Abstract
Epidemiologic studies have documented that injury survivors are at increased risk for suicide. We evaluated 206 trauma survivors to examine demographic, clinical, and injury characteristics associated with suicidal ideation during hospitalization and across one-year. Results indicate that mental health functioning, depression symptoms, and history of mental health services were associated with suicidal ideation in the hospital; being a parent was a protective factor. Pre-injury posttraumatic stress disorder symptoms, assaultive injury mechanism, injury-related legal proceedings, and physical pain were significantly associated with suicidal ideation across one-year. Readily identifiable risk factors early after traumatic injury may inform hospital-based screening and intervention procedures.
Introduction
Suicide accounts for approximately 1 million deaths annually worldwide and is the 11th leading cause of death in the United States. Advances in the establishment of empirically supported psychosocial treatments to reduce suicide and suicide attempts have been documented in the research literature (Brown et al., 2005; Fleischmann et al., 2008; Linehan et al., 2006; Motto & Bostrom, 2001); however, these treatment advances have not coincided with a significant decline in the overall suicide rate. One potential explanation for this observation is that many suicidal individuals may not be identified and treated unless they are currently receiving mental health services or survive a suicide attempt (Bruffaerts et al., 2011). Although suicide attempt survivors are estimated to be at 30–40% increased risk for completed suicide compared to the general population (Harris & Barraclough, 1997), previous research suggests that up to 56% of individuals die as a result of their first suicide attempt (Isometsa & Lonnqvist, 1998). Thus, it is imperative to improve earlier identification of suicidal individuals who may be undertreated by the health care system.
Each year in the United States over 30 million individuals visit acute care medical settings after incurring traumatic injuries and between 1.5–2.5 million Americans are so severely injured annually that they require inpatient hospitalization (Bonnie, Fulco, & Liverman, 1999; Centers for Disease Control, 2009). A series of epidemiologic investigations suggest that hospitalized injured patients are at increased risk for suicide (Grossman, Soderberg, & Rivara, 1993; Ryb, Soderstrom, Kufera, & Dischinger, 2006; Zambon, Laflamme, Spolaore, Visentin, & Hasselberg, 2011). Grossman et al. reports a 5 times greater risk of suicide for patients previously admitted for unintentional injuries and 4.5 times greater risk for patients who had been previously admitted for assault compared to the general population in Washington State (Grossman, et al., 1993). Ryb and colleagues examined data from a sample (N = 27,399) of patients discharged from a level 1 trauma center for up to 14.5 years and found trauma patients to have significantly greater risk for suicide (standard mortality rate = 1.71) as compared to the general population (Ryb, et al., 2006). A more recent population-based study of N = 1,616,342 subjects aged 7–26 years found patients hospitalized for unintentional injuries to be at 3 times greater risk for suicide compared to the general population (Zambon, et al., 2011).
Beyond these epidemiologic studies, few prospective clinical investigations have comprehensively assessed demographic, clinical, and injury characteristics associated with suicidal ideation and behaviors in order to inform hospital based screening and intervention procedures. Although high posttraumatic stress disorder (PTSD) symptom levels occur in approximately 20% of US trauma survivors (Zatzick et al., 2007), a literature review revealed no investigations that assessed suicidal ideation among civilian traumatic injury survivors with high PTSD symptom levels. A series of investigations in US veteran and other patient populations suggest that PTSD may be associated with markedly elevated rates of suicidal ideation (Ferrada-Noli, Asberg, Ormstad, Lundin, & Sundbom, 1998; Jakupcak et al., 2010; Nock et al., 2009; Ryb, et al., 2006). Other investigations suggest that additional risk factors for suicidal ideation among hospitalized patients may include prior psychiatric and alcohol use diagnoses (Botega et al., 2010; Kishi, Robinson, & Kosier, 2001b). Potential risk factors for suicide not comprehensively examined among physically injured patients include physical pain (Almeida et al., 2012; Van Orden & Conwell, 2011), trauma history and physical assault (Nock & Kessler, 2006), absence of children (Clark & Fawcett, 1994), history of mental health services (Appleby et al., 1999), quality of life functioning (Goldney, Fisher, Wilson, & Cheok, 2000), homelessness (Eynan et al., 2002), traumatic brain injury (Bryan & Clemans, 2013), and involvement in legal proceedings (Logan, Hall, & Karch, 2011).
A review of the existing literature revealed few studies that assessed suicidal ideation among hospitalized patients and also followed patients longitudinally. Kishi et al. reports in a clinical sample of rehabilitation patients that a current plan to suicide during hospitalization was significantly associated with depression, current use of psychotropic medication, alcohol use disorders, younger age, and smoking (Kishi, et al., 2001b); the onset of post-hospitalization suicidal ideation in the same sample was related to higher levels of depression and lack of social support during the index admission (Kishi, Robinson, & Kosier, 2001a).
The current study had two main objectives. First, it aimed to evaluate the presence of suicidal ideation in hospitalized survivors of traumatic injury during the inpatient stay and longitudinally that may have been at increased risk due to high early post-injury PTSD symptom levels. Second, the study aimed to comprehensively assess readily identifiable demographic and clinical risk factors associated with suicidal ideation both during the hospitalization and over the course of the year after injury. We hypothesized that elevated mental health symptoms, including anxiety and depression, during hospitalization would be associated with the presence of suicidal ideation at baseline and longitudinally. We also explored the associations between other demographic, clinical, and injury characteristics present at the time of the inpatient admission and the presence of suicidal ideation at baseline and longitudinally.
Methods
Sample
The current study utilized data from the Trauma Survivors Outcomes and Support Study II (Zatzick et al., 2013), which recruited patients from April 2006 to September 2009 at Harborview Medical Center, the level 1 trauma center affiliated with the University of Washington. English speaking patients requiring admission to an inpatient surgical floor were eligible to participate in the study unless they were < 18 years of age, lived > 100 miles from the hospital, required immediate psychiatric services (e.g., acutely psychotic, persistently altered mental status), had recent histories of severe violence and were likely to face criminal charges, or were currently incarcerated. Patients with self-inflicted injuries were excluded. A member of the research team visited patients at their bedside, provided information about the study, and led the patient through a written informed consent process. Injured patients were screened twice for high early PTSD symptom levels in the days and weeks after injury hospitalization (Zatzick et al., 2011). Patients with sustained high PTSD symptom levels on both assessments were recruited into the study. After completing a baseline surgical ward assessment, patients were then randomized to receive either a stepped collaborative care intervention or care as usual for the next 12 months, the results of which have been published elsewhere (Zatzick, et al., 2013). Patients completed follow-up interviews at 1, 3, 6, 9, and 12 months. All study procedures were approved by the University of Washington Institutional Review Board.
Measures
Suicidal ideation and depression clinical characteristics
Presence of suicidal ideation was determined by any positive score on item 9 of the Patient Health Questionnaire depression screen (PHQ-9), which inquires about current thoughts of being better off dead or hurting one’s self in some way (Kroenke, Spitzer, & Williams, 2001). The PHQ-9 is a validated depression screening instrument that takes minutes to complete and is used in numerous clinical settings. Item 9 of the PHQ-9 has shown acceptable psychometric properties in detecting suicidal ideation when compared to a gold standard structured clinical interview, with specificity of 0.84 and sensitivity of 0.69 (Uebelacker, German, Gaudiano, & Miller, 2011) and has been used to measure suicidal ideation in general medical settings (Bauer, Chan, Huang, Vannoy, & Unutzer, 2012). We utilized the 8 remaining items on the PHQ-9 to determine severity of depressive symptoms (referred to below as PHQ-8) (Kroenke et al., 2009). Previous history of depressive episodes was also derived from the PHQ-9.
Posttraumatic stress disorder symptoms
The PTSD Checklist Civilian Version (PCL-C) was utilized to assess severity of posttraumatic stress (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Ruggiero, Del Ben, Scotti, & Rabalais, 2003). The PCL-C is a 17-item measure developed to assess PTSD diagnosis criteria as it is defined by the American Psychiatric Association Diagnostic and Statistical Manual (DSM-IV)(American Psychiatric Association, 2000). Participants were asked to use a five-point Likert scale ranging from one (“not at all”) to five (“extremely”) to rate how bothered they had been by each of the PCL-C items, and were asked to think about their symptoms “since the event in which they were injured”. Past research has established the reliability and validity of the PCL-C across trauma-exposed populations (Bliese et al., 2008). The current study applied a PCL-C cutoff of ≥ 35 as an indicator of high early PTSD symptom levels based on prior experience in early intervention studies and literature review (Zatzick, et al., 2011).
Other clinical characteristics
We used items from the National Co-morbidity Survey investigations to determine history of traumatic events, history of posttraumatic stress, and history of receiving mental health services (Mackenzie et al., 2007). Based upon previous research findings, we dichotomized history of traumatic events into two categories (< 4 or ≥ 4 types of traumatic events; (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995)). Physical and mental health functioning were assessed with the Physical and Mental Component Summaries of the Medical Outcomes Study Short Form 36 (Ware & Sherbourne, 1992). We used single items screens derived from the first item of the Alcohol Use Disorders Identification Test to assess alcohol, marijuana, amphetamines, cocaine, and opiate use. A series of investigations in acute and primary care general medical settings have established the reliability and validity of single item substance use screens (Donovan et al., 2011; Ramchand et al., 2009; Saitz, 2010). Finally, we measured physical pain using a single item screen adapted from the short-form McGill Pain Questionnaire (Melzack, 1987).
Injury characteristics
The investigation determined injury severity at baseline during the index admission from the medical record International Classification of Diseases, 9th Revision, Clinical Modification Codes using the Abbreviated Injury Scale and Injury Severity Score (Blanchard, et al., 1996; Civil & Schwab, 1985; Mackenzie, et al., 2007). Additional clinical characteristics abstracted from the electronic medical record included injury type (intentional or unintentional), blood alcohol content (negative or not tested vs. positive), whether care was provided in an intensive care unit, and any indication of drug use upon admission through urinalysis lab results.
Demographic characteristics
The baseline interview included a comprehensive assessment of socio-demographic characteristics that were examined as correlates of suicidal ideation. These include patient age, gender, race, high school completion, current marital status (married/living with partner vs. not married), insurance status (private, public, or none), traumatic brain injury (none, mild, or moderate/severe), whether the patient was involved in a legal issue since injury occurred, current homelessness (yes/no), if the patient has children (yes/no), and patient’s income in previous year (dichotomized into < or ≥ $30,000).
Statistical Analysis
We first calculated the frequency of patients who reported suicidal ideation during the baseline hospitalization assessment and at each of the follow-up interviews. Next, we used Poisson regression to estimate univariate associations between baseline hospitalization demographic and clinical characteristics and the presence of suicidal ideation during the inpatient stay. Finally, we examined the associations between the baseline demographic and clinical characteristics and suicidal ideation longitudinally using mixed-effect Poisson regression with robust error variance to account for intra-individual correlations in longitudinal data. The dependent variable for all regression analyses was the dichotomized (yes/no) PHQ-9 suicide item 9. For both baseline and longitudinal regression analyses, variables that were associated with suicidal ideation at p ≤ 0.20 were retained for multivariable models (Hosmer & Lemeshow, 2000). A Poisson regression model with robust error variance to estimate adjusted relative risks (RRs) and 95% confidence intervals (Zou, 2004) was then fit using a backwards elimination method that retained only those variables accounting for significant variance above and beyond other significant correlates (Zatzick, et al., 2007). Given their important role in injury prevention research, age, gender, and injury severity score were included in the final baseline model (Zatzick, et al., 2007). Time and intervention group were also included in the final longitudinal model.
Results
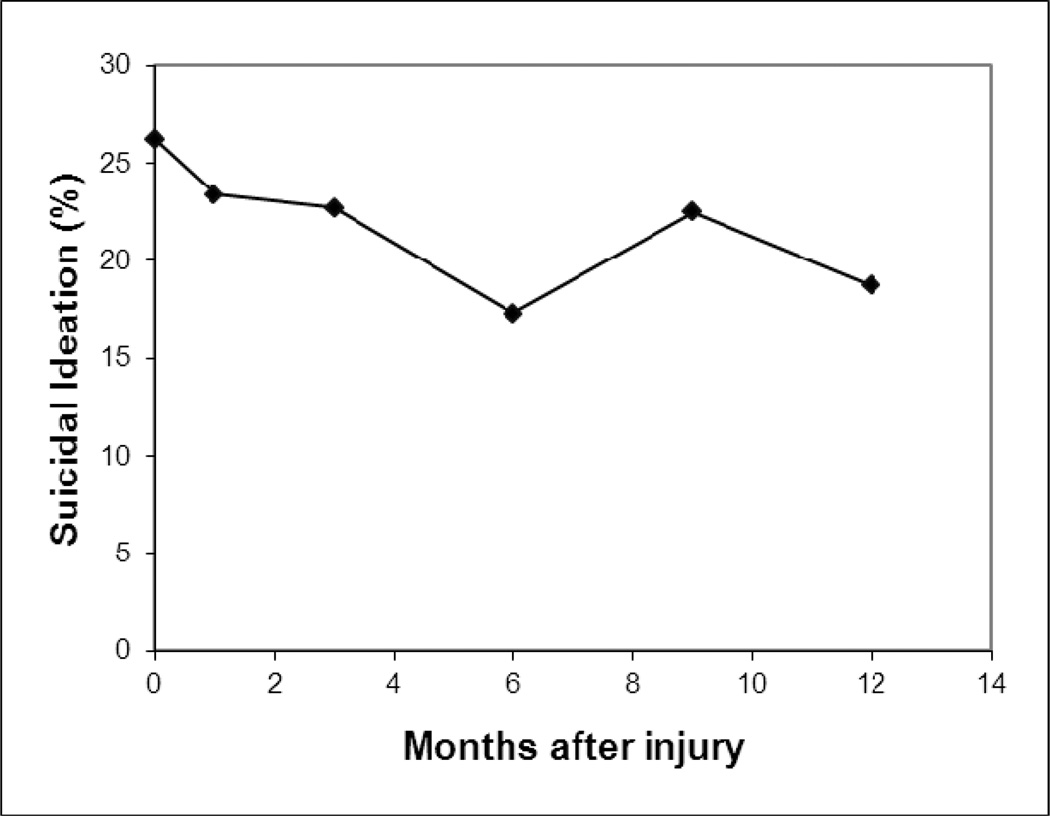
Twenty-six percent of adults endorsed suicidal ideation during the baseline hospital admission (Figure 1). The investigation attained 85%, 79%, 78%, 75%, and 81% follow-up at each of the respective assessments. Forty-nine percent of patients endorsed suicidal ideation at some point during the 12-month period after the baseline assessment.
Figure 1.
Percentage of study patients endorsing suicidal ideation at each time point.
Univariate Analyses
Univariate factors associated with suicidal ideation while hospitalized included having ever visited a mental health practitioner, trauma history screening of ≥ 4, history of a major depressive episode, higher PCL-C total score, higher PHQ-8 depression total score, worse mental health functioning, and positive screen for substance use (Table 1). Associations across the 12-month follow-up period differed, with older age and positive blood alcohol content on admission being associated with significant increases in suicidal ideation, while a positive screen for marijuana was associated with a significantly reduced risk of reporting suicidal ideation (Table 1).
Table 1.
Univariate Associations Between Demographic, Injury, Clinical Characteristics and Suicidal Ideation During Hospitalization and Longitudinally Across 12-Months
| Characteristics | Hospitalization | Longitudinally Across 12-Months^ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Not Suicidal % (n = 152) |
Suicidal % (n = 54) |
RR | Lower CI | Upper CI | RR | Lower CI | Upper CI | |
| Demographic | |||||||||
| Age, mean (SD), years | 39.1(13.2) | 37.3(13.0) | 0.99 | 0.97 | 1.01 | 1.02* | 1.00 | 1.03 | |
| Female | 99 | 49.3 | 44.4 | 0.86 | 0.54 | 1.37 | 1.13 | 0.76 | 1.68 |
| Race/ethnicity | |||||||||
| White | 123 | 56.6 | 68.5 | Reference | Reference | ||||
| Black | 38 | 21.0 | 11.1 | 0.52 | 0.24 | 1.15 | 0.90 | 0.56 | 1.42 |
| American Indian | 27 | 14.5 | 9.3 | 0.62 | 0.27 | 1.42 | 1.15 | 0.62 | 2.14 |
| Asian | 12 | 5.9 | 5.5 | 0.83 | 0.30 | 2.30 | 0.73 | 0.22 | 2.49 |
| Latino | 6 | 2.0 | 5.6 | 1.66 | 0.71 | 3.87 | 0.37 | 0.07 | 1.87 |
| High school or equivalent degree | 109 | 54.0 | 50.0 | 0.89 | 0.56 | 1.41 | 1.36 | 0.91 | 2.04 |
| Marital status | 154 | 74.3 | 75.9 | 1.06 | 0.62 | 1.83 | 1.07 | 0.70 | 1.64 |
| Not married | |||||||||
| Homeless/Shelter | 19 | 8.0 | 13.0 | 1.46 | 0.77 | 2.77 | 1.64 | 0.73 | 3.68 |
| Medical Insurance | |||||||||
| None | 50 | 23.0 | 27.8 | Reference | Reference | ||||
| Public | 111 | 52.6 | 57.4 | 0.93 | 0.55 | 1.57 | 1.31 | 0.78 | 2.18 |
| Private | 45 | 24.4 | 14.8 | 0.59 | 0.28 | 1.27 | 0.65 | 0.33 | 1.26 |
| Household income | |||||||||
| ≥ $30,000 | 55 | 27.0 | 25.9 | Reference | Reference | ||||
| < $30,000 | 82 | 38.8 | 42.6 | 1.10 | 0.62 | 1.95 | 1.22 | 0.78 | 1.93 |
| Unknown | 69 | 34.2 | 31.5 | 0.97 | 0.52 | 1.79 | 0.97 | 0.58 | 1.62 |
| Have Children | 122 | 62.9 | 50.0 | 0.68 | 0.43 | 1.07 | 1.08 | 0.72 | 1.62 |
| Acute care injury & medical | |||||||||
| Injury severity category | |||||||||
| 0–8 | 46 | 23.0 | 20.4 | Reference | Reference | ||||
| 9–15 | 92 | 47.4 | 37.0 | 0.91 | 0.48 | 1.74 | 0.79 | 0.49 | 1.28 |
| ≥ 16 | 68 | 29.6 | 42.6 | 1.41 | 0.76 | 2.62 | 1.14 | 0.70 | 1.84 |
| Traumatic brain injury | |||||||||
| None | 127 | 64.5 | 53.7 | Reference | Reference | ||||
| Mild | 55 | 25.6 | 29.6 | 1.27 | 0.75 | 2.15 | 1.22 | 0.78 | 1.91 |
| Moderate/severe | 24 | 9.9 | 16.7 | 1.64 | 0.89 | 3.02 | 1.72 | 1.02 | 2.90 |
| Injury type, assault | 47 | 19.7 | 31.5 | 1.55 | 0.97 | 2.50 | 1.73 | 1.14 | 2.61 |
| Treated in Intensive Care Unit | 70 | 30.9 | 42.6 | 1.44 | 0.91 | 2.28 | 1.27 | 0.84 | 1.92 |
| Clinical | |||||||||
| History of mental health services | 149 | 68.4 | 83.3 | 1.91* | 1.27 | 3.10 | 1.84 | 0.99 | 3.43 |
| Trauma history screen ≥ 4 | 161 | 74.3 | 88.9 | 2.24* | 1.02 | 4.90 | 1.52 | 0.91 | 2.53 |
| History of posttraumatic stress | 130 | 62.5 | 64.8 | 1.08 | 0.66 | 1.75 | 1.84 | 1.19 | 2.85 |
| History of major depressive episode | 181 | 84.9 | 96.3 | 3.59* | 0.93 | 13.88 | 1.66 | 0.59 | 4.68 |
| Baseline 1st PCL-C total score, mean (SD)† | 49.5(9.8) | 53.8(11.7) | 1.03* | 1.01 | 1.05 | 1.01 | 0.99 | 1.03 | |
| Baseline PHQ-8 depression total score, mean (SD)† | 12.6(5.0) | 16.1(4.9) | 1.11*** | 1.06 | 1.17 | 1.01 | 0.97 | 1.05 | |
| SF12 mental function | 44.7(11.9) | 38.6(11.4) | 0.97** | 0.95 | 0.99 | 0.99 | 0.97 | 1.00 | |
| SF12 physical function | 49.8(10.9) | 48.4(12.0) | 0.99 | 0.97 | 1.01 | 0.98 | 0.96 | 0.998 | |
| Pre-injury AUDIT-C score, mean (SD) | 3.3(3.1) | 3.5(3.7) | 1.01 | 0.94 | 1.09 | 1.01 | 0.95 | 1.07 | |
| Positive blood alcohol on admission | 73 | 33.6 | 40.7 | 1.25 | 0.79 | 1.99 | 1.58* | 1.07 | 2.33 |
| Positive for single item substance use screening | 50 | 19.1 | 38.9 | 1.99** | 1.27 | 3.10 | 0.83 | 0.50 | 1.35 |
| Positive for single item marijuana screening | 70 | 30.9 | 42.6 | 1.44 | 0.91 | 2.28 | 0.54* | 0.35 | 0.83 |
| Urine toxicology screen positive for substance use | 107 | 53.3 | 48.2 | 0.86 | 0.54 | 1.36 | 1.11 | 0.75 | 1.64 |
| Urine toxicology screen positive for marijuana | 34 | 15.8 | 18.5 | 1.15 | 0.64 | 2.06 | 0.99 | 0.59 | 1.67 |
| Pain Rating | 6.9(2.1) | 6.8(2.2) | 0.98 | 0.88 | 1.09 | 1.13 | 1.03 | 1.23 | |
| Use weapon to harm other | 8 | 2.7 | 7.7 | 1.99 | 0.95 | 4.16 | 1.06 | 0.40 | 2.78 |
| Arrested for violent crime | 22 | 10.2 | 13.2 | 1.23 | 0.64 | 2.39 | 0.59 | 0.26 | 1.33 |
| Injury-related legal proceedings | 8 | 4.1 | 3.9 | 0.95 | 0.28 | 3.22 | 4.12 | 2.53 | 6.70 |
| Number of posttraumatic concerns | 1.5(0.7) | 1.5(0.9) | 1.10 | 0.85 | 1.43 | 0.82 | 0.64 | 1.06 | |
For PCL-C and PHQ-8 baseline assessments inpatients were asked to report symptoms since the injury event.
Abbreviations: AUDIT-C, The Alcohol Use Disorders Identification Test – Consumption Items; PCL-C, PTSD Checklist Civilian Version; PHQ, Patient Health Questionnaire; PTSD, posttraumatic stress disorder; SD, standard deviation, CI, confidence interval, RR, risk ratio
All longitudinal models adjust for time and baseline suicidal ideation
p < .05
p < .01
p < .001
Multivariable Analyses
The baseline hospitalization regression revealed significant associations between increased risk of suicidal ideation during hospitalization and higher PHQ-8 total score, history of visiting a mental health practitioner, and worse mental health functioning (Table 2). Having a child was a significant protective factor against endorsing suicidal ideation during hospitalization (Table 2). In the longitudinal regression models, older age, suicidal ideation during the index hospitalization, pre-injury PTSD symptoms, assaultive injury mechanism, injury related legal proceedings, and higher physical pain were all significantly associated with suicidal ideation across the 12-month follow-up period.
Table 2.
Multivariable Model Measuring Associations Between Demographic, Injury, Clinical Characteristics and Suicidal Ideation During Hospitalization and Longitudinally Across 12-Month
| Hospitalization | Longitudinally Across 12-Months | |||||||
|---|---|---|---|---|---|---|---|---|
| RR | Lower CI | Upper CI | p value | RR | Lower CI | Upper CI | p value | |
| Time | ||||||||
| Baseline | Reference | Reference | ||||||
| 1 month | - | - | - | - | 1.03 | 0.76 | 1.40 | 0.86 |
| 3 month | - | - | - | - | 0.75 | 0.51 | 1.09 | 0.13 |
| 6 month | - | - | - | - | 1.00 | 0.71 | 1.40 | 1.00 |
| 12 month | - | - | - | - | 0.82 | 0.57 | 1.18 | 0.29 |
| Gender | 0.77 | 0.50 | 1.19 | 0.24 | 1.08 | 0.72 | 1.60 | 0.72 |
| Age | 1.00 | 0.98 | 1.02 | 0.75 | 1.03 | 1.01 | 1.04 | < 0.001 |
| ISS category | ||||||||
| 0–8 | Reference | Reference | ||||||
| 9–15 | 0.90 | 0.48 | 1.68 | 0.75 | 0.93 | 0.58 | 1.49 | 0.75 |
| ≥ 16 | 1.64 | 0.92 | 2.94 | 0.10 | 1.51 | 0.94 | 2.43 | 0.09 |
| History of mental health visit | 1.89 | 1.02 | 3.50 | 0.04 | - | - | - | - |
| Having children | 0.55 | 0.35 | 0.85 | 0.01 | - | - | - | - |
| PHQ8 total score | 1.12 | 1.07 | 1.19 | < 0.001 | - | - | - | - |
| SF12 mental subscale | 0.98 | 0.97 | 1.00 | 0.04 | - | - | - | - |
| Suicidal ideation in hospital | - | - | - | - | 3.34 | 2.28 | 4.89 | < 0.001 |
| History of Posttraumatic stress | - | - | - | - | 1.72 | 1.09 | 2.71 | 0.02 |
| Injury type, assault | - | - | - | - | 2.03 | 1.28 | 3.20 | < 0.01 |
| Injury-related legal proceedings | - | - | - | - | 4.32 | 2.24 | 8.33 | < 0.001 |
| Pain rating | - | - | - | - | 1.11 | 1.00 | 1.22 | 0.05 |
| Treatment Condition, Control | - | - | - | - | 1.19 | 0.83 | 1.71 | 0.34 |
For PHQ-8 baseline assessment inpatients were asked to report symptoms since the injury event.
Abbreviations: RR, risk ratio; CI, confidence interval ISS, injury severity score; PHQ, Patient Health Questionnaire
Discussion
The current study provides novel information about risk factors for suicidal ideation during acute inpatient hospitalization following a traumatic physical injury, as well as the 12-month post-hospitalization period. Results suggest that there are specific factors significantly associated with elevated risk of suicidal ideation among physically injured inpatients with high PTSD symptom levels including the presence of depressive symptoms, a history of receiving mental health services, and worse general mental health functioning. These findings are consistent with the literature on risk factors for suicidal ideation in acute inpatient, primary care, and inpatient psychiatry settings.
Our finding that being a parent is associated with significantly reduced likelihood of experiencing suicidal ideation is consistent with previous research (Clark & Fawcett, 1994) and the Interpersonal-Psychological Theory of Suicide which posits that social connectedness is a buffer against desiring death (Van Orden et al., 2010). Specifically, the model identifies individuals who experience thwarted belongingness and perceived burdensomeness as having a greater likelihood of being drawn towards suicide, while patients who have experienced greater physical injury are likely to move closer towards acquiring the capability to suicide through systematic reductions in pain sensitivity and fear-related cognitions about self-injury. This model can be readily applied to our inpatient trauma population, where patients are buoyed by the support of their social networks, but may also place a greater burden on families who must care for them during a potentially lengthy and expensive rehabilitation process. Acquired capability is a quantitative developmental construct, in that patients accumulate risk across time but cannot regress towards a lower risk profile. Trauma patients are therefore thrust forward on this spectrum of lethality given their most recent injury.
The inpatient demographic and clinical correlates of suicidal ideation differed in the baseline and longitudinal analyses. We found older age, history of PTSD, having been assaulted during the index injury, greater physical pain, ongoing legal proceeding related to the injury, and baseline report of suicidal ideation to be associated with suicidal ideation in the 12 months following hospital discharge. These findings are consistent with previous research demonstrating elevated risk of suicide in patients assaulted and treated for physical injuries in an inpatient medical setting (Grossman, et al., 1993), while to our knowledge, this is the first study to examine the impact of physical pain, legal involvement, and PTSD on endorsement of suicidal ideation in a prospective study of injured trauma survivors. These findings suggest that the presence of suicidal ideation during the acute injury and longitudinal rehabilitation periods may reflect difficulties with different aspects of coping and recovery. In the multivariable models, current mental health functioning seemed to have a greater impact on endorsing suicidal thoughts, whereas the longitudinal correlates included characteristics specifically linked to the context of the trauma, including type of injury and ongoing legal proceedings. We Although we found those who reported suicidal ideation in the hospital were more likely to do so across the follow-up period, we were not able to determine the extent to which suicidal ideation would have been present regardless of the index traumatic injury given the limitations of the research design.
The study findings also demonstrated a lack of significant associations for several empirically-supported risk factors for suicidal ideation. These included severity of traumatic brain injury, presence of alcohol and substance abuse, quality of life functioning, and homelessness. Of these, severe traumatic brain injury did demonstrate a growing impact on presence of suicidal ideation in the univariate longitudinal model, but still did not account for significant partial variance in the multivariable model. While this subgroup was noticeably under-powered (n=26), the course of increasingly severe mental health functioning across time is consistent with what would be expected for patients with this type of injury. Alternatively, it may be that certain correlates are less impactful regarding suicidal ideation when additional information is taken into account.
This investigation identified clinical, injury, and demographic characteristics present at the time of hospitalization that could be targeted for systematic screening and intervention procedures. Our interdisciplinary team has conducted a series of investigations moving from initial descriptive studies to screening and intervention in acute care medical settings; results are mandates for alcohol screening and intervention by the American College of Surgeons and clinical practice guidelines for PTSD. Recent progress has been made on automated screening and intervention procedures for PTSD and alcohol that use information contained within the electronic medical record to identify high risk patients (Russo, Katon, & Zatzick, 2013). With this initial attempt at identifying correlates of suicidal ideation in hospitalized trauma patients, we believe a risk predictor model that included (1) history of mental health treatment, (2) history of mental health concerns, (3) age, (4) assault during traumatic injury, and (5) having children may help in identifying patients at elevated risk of suicidal ideation during hospitalization and longitudinally. These are all typically available in electronic medical records and would not require additional manpower required in universal screening efforts. Once identified, those at-risk can be approached by a care provider to gather more specific information regarding current depression, posttraumatic stress, previous self-directed violence, current or past suicidal thoughts, on-going legal proceedings, and current pain rating. We believe this measured approach addresses the desire to provide evidence-based trauma-centered care that is acceptable, realistic, and sustainable for patients, providers and the acute inpatient hospital setting. Ultimately, such an approach would assist in improved identification and treatment of suicidal patients in inpatient medical settings.
The current study had limitations. The sample is derived of patients enrolled in a randomized controlled trial, rather than a prospective cohort study. We included treatment condition in our longitudinal models to control for intervention effects that may confound our analysis; treatment group status was not significantly associated with suicidal ideation longitudinally. Our results are limited to patients who have elevated posttraumatic stress one month following their traumatic injury. This is a rigorous evaluation process to ensure high-risk patients are enrolled in a clinical trial, but is not generalizable to all patients hospitalized following a traumatic injury. However, we believe our sample does reflect a group at markedly high risk for suicidal ideation among the larger population of hospitalized trauma patients, given the presence of elevated posttraumatic stress symptoms during both the baseline and 1-month assessments. Our assessment of suicidal ideation is limited to the single PHQ-9 item, but is consistent with other “real world” general medical setting reports in this evolving area of suicide prevention research (Bauer, et al., 2012). Additionally, item 9 on the PHQ-9 asks about thoughts of hurting oneself or being better off dead. It is possible that some participants endorsing this item were referring to thoughts of non-suicidal self-injury, which limits our ability to more specifically classify this item as reflecting a desire to die.
Traumatic injuries are by nature unpredictable and unsettling with research demonstrating elevated rates of PTSD, depression, and suicide in injured trauma patients compared to the general population. As the National Institutes of Health attempts to meaningfully reduce the overall rate of suicide and suicide attempts, it may be helpful to target at-risk populations engaged in the medical system that may not otherwise receive mental health services, such as injured trauma patients, but may experience elevated rates of suicidal ideation compared to the general population. Brief screening and intervention models that combine elements of evidence-based suicide intervention with collaborative stepped care procedures may be a particularly useful method for improving patient functioning and reducing suicide risk following discharge from an inpatient acute medical setting (O'Connor et al., 2013; Zatzick, et al., 2013).
Acknowledgements
The current study was funded by grants R01/MH073613 and K24/MH086814 from the National Institute of Mental Health and T32/HS013835 from the National Institute of Child Health and Human Services.
Contributor Information
Stephen S. O’Connor, Department of Psychology, Western Kentucky University, Bowling Green, KY, USA
Kyl Dinsio, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Jin Wang, Department of Surgery, University of Washington, Seattle, WA, USA.
Joan Russo, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Frederick P. Rivara, Department of Pediatrics, University of Washington, Seattle, WA, USA.
Jeff Love, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Collin McFadden, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Leiszle Lapping-Carr, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Roselyn Peterson, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
Douglas F. Zatzick, Department of Psychiatry & Behavioral Sciences, University of Washington, Seattle, WA, USA
References
- Almeida OP, Pirkis J, Kerse N, Sim M, Flicker L, Snowdon J, Pfaff JJ. A randomized trial to reduce the prevalence of depression and self-harm behavior in older primary care patients. Annals of Family Medicine. 2012;10(4):347–356. doi: 10.1370/afm.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, American Psychiatric Press; 2000. [Google Scholar]
- Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, Parsons R. Suicide within 12 months of contact with mental health services: national clinical survey. British Medical Journal. 1999;318(7193):1235–1239. doi: 10.1136/bmj.318.7193.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer AM, Chan YF, Huang H, Vannoy S, Unutzer J. Characteristics, Management, and Depression Outcomes of Primary Care Patients Who Endorse Thoughts of Death or Suicide on the PHQ-9. Journal of General Internal Medicine. 2012 doi: 10.1007/s11606-012-2194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology. 2008;76(2):272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- Bonnie RJ, Fulco CE, Liverman CT, editors. Reducing the burden of injury: Advancing prevention and treatment. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- Botega NJ, de Azevedo RC, Mauro ML, Mitsuushi GN, Fanger PC, Lima DD, da Silva VF. Factors associated with suicide ideation among medically and surgically hospitalized patients. General Hospital Psychiatry. 2010;32(4):369–400. doi: 10.1016/j.genhosppsych.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Bruffaerts R, Demyttenaere K, Hwang I, Chiu WT, Sampson N, Kessler RC, Nock MK. Treatment of suicidal people around the world. British Journal of Psychiatry. 2011;199(1):64–70. doi: 10.1192/bjp.bp.110.084129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Clemans TA. Repetitive Traumatic Brain Injury, Psychological Symptoms, and Suicide Risk in a Clinical Sample of Deployed Military Personnel. Journal of the American Medical Association Psychiatry. 2013:1–6. doi: 10.1001/jamapsychiatry.2013.1093. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Trauma Centers Fact Sheet 2009. Atlanta: 2009. [Google Scholar]
- Civil ID, Schwab CW. In: The Abbreviated Injury Scale: 1985 revision. Scaling CoI., editor. Morton Grove: Committee on Injury Scaling, American Association for the Advancement of Automotive Medicine; 1985. [Google Scholar]
- Clark DC, Fawcett J. The relation of parenthood to suicide. Archives of General Psychiatry. 1994;51(2):160. doi: 10.1001/archpsyc.1994.03950020084009. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Bigelow GE, Brigham GS, Carroll KM, Cohen AJ, Gardin JG, Wells EA. Primary outcome indices in illicit drug dependence treatment research: systematic approach to selection and measurement of drug use end-points in clinical trials. Addiction. 2011 doi: 10.1111/j.1360-0443.2011.03473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eynan R, Langley J, Tolomiczenko G, Rhodes AE, Links P, Wasylenki D, Goering P. The association between homelessness and suicidal ideation and behaviors: results of a cross-sectional survey. Suicide and Life-Threatening Behavior. 2002;32(4):418–427. doi: 10.1521/suli.32.4.418.22341. [DOI] [PubMed] [Google Scholar]
- Ferrada-Noli M, Asberg M, Ormstad K, Lundin T, Sundbom E. Suicidal behavior after severe trauma. Part 1: PTSD diagnoses, psychiatric comorbidity, and assessments of suicidal behavior. Journal of Traumatic Stress. 1998;11(1):103–112. doi: 10.1023/A:1024461216994. [DOI] [PubMed] [Google Scholar]
- Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, Thanh HT. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bulletin of the World Health Organization. 2008;86(9):703–709. doi: 10.2471/BLT.07.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldney RD, Fisher LJ, Wilson DH, Cheok F. Major depression and its associated morbidity and quality of life in a random, representative Australian community sample. Australian and New Zealand Journal of Psychiatry. 2000;34(6):1022–1029. doi: 10.1080/000486700279. [DOI] [PubMed] [Google Scholar]
- Grossman DC, Soderberg R, Rivara FP. Prior injury and motor vehicle crash as risk factors for youth suicide. Epidemiology. 1993;4(2):115–119. doi: 10.1097/00001648-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: Wiley; 2000. [Google Scholar]
- Isometsa ET, Lonnqvist JK. Suicide attempts preceding completed suicide. British Journal of Psychiatry. 1998;173:531–535. doi: 10.1192/bjp.173.6.531. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Vannoy S, Imel Z, Cook JW, Fontana A, Rosenheck R, McFall M. Does PTSD moderate the relationship between social support and suicide risk in Iraq and Afghanistan War Veterans seeking mental health treatment? Depression and Anxiety. 2010;27(11):1001–1005. doi: 10.1002/da.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kishi Y, Robinson RG, Kosier JT. Suicidal ideation among patients during the rehabilitation period after life-threatening physical illness. Journal of Nervous and Mental Disease. 2001a;189(9):623–628. doi: 10.1097/00005053-200109000-00009. [DOI] [PubMed] [Google Scholar]
- Kishi Y, Robinson RG, Kosier JT. Suicidal ideation among patients with acute life-threatening physical illness: patients with stroke, traumatic brain injury, myocardial infarction, and spinal cord injury. Psychosomatics. 2001b;42(5):382–390. doi: 10.1176/appi.psy.42.5.382. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Logan J, Hall J, Karch D. Suicide categories by patterns of known risk factors. Archives of General Psychiatry. 2011;68(9):935–941. doi: 10.1001/archgenpsychiatry.2011.85. [DOI] [PubMed] [Google Scholar]
- Mackenzie EJ, Rivara F, Jurkovich G, Nathens AB, Frey KP, Egleston BL, Scharfstein DO. The national study on costs and outcomes of trauma. Journal of Trauma. 2007;63(6 Suppl):S54–S67. doi: 10.1097/TA.0b013e31815acb09. [DOI] [PubMed] [Google Scholar]
- Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services. 2001;52(6):828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, Williams DR. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. Public Library of Science Medicine. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. Journal of Abnormal Psychology. 2006;115(3):616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- O'Connor SS, Zatzick DF, Comtois KA, Ziemba L, Peterson R, McFadden C, Simpson S. Pilot study of a brief intervention delivered to patients admitted to acute care medical/surgical floor following a suicide attempt; Paper presented at the American Association of Suicidology; Austin, TX. 2013. [Google Scholar]
- Ramchand R, Marshall GN, Schell TL, Jaycox LH, Hambarsoomians K, Shetty V, Belzberg H. Alcohol abuse and illegal drug use among Los Angeles County trauma patients: Prevalence and evaluation of single item screener. Journal of Trauma. 2009;66(5):1461–1467. doi: 10.1097/TA.0b013e318184821d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist-Civilian Version. Journal of Traumatic Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Russo J, Katon W, Zatzick CD. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. General Hospital Psychiatry. 2013 doi: 10.1016/j.genhosppsych.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryb GE, Soderstrom CA, Kufera JA, Dischinger P. Longitudinal study of suicide after traumatic injury. Journal of Trauma. 2006;61(4):799–804. doi: 10.1097/01.ta.0000196763.14289.4e. [DOI] [PubMed] [Google Scholar]
- Saitz R. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug and Alcohol Review. 2010;29(6):631–640. doi: 10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uebelacker LA, German NM, Gaudiano BA, Miller IW. Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. Primary Care Companion for CNS Disorders. 2011;13(1) doi: 10.4088/PCC.10m01027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden K, Conwell Y. Suicides in late life. Current Psychiatry Reports. 2011;13(3):234–241. doi: 10.1007/s11920-011-0193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden K, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Zambon F, Laflamme L, Spolaore P, Visentin C, Hasselberg M. Youth suicide: An insight into previous hospitalization fro injury and sociodemographic conditions from a nationwide cohort survey. Injury Prevention. 2011;17:176–181. doi: 10.1136/ip.2010.030080. [DOI] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Katon W. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery. 2013;257(3):390–399. doi: 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Rivara F, Jurkovich G, Russo J, Trusz SG, Wang J, Katon W. Enhancing the population impact of collaborative care interventions: mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. General Hospital Psychiatry. 2011;33(2):123–134. doi: 10.1016/j.genhosppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan MY, Mackenzie EJ. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine. 2007;37(10):1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]