Abstract
Tobacco smoking continues to be the leading preventable cause of morbidity and mortality worldwide. Each year more than 5 million smokers die prematurely because of their habit wreaking havoc on the welfare of families and communities worldwide. While cigarettes remain the main tobacco killer worldwide, for many youth tobacco use and addiction is maintained by means other than cigarettes. In particular, over the past decade, waterpipe smoking (a.k.a. hookah, shisha, narghile) has become increasingly popular among youth in the Middle East, and is rapidly spreading globally. Available evidence suggests that waterpipe smoking is associated with many of the known risks of tobacco smoking, particularly cancer. Despite these worrisome signs, policies and interventions to address this emerging public health problem have been lagging behind. In this short review I discuss briefly the evidence generated mostly in the past decade about the global spread of waterpipe smoking and its cancer risk potential.
Keywords: Waterpipe, Hookah, Cancer, Risk
1. Introduction
Tobacco smoking continues to be the leading preventable cause of morbidity and mortality worldwide. Each year more than million smokers die prematurely because of their habit wreaking havoc on the welfare of families and communities worldwide. Most of the brunt of the tobacco epidemic is currently borne by developing countries, and this is likely to worsen unless an effective and comprehensive response is materialized [1]. While cigarettes remain the main tobacco killer worldwide, for many youth tobacco use and addiction is maintained by means other than cigarettes. In particular, over the past decade, waterpipe smoking (a.k.a. hookah, shisha, narghile) has become increasingly widespread among youth in the Middle East, and is rapidly spreading elsewhere [2]. Many factors are suggested as the main drives behind the re-emergence of this ancient tobacco use method including; the introduction of manufacture sweetened-flavored waterpipe tobacco (a.k.a. Maassel), the harm-reduced perception of waterpipe smoking, and the communication revolution brought about by the internet [2].
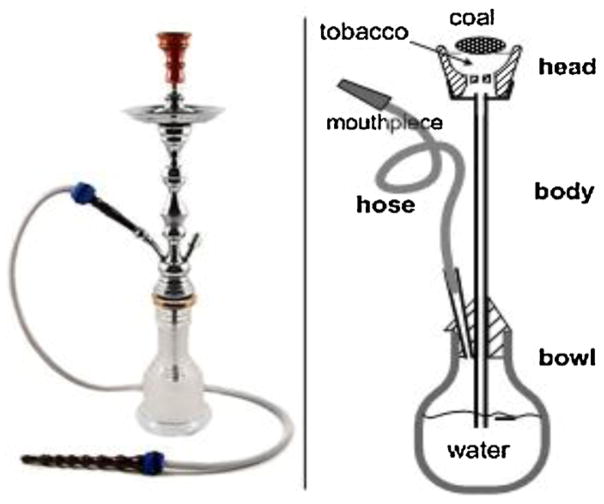
The waterpipe, known in many cultures under different shapes and names (e.g., hookah, shisha, narghile), is a centuries-old tobacco use method that has traditionally been associated with eastern societies. Evidence from around the world is accumulating to signify the emergence of waterpipe smoking as a global threat to public health [3–8]. In the waterpipe, charcoal-heated air passes through a perforated aluminum foil separating the charcoal from the flavored tobacco to become smoke that cools as it bubbles through the water on its way to the smoker (Fig. 1). This last feature; i.e. the passage of smoke through water, underlies much of the widespread misperception about waterpipe’s “reduced” harm and addictiveness [9]. Available evidence however, suggests that waterpipe smoking is associated with smoking-related diseases [10]. Despite these worrisome signs of fast spread and potential health risks, policies and interventions to address this emerging public health problem have been lagging behind. In this short review I discuss briefly the evidence generated mostly in the past decade about the global spread of waterpipe smoking and its cancer risk potential.
Fig. 1.
Waterpipe picture (left) and schematic showing main parts (right).
2. The global epidemic of waterpipe smoking
Epidemiological trends of waterpipe smoking are very alarming, and what started in the 1990s as a local phenomenon among youth in the Middle East soon became a global trend [2]. In the Middle East, prevalence estimates of waterpipe smoking among youth have already surpassed those of cigarette for most of countries, and has been increasing considerably in the past decade or so [5]. For example, in a representative sample (n = 1781) of 7th graders (≈13 years) in Irbid-Jordan, the prevalence of waterpipe smoking was more than double that of cigarette for both boys (20% vs. 9%) and girls (7.5% vs. 2.3%) [11]. This same study showed 79% increase in ever waterpipe smoking and 42% increase in current waterpipe smoking among students within 2 years of follow up. A multi-county study involving a representative sample of all 13–15 year school children in several Arab gulf countries (Bahrain, Oman, Qatar, UAE, Kuwait, Yemen) showed a prevalence of waterpipe smoking ranging from 9 to 15%, and mostly surpassing the prevalence of cigarette smoking among these populations [12]. Recent evidence from dispersed populations and societies around the world shows that the rest of the world is catching up on the waterpipe trend [13]. For example, among college students in the US, waterpipe smoking is steadily becoming the second most popular form of tobacco use. According to a recent survey involving more than 100,000 students in 152 colleges in the US, current waterpipe smoking was reported by 8.4% of students, second only to cigarettes (16.8%) [14]. The global spread of waterpipe smoking among youth is best revealed by the Global Youth Tobacco Survey (GYTS); the largest to date surveillance of tobacco use among youth (13–15 years) with 209 surveys conducted in 95 countries. Time trends from the GYTS (1999–2008) involving more than half million participants worldwide, show that while cigarette smoking is either stable or declining, other forms of tobacco are showing a rising trend, most notably waterpipe smoking [15]. In epidemiological terms, such trends covering vast geographical territories, diverse societies, and encompassing several age groups are indicative of an epidemic that has taken hold among youth rather than a passing fad. This trend has the potential only to exacerbate unless we do something about it.
3. Epidemiological evidence of waterpipe cancer risk
So far, solid epidemiological evidence about cancer risk associated with waterpipe smoking is scarce. What we have is converging evidence from several lines of inquiry about the cancer-inducing potential of waterpipe smoking. A recent systematic review of studies of health effects of waterpipe smoking shows for example that waterpipe smoking more than doubles the risk of lung cancer, but was not significantly associated with bladder cancer, nasopharyngeal cancer, esophageal cancer, or oral dysplasia [10]. At the same time the review highlights the methodological problems of the available literature on the long term health effects of waterpipe smoking. Specifically, most waterpipe-lung cancer studies concerned local types (e.g. Chinese) of waterpipe that are different from the waterpipe used in most parts of the world nowadays, and suffered from inadequate attention to confounding such as exposure to secondhand smoke, or occupational exposures [10]. More recently, a recent-case control study of the association between waterpipe smoking and lung cancer in the Kashmir valley showed that waterpipe smoking is associated with a 6-fold increase in lung cancer risk compared to nonsmoking [16]. This study again, did not control for any other exposures (secondhand smoke, occupational exposures), or even socio-economic factors.
The relation between waterpipe smoking and oral cancers is even less studied. To date, only one study looked at waterpipe smoking and nasopharyngeal cancer, but the small sample size of that study precluded any meaningful conclusions about that cancer risk [17]. The lack of studies of waterpipe smoking and oral cancers lies in contrast with the strong potential of this tobacco use method to cause such cancers. This potential has been highlighted in two recent reports based on the (1) high levels of oral and oropharyngeal cancers in some countries of the Middle East compared to other parts of the world, (2) extended exposure to the carcinogenic smoke content (e.g. tar, PAH, aldehydes) associated with waterpipe smoking (average session time 1 hour), (3) chronic mechanical trauma and irritation from the wooden or plastic mouth piece, (4) chronic infection triggered by waterpipe sharing, (5) oral complications of waterpipe smoking such as bone loss and acute osteitis, and (6) oral epithelial cells reaction to exposure to waterpipe smoke indicative of early carcinogenic processes [18–20].
Most of the direct epidemiological evidence about waterpipe smoking and cancer risk lacks the methodological rigor needed to provide clear public health and policy guidance. On the other hand, the relative novelty of the waterpipe epidemic is another barrier for epidemiological studies looking at the long term health effects of waterpipe smoking akin of the case control and cohort studies of the 1950s that led the way for tobacco control efforts against cigarettes. However, awaiting such evidence can be very costly, as the history of the cigarette epidemic clearly demonstrates. In addition, already existing evidence draws a picture of a highly hazardous and widespread behavior that requires urgent attention by policy makers and tobacco control advocates. Below I review some of indirect evidence of waterpipe cancer risk based on studies of waterpipe smoke constituents and smokers’ exposure to known smoking-related carcinogens, as well as some evidence about waterpipe-related genetic toxicity.
4. Waterpipe smoke constituents related to cancer risk
Several studies pioneered by one of our collaborators at the American University of Beirut (Alan Shihadeh, AUB), have demonstrated the presence of high levels of major tobacco-related carcinogens and toxicants in waterpipe smoke (Table 1) [21]. Most of these studies relied on analyzing machine-generated smoke (programed to imitate actual waterpipe smoking behaviors) that showed good correlation with human exposure for several key waterpipe smoking related toxicants [22,23]. One note of caution when interpreting the waterpipe/cigarettes comparative data of smoke constituents is that when comparing one “unit” of waterpipe and cigarette we need to bear in mind that a typical waterpipe smoking cession involves exposure to much larger volumes of smoke due to larger puff volume (about 500 ml for waterpipe compared to 50 ml for cigarette) and longer session duration (about 1 h for waterpipe compared to 5–6 min for cigarette) [21–26]. Studies of smoke constituents have shown that waterpipe smoke contains known carcinogens such as polycyclic aromatic hydrocarbons (PAHs), and naphthylamines [22,24]. Specifically, a group at the German Federal Institute for Risk Assessment demonstrated recently that waterpipe smoke contains a variety of carcinogenic and toxic substances such as tobacco-specific nitrosamines, polycyclic aromatic hydrocarbons, primary aromatic amines and carbon monoxide [24,25]. Furthermore, Al Rashidi et al. at AUB reported that carbonyls, like formaldehyde (IARC group 1) (IARC 2006), acetaldehyde (IARC group 2B) (IARC 1999) or acrolein, are also present in the waterpipe smoke, and that the levels of these toxicants were significantly higher than in cigarette smoke [26].
Table 1.
Comparison of smoke toxicants yield between waterpipe and cigarette.a
| Waterpipe | Cigarette | Waterpipe/cig | |
|---|---|---|---|
| “Tar” (mg) | 802 | 15–29 | 8–53 |
| Nicotine (mg) | 3.09 | 1–3 | 1–3 |
| CO (mg) | 145 | 10–23 | 6–15 |
| PAH | |||
| Benzo(a)pyrene (ng) | 307 | 20–40 | 8–15 |
| Dibenz(a,h)anthracene (ng) | 147 | 4 | 37 |
| Indeno(1,2,3-cd)pyrene (ng) | 183 | 4–20 | 9–45 |
| Aldehydes | |||
| Formaldehyde (mg) | 630 | 70–100 | 6–9 |
| Acetaldehyde (mg) | 2520 | 500–1400 | 2–5 |
| Acrolein (mg) | 892 | 60–140 | 6–14 |
| Heavy metals | |||
| Arsenic (ng) | 165 | 40–120 | 1–4 |
| Chromium (ng) | 1340 | 4–70 | 19–335 |
| Lead (ng) | 6870 | 34–85 | 80–200 |
| Phenols (μg) | |||
| Phenol | 58.0 | 22.3 | 2.6 |
| o-Cresol | 4.41 | 5.79 | 0.8 |
| m-Cresol | 4.66 | 4.33 | 1.1 |
| p-Cresol | 5.38 | 10.1 | 0.5 |
| Catechol | 316 | 40.7 | 7.8 |
| Resorcinol | 1.69 | 0.79 | 2.1 |
| Hydroquinone | 111 | 34.6 | 3.2 |
5. Waterpipe smokers’ exposure to tobacco smoke carcinogens
The above mentioned studies about waterpipe smoke constituents are telling about the potential cancer risks associated with waterpipe smoking, but they need to be complemented by studies showing that these toxicants actually get to the smokers. We are beginning to learn about that as the first in vivo evidence about waterpipe smokers’ exposure to major tobacco related carcinogens came recently from Jacob and colleagues at UCSF [27]. This group enrolled 16 waterpipe smokers and measured several markers of tobacco smoke exposure in the blood and urine of these smokers before and after one waterpipe smoking session. They found that urinary excretion of tobacco-specific nitrosamine 4-(methylni-trosamino)-1-(3-pyridyl)-1-butanol (NNAL) and polycyclic aromatic hydrocarbon (PAH) metabolite biomarker increased significantly following waterpipe smoking [27]. A more recent study confirmed this initial observation by comparing urinary levels of (NNAL) and its glucuronides (NNAl-Gluc) in males who were either current cigarette or waterpipe smokers with their nonsmoking wives in rural Egypt. This study found significantly higher levels of urinary NNAL among male smokers of either cigarettes or waterpipe compared with their nonsmoking wives [28]. Together, the smoke constituents and exposure data provide compelling evidence about hazardous exposures associated with waterpipe smoking and their potential cancer risk for smokers.
6. Waterpipe smoking and genetic toxicity
Genetic toxicity is one of the main mechanisms of carcinogenesis, and demonstrating markers of genetic material damage as a result of exposure to waterpipe smoke or in waterpipe smokers can provide early evidence about waterpipe’s cancer potential. For example, in 2000 Yadav and Thakur compared the mitotic index, chromosomal aberrations, sister chromatid exchanges, and satellite associations in waterpipe smokers and nonsmokers, and found all to be significantly increased in waterpipe smokers [29]. Later on El-Setouhy et al. conducted a micronuclei assessment in the exfoliated oral cells of waterpipe smokers and never smokers, and found a higher level of total micronuclei in waterpipe smokers compared to nonsmokers [18]. More recently, an in vitro study looking at the mutagenicity of waterpipe smoke condensate using the Ames test (Salmonella reverse mutagenicity assay) failed to show sufficient mutagenic effect at the usual dose range, but some mutagenic response was seen at the highest tested dose [30]. Finally, human study of waterpipe smoking related genotoxicity to peripheral blood lymphocytes using chromosomal aberrations was recently conducted. The results showed that similarly to cigarette smoking, waterpipe smoking significantly increased the frequencies of chromosomal aberrations, and that these aberration’s increased with more waterpipe use [31]. As such, converging evidence from several lines of inquiry support the notion that, like cigarette, waterpipe smoking involves cancer risk to smokers.
7. Conclusions
Waterpipe smoking bears all the signs of burgeoning global epidemic with grave outlook for tobacco-related morbidity and mortality. Despite waterpipe’s alarming trends, there is a failure of policies and regulations to address this emerging public health threat. Most tobacco control policies and regulations, including the Framework Convention on Tobacco Control (FCTC), either exempt waterpipe smoking or are mostly tilted toward cigarettes and the traditional tobacco industry of cigarette manufacturers [32,33]. This policy failure perhaps represents one of the important drives of the current waterpipe epidemic. Well designed and conducted studies about waterpipe long term health risks such lung and oral cancers are likely to help drive powerful policy and intervention initiatives to limit the spread of waterpipe smoking. In the meantime, we have enough evidence from studies of waterpipe smoke constituents and smokers exposure to predict these long term effects, and start active public health campaigns to alert smokers and policy makers to this emerging public health threat. Delaying that response or failing to react to the waterpipe epidemic will mean repeating the mistakes of the past and reaping their consequences of preventable death and suffering.
Acknowledgments
This work is supported by the National Institute on Drug Abuse (NIDA) Grants R01 DA024876 and R01 DA035160.
Footnotes
Conflict of interest
None.
References
- 1.WHO report on the global tobacco epidemic, 2011. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36(1–2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Waterpipe tobacco smoking: health effects, research needs and recommended actions by regulators. Geneva: WHO Document Production Services; 2005. [Google Scholar]
- 4.American Lung Association. Tobacco policy trend alert AN EMERGING DEADLY TREND: WATERPIPE TOBACCO USE. 2009 < www.slati.lungusa.org/alerts/Trend%20Alert_Waterpipes.pdf>.
- 5.El-Awa F, Warren CW, Jones NR. Changes in tobacco use among 13–15-year-olds between 1999 and 2007: findings from the Eastern Mediterranean Region. East Mediterr Health J. 2010;16(3):266–73. [PubMed] [Google Scholar]
- 6.Quenqua D. New York Times. 2011. May 30, Putting a crimp in the Hookah. [Google Scholar]
- 7.Qureshi H. The Guardian. 2011. Aug 22, Smoking shisha: how bad is it for you? [Google Scholar]
- 8.Gatrad R, Gatrad A, Sheikh A. Hookah smoking. Br Med J. 2007;335(7609):20. doi: 10.1136/bmj.39227.409641.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34:275–85. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39(3):834–57. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 11.Mzayek F, Khader Y, Eissenberg T, Al Ali R, Ward KD, Maziak W. Patterns of water-pipe and cigarette smoking initiation in schoolchildren: Irbid longitudinal smoking study. Nicotine Tob Res. 2012;14(4):448–54. doi: 10.1093/ntr/ntr234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moh’d Al-Mulla A, Abdou Helmy S, Al-Lawati J, Al Nasser S, Ali Abdel Rahman S, Almutawa A, et al. Prevalence of tobacco use among students aged 13–15 years in Health Ministers’ Council/Gulf Cooperation Council Member States, 2001–2004. J Sch Health. 2008;78(6):337–43. doi: 10.1111/j.1746-1561.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- 13.Akl EA, Gunukula SK, Aleem S, Obeid R, Jaoude PA, Honeine R, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Primack BA, Shensa A, Kim KH, Carroll MV, Hoban MT, Leino EV, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res. 2012 doi: 10.1093/ntr/nts076. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13–15 year olds between 1999 and 2008: findings from the Global Youth Tobacco Survey. Glob Health Promot. 2009;16(Suppl 2):38–90. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- 16.Koul PA, Hajni MR, Sheikh MA, Khan UH, Shah A, Khan Y, et al. Hookah smoking and lung cancer in the Kashmir valley of the Indian subcontinent. Asian Pac J Cancer Prev. 2011;12(2):519–24. [PubMed] [Google Scholar]
- 17.Feng BJ, Khyatti M, Ben-Ayoub W, Dahmoul S, Ayad M, Maachi F, et al. Cannabis, tobacco and domestic fumes intake are associated with nasopharyngeal carcinoma in North Africa. Br J Cancer. 2009;101(7):1207–12. doi: 10.1038/sj.bjc.6605281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Setouhy M, Loffredo CA, Radwan G, Abdel Rahman R, Mahfouz E, Israel E, et al. Genotoxic effects of waterpipe smoking on the buccal mucosa cells. Mutat Res. 2008;655(1–2):36–40. doi: 10.1016/j.mrgentox.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rastam S, Li FM, Fouad FM, Al Kamal HM, Akil N, Al Moustafa AE. Water pipe smoking and human oral cancers. Med Hypotheses. 2010;74(3):457–9. doi: 10.1016/j.mehy.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Dar-Odeh NS, Abu-Hammad OA. Narghile smoking and its adverse health consequences: a literature review. Br Dent J. 2009;206(11):571–3. doi: 10.1038/sj.bdj.2009.475. [DOI] [PubMed] [Google Scholar]
- 21.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003;41(1):143–52. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 22.Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food Chem Toxicol. 2008;46:1582–90. doi: 10.1016/j.fct.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 23.Shihadeh AL, Eissenberg TE. Significance of smoking machine toxicant yields to blood-level exposure in water pipe tobacco smokers. Cancer Epidemiol Biomarkers Prev. 2011;20(11):2457–60. doi: 10.1158/1055-9965.EPI-11-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schubert J, Hahn J, Dettbarn G, Seidel A, Luch A, Schulz TG. Mainstream smoke of the waterpipe: does this environmental matrix reveal as significant source of toxic compounds? Toxicol Lett. 2011;205(3):279–84. doi: 10.1016/j.toxlet.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 25.Schubert J, Kappenstein O, Luch A, Schulz TG. Analysis of primary aromatic amines in the mainstream waterpipe smoke using liquid chromatography–electrospray ionization tandem mass spectrometry. J Chromatogr A. 2011;1218:5628–37. doi: 10.1016/j.chroma.2011.06.072. [DOI] [PubMed] [Google Scholar]
- 26.Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem Toxicol. 2008;46:3546–9. doi: 10.1016/j.fct.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacob P, 3rd, Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, et al. Nicotine, carbon monoxide, and carcinogen exposure after a single use of a water pipe. Cancer Epidemiol Biomarkers Prev. 2011;20(11):2345–53. doi: 10.1158/1055-9965.EPI-11-0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radwan G, Hecht SS, Carmella SG, Loffredo CA. Tobacco-specific nitrosamine exposures in smokers and nonsmokers exposed to cigarette or waterpipe tobacco smoke. Nicotine Tob Res. 2012 doi: 10.1093/ntr/nts099. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yadav JS, Thakur S. Genetic risk assessment in hookah smokers. Cytobios. 2000;101(397):101–13. [PubMed] [Google Scholar]
- 30.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro cytotoxicity and mutagenicity of mainstream waterpipe smoke and its functional consequences on alveolar type II derived cells. Toxicol Lett. 2012;211(3):220–31. doi: 10.1016/j.toxlet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alsatari ES, Azab M, Khabour OF, Alzoubi KH, Sadiq MF. Assessment of DNA damage using chromosomal aberrations assay in lymphocytes of waterpipe smokers. Int J Occup Med Environ Health. 2012;25(3):218–24. doi: 10.2478/S13382-012-0027-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakkash R, Khalil J. Health warning labelling practices on narghile (shisha, hookah) waterpipe tobacco products and related accessories. Tob Control. 2010;19:235, e239. doi: 10.1136/tc.2009.031773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noonan D. Exemptions for hookah bars in clean indoor air legislation: a public health concern. Public Health Nurs. 2010;27(1):49–53. doi: 10.1111/j.1525-1446.2009.00826.x. [DOI] [PubMed] [Google Scholar]
- 34.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43(5):655–61. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 35.Sepetdjian E, Shihadeh A, Saliba N. Phenolic compounds in particles of mainstream waterpipe smoke. Nicotine Tob Res. doi: 10.1093/ntr/nts255. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jenkins R, Guerin M, Tomkins B. The chemistry of environmental tobacco smoke. Boca Raton: Lewis Publishers; 2000. [Google Scholar]