit in the affected eye and expand the field of single binocular vision.3
Partial vertical rectus muscle transposition to treat complete abducens nerve palsy was first described by Hummelsheim in 1908.4 Modifications of his procedure include the Jensen procedure (1964)5 and an adjustable partial-tendon transposition (1974).6 Full-tendon vertical rectus muscle transposition was first described in 1959 by Schillinger,7 whose procedure has been modified with adjustable techniques.8,9
One pivotal modification of the full-tendon vertical muscle transposition introduced by Scott Foster was the addition of an equatorial lateral fixation suture (augmentation suture) to the transposed vertical rectus muscles. This modification was shown by imaging to increase the lateralization of the transposed muscles, maximizing the tonic abducting force.10 The authors of a recent case series describe good results after superior rectus transposition combined with medial rectus recession on an adjustable suture for Duane syndrome patients and patients with abducens nerve palsy.11
Transposition procedures often are combined with medial rectus muscle weakening, especially when forced duction testing reveals restriction. Medial rectus recession or injection of the medial rectus muscle with botulinum toxin A can be staged or performed at the time of the transposition procedure; however, simultaneous medial rectus weakening raises concerns of anterior segment ischemia, especially in the setting of a full-tendon transposition procedure.
Despite the array of techniques available for improving alignment with abducens nerve palsy, none has proved uniformly effective. We have observed several advantages to the augmented Hummelsheim procedure. Subjectively, we have observed more consistent and predictable outcomes when using the augmented Hummelsheim procedure combined with medial rectus recession than we did when we used a full-tendon transposition procedure with lateral fixation suture combined with botulinum toxin to the medial rectus muscle.
A comparison of outcomes with various procedures is difficult because series reported in the literature are relatively small. Furthermore, most reports (including ours) combine the authors’ experience using a given transposition procedure to treat patients affected with a variety of forms of strabismus, including unilateral and bilateral abducens nerve palsy as well as Duane syndrome and multiple cranial nerve palsies. In addition, in many reports authors include patients who have had previous surgery. A review of a series of a variety of transposition procedures reveals that the mean change in horizontal deviation has been reported to be anywhere between 31Δ and 66Δ, with ranges as wide as 12Δ to 122Δ in a single series.9
Even if the comparison is limited to patients with isolated unilateral abducens nerve palsy who have never undergone previous surgery, a tremendous amount of variation exists in the results reported with any given procedure. This variation often is masked by the tendency for authors to report only the mean postoperative alignment after the procedure as the main measure of the success of the procedure. For example, Leiba and colleagues12 recently reported a postoperative mean primary position distance alignment of 7.9Δ ± 8.8Δ esotropia in their study of the long-term outcome of vertical rectus muscle transposition and botulinum toxin for sixth nerve palsy. Additional analysis of the data, excluding patients with bilateral abducens nerve palsy and with a history of previous recession-resection surgery, reveals the range of exoshift following the procedure to be from 10Δ to 75Δ, with a median exoshift of 30Δ. This type of variation seems to be common in many series, including most types of transposition procedures with or without weakening of the ipsilateral medial rectus muscle.6,9,13–19 If we consider only the patients with isolated unilateral abducens nerve in our series, we find a mean exoshift of 38Δ and a median exoshift 36Δ (range, 28Δ–53Δ). Although a meta-analysis of the literature is beyond the scope of this report, in our experience, results of the augmented Hummelsheim combined with medial rectus muscle recession have been more predictable and uniform than results we observed using other techniques.
Advantages of the augmented Hummelsheim procedure over some other transposition procedures include sparing of at least one ciliary vessel on each of the vertical rectus muscles and avoiding placement of a lateral fixation suture. Sparing of the ciliary vessels, at least in theory, should reduce the risk of anterior segment ischemia and allow for simultaneous recession of the ipsilateral medial rectus muscle. Use of fornix incisions rather than limbal incisions may also contribute to a reduced risk of anterior segment ischemia.20 The authors are aware, however, of an unpublished case of anterior segment ischemia at an outside institution after the augmented Hummelsheim procedure was performed in an elderly patient with severe perioperative hypertension.
Induced vertical deviations are a relatively common complication of vertical rectus muscle transposition surgery, and have been reported to occur in between 0% and 27% of patients undergoing partial and full vertical rectus muscle transpositions with or without medical rectus muscle weakening procedures.9 Of our patients, 2 had induced vertical deviations at their final postoperative examination. In one of these patients, the vertical deviation was thought to be the result of a slipped inferior rectus muscle, but the patient declined reoperation. The second patient had very poor vision with poor fusional potential. Thus, the rate of induced vertical deviations caused by the augmented Hummelsheim procedure is consistent with that of other procedures.
Most of our patients were orthotropic or had a small residual esodeviation at their final follow-up visit; however, one patient was overcorrected, resulting in a consecutive exotropia of 12Δ at her initial postoperative visit, 9 days after surgery, which improved on long term follow-up. This patient (Patient 4) had both a complete abducens nerve palsy and a partial oculomotor nerve palsy from an internal carotid artery aneurysm. We suspect that residual weakness of the medial rectus muscle from the underlying oculomotor nerve palsy led to the overcorrection. We now stage recession of the antagonist muscle as a second procedure in any patient in whom weakness of the antagonist muscle might be reasonably anticipated. A staged approach in any patient in whom the direct antagonist of the paralyzed muscle might also be weak has also proved useful in patients undergoing augmented Hummelsheim procedure of the horizontal rectus muscles for vertical muscle paresis.
The augmented Hummelsheim procedure combined with recession of the ipsilateral medial rectus muscle successfully corrected primary position esotropia in our patients with complete abducens nerve palsy. We acknowledge that our definition of success was arbitrary and that the magnitude of residual head turn and/or degrees of single binocular vision would have been more appropriate measures of success, but these measurements could not be obtained in this retrospective study. It is possible that medial rectus muscle recession at the time of vertical muscle transposition could have limited adduction and reduced the field of single binocular vision. This scenario is unlikely because postoperative adduction deficits were not common in our patients unless a coexisting oculomotor nerve palsy was present. We considered patients unable to abduct to midline as cases of complete abducens nerve palsy, although all had documented evidence of medial rectus restriction that could have affected their ability to abduct. Force generation testing and the presence of floating saccades were not consistently documented. Because the number of patients enrolled in the study was small and some patients had other cranial nerve palsies, it is difficult to make meaningful comparisons to the outcomes of other studies that are similarly limited. Finally, our results are limited by the very short mean follow-up since ongoing changes in alignment are common in this population of patients.
Supplementary Material
Acknowledgments
Supported in part by an unrestricted grant to the Emory Eye Center from Research to Prevent Blindness, Inc, New York, New York.
References
- 1.Brooks SE, Olitsky SE, deB Ribeiro G. Augmented Hummelsheim procedure for paralytic strabismus. J Pediatr Ophthalmol Strabismus. 2000;37:189–95. doi: 10.3928/0191-3913-20000701-04. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum AL. Costenbader lecture. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004;8:409–19. doi: 10.1016/j.jaapos.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds JD, Coats DK. Transposition procedures for sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 2009;46:324–6. doi: 10.3928/01913913-20091104-01. [DOI] [PubMed] [Google Scholar]
- 4.Hummelsheim E. Weitere Ertahunger mit partiellar Sehnenuberpflanzung an der Augenmuskln (abstract) Arch Augenheilkd. 1908–1909;62:71. [Google Scholar]
- 5.Jensen CD. Rectus muscle union: A new operation for paralysis of the rectus muscles. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1964;45:359–87. [PubMed] [Google Scholar]
- 6.Carlson MR, Jampolsky A. An adjustable transposition procedure for abduction deficiences. Am J Ophthalmol. 1979;87:382–7. doi: 10.1016/0002-9394(79)90081-3. [DOI] [PubMed] [Google Scholar]
- 7.Schillinger RJ. A new type of tendon transplant operation for abducens paralysis. J Int Coll Surg. 1959;31:593–600. [PubMed] [Google Scholar]
- 8.Laby DM, Rosenbaum AL. Adjustable vertical rectus muscle transposition surgery. J Pediatr Ophthalmol Strabismus. 1994;31:75–8. doi: 10.3928/0191-3913-19940301-03. [DOI] [PubMed] [Google Scholar]
- 9.Phamonvaechavan P, Anwar D, Guyton DL. Adjustable suture technique for enhanced transposition surgery for extraocular muscles. J AAPOS. 2010;14:399–405. doi: 10.1016/j.jaapos.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997;1:20–30. doi: 10.1016/s1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 11.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition combined with medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130:195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leiba H, Wirth GM, Amstuz C, Landau K. Long-term results of vertical transposition and botulinum toxin for sixth nerve palsy. J AAPOS. 2010;14:498–501. doi: 10.1016/j.jaapos.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum AL, Kushner BJ, Kirschen D. Vertical rectus muscle transposition and botulinum toxin (Oculinum) to medial rectus for abducens palsy. Arch Ophthalmol. 1989;107:820–23. doi: 10.1001/archopht.1989.01070010842025. [DOI] [PubMed] [Google Scholar]
- 14.McManaway JW, 3rd, Buckley EG, Brodsky MC. Vertical rectus muscle transposition with intraoperative botulinum injection for treatment of chronic sixth nerve palsy. Graefes Arch Clin Exp Ophthalmol. 1990;228:401–6. doi: 10.1007/BF00927250. [DOI] [PubMed] [Google Scholar]
- 15.Flanders M, Qahtani F, Gans M, Beneish R. Vertical rectus muscle transposition and botulinum toxin for complete sixth nerve palsy. Can J Ophthalmol. 2001;36:18–25. doi: 10.1016/s0008-4182(01)80062-4. [DOI] [PubMed] [Google Scholar]
- 16.Simons BD, Siatkowski RM, Neff AG. Posterior fixation suture augmentation of full-tendon vertical rectus muscle transposition for abducens palsy. J Neuroophthalmol. 2000;20:119–22. doi: 10.1097/00041327-200020020-00012. [DOI] [PubMed] [Google Scholar]
- 17.Struck MC. Augmented vertical rectus transposition surgery with single posterior fixation suture: Modification of Foster technique. J AAPOS. 2009;13:343–9. doi: 10.1016/j.jaapos.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 18.Hong S, Chang YH, Han SH, Lee JB. Effect of full tendon transposition augmented with posterior intermuscular suture for paralytic strabismus. Am J Ophthalmol. 2005;140:477–83. doi: 10.1016/j.ajo.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 19.Yurdakul NS, Ugurlu S, Maden A. Surgical management of chronic complete sixth nerve palsy. Ophthalmic Surg Lasers Imaging. 2011;42:72–7. doi: 10.3928/15428877-20110120-02. [DOI] [PubMed] [Google Scholar]
- 20.Fishman PH, Repka MX, Green WR, D’Anna SA, Guyton DL. A primate model of anterior segment ischemia after strabismus surgery. The role of the conjunctival circulation. Ophthalmology. 1990;97:456–61. doi: 10.1016/s0161-6420(90)32561-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.