Abstract
Introduction
Perioperative mortality in the elderly is high following emergency surgery and varies significantly between hospitals– an observation partially explained by differences in failure to rescue. We hypothesize that failure to rescue following certain types of complications underlies the disproportionately poor outcomes observed in elderly patients.
Methods
We identified 23,217 patients undergoing emergent general or vascular surgery procedures at 41 hospitals within the Michigan Surgical Quality Collaborative between 2007 and 2012. Patients’ first complications were identified and categorized by type. We compared failure to rescue rates at the patient-level between patients <75 and ≥75 years of age. We then compared failure to rescue rates after specific complications across hospitals grouped in tertiles by risk-adjusted 30-day mortality.
Results
Risk-adjusted failure to rescue rates were significantly higher in the elderly after a first infectious (21.7% vs. 10.3%; p<0.01) or pulmonary (38.2% vs. 20.4%; p<0.01) complication when compared to younger patients. At the hospital level, high morality centers failed to rescue elderly patients more frequently than low mortality centers after a first infectious (35.6% v. 22.2%; p<0.01) and pulmonary (24.3 v. 14.3; p<0.01) complication. Failure to rescue rates following cardiovascular complications did not differ significantly across patient ages or tertiles of hospital mortality.
Conclusion
Hospitals fail to rescue elderly patients at higher rates than younger patients after infectious and pulmonary complications. Efforts to recognize and manage these specific complications have the potential to improve emergency surgical care of the elderly in Michigan.
Introduction
Addressing the challenges that come from providing surgical care to an aging population is a national priority. Elderly patients are complex, high-risk, and represent the largest growing demographic in surgical practice.(1, 2) These concerns are amplified for emergent surgeries, where elderly patients experience particularly poor outcomes.(3–5) In this context, recent evidence suggests that reducing failure to rescue events may be the most appropriate target for quality improvement within this demographic.(6)
Whether the risks of failure to rescue are higher following specific types of complications remains unclear. Previous findings indicate a relationship between cardiovascular or pulmonary complications and postoperative mortality in the elderly.(7, 8) However, these studies do not consider the time sequence of complications or how these observations may vary across hospitals. Preventing failure to rescue events requires both the recognition and subsequent management of complications.(9, 10) Given this, there may be particular utility in understanding the influence of patients’ first complications on the hospital’s ability to coordinate failure to rescue countermeasures.
In this context, we conducted a population-based study using data from the Michigan Surgical Quality Collaborative to investigate the impact of a patient’s first complication on mortality after emergency surgery. In addition to comparing outcomes between the elderly and non-elderly, we assessed the relationship between specific complications and failure to rescue rates in elderly patients across hospitals stratified by mortality.
Methods
Data Source and Study Population
We studied data from the Michigan Surgical Quality Collaborative (MSQC) prospective clinical registry from 2007 through 2012 for patients undergoing emergent general or vascular surgery. The MSQC represents a partnership between two entities- Blue Cross and Blue Shield of Michigan and 52 Michigan hospitals. This project followed standard data definitions and collection protocols as we have previously described.(11) Data collection occurs at the hospital level by specific MSQC data-collection nurses. Accuracy of data collection and maintenance is ensured by rigorous training of staff and data audits performed at participating sites. We excluded all patients under the age of 18 or those with incomplete registry data. All available variables were collected for this analysis including patient demographics, preoperative risk factors, laboratory values, perioperative factors, and 30-day postoperative morbidity and mortality.
Outcomes
The primary outcomes for this study were 30-day in-hospital mortality, major complication, and failure to rescue. We determined various in-hospital postoperative complications such as surgical site infection (superficial, deep, and organ space), deep venous thrombosis, urinary tract infection, acute renal failure, postoperative bleeding requiring transfusion, stroke, unplanned intubation, fascial dehiscence, prolonged mechanical ventilation over 48 hours, myocardial infarction, pneumonia, pulmonary embolism, sepsis, vascular graft loss, and renal insufficiency. We excluded urinary tract infection, deep venous thrombosis, renal insufficiency, and superficial surgical site infection in determining the incidence of major complications as has been previously described.(12) We grouped complications a priori by type in to three categories: cardiovascular (myocardial infarction, stroke, cardiac arrest), pulmonary (reintubation, prolonged ventilation, pneumonia), and infectious (deep and organ space surgical site infection, sepsis, septic shock). These complications have been previously identified as both common and correlated with mortality in elderly surgical patients.(8, 13) Complications were grouped by physiologic similarity, in addition to having similar management (recue) strategies. We defined failure to rescue as death following at least one major complication. For this study we were particularly interested in the sequence of patients’ complications. The MSQC registry maintains data on the dates when each documented complication occurred, defined as the date the patient met standardized registry criteria (clinical, laboratory, and radiologic as applicable) for the complication. We calculated the time to development of an initial complication as the number of days between the index operation and the first documented postoperative complication.
Statistical Analysis
We compared demographic, comorbidity, and operative differences between patients using Student’s t-test, Pearson Chi-squared (χ2) and analysis of variance (ANOVA) as appropriate. For this study, we performed two distinct analyses stratifying subjects at the (1) patient-level and the (2) hospital-level. For our patient-level analysis, we stratified subjects by age – deeming those greater than or equal to 75 years of age elderly. The remaining patients were regarded as non-elderly. We used multilevel mixed-effects regression modeling to risk-adjust all outcomes. Models were assembled using backwards-stepwise selection. We adjusted the incidence of each outcome at the patient level for variables such as age, sex, race, BMI, diabetes, smoking status, alcohol use, dyspnea, do-not-resuscitate (DNR) status, preoperative functional status, chronic obstructive pulmonary disease (COPD), pneumonia, ascites, congestive heart failure, need for dialysis, hemiplegia, transient ischemic attack (TIA), disseminated cancer, steroid use, bleeding disorders, chemotherapy, radiotherapy, sepsis, esophageal varices, prior myocardial infarction, angina, hypertension requiring medication, peripheral vascular disease, prior operations, American Society of Anesthesiologists (ASA) class, operative duration (minutes), surgeon specialty, work Relative Value Units (RVU), and the need for intraoperative transfusion. The c-statistic for all models ranged between 0.77 and 0.84 with good calibration across deciles of risk on the basis of Hosmer-Lemeshow test.
We performed a similar analysis at the hospital-level using the same covariates listed above for risk-adjustment of 30-day mortality. However, for this analysis, we adjusted for reliability using empirical Bayes techniques.(14) This was done in order to minimize the effects of random variation in mortality differences between hospitals that can result from small sample size. We then used the risk- and reliability-adjusted mortality rates to rank hospitals and group them in to tertiles- low, middle, and high mortality. We then calculated the incidence of complications and failure to rescue for each group of hospitals. Our hospital analysis focused solely on the elderly cohort of patients in order to elucidate the possible mechanism of high mortality in this demographic.
All statistical analyses were performed using Stata statistical software version12.1 (College Station, Texas). This study was approved by the University of Michigan Institutional Review Board.
Results
Patient Characteristics
Patients’ demographics and comorbid disease profile are detailed in Table 1. The median age for the non-elderly cohort was 49 (IQR=27) and 81 (IQR=6) for elderly patients. The non-elderly cohort of patients contained a higher percentage of patients of non-white race (30.3% vs. 20.9%; p<0.01). Overall, elderly patients had a higher comorbid disease burden when compared to non-elderly patients. However, a greater number of non-elderly patients were active smokers at the time of surgery (33.3% v. 9.4%; p<0.01). The most common operation for both elderly (23.9%) and non-elderly (11.1%) was colectomy. When assessing overall case distribution between cohorts.
Table 1.
Patient demographics and clinical characteristics stratified by patient age.
| Demographics | Non-Elderly (n=18,897) | Elderly (n=4,320) | P-value |
|---|---|---|---|
| Median age, y (IQR) | 49 (27) | 81 (6) | <0.01 |
| Male sex, % | 49.1% | 40.8% | <0.01 |
| Non-white race, % | 30.3% | 20.9% | <0.01 |
| Mean BMI, (Kg/m2) | 29.1 | 26.3 | <0.01 |
| Comorbidities, %
| |||
| Diabetes mellitus | 13.2% | 20.4% | <0.01 |
| Smoking in past year | 33.3% | 9.4% | <0.01 |
| Acute renal failure | 1.8% | 3.8% | <0.01 |
| Preoperative sepsis | 15.5% | 21.2% | <0.01 |
| Chronic obstructive pulmonary disease | 6.1% | 15.4% | <0.01 |
| Dialysis | 2.8% | 3.8% | <0.01 |
| Disseminated cancer | 1.8% | 3.1% | <0.01 |
| Steroid use | 3.5% | 6.1% | <0.01 |
| Albumin <3.5 g/dl | 25.4% | 53.1% | <0.01 |
| Dependent functional status | 11.4% | 33.8% | <0.01 |
| Hypertension requiring medication | 36.2% | 78.4% | <0.01 |
| DNR | 0.5% | 5.5% | <0.01 |
| Procedure Mix, %
| |||
| Colectomy | 11.1% | 23.9% | |
| Small bowel resection | 4.2% | 9.8% | |
| Laparoscopic cholecystectomy | 5.9% | 3.1% | <0.01 |
| Ventral hernia repair | 2.6% | 2.6% | |
| Lower extremity amputation | 1.1% | 1.3% | |
Comparing Outcomes Between the Non-Elderly and Elderly
Elderly patients had higher overall (46.2% v. 22.9%) and major complication (40.6% v. 19.3%) rates when compared to younger patients (p<0.01 for both). (Table 2) Of those patients with complications, elderly patients experienced a first cardiovascular (4.6% v. 2.7%; p<0.01) or pulmonary (25.6% v. 20.3%; p<0.01) complication more often than non-elderly patients. Elderly patients experienced a first infectious complication less frequently than non-elderly patients (17.2% v. 23.4%; p<0.01). Mortality was significantly higher in elderly patients (19.7% v. 4.6%; p<0.01). Failure to rescue rates were significantly higher in elderly patients who experienced a first pulmonary (38.2% v. 20.4%; p<0.01) or infectious (21.7% v. 10.3%; p<0.01) complications. (Figure 1) Failure to rescue rates were not significantly different following a first cardiovascular complication (43.1% v. 41.5%; p=0.15).
Table 2.
Rates of morbidity and mortality stratified by patient age.
| Outcomes | Non-Elderly | Elderly | P-value |
|---|---|---|---|
| Any Complication | 22.9% | 46.2% | <0.01 |
| Major Complication | 19.3% | 40.6% | <0.01 |
| Cardiovascular1 | 2.7% | 4.6% | <0.01 |
| Pulmonary1 | 20.3% | 25.6% | <0.01 |
| Infectious1 | 23.4% | 17.2% | <0.01 |
| Mortality | 4.6% | 19.7% | <0.01 |
Type of patients’ first documented complication in those patients with complications.
Figure 1.
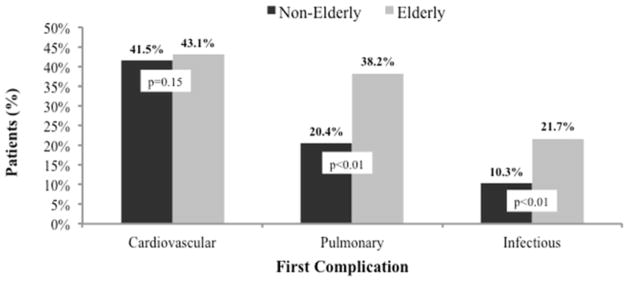
Risk-adjusted failure to rescue rates for elderly and non-elderly patients stratified by type of first documented complication.
Outcomes in Elderly Patients at Low, Middle, and High Mortality Hospitals
The incidence of any and specific postoperative complications were not significantly different across low, middle, and high mortality hospitals. (Table 3) Failure to rescue rates increased in a stepwise fashion from low, middle, and high mortality hospitals in elderly patients who experienced a first pulmonary (22.2%, 29.8%, 35.6%) or infectious (14.3%, 18.5%, 24.3%) complication (p<0.01 between low and high mortality for both). (Figure 2) Failure to rescue rates following a first cardiovascular complication were not significantly different across low, middle, and high mortality hospitals (41.2%, 38.3%, 44.1%; p=0.32).
Table 3.
Distribution of overall and first complications in elderly patients across hospitals stratified by mortality.
| Outcomes | Hospital Mortality
|
p-value2 | ||
|---|---|---|---|---|
| Low | Middle | High | ||
| Any Complication | 48.5% | 44.5% | 44.2% | 0.91 |
| Major Complication | 42.4% | 39.5% | 38.6% | 0.84 |
| Cardiovascular1 | 4.6% | 5.7% | 3.7% | 0.44 |
| Pulmonary1 | 26.0% | 25.9% | 23.9% | 0.36 |
| Infectious1 | 17.0% | 21.5% | 14.4% | 0.18 |
Type of patients’ first documented complication in those patients with complications.
P-value represents comparison of means across three tertiles.
Figure 2.
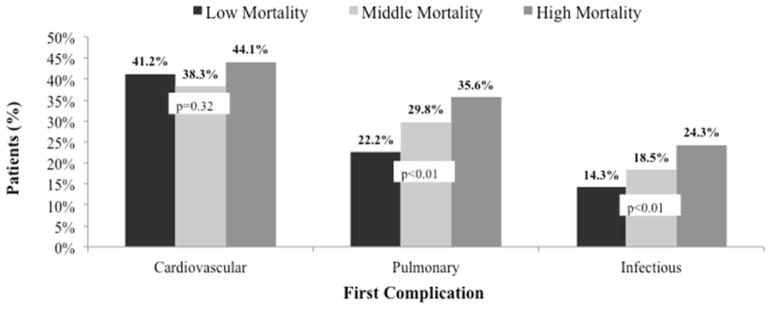
Failure to rescue rates for elderly patients treated at low, middle, and high mortality hospitals. Patients are stratified by the type of first documented complication. P-values represent the comparison between low and high mortality hospitals.
Discussion
In this study, we report on differences in failure to rescue following specific complications in an elderly emergent surgical population. We found that failure to rescue rates are markedly different between elderly and non-elderly patients following an initial pulmonary or infectious complication. In contrast, there were no significant differences observed after cardiovascular complications. This observation persisted at the hospital-level, where high mortality centers failed to rescue elderly patients from pulmonary or infectious complications at significantly higher rates than low mortality centers. These findings offer more granular data for hospitals as they address failure to rescue in elderly surgical patients.
Managing the risks of surgical care in elderly patients is complex. Opportunities to improve outcomes exist both before and after the operation. Recent evidence suggests that addressing issues such as nutritional status and polypharmacy can enhance risk-stratification and reduce morbidity in the elderly population.(15, 16) However, the acuity of elderly patients presenting for emergent surgical care renders many preoperative care practices impractical. Shifting the focus to postoperative care can identify tangible quality improvement targets for surgeons and hospitals.(6, 17) Intuitively, certain complications are more serious than others – specifically those associated with cardiopulmonary compromise.(7, 8, 13, 18) Others have shown that advanced age also predisposes patients to more serious renal and wound complications.(19) How these complications are managed may be a crucial determinant in how elderly patients fare after emergent operations.
Here we have shown that a patient’s first complication is important. Recognition of a patient’s first complication initiates the rescue effort. Despite similar outcomes following cardiovascular complications, elderly patients died more frequently than the non-elderly after an initial pulmonary or infectious complication. Clearly, cardiovascular complications are important for all patients and failure to rescue rates were universally high. For these complications, age may be less of a determinant of mortality than the physiologic insult itself. We also posit that diagnosis and management of a myocardial infarction, for example, is a highly protocolled endeavor.(20) Rescue practices may not vary significantly between patients or hospitals. Conversely, the diagnosis and management of postoperative pneumonia may be more subjective.(21, 22) How hospitals rescue patients from pulmonary and infectious complications underscores differences surgical mortality for elderly patients. This observation is substantiated by the fact that our results did not differ after accounting for the development of subsequent complications. Clinical management protocols have been shown to improve outcomes in patients with sepsis or ventilator associated pneumonia.(23, 24) However, few studies systematically examine these interventions for surgical patients. Further, the timeliness with which protocols are initiated may be particularly important for following surgery – as complications must first be recognized and diagnosed by care teams. Surgeons must also consider whether management protocols differ in efficacy between medical and surgical patients. Nonetheless, protocolled practices have improved the management of pulmonary and infectious disease processes and may represent a novel avenue for surgical quality improvement.
This study should be interpreted with consideration of several limitations. This is a retrospective study and as a result we are unable to assert causation. As with any large data registry, there are issues with data reliability and accuracy. However, the MSQC performs data audits and educates abstractors to ensure accuracy.(11) Complications are identified through specific clinical criteria. Nonetheless, we are unable to account for severity of complications. While abstractors report the date of diagnosis for each complication, this information is contingent on care teams documenting these findings in the medical record. Although this is a limitation, we do not believe that this would confound our data differentially for patients of different ages. Further, we do not have information on specific care practices that may influence outcomes at these hospitals. Despite this, we believe this data provides the necessary context to study these critical issues.
In the emergent setting, surgeons rely on their postoperative management to mitigate the high risks ascribed to elderly patients. This study substantiates growing sentiments that appropriate surgical care is age-specific. Efforts to improve the coordination of care for pulmonary and infectious complications may attenuate the large mortality differences between elderly and non-elderly patients. Our Statewide surgical collaborative will use this information to augment existing quality improvement initiatives for Michigan’s elderly surgical patients.
Acknowledgments
This study was supported by National Institute on Aging grant R01AG042340 awarded to Drs. Birkmeyer, Campbell, and Ghaferi.
Abbreviations
- MSQC
Michigan Surgical Quality Collaborative
- ASA
American Society of Anesthesiologists
- RVU
Relative value units
Footnotes
Disclosure: John D. Birkmeyer is Chief Scientific Officer with a financial interest in Arbormetrix, Inc., which had no role in this study. The other authors have no conflicts of interest to disclose.
Presented at the Surgical Forum, American College of Surgeons 99th Annual Clinical Congress, Washington DC, October 2013.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJ, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Annals of surgery. 2012 Jan;255(1):1–5. doi: 10.1097/SLA.0b013e3182402c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Annals of surgery. 2003 Aug;238(2):170–7. doi: 10.1097/01.SLA.0000081085.98792.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Variation in quality of care after emergency general surgery procedures in the elderly. Journal of the American College of Surgeons. 2011 Jun;212(6):1039–48. doi: 10.1016/j.jamcollsurg.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005 Mar;53(3):424–9. doi: 10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 5.Scarborough JE, Pappas TN, Bennett KM, Lagoo-Deenadayalan S. Failure-to-pursue rescue: explaining excess mortality in elderly emergency general surgical patients with preexisting “do-not-resuscitate” orders. Annals of surgery. 2012 Sep;256(3):453–61. doi: 10.1097/SLA.0b013e31826578fb. [DOI] [PubMed] [Google Scholar]
- 6.Sheetz KH, Waits SA, Krell RW, Campbell DA, Jr, Englesbe MJ, Ghaferi AA. Improving mortality following emergent surgery in older patients requires focus on complication rescue. Annals of surgery. 2013 Oct;258(4):614–7. doi: 10.1097/SLA.0b013e3182a5021d. discussion 7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY. Identification of specific quality improvement opportunities for the elderly undergoing gastrointestinal surgery. Arch Surg. 2009 Nov;144(11):1013–20. doi: 10.1001/archsurg.2009.114. [DOI] [PubMed] [Google Scholar]
- 8.Gajdos C, Kile D, Hawn MT, Finlayson E, Henderson WG, Robinson TN. Advancing age and 30-day adverse outcomes after nonemergent general surgeries. J Am Geriatr Soc. 2013 Sep;61(9):1608–14. doi: 10.1111/jgs.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. The New England journal of medicine. 2009 Oct 1;361(14):1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 10.Silber JH, Williams SV, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Medical care. 1992 Jul;30(7):615–29. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Campbell DA, Jr, Englesbe MJ, Kubus JJ, et al. Accelerating the pace of surgical quality improvement: the power of hospital collaboration. Arch Surg. 2010 Oct;145(10):985–91. doi: 10.1001/archsurg.2010.220. [DOI] [PubMed] [Google Scholar]
- 12.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in Hospital Mortality Associated with Inpatient Surgery. New England Journal of Medicine. 2009:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 13.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Annals of surgery. 2009 Dec;250(6):1029–34. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 14.Dimick JB, Ghaferi AA, Osborne NH, Ko CY, Hall BL. Reliability adjustment for reporting hospital outcomes with surgery. Annals of surgery. 2012 Apr;255(4):703–7. doi: 10.1097/SLA.0b013e31824b46ff. [DOI] [PubMed] [Google Scholar]
- 15.Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. Journal of the American College of Surgeons. 2012 Oct;215(4):453–66. doi: 10.1016/j.jamcollsurg.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 16.Robinson TN, Eiseman B, Wallace JI, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Annals of surgery. 2009 Sep;250(3):449–55. doi: 10.1097/SLA.0b013e3181b45598. [DOI] [PubMed] [Google Scholar]
- 17.Smith M, Hussain A, Xiao J, et al. The importance of improving the quality of emergency surgery for a regional quality collaborative. Annals of surgery. 2013 Apr;257(4):596–602. doi: 10.1097/SLA.0b013e3182863750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kazaure HS, Roman SA, Rosenthal RA, Sosa JA. Cardiac arrest among surgical patients: an analysis of incidence, patient characteristics, and outcomes in ACS-NSQIP. JAMA Surg. 2013 Jan;148(1):14–21. doi: 10.1001/jamasurg.2013.671. [DOI] [PubMed] [Google Scholar]
- 19.Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. Journal of the American College of Surgeons. 2006 Dec;203(6):865–77. doi: 10.1016/j.jamcollsurg.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 20.van Waes JA, Nathoe HM, de Graaff JC, et al. Myocardial injury after noncardiac surgery and its association with short-term mortality. Circulation. 2013 Jun 11;127(23):2264–71. doi: 10.1161/CIRCULATIONAHA.113.002128. [DOI] [PubMed] [Google Scholar]
- 21.Canadian Critical Care Trials G. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. The New England journal of medicine. 2006 Dec 21;355(25):2619–30. doi: 10.1056/NEJMoa052904. [DOI] [PubMed] [Google Scholar]
- 22.Wren SM, Martin M, Yoon JK, Bech F. Postoperative pneumonia-prevention program for the inpatient surgical ward. Journal of the American College of Surgeons. 2010 Apr;210(4):491–5. doi: 10.1016/j.jamcollsurg.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 23.Ding S, Kilickaya O, Senkal S, Gajic O, Hubmayr RD, Li G. Temporal trends of ventilator-associated pneumonia incidence and the effect of implementing health-care bundles in a suburban community. Chest. 2013 Nov;144(5):1461–8. doi: 10.1378/chest.12-1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrer R, Artigas A, Levy MM, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA : the journal of the American Medical Association. 2008 May 21;299(19):2294–303. doi: 10.1001/jama.299.19.2294. [DOI] [PubMed] [Google Scholar]


