Abstract
Background
To determine relative fixation strengths of a single lateral locking plate, a double construct of a locking plate, and a tibial nail used in treatment of proximal tibial extra-articular fractures.
Methods
Three groups of composite tibial synthetic bones consisting of 5 specimens per group were included: lateral plating (LP) using a locking compression plate-proximal lateral tibia (LCP-PLT), double plating (DP) using a LCP-PLT and a locking compression plate-medial proximal tibia, and intramedullary nailing (IN) using an expert tibial nail. To simulate a comminuted fracture model, a gap osteotomy measuring 1 cm was created 8 cm below the knee joint. For each tibia, a minimal preload of 100 N was applied before loading to failure. A vertical load was applied at 25 mm/min until tibial failure.
Results
Under axial loading, fixation strength of DP (14,387.3 N; standard deviation [SD], 1,852.1) was 17.5% greater than that of LP (12,249.3 N; SD, 1,371.6), and 60% less than that of IN (22,879.6 N; SD, 1,578.8; p < 0.001, Kruskal-Wallis test). For ultimate displacement under axial loading, similar results were observed for LP (5.74 mm; SD, 1.01) and DP (4.45 mm; SD, 0.96), with a larger displacement for IN (5.84 mm; SD, 0.99). The median stiffness values were 2,308.7 N/mm (range, 2,147.5 to 2,521.4 N/mm; SD, 165.42) for the LP group, 4,128.2 N/mm (range, 3,028.1 to 4,831.0 N/mm; SD, 832.88) for the DP group, and 5,517.5 N/mm (range, 3,933.1 to 7,078.2 N/mm; SD, 1,296.19) for the IN group.
Conclusions
During biomechanical testing of a simulated comminuted proximal tibial fracture model, the DP proved to be stronger than the LP in terms of ultimate strength. IN proved to be the strongest; however, for minimally invasive osteosynthesis, which may be technically difficult to perform using a nail, the performance of the DP construct may lend credence to the additional use of a medial locking plate.
Keywords: Proximal tibial fracture, Locking plate, Nail, Biomechanical study
Proximal metaphyseal tibial fractures often occur as a result of high-energy injuries; treatment of such fractures remains a significant clinical challenge and is fraught with potential complications.1,2) Excellent clinical results have been achieved with the use of intramedullary nails, which are the treatment of choice for unstable tibial fractures.2) However, in 58% to 84% of cases, their use has been associated with malalignment and is more likely to result in loss of proximal fragment fixation due to deforming forces created by the extensor mechanism around the knee coupled with significant comminution.3,4) The popularity of nailing for treatment of this type of fracture has increased significantly due to recent design changes to intramedullary nails and adjunctive fixation techniques.2)
Along with the development of minimally invasive plate osteosynthesis, the popularity of locked plating for treatment of these complex fractures has increased significantly because there is no need for large incisions or there is no fear of soft tissue stripping, which lead to subsequent failure due to infection and nonunion. As a load sparing device, a locked plate is inferior to nailing in its ability to tolerate axial load;5) however, it is superior to conventional plating. In addition, loss of alignment during healing after lateral locked plating for treatment of this type of injury has been reported.1,6)
Despite the fact that both nailing and locked plating are the primary methods employed in minimally invasive techniques, only few studies reporting on their biomechanical performance can be found in the literature. According to our hypothesis, significant differences can be observed in the degree of stabilization provided by the different constructs used for treatment of comminuted fracture of the proximal tibia. The aim of this study was to compare fixation strengths and failure strengths of a single lateral locking plate, double locking plates, and an intramedullary (IM) nail in a comminuted fracture model of the proximal tibia.
METHODS
Eighteen synthetic adult-sized left tibial models (Model 3402, Pacific Research Laboratories Inc., Vashon, WA, USA) were employed for mechanical testing. Each model was made of a rigid foam cortical shell, which contained cancellous material in both its distal and proximal ends. Tibiae measured 40.5 cm in length with an IM canal diameter of 10 mm. The use of synthetic tibiae minimized variability between specimens and ensured consistency in specimen size.
Instrumentation
Three types of implants (locking compression plate-proximal lateral tibia [LCP-PLT, Synthes, Oberdorf, Switzerland], locking compression plate-medial proximal tibia [LCP-MPT, Synthes], and expert tibial nail [ETN, Synthes]) were used in the study. LCP-MPT was used only as an additional plate for the double plating (DP) constructs. For the purpose of comparison, implants of a similar length were chosen: LCP-PLT, 11 holes (260 mm); ETN, 315 mm with a diameter of 10 mm. An LCP-MPT with 8 holes (178 mm) was chosen.
Lateral plating
Six locking screws (diameter 5.0 mm) ranging in length from 46 mm to 75 mm were used for proximal condylar fixation of LCP-PLT. Distal fixation was achieved in screw holes 5, 7, 9, and 11 (1 being the most proximal and 11 being the most distal) by using 28 mm to 30 mm bicortical screws.
Double plating
Following lateral plating (LP), additional fixation of the LCP-MPT was performed on the medial side of the synthetic bone. Three locking screws (diameter 5.0 mm) ranging in length from 30 mm to 55 mm were used for proximal segment fixation. Distal fixation was achieved in screw holes 6, 7, and 8 (1 being the most proximal and 8 being the most distal) by using 28 mm to 30 mm bicortical screws.
Intramedullary nailing
Proximal fixation of the expert tibial nail (315 mm in length, 10 mm in diameter) was achieved by using a cancellous bone locking screw measuring 70 mm in length and two 5.0-mm interlocking screws (36 mm and 46 mm long). Two 5.0-mm interlocking screws were used for distal nail fixation.
Finally, radiological examination of all the tibiae was performed in order to confirm success of the final implantation.
Set-up
A fracture model simulating a comminuted fracture of the proximal tibia was developed for biomechanical testing. A gap osteotomy measuring 1 cm was created 8 cm below the knee joint, perpendicular to the axis of the tibial shaft (Fig. 1). Osteotomies were created after the application of implants to bone. The proximal and distal ends of the tibiae were then potted in custom made boxes and a metal alloy was used for fixation. To simulate anatomic positioning, each potted tibia was placed in a servo-hydraulic testing machine (MTS Bionix 793 axial compression testing machine; MTS Systems, Eden Prairie, MN, USA) and held at 90 degrees to the ground using custom fixation devices. In order to hold the construct securely, each tibia was potted distally in a reinforced Fiberglass Resin (Bondo, Atlanta, GA, USA) and proximally in a lead-bismuth alloy. The use of the mold allowed for even distribution of the axial force applied during testing (Fig. 1).
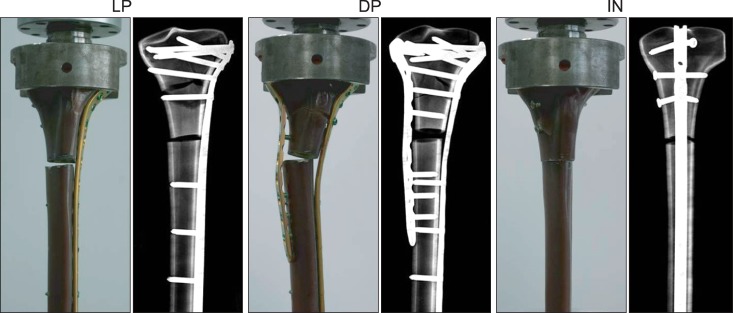
Fig. 1.

Three types of instruments were used in the proximal tibia fracture models with a gap osteotomy measuring 1 cm (LP, DP, and IN from the left). Typical experimental set-ups for mechanical testing are also shown alongside the radiographic constructs. LP: lateral plating, DP: double plating, IN: intramedullary nailing.
Test
One of the six constructs of each of the three types of instrumentation was used for cyclic load testing and the other five constructs were used for load to failure testing. In order to stabilize the construct, an axial preload of 100 N was applied proximally and an axial compressive load of 1,000 N was then applied at a rate of 10 mm/min. By using an MTS crosshead motion sensor, axial displacements from the initial position to preload and from preload to maximum load were recorded continuously. The constructs were then subjected to axial cyclic loading from 100 N to 1,000 N for 10,000 cycles at 3 Hz.
Loading was continued until failure of the bone-implant construct occurred, as demonstrated by a marked decrease in the load versus displacement curve. Failure was defined as complete medial or lateral collapse or hardware bending or fracture. Maximum compressive load before failure was recorded for all of the specimens. Construct stiffness was measured at 5,000 N load, because all of the specimens withstood this load.
Data showed normal distribution, as indicated by the parametric statistical methods. The three instrumentation groups were compared. Both ultimate displacement and load to failure data were analyzed using the Kruskal-Wallis test.
RESULTS
The results demonstrated that all of the specimens withstood cyclic loading up to 1,000 N for 10,000 cycles. Gross failure of constructs was not observed during cyclic testing.
Mode of Failure
Cracks were observed at the bone-proximal locking screw interface (nearest to the gap) in four of the five LP constructs, and one LP construct showed plate bending at the osteotomy gap. Cracks were observed at the bone-proximal locking screw interface (nearest to the gap) in all of the five DP constructs; four of the five DP constructs showed bending of plates at the osteotomy gap. All of the intramedullary nailing (IN) constructs demonstrated bending of interlocking screws at the proximal and distal segments; however, failure at the bone-metal interface or bending of nail was not observed (Fig. 2).
Fig. 2.
Failures after axial load testing for all constructs and resulting radiographs. Development of bone cracks at the bone-proximal locking screw interface was observed in four of the five LP constructs. Bone cracks were observed at the bone-proximal locking screw interface in all five DP constructs, and four of them showed bending of plates at the osteotomy gap. Failure at interlocking screws, without bending of the nail was observed in all IN constructs. LP: lateral plating, DP: double plating, IN: intramedullary nailing.
Load to Failure
Results for ultimate displacement under axial loading were similar in the LP (5.74 mm; standard deviation [SD], 1.01), DP (4.45 mm; SD, 0.96), and IN groups (5.84 mm; SD, 0.99; p = 0.35, Kruskal-Wallis test). Compared to the LP construct (12,249.3 N; range, 10,959.6 to 13,877.5 N), the average load to failure for the DP construct (14,387.3 N; range, 13,273.8 to 17,157.3 N) was 17.5% greater under axial loading, and 60% less when compared with that of the IN construct (22,879.6 N; range, 20,692.1 to 24,337.4 N; p < 0.001, Kruskal-Wallis test) (Fig. 3). Data on ultimate displacement and load to failure are shown in Table 1.
Fig. 3.
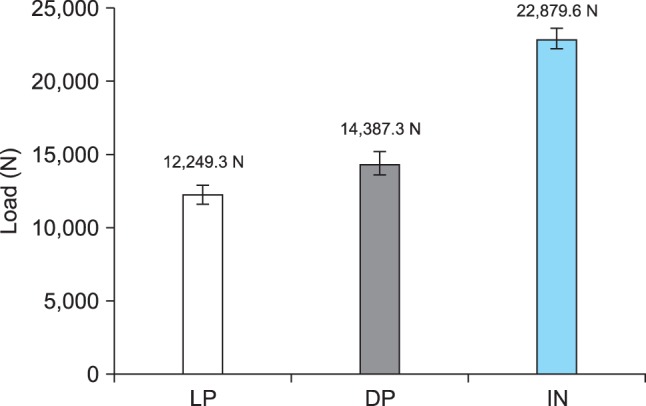
Comparison of axial load to failure for all construct groups. The intramedullary nailing (IN) was found to be the strongest construct. In terms of axial loading, the average load to failure of the double plating (DP) construct was 17.5% greater than that of the lateral plating (LP) construct (p < 0.001).
Table 1.
Displacement and Maximum Load to Failure Data of Specimens Fitted with LP, DP, and IN Constructs
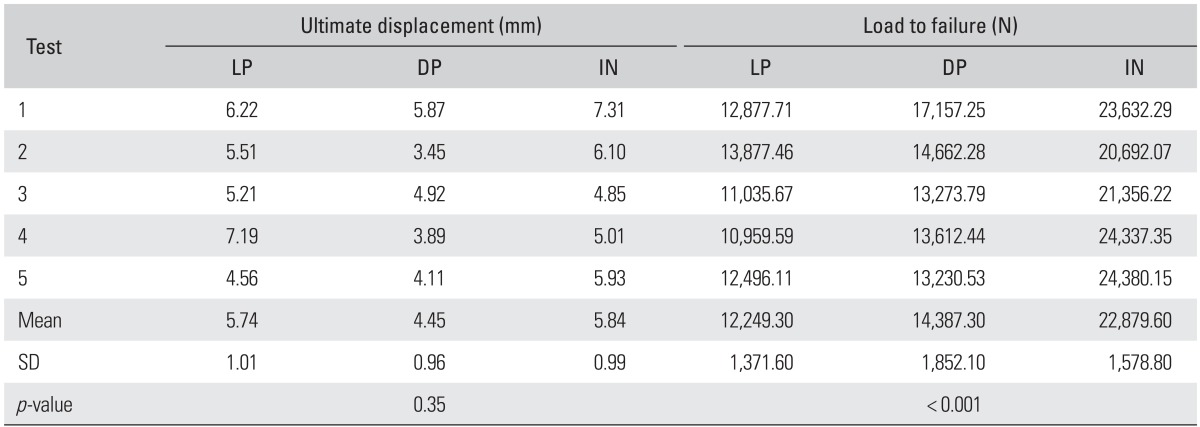
Statistical analysis was performed by the Kruskal-Wallis test.
LP: lateral plating, DP: double plating, IN: intramedullary nailing, SD: standard deviation.
Stiffness
The median stiffness values were 2,308.7 N/mm (range, 2,147.5 to 2,521.4 N/mm; SD, 165.42) for the LP group, 4,128.2 N/mm (range, 3,028.1 to 4,831.0 N/mm; SD, 832.88) for the DP group, and 5,517.5 N/mm (range, 3,933.1 to 7,078.2 N/mm; SD, 1,296.19) for the IN group.
DISCUSSION
Treatment of extra-articular proximal tibial fractures is challenging, and it is associated with higher rates of complications when compared with treatment of diaphyseal tibial fractures.1) Most of these fractures result from high energy, direct trauma that causes extensive injury to the soft tissue and bone; therefore, it is desirable to limit the extent of direct open exposure. A high incidence of wound breakdown, infection, and fixation failure has been observed in association with conventional plating of the proximal tibia. To prevent these complications, irrespective of whether an IM nail or a locking plate is used, employment of minimally invasive techniques has been advocated. However, only few studies comparing the biomechanical properties of the IM nail versus the locking plate for treatment of a comminuted fracture of the proximal tibia have been published.
With respect to the concepts of minimally invasive surgery and enhanced fracture healing, IM nail is an ideal load sharing implant, and its bending stiffness is superior to that of the locking plate.7) In addition, after recent improvements in oblique interlocking screws used in treatment of fractures of the proximal metaphysis,2,8) stability of modern tibial nails is greater than that of old nails with two transverse interlocking screws. In accordance with this concept, we used the nail with three locking screws in the current study. The IN construct was found to be significantly stiffer than the DP or LP constructs of locking plates; therefore, from the biomechanical viewpoint, IN may be the ideal option for treating extra-articular proximal tibial fractures. However, for nailing, fractures with a short proximal end segment present a challenge, and a higher incidence of malreduction resulting in nonunion has been reported, compared with locked plating.5) In the current study, the implant was fixed prior to creation of the osteotomy simulating the fracture; therefore, the issue of malalignment related to primary reduction was not addressed. However, this study was purely a laboratory investigation performed in the absence of soft tissues surrounding the bone, which may not be observed frequently in clinical practice. Therefore, from the clinical point of view, malreduction after IN should not be overlooked, although several technical tips may help to reduce the occurrence of this complication in patients with proximal tibial fractures.3,9,10)
Early motion and weight-bearing are helpful for rehabilitation; therefore, maintaining the reduction of proximal tibial fractures is important. Loss of initial reduction with IN is observed significantly less often nowadays, and its incidence has been reported to be 0% in several studies.4,9) However, due to its lesser ability to tolerate axial load, loss of reduction after LP is not uncommon during the healing period.6,11,12,13) Many surgeons prefer to delay weight-bearing for a few months in patients treated with LP. In the DP construct used in this study, we added the medial locked plate, which appeared to be stiffer than the conventional plate used in another study. Use of the additional medial plate resulted in significantly enhanced stability of DP by approximately 17.5%; therefore, the DP construct with a locked plate may be ideal for use in treatment of fractures of the proximal tibia that need plating.
During treatment of bicondylar fractures of the proximal tibia, no differences were observed in the stiffness of the dual plating construct when compared to that of the lateral fixed angle plate.14,15) However, in this study that used the extra-articular model, the DP construct showed significantly greater stiffness when compared that in the study by LP. Peindl et al.,16) which reported a similar result of greater stiffness of DP when compared to that of the lateral single plate or external fixator constructs, even with relatively short plates. DP was found to be the least soft tissue-friendly method when used during an open approach; therefore, they concluded that it was not advisable to use DP in clinical situations. However, minimally invasive plate osteosynthesis (MIPO) on the medial side is also gaining in popularity,17) and from both the biomechanical and biological viewpoints, we assume that DP with a minimally invasive technique can be successful.
Although there are multiple loading forces on the knee joint, including bending, torsional, axial, and shear load, only axial loads were applied in the current study, which is a limitation of this study. However, axial load is the most important and it causes fixation failure in a clinical situation,18) since main forces during gait are applied in the axial direction.19)
Another limitation of this study is that the human cadaveric bone, an ideal test material, was not used. The synthetic bone does not have soft tissue attachment of tendons or muscles, which are known to be cause malreduction. However, synthetic tibiae offer several advantages over cadaveric tibiae. Composite tibiae provide standard dimensions and properties of specimens; thus, the implantation techniques were reproducible and implants of the same size were used.20) The modulus of elasticity of composite bones is similar to that of native bones. In addition, there were no variations in the dimensions, age, and bone density of cadaveric specimens.
In summary, the IM nail was found to be the most stable implant for use in treatment of comminuted extra-articular fractures of the proximal tibia. However, when it is difficult to achieve satisfactory reduction by nailing, dual locked plates may be a stronger implant for use in MIPO when compared to lateral locked plating, which is currently being used.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007;21(2):83–91. doi: 10.1097/BOT.0b013e318030df96. [DOI] [PubMed] [Google Scholar]
- 2.Hansen M, Blum J, Mehler D, Hessmann MH, Rommens PM. Double or triple interlocking when nailing proximal tibial fractures? A biomechanical investigation. Arch Orthop Trauma Surg. 2009;129(12):1715–1719. doi: 10.1007/s00402-009-0954-1. [DOI] [PubMed] [Google Scholar]
- 3.Nork SE, Barei DP, Schildhauer TA, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma. 2006;20(8):523–528. doi: 10.1097/01.bot.0000244993.60374.d6. [DOI] [PubMed] [Google Scholar]
- 4.Ricci WM, O'Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001;15(4):264–270. doi: 10.1097/00005131-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009;23(7):485–492. doi: 10.1097/BOT.0b013e3181b013d2. [DOI] [PubMed] [Google Scholar]
- 6.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005;439:207–214. doi: 10.1097/00003086-200510000-00036. [DOI] [PubMed] [Google Scholar]
- 7.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84(8):1093–1110. doi: 10.1302/0301-620x.84b8.13752. [DOI] [PubMed] [Google Scholar]
- 8.Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM. Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma. 2003;17(7):496–502. doi: 10.1097/00005131-200308000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Krettek C, Miclau T, Schandelmaier P, Stephan C, Mohlmann U, Tscherne H. The mechanical effect of blocking screws ("Poller screws") in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma. 1999;13(8):550–553. doi: 10.1097/00005131-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Matthews DE, McGuire R, Freeland AE. Anterior unicortical buttress plating in conjunction with an unreamed interlocking intramedullary nail for treatment of very proximal tibial diaphyseal fractures. Orthopedics. 1997;20(7):647–648. doi: 10.3928/0147-7447-19970701-14. [DOI] [PubMed] [Google Scholar]
- 11.Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res. 2006;445:222–229. doi: 10.1097/01.blo.0000203467.58431.a0. [DOI] [PubMed] [Google Scholar]
- 12.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–535. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007;21(5):301–306. doi: 10.1097/BOT.0b013e3180500359. [DOI] [PubMed] [Google Scholar]
- 14.Mueller CA, Eingartner C, Schreitmueller E, et al. Primary stability of various forms of osteosynthesis in the treatment of fractures of the proximal tibia. J Bone Joint Surg Br. 2005;87(3):426–432. doi: 10.1302/0301-620x.87b3.14353. [DOI] [PubMed] [Google Scholar]
- 15.Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma. 1999;13(8):545–549. doi: 10.1097/00005131-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Peindl RD, Zura RD, Vincent A, Coley ER, Bosse MJ, Sims SH. Unstable proximal extraarticular tibia fractures: a biomechanical evaluation of four methods of fixation. J Orthop Trauma. 2004;18(8):540–545. doi: 10.1097/00005131-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Oh CW, Oh JK, Kyung HS, et al. Double plating of unstable proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. Acta Orthop. 2006;77(3):524–530. doi: 10.1080/17453670610012548. [DOI] [PubMed] [Google Scholar]
- 18.Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003;(412):189–195. doi: 10.1097/01.blo.0000071754.41516.e9. [DOI] [PubMed] [Google Scholar]
- 19.D'Lima DD, Patil S, Steklov N, Slamin JE, Colwell CW., Jr Tibial forces measured in vivo after total knee arthroplasty. J Arthroplasty. 2006;21(2):255–262. doi: 10.1016/j.arth.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Zdero R, Rose S, Schemitsch EH, Papini M. Cortical screw pullout strength and effective shear stress in synthetic third generation composite femurs. J Biomech Eng. 2007;129(2):289–293. doi: 10.1115/1.2540926. [DOI] [PubMed] [Google Scholar]


