Abstract
Importance
Fungal meningitis due to contaminated methylprednisolone injections can present with vascular sequelae in immunocompetent individuals. This is particularly germane to neurologists as better recognition of the clinical characteristics of patients with fungal meningitis and ischemic stroke will provide more timely and efficient care.
Observations
A case series of three patients who presented to Vanderbilt University Medical Center with acute ischemic stroke and later diagnosed with fungal meningitis attributed to contaminated methylprednisolone epidural injections. Of these three cases, 2 were female, 1 male, mean age of 75.3. Medical records and imaging were reviewed. All cases presented with acute ischemic strokes, and had a history of epidural methylprednisolone spinal injections for low back pain. Patients had one or more traditional risk factors for stroke. There were differing vascular patterns of presentation: 2 presented with small vessel (lacunar) pattern infarctions, while the other presented with a large vessel infarct. Of these cases, 2 died and underwent autopsy evaluation, which revealed Exserohilum rostratum as the presumed cause of death. In 2 cases, fever and meningeal signs were absent on presentation.
Conclusions
Patients with fungal meningitis may present with ischemic stroke on initial imaging. Definitive diagnosis should not delay early antifungal treatment.
Search terms: Cerebrovascular disease/Stroke, Meningitis, Fungal infections
Background
Recent identification of contaminated methylprednisolone injections has highlighted the diverse clinical presentation of fungal meningitis. When a contaminated methylprednisolone injection is the cause of fungal meningitis, there is often a prolonged incubation period between the last spinal injection to clinical presentation lasting 1 to 4 weeks, yet even longer incubation times have been reported.1,2,3 A recent series of the Tennessee cases revealed approximately 1/8 of patients have presented with strokes.3 These cases show that the organisms were primarily Exserohilum rostratum and in one case, Aspergillus fumigates. Increased risk of infection is due to specific contaminated lots, older vials, higher corticosteroid doses, multiple procedures, and a translaminar approach. 3 The objective of this series is to describe a cohort of patients who present with ischemic infarction in differing vascular distributions. These cases emphasize an unusual diagnostic dilemma, where an ischemic infarct is initially attributable to known stroke risk factor such as atrial fibrillation or the presence of antiphospholipid protein antibodies, yet patients were later found to have a fungal infection accounting for the presentation.
Case Series
Case one
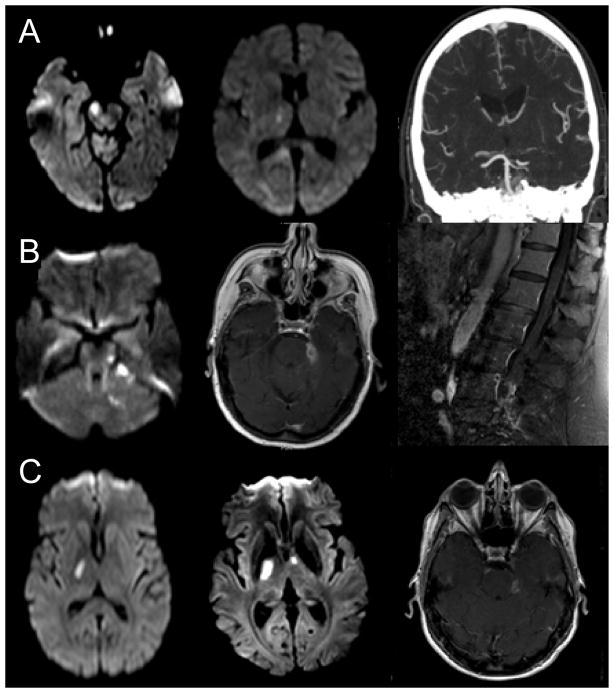
A 78-year-old-male presented with acute onset left sided weakness and dysarthria. Past medical history included low back pain, hyperlipidemia (HLD), hypertension (HTN), and atrial fibrillation. Upon presentation, he was afebrile and complained of a mild persistent headache. Neurologic examination revealed dysarthria, left lower facial weakness, left upper and lower extremity weakness in an upper motor neuron distribution. No meningeal signs were noted. Initial work up was notable for a mild leukocytosis. Magnetic resonance imaging (MRI) of the brain showed a small vessel (lacunar) ischemic infarct of the right anterior superior pons/lower midbrain (Figure 1). Magnetic resonance angiography (MRA) of the head and neck, and transthoracic echocardiogram (TTE) were unremarkable. On hospital day 3, the patient had an exacerbation of left sided weakness. Repeat MRI showed an extension of the infarct in the right midbrain and a new small lacunar infarct in the right thalamus (See Figure 1, Panel A2). On hospital day 4, the patient became unresponsive with a right dilated pupil. Repeat imaging showed enlargement and evolution prior infarcts, along with a new right superior cerebellar artery occlusion. The patient died on hospital day 6. An autopsy was performed as he was noted to have received an epidural steroid injection approximately two weeks prior to presentation. Autopsy showed small areas of focal cortical and pontine subarachnoid hemorrhage, as well as fungal cerebral vasculitis with aneurysm formation. Exserohilum species were found microscopically.
Figure 1. Imaging Findings.
A. Case 1 (1) Hospital day 1, diffusion weighted imaging (DWI) with acute upper pontine/lower midbrain ischemic stroke suggestive of small vessel etiology (2) Hospital day 3, repeat MRI with direct extension of stroke into right thalamus suggestive of a large vessel etiology (3) Hospital day 4, CTA with occlusion of right superior cerebellar artery
B. Case 2 (1) Hospital day 1, DWI with acute left pontine and cerebellar ischemic strokes suggestive of large vessel etiology (2) Hospital day 15, T1 sequence with contrast revealing an abscess adjacent to the left cerebellopontine angle (3) Hospital day 15, lumbar MRI T1 sequence with contrast showing extradural enhancement and clumping of nerve roots suggesting arachnoiditis
C. Case 3 (1) Hospital day 1, DWI with right small vessel internal capsule stroke (2) Hospital day 7, DWI with right internal capsule and left internal capsule genu stroke (3) Hospital day 7, T1 sequence with contrast also revealing a left sided cerebellopontine abscess
Case two
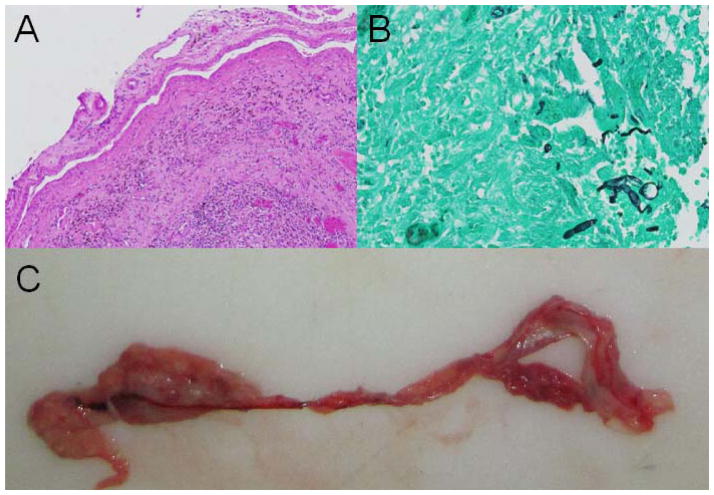
A 78-year-old female presented with subacute complaints of vertigo, nausea and headache. Past medical history noted low back pain, HTN, HLD, and coronary artery disease (CAD). Exam was notable for left hand dysmetria and mild ataxia. MRI revealed ischemic infarcts of the left lateral pons, superior cerebellar peduncle, and superior cerebellum suggestive of a large vessel (superior cerebellar artery) etiology (Figure 1). CTA did not reveal any significant posterior circulation stenosis and TTE was unremarkable. Screening labs revealed a new diagnosis of diabetes mellitus type II. Due to history of several prior miscarriages and infarct pattern, a hypercoaguable panel was ordered and positive for lupus anticoagulant and elevated antiphospholipid protein antibodies. The patient was anticoagulated. On hospital day 4, a low grade fever and mild encephalopathy was noted. Repeat brain MRI showed a new ischemic left pontine stroke. On hospital day 6, the patient developed acute urinary retention. Since she had received an epidural injection two weeks prior to admission, a lumbar spine MRI with and without contrast was obtained, and abnormal periarticular enhancement with central canal enhancement at L4-5 was noted but no drainable fluid. Initial blood cultures revealed methicillin sensitive staphylococcus aureus. Later, due to continued altered mental status and a recent report of fungal meningitis4 a lumbar puncture was performed (Table 1). Intravenous (IV) antibiotics and voriconazole at 6 mg/kg IV twice daily for two doses, followed by 4 mg/kg twice daily were initiated 15 days after initial presentation. Despite therapy, the patient died 50 days after presentation. Autopsy revealed a left superior cerebellar artery mycotic aneurysm with vascular infiltration of the arterial wall by hyphal fungal forms (Figure 2). Based on positive pre-mortem CDC PCR studies, these forms are thought to represent Exserohilum.
Table 1.
Case Presentation, Lab and Imaging Summary
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Ages | 78 | 78 | 70 |
| Gender | Male | Female | Female |
| Presenting symptoms and signs | Headache, left sided weakness, dysarthria | Headache, vertigo, nausea, dysmetria, ataxia | Headache, nuchal rigidity, fever, dysarthria, dysmetria |
| Last epidural injection prior to admission | 2 weeks | 2 weeks | One month |
|
| |||
| CSF results: | N/A | ||
| Nucleated cells (per μL) | 2,974 | 1485 | |
| Polymorphonuclear cells (%) | 93 | 53 | |
| Lymphocytes (%) | 4 | 36 | |
| Red cells (per μL) | 468 | 6 | |
| Protein (mg/dL) | 245 | 290 | |
| Glucose mg/dL) | 28 | 12 | |
| Gram stain | No bacteria | No bacteria | |
| Bacterial culture | No growth | No growth | |
| CDCa Exserohilum PCR | Positive | Negative | |
| AFB culture | No growth | No growth | |
| Aspergillus antigen index | Negative | Negative | |
| Methenamine silver stain | N/A | Negative | |
|
| |||
| Initial Imaging results | Pontine/midbrain small vessel ischemic stroke | Pontine, cerebellar ischemic strokes suggesting large vessel etiology | Thalamic/internal capsule small vessel ischemic stroke |
|
| |||
| Pathologic/Autopsy results | Exserohilum rostratum | Fungus with hyphal features | N/A |
Centers for Disease Control
Figure 2. Pathology Findings.
A. Hematoxylin and eosin stain of mycotic aneurysm of the left superior cerebellar artery
B. Higher power view of Gomori’s methenamine silver stain of hyphal elements within the mycotic aneurysm of the superior cerebellar artery
C. Gross photograph: mycotic aneurysm of the left superior cerebellar artery
Case Three
A 70-year-old female presented with headaches, balance difficulty, nuchal rigidity and fever. Past medical history was notable for HLD and chronic back pain with most recent epidural spinal injection one month prior. Exam revealed mild dysarthria and bilateral dysmetria. MRI brain revealed acute small vessel right thalamic and internal capsule ischemic strokes. MRA of the head and neck showed no significant stenoses. Due to concern for meningitis, a lumbar puncture was performed (see Table 1). Based on initial CSF results intravenous antibiotics, voriconazole in a similar regimen to case 2, and liposomal amphotercin B (stopped after 4 days) were initiated. A MRI thoracic and lumbar spine revealed evidence of lumbosacral arachnoiditis with abnormal enhancement within the posterior epidural space at L4-5 and L5-S1 but again no drainable fluid. On hospital day 7, the patient became encephalopathic and repeat MRI revealed a new acute small vessel left internal capsule. Mental status and CSF cell counts slowly improved with voriconazole monotherapy. The patient was discharged 37 days later.
Comment
We describe three cases presenting with acute ischemic strokes but upon further workup revealed fungal infections attributable to contaminated lots of methylprednisolone associated with epidural injections reportedly received at identified healthcare facilities5. Presenting symptoms in all three patients were, at least in part, related to neurologic sequelae of ischemic stroke. Early MRI findings had evidence of restricted diffusion. Initial imaging did not show evidence of hemorrhage or mycotic aneurysm. Interestingly, all cases were in the 8th decade and all had one or more traditional risk factors for stroke. The pattern of infarcts differed, where two cases initially presented with a small vessel infarcts and one with a large vessel pattern. In case 2, progressive vascular occlusion of the superior cerebellar artery was attributed to fungal infiltration at autopsy. Importantly, case 3 received earlier antifungal treatment and we suspect that this halted further vascular progression of her infection.
Regarding the territory of strokes, all presented with posterior circulation infarcts (supplied by the basilar, superior cerebellar and posterior cerebral artery branches/perforators). It is now apparent that a high index of suspicion should be raised for possible fungal meningitis in patients who present with posterior circulation ischemic strokes after recent epidural spinal injection3. However, it remains unknown why there appears to be a predilection for the posterior circulation in epidural injection associated fungal meningitis. We hypothesize that the proximity of the epidural space may account for fungal infiltration to the posterior vasculature. Definitive diagnosis could not be made during hospitalization, and was made upon autopsy or by polymerase chain reaction (PCR) test for Exserohilum. Due clinical suspicion, the patient without a known causative agent was treated early with both antibiotics and antifungals. This patient survived hospitalization.
Though much larger in scale, this is not the first fungal meningitis outbreak due to epidural spinal injection of contaminated corticosteroids. 6,7,8 These cases highlight a diagnostic dilemma of neurologists. Patients with fungal meningitis who present with ischemic strokes may be afebrile, lack signs of meningeal irritation, and have traditional stroke risk factors. In cases where small vessel infarctions expand locally or develop new infarctions in the same vascular territory, an atypical pathogenesis should be considered. We highlight that the angioinvasive nature of some fungal species4, including Exserohilum, can lead to progressive vascular occlusion. An awareness of the presentation and vascular sequelae of fungal meningitis in immunocompetent patients should lead to earlier treatment and improved outcomes prior to a definitive diagnosis.
Footnotes
Contributions:
Kleinfeld, K MD: design and conceptualization of study, analysis and interpretation of data, drafting and revising manuscript for intellectual content
Jones, P MD: design and conceptualization of study, analysis and interpretation of data, drafting and revising manuscript for intellectual content
Riebau, D MD: design and conceptualization of study, analysis and interpretation of data, revising manuscript for intellectual content
Beck, A MD: analysis and interpretation of data, revising manuscript for intellectual content
Paueksakon, P MD: analysis and interpretation of data, revising manuscript for intellectual content
Abel, TW MD, PhD: analysis and interpretation of data, revising manuscript for intellectual content
Claassen, D MD: design and conceptualization of study, analysis and interpretation of data, drafting and revising manuscript for intellectual content
Disclosures:
Dr. Kleinfeld reports no disclosures.
Dr. Jones reports no disclosures.
Dr. Riebau reports no disclosures.
Dr. Beck reports no disclosures.
Dr. Paueksakon reports no disclosures.
Dr. Abel reports no disclosures.
Dr. Claassen reports no disclosures.
References
- 1.Centers for Disease Control and Prevention (CDC) [Accessed December 7, 2012];Multistate fungal meningitis outbreak investigation current situation [online] Available at: www.cdc.gov/hai/outbreaks/currentsituation.
- 2.Slama T, Kauffman CA, Patterson TF, Neill MA. Clin Infect Dis. Vol. 56. United States: 2013. Fungal Outbreak Update From IDWeek; pp. 621–624. [DOI] [PubMed] [Google Scholar]
- 3.Kainer MA, Reagan DR, Nguyen DB, Wiese AD, Wise ME, Ward J, Park BJ, Kanago ML, Baumblatt J, Schaefer MK, Berger BE, Marder EP, Min JY, Dunn JR, Smith RM, Dreyzehner J, Jones TF. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012;367(23):2194–2203. doi: 10.1056/NEJMoa1212972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC, Wang XJ, Spires SS, Pugh ME. The index case for the fungal meningitis outbreak in the United States. N Engl J Med. 2012;367(22):2119–2125. doi: 10.1056/NEJMoa1212292. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) [Accessed April 24, 2013];Multistate fungal meningitis outbreak: healthcare facilities [online] Available at: www.cdc.gov/hai/outbreaks/meningitis-facilities-map.
- 6.Lyons JL, Gireesh ED, Trivedi JB, Bell WR, Cettomai D, Smith BR, Karram S, Chang T, Tochen L, Zhang SX, McCall CM, Pearce DT, Carroll KC, Chen L, Ratchford JN, Harrison DM, Ostrow LW, Stevens RD. Ann Intern Med. Vol. 157. United States: 2012. Fatal exserohilum meningitis and central nervous system vasculitis after cervical epidural methylprednisolone injection; pp. 835–836. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Exophiala infection from contaminated injectable steroids prepared by a compounding pharmacy—United States, July–November 2002. MMWR Morb Mortal Wkly Rep. 2002;51(49):1109–1112. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Exophiala infection from contaminated injectable steroids prepared by a compounding pharmacy—United States, July–November 2002. JAMA. 2003;289(3):291–293. [PubMed] [Google Scholar]