Abstract
Context
In 2012, the National Action Alliance for Suicide Prevention (Action Alliance)'s Research Prioritization Task Force (RPTF) released a series of Aspirational Goals (AGs) to decrease suicide deaths and attempts. The RPTF asked experts to summarize what was known about particular AGs, and to propose research pathways that would help reach them. This manuscript describes what is known about the benefits of access to health care (AG8) and continuity of care (AG9) for individuals at risk for suicide. Research pathways are proposed to address limitations in current knowledge, particularly in U.S. healthcare-based research.
Evidence acquisition
Using a three-step process, the expert panel reviewed available literature from electronic databases. For two AGs, the experts summarized the current state of knowledge, determined breakthroughs needed to advance the field, and developed a series of research pathways to achieve prevention goals.
Evidence synthesis
Several components of healthcare provision have been found to be associated with reduced suicide ideation, and in some cases mitigated suicide deaths. Randomized trials are needed to provide more definitive evidence. Breakthroughs that support more comprehensive patient data collection (e.g., real-time surveillance, death record linkage, patient registries) would facilitate the steps needed to establish research infrastructure so that various interventions could be tested efficiently within various systems of care. Short-term research should examine strategies within the current healthcare systems, and long-term research should investigate models that redesign the health system to prioritize suicide prevention.
Conclusions
Evidence exists to support optimism regarding future suicide prevention, but knowledge is limited. Future research is needed on U.S. healthcare services and system enhancements to determine which of these approaches can provide empirical evidence for reducing suicide.
Introduction
Suicide is a major public health concern.1,2 Despite numerous prevention and intervention efforts, the overall rates of suicide in the U.S. have not decreased significantly over time.3,4 In fact, according to the CDC, adult suicide rates have actually risen by nearly 30% over the last decade.5 This is due, in part, to the limited evidence available to support informed and targeted strategies to reduce suicide. In 2012, the National Action Alliance for Suicide Prevention's (Action Alliance) Research Prioritization Task Force (RPTF) identified a series of Aspirational Goals (AGs), which, if achieved, might make a difference in mitigating suicide in the U.S.6 Following the establishment of these goals, the RPTF teamed with researchers who had expertise related to each of the goals. Experts were asked to review the state of knowledge for each AG, identify areas where breakthroughs were needed, and develop pathways to guide future research most likely to reduce suicide mortality and morbidity. This review discusses the expert panel findings for AGs 8 and 9 The first of these goals (AG8) is “to design new healthcare delivery strategies to ensure that affordable, accessible, effective care is available to all individuals at risk for suicidal behavior.” The second of these goals (AG9) is “for suicidal individuals, reduce treatment dropout at all stages of the care process by providing better continuity.”6 Because much of the current evidence overlaps for these goals, they have been combined in this review. The other manuscripts in this supplement address research pathways for the remainder of the AGs.
Evidence Acquisition
Using a three-step process, evidence was compiled from a comprehensive search of all available electronic databases for published literature on access to and engagement in health services for individuals at risk for suicide. First, the RPTF identified systematic reviews and other primary studies from all of the major electronic databases, including MEDLINE, the Cochrane Library, PsychINFO, and Google Scholar. All English-language studies using human subjects were evaluated by doctoral-level researchers. Second, the information obtained by the RPTF was shared with the topic area experts examining AG8 and AG9: Drs. Steven Vannoy and Jürgen Unützer, from the University of Washington. Drs. Vannoy and Unützer supplemented the information with their experience, and additional articles of importance to the field. They summarized the findings from both sets of reviews in presentation format for a panel of overview experts. Finally, in the third step, Dr. Brian Ahmedani, from Henry Ford Health System (HFHS), and Dr. Vannoy conducted a final investigation and examination of the literature. The three-step search process yielded evidence to support future research pathways for AG8 and AG9.
Suicide prevention efforts exist on several levels across the entire continuum of health care and can target the spectrum of suicide related behavior, including: (1) suicide deaths; (2) suicide attempts; and (3) suicide ideation (thoughts or plans). Intermediate outcomes, such as improved treatment adherence or a reduction in repeated crisis visits to emergency care should also be considered outcomes in research efforts, as these behaviors incur high levels of burden. Gordon's7 definitions of prevention have been applied to public health approaches for preventing mental disorders and can be applied to suicide prevention. Specifically, universal approaches are applied to all individuals in a population. In the healthcare system, this could translate to a universal screening effort. Selective approaches are for those with characteristics that are associated with increased risk, such as among individuals with behavioral health conditions. Indicated approaches focus on those with specific known risk, such as those individuals who exhibit suicide-related thoughts or have a history of attempting suicide. Suicide risk management can be considered skills needed to assess these levels of risk, and then to inform patients, provide treatment, coordinate care, and respond to crises for those who have been identified.8 Risk management activities can be distributed across settings and types of providers. The authors draw from research demonstrating the benefits of the chronic care management model as it has been applied to common mental disorders.9 This model involves patient engagement in care, delivering brief assessment and intervention, care coordination across the system, and tracking outcomes as components of quality improvement efforts.
Evidence Synthesis
There are significant challenges to determining which health services are, or are not, helping individuals to engage in care and receive the help they need. Few healthcare systems routinely link patient care history with suicide attempt or death outcomes, and ideation is not routinely assessed.10 Universal screening in primary care is likely to lead to many false positives,11,12 and few studies have shown how best to identify those at risk in general medicine settings and refer them to effective specialty care. The U.S. Preventive Services Task Force (USPSTF) currently does not recommend screening for suicide risk in primary care owing to the lack of evidence-based interventions.13 Moreover, individuals who need care do not always seek help for suicide-related concerns from healthcare providers for various reasons, some associated with the healthcare system (e.g. beliefs about ineffective care).14 In other cases, embarrassment or shame felt by the individuals or family members and friends who might help the at-risk individual may result in fewer opportunities for intervention when these beliefs are not adequately addressed by healthcare outreach efforts.15,16
Even if individuals access health care, the majority of those who die by suicide are likely to be seen in primary care settings where suicide risk is often under-detected and -treated.17–19 For example, the Mental Health Research Network recently found that most healthcare visits prior to suicide occur in primary care or general medical specialty settings, and half of all visits are not coded with mental health diagnoses.20 This is troubling for individuals at risk for suicide, as more than 90% meet criteria for mental health conditions in psychological autopsy studies.21 As discussed in this supplement and elsewhere, one concern is that general medical providers often lack the training and knowledge needed to identify and treat mental health and suicide risk, as well as limited time to discuss these issues with patients.22,23 Thus, the current healthcare system relies on the limited number of referrals that make it to specialty mental health care and emergency services, where the skill levels of providers may also be limited with regard to suicide risk management.
Access to specialty mental health and substance use care has been limited, and where available, it may be cost prohibitive.24 Thus, affordability has been a barrier to accessing needed care, particularly for individuals without health insurance. Recent healthcare legislation may improve these circumstances and in turn decrease suicide risk. For example, one study found that increased access to healthcare services attributed to the passage of state mental health parity laws was associated with a 5% reduction in the suicide death rate in those states.25 Parity laws mandate equal insurance coverage for mental health and general medical care on select health plans. The research pathways considered here are timely, as the federal Affordable Care Act, along with numerous other state and federal parity laws, have provisions that aim to extend mental health care insurance coverage, which could improve access and thereby potentially mitigate suicide risk.24
Several studies describing deliberate changes in health system models to enhance care of suicidal individuals or depression as a major risk factor have shown promise. Chronic disease care models have improved treatment access, adherence, and continuity for mental health conditions. Collaborative care, as one approach to chronic care management, has been applied to depression, resulting in reduced frequency and intensity of suicidal ideation.26,27 Similarly, mandated coordinated care in the United Kingdom (UK) resulted in a decrease in suicide attempts.28 While and colleagues29 also found that a series of large healthcare system enhancements in the UK were associated with a reduction in suicide deaths. Alternative treatments, such as telephone and web-based interventions, are effective for mental health conditions.30,31 These alternative treatments may improve continuity of care in mental health services and subsequently enhance suicide prevention. However, the U.S. healthcare model is vastly different than that of the UK, as it relies upon reimbursement from multiple sources (e.g., government, private payers, and individuals). Thus, implementation of these prevention models requires advancements in methods of billing and reimbursement. There may be opportunities to reform reimbursement methods as part of the Affordable Care Act. Although each of these interventions appears suited for suicide prevention in the U.S., evidence of their potential impact remains limited.
Interventions that target suicide behavior directly are considered by many to be essential in selective suicide prevention efforts, with current studies focused on individuals who have either presented to emergency or specialty care, as discussed in this supplement.32 As noted by the recent USPSTF report,13 few studies have tested interventions for suicide mitigation in primary care beyond collaborative depression care for older adults. Two European randomized trials33,34 promoting continuity of care in health systems did not find evidence for reduction of suicidal behavior. Furthermore, very limited data are available on suicide-related outcomes from treatment adherence interventions, which have shown effectiveness for individuals with depression.35 Suicide crisis phone lines, such as the National Suicide Prevention Lifeline, are showing promise for reducing distress and linking callers to services.36,37 The Lifeline was recently established in response to prior National Suicide Goals to enhance access and community outreach.38 The means restriction method of suicide prevention, including removing access to firearms and other lethal items, has shown promise in previous research.39–41 However, expanding means restriction may require public health changes.42 This is discussed in more detail elsewhere in this supplement.
Currently funded research on suicide approaches within care systems is underway to examine several questions. For example, the Department of Defense (DoD) has funded a Military Suicide Research Consortium to examine multiple assessment and intervention models for service members and veterans (msrc.fsu.edu/). The Mental Health Research Network has begun a feasibility study of two population-based health system interventions to reduce suicide attempts (NIH #UH2AT007755). A potential second phase could include a large pragmatic trial across multiple health systems.
Although some evidence exists to support optimism regarding suicide prevention in the future, numerous gaps remain in our knowledge. Breakthroughs are needed in a number of areas in order to enhance suicide prevention (Table 1). First, suicide prevention must be prioritized across all levels of care, as evidenced in the Henry Ford Health System (HFHS) and U.S. Air Force Initiatives.43–45 The Perfect Depression Care (PDC) Initiative at HFHS shifted the behavioral health department's cultural focus towards the goal of eliminating suicides among all patients, included multi-level suicide risk assessment to inform care pathways, and offered numerous access points to care.44,45 The PDC initiative also has a component on means restriction, which encourages individuals and their families to remove access to firearms and other lethal means. The “Zero Suicides” goal from PDC has been adopted as a national standard by the Action Alliance.
Table 1.
Breakthroughs needed to enhance suicide prevention by improving health services access and engagement
| 1. Prioritization of suicide across all levels of care |
| 2. Effective identification and assessment strategies |
| 3. Comprehensive surveillance systems and outcome tracking |
| 4. Large registries linking risk across systems and providers |
| 5. Enhanced electronic medical records with real-time notification of risk |
| 6. Care coordination within and between providers, departments, and systems |
| 7. Effective interventions using existing and alternative approaches to care |
| 8. Informed care pathways |
| 9. Stepped care treatment approaches |
| 10. Treatment engagement |
To achieve a suicide prevention-prioritized health system, the first step is to develop improved surveillance systems that are capable of tracking patient suicidal behavior (i.e., ideation, attempts, and deaths). These systems can be modeled after the recently launched DoD Suicide Event Report (DODSER) surveillance system, which was created in response to a prior national suicide goal.38,46 This system tracks suicide-related behavior, including mortality, attempts, and ideation, across all divisions of the U.S. Armed Forces and links events to military, psychosocial, and treatment history for each person. In practice, the electronic medical record (EMR) can be leveraged to screen for suicide risk, and make information immediately available to providers. Once individuals are identified, large registries can link information across systems and care platforms. These systems can provide real-time notifications to healthcare providers regarding each individual's status within the EMR. Using this information, care systems can also investigate and learn from adverse events and be optimally informed to prevent future events through more effective identification and risk assessment strategies for acute risk, especially in primary care and general medical settings. Second, based on these surveillance efforts, leaders can make decisions as to where improved care is needed, implement changes, and again evaluate whether suicide risk is reduced through improved processes. Third, improved care coordination strategies within and between care disciplines can support system-wide improvements that may lead to synergistic benefits that would exceed any combination of individual care improvement components. These can leverage the EMR to share information. Most importantly, each of these processes must be designed practically, so that health systems and providers can easily incorporate them into their daily routines. As discussed elsewhere in this supplement, enhanced technologies, detailed training, and workforce development interventions need to be developed and tested to improve each of these processes.
Fully connected systems and providers need tools to provide effective treatment. Thus, additional strategies are needed to improve suicide interventions that are tested in care systems. This includes optimizing and refining suicide research methodology, which encompasses developing targeted RCTs with larger sample sizes and well-planned quasi-experimental and observational studies. RCTs using waitlist control designs are an optimal approach for large implementation studies in healthcare settings. Interventions should specifically focus on suicide risk and behavior. This includes identifying the best ways to increase the willingness of non-mental health specialists to engage in prevention and intervention. Interventions should also be tested within the daily routines of standard health care to ensure that, if successful, they can be efficiently implemented.
One feasible and practical approach for busy healthcare providers may be brief interventions. These can be developed to provide immediate assessment and treatment, improve access, and inform care pathways.47 The lack of empirically based risk stratification screening and assessment limits providers' abilities to match patient needs to care. Stepped care treatment models may offer a solution for indicated suicide risk, but should be tested in more rigorous ways. Finally, strategies should be developed to track and facilitate engagement in care once individuals have accessed the service system.
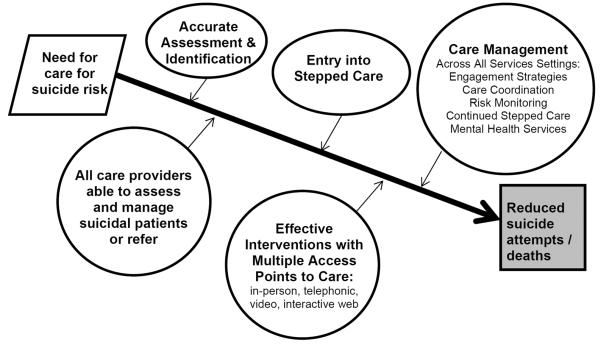
Figure 1 depicts a proposed research pathway based upon available evidence, which provides a hypothesis for how suicide prevention could be designed in a healthcare setting. Using this hypothesis-driven model, suicide prevention should begin the moment individuals make contact with the health system. Furthermore, all at-risk individuals should be accurately identified and assessed. All care providers should be able to assess and manage patients at a level appropriate to their healthcare role, and be able to successfully participate in coordinated care efforts with specialists and other care providers. Once identified, individuals should be entered into a stepped care treatment pathway. They may be offered numerous opportunities to access and engage in effective treatment, including standard in-person options as well as telephonic, interactive video, web-based, and smartphone interventions. Healthcare professionals should be encouraging and supportive of participation. Care management should be collaborative across all health service settings. In this proposed model, acute, primary, specialty, mental health, and chemical dependency care are all part of one united system with a common goal of preventing suicide. The focus of care management may be enhancing engagement, care coordination, risk monitoring, continued stepped care, and provision of mental health services. Combined, a comprehensive system using all of these efforts may help mitigate suicide risk by improving access to, and engagement in, healthcare services.
Figure 1.
Proposed research pathways for suicide prevention research on health services access and engagement
Although this utopian health system may exist in the future, there is not enough evidence available on the best approaches along each step in the process, how to implement and tailor the best protocols within the current healthcare delivery system, or ways to reinvent the healthcare system for optimal suicide prevention. In particular, evidence is lacking on specific ideas that are practical for health providers and are easy to implement within health systems, given increasing demands. This may be one of the largest barriers to successful suicide prevention in healthcare settings. Thus, practical dissemination and implementation approaches must also be studied. In order to achieve the goals set forth by the Action Alliance, innovative and well-designed projects need to be conducted within and across each area of the proposed research pathway. New projects need to use radical new ideas, designs, methods, and analyses that revolutionize the field, as the current models have not produced the intended reductions in suicide. There are several short- and long-term priorities that can facilitate learning over time.
Short-term research must first include epidemiologic and observational studies examining the best ways to identify those at risk and provide adequate monitoring approaches without taxing the system, particularly among those with universal risk in primary care and general medical settings who have not been diagnosed with a mental health condition. For individuals with risk factors (indicated prevention approaches), identification and assessment strategies could consider testing collaborative stepped care models. For those identified as being at risk (selective prevention), research investigating the effectiveness of existing interventions (or their pragmatic adaptations such as Screening, Brief Intervention, and Referral to Treatment for improving treatment engagement)48 targeting suicidal thoughts and behavior is needed. These studies should use strong research methodology, such as randomized trials or carefully planned quasi-experimental designs, while developing collaborative partnerships across systems to increase sample sizes. Researchers also can develop and test new and innovative ways to measure the effectiveness of suicide interventions. For example, researchers can harness the power of the EMR to capture longitudinal information on standardized mental health and suicide risk assessments and treatment utilization. Many systems have already incorporated mental health and suicide screening practices into their daily workflows.49,50
Long-term research can evaluate innovative techniques to redesign the healthcare system to provide treatment and follow-up in novel ways, with a particular focus on suicide prevention. New interventions should be pragmatic and include technology-based strategies that may be able to reach more individuals beyond standard care seekers. Care systems may also evaluate new health plan reimbursement models, which fit within recent healthcare legislations expanding coverage for more individuals. These models may follow the innovative approach developed and implemented in Minnesota for collaborative depression care reimbursement as part of the Depression Improvement Across Minnesota, Offering a New Direction (DIAMOND) initiative.51
In all research, but particularly in intervention studies, protocols must account for ethical and safety concerns.52,53 There should be a clear protocol to monitor and intervene regarding suicide risk for all participants (both treatment and control/comparison groups), including detailing specific steps based on varying levels of severity. Researchers should consider expanded monitoring of all participants for suicide risk and set clear guidelines for when individuals should be censored or referred for specialized care as well as rules for “stopping” any study.52 The consent process is also critical, specifically for intervention studies. It is essential to provide detailed information regarding the risks and benefits to participants, and to the parent/guardian for youth participants, while outlining the rules and regulations about confidentiality and duty to protect. In some circumstances, researchers should consult local laws regarding possible involvement of youth in studies in which it may be difficult to obtain parent/guardian consent to do history of abuse/neglect, drug use, or other circumstances.53
Conclusions
Overall, research implies that suicide is preventable, and at-risk individuals served by healthcare systems deserve care that is evidence-based. More research is needed on practical ways to identify and assess suicide risk and to test and implement effective interventions. Major progress has already been made by the Action Alliance through the declaration of the AGs. The research pathways presented here can help facilitate future suicide prevention and health services research.
Acknowledgments
Sources of funding: Fund for Henry Ford Hospital; NIH (U19MH092201; UH2AT007755)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Heron M. Deaths: leading causes for 2009. Natl Vit Stat Rep. 2012;61(7):1–94. [PubMed] [Google Scholar]
- 2.Rockett IR, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: U.S., 2000–2009. Am J Public Health. 2012;102(11):e84–92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crosby AE, Ortega L, Stevens MR. Suicides—U.S., 1999–2007. MMWR Surveill Summ. 2011;60(1S):S56–S59. [Google Scholar]
- 4.Holinger PC, Klemen EH. Violent deaths in the U.S., 1900–1975. Relationships between suicide, homicide and accidental deaths. Soc Sci Med. 1982;16(22):1929–38. doi: 10.1016/0277-9536(82)90392-6. [DOI] [PubMed] [Google Scholar]
- 5.CDC Suicide among adults aged 35–64 years—U.S., 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(17):321–5. [PMC free article] [PubMed] [Google Scholar]
- 6.USDHHS and National Action Alliance for Suicide Prevention . 2012 national strategy for suicide prevention: goals and objectives for action. USDHHS; Washington DC: 2012. [Google Scholar]
- 7.Mrazek PJ, Haggerty RJ. Reducing risks for mental disorders: frontiers for preventive intervention research. National Academy Press; Washington DC: 1994. [PubMed] [Google Scholar]
- 8.McDowell AK, Lineberry TW, Bostwick JM. Practical suicide-risk management for the busy primary care physician. Mayo Clin Proc. 2011;86(8):792–800. doi: 10.4065/mcp.2011.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Unutzer J, Schoenbaum M, Druss BG, Katon WJ. Transforming mental health care at the interface with general medicine: report for the presidents commission. Psychiatr Serv. 2006;57(1):37–47. doi: 10.1176/appi.ps.57.1.37. [DOI] [PubMed] [Google Scholar]
- 10.Ahmedani BK, Coffey MJ, Coffey CE. Collecting mortality data to drive real-time improvement in suicide prevention. Am J Manag Care. 2013;19(11):e386–90. [PubMed] [Google Scholar]
- 11.Simon GE, VonKorff M. Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol. 1998;147(2):155–60. doi: 10.1093/oxfordjournals.aje.a009428. [DOI] [PubMed] [Google Scholar]
- 12.McMillan D, Gilbody S, Beresford E, Neilly L. Can we predict suicide and non-fatal self-harm with the Beck Hopelessness Scale? A meta-analysis. Psychol Med. 2007;37(6):769–78. doi: 10.1017/S0033291706009664. [DOI] [PubMed] [Google Scholar]
- 13.O'Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP. Screening for and treatment of suicide risk relevant to primary care: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158(10):741–54. doi: 10.7326/0003-4819-158-10-201305210-00642. [DOI] [PubMed] [Google Scholar]
- 14.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 15.Ahmedani BK. Mental health stigma: society, individuals, and the profession. J Soc Work Values Ethics. 2011;8(2):41–416. [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmedani BK, Kubiak SP, Kessler RC, et al. Embarrassment when illness strikes a close relative: a World Mental Health Survey Consortium Multi-Site Study. Psychol Med. 2013;43(10):2191–202. doi: 10.1017/S003329171200298X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vannoy SD, Tai-Seale M, Duberstein P, Eaton LJ, Cook MA. Now what should I do? Primary care physicians' responses to older adults expressing thoughts of suicide. J Gen Intern Med. 2011;26(9):1005–11. doi: 10.1007/s11606-011-1726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vannoy SD, Fancher T, Meltvedt C, Unutzer J, Duberstein P, Kravitz RL. Suicide inquiry in primary care: creating context, inquiring, and following up. Ann Fam Med. 2010;8(1):33–9. doi: 10.1370/afm.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870–7. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 22.Hooper LM, Epstein SA, Weinfurt KP, DeCoster J, Qu L, Hannah NJ. Predictors of primary care physicians' self-reported intention to conduct suicide risk assessments. J Behav Health Serv Res. 2012;39(2):103–15. doi: 10.1007/s11414-011-9268-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graham RD, Rudd MD, Bryan CJ. Primary care providers' views regarding assessing and treating suicidal patients. Suicide Life Threat Behav. 2011;41(6):614–23. doi: 10.1111/j.1943-278X.2011.00058.x. [DOI] [PubMed] [Google Scholar]
- 24.Garfield RL, Druss BG. Health reform, health insurance, and mental health care. Am J Psychiatry. 2012;169(7):675–7. doi: 10.1176/appi.ajp.2012.12040506. [DOI] [PubMed] [Google Scholar]
- 25.Lang M. The impact of mental health insurance laws on state suicide rates. Health Econ. 2013;22(1):73–88. doi: 10.1002/hec.1816. [DOI] [PubMed] [Google Scholar]
- 26.Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–91. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 27.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 28.Gunnell D, Metcalfe C, While D, et al. Impact of national policy initiatives on fatal and non-fatal self-harm after psychiatric hospital discharge: time series analysis. Br J Psychiatry. 2012;201(3):233–8. doi: 10.1192/bjp.bp.111.104422. [DOI] [PubMed] [Google Scholar]
- 29.While D, Bickley H, Roscoe A, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross-sectional and before-and-after observational study. Lancet. 2012;379(9820):1005–12. doi: 10.1016/S0140-6736(11)61712-1. [DOI] [PubMed] [Google Scholar]
- 30.Mohr DC, Ho J, Duffecy J, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307(21):2278–85. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010;5(10):e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Linehan MM. Suicide intervention research: a field in desperate need of development. Suicide Life Threat Behav. 2008;38(5):483–5. doi: 10.1521/suli.2008.38.5.483. [DOI] [PubMed] [Google Scholar]
- 33.Morthorst B, Krogh J, Erlangsen A, Alberdi F, Nordentoft M. Effect of assertive outreach after suicide attempt in the AID (assertive intervention for deliberate self harm) trial: randomised controlled trial. BMJ. 2012;345:e4972. doi: 10.1136/bmj.e4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johannessen HA, Dieserud G, De LD, Claussen B, Zahl PH. Chain of care for patients who have attempted suicide: a follow-up study from Baerum, Norway. BMC Public Health. 2011;11:81. doi: 10.1186/1471-2458-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simon GE, Ludman EJ, Rutter CM. Incremental benefit and cost of telephone care management and telephone psychotherapy for depression in primary care. Arch Gen Psychiatry. 2009;66(10):1081–9. doi: 10.1001/archgenpsychiatry.2009.123. [DOI] [PubMed] [Google Scholar]
- 36.Britton PC, Bossarte RM, Thompson C, Kemp J, Conner KR. Influences on call outcomes among veteran callers to the National Veterans Crisis Line. Suicide Life Threat Behav. 2013;43(5):494–502. doi: 10.1111/sltb.12033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gould MS, Munfakh JL, Kleinman M, Lake AM. National suicide prevention lifeline: enhancing mental health care for suicidal individuals and other people in crisis. Suicide Life Threat Behav. 2012;42(1):22–35. doi: 10.1111/j.1943-278X.2011.00068.x. [DOI] [PubMed] [Google Scholar]
- 38.DeMartino RE, Crosby AE, EchoHawk M, et al. A call to collaboration: the federal commitment to suicide prevention. Suicide Life Threat Behav. 2003;33(2):101–10. doi: 10.1521/suli.33.2.101.22772. [DOI] [PubMed] [Google Scholar]
- 39.Miller M, Hemenway D. Guns and suicide in the U.S. N.Engl J Med. 2008;359(10):989–91. doi: 10.1056/NEJMp0805923. [DOI] [PubMed] [Google Scholar]
- 40.Miller M, Warren M, Hemenway D, Azrael D. Firearms and suicide in U.S. cities. Inj Prev. 2013 doi: 10.1136/injuryprev-2013-040969. in press. [DOI] [PubMed] [Google Scholar]
- 41.Reisch T, Steffen T, Habenstein A, Tschacher W. Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 “Army XXI” reform. Am J Psychiatry. 2013;170(9):977–84. doi: 10.1176/appi.ajp.2013.12091256. [DOI] [PubMed] [Google Scholar]
- 42.Hemenway D. Preventing gun violence by changing social norms. JAMA Intern Med. 2013;173(13):1167–8. doi: 10.1001/jamainternmed.2013.6949. [DOI] [PubMed] [Google Scholar]
- 43.Knox KL, Litts DA, Talcott GW, Feig JC, Caine ED. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the U.S. Air Force: cohort study. BMJ. 2003;327(7428):1376. doi: 10.1136/bmj.327.7428.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hampton T. Depression care effort brings dramatic drop in large HMO population's suicide rate. JAMA. 2010;303(19):1903–5. doi: 10.1001/jama.2010.595. [DOI] [PubMed] [Google Scholar]
- 45.Coffey CE, Coffey MJ, Ahmedani BK. An update on perfect depression care. Psychiatr Serv. 2013;64(4):396. doi: 10.1176/appi.PS.640422. [DOI] [PubMed] [Google Scholar]
- 46.Gahm GA, Reger MA, Kinn JT, Luxton DD, Skopp NA, Bush NE. Addressing the surveillance goal in the National Strategy for Suicide Prevention: the Department of Defense Suicide Event Report. Am J Public Health. 2012;102(1S):S24–S28. doi: 10.2105/AJPH.2011.300574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Britton PC, Conner KR, Maisto SA. An open trial of motivational interviewing to address suicidal ideation with hospitalized veterans. J Clin Psychol. 2012;68(9):961–71. doi: 10.1002/jclp.21885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pecoraro A, Royer-Malvestuto C, Rosenwasser B, et al. Factors contributing to dropping out from and returning to HIV treatment in an inner city primary care HIV clinic in the U.S. AIDS Care. 2013;25(11):1399–406. doi: 10.1080/09540121.2013.772273. [DOI] [PubMed] [Google Scholar]
- 49.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reiss-Brennan B, Briot P, Daumit G, Ford D. Evaluation of “depression in primary care” innovations. Adm Policy Ment Health. 2006;33(1):86–91. doi: 10.1007/s10488-005-4239-x. [DOI] [PubMed] [Google Scholar]
- 51.Solberg LI, Glasgow RE, Unutzer J, et al. Partnership research: a practical trial design for evaluation of a natural experiment to improve depression care. Med Care. 2010;48(7):576–82. doi: 10.1097/MLR.0b013e3181dbea62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pearson JL, Stanley B, King CA, Fisher CB. Intervention research with persons at high risk for suicidality: safety and ethical considerations. J Clin Psychiatry. 2001;62(25S):S17–S26. [PubMed] [Google Scholar]
- 53.King CA, Kramer AC. Intervention research with youths at elevated risk for suicide: meeting the ethical and regulatory challenges of informed consent and assent. Suicide Life Threat Behav. 2008;38(5):486–97. doi: 10.1521/suli.2008.38.5.486. [DOI] [PMC free article] [PubMed] [Google Scholar]