Abstract
Ambulatory blood pressure (BP) monitoring provides valuable information on a person’s BP phenotype. Abnormal ambulatory BP phenotypes include white-coat hypertension, masked hypertension, nocturnal nondipping, nocturnal hypertension, and high BP variability. Compared to people with sustained normotension (normal BP in the clinic and on ambulatory BP monitoring), the limited research available suggests that the risk of developing sustained hypertension (abnormal BP in the clinic and on ambulatory BP monitoring) over 5 to 10 years is approximately two to three times greater for people with white-coat or masked hypertension. More limited data suggest that nondipping might predate hypertension, and no studies, to our knowledge, have examined whether nocturnal hypertension or high ambulatory BP variability predict hypertension. Ambulatory BP monitoring may be useful in identifying people at increased risk of developing sustained hypertension, but the clinical utility for such use would need to be further examined.
Keywords: Hypertension, ambulatory blood pressure monitoring, ambulatory blood pressure phenotypes, white-coat hypertension, masked hypertension, incidence of hypertension, nondipping, blood pressure variability
INTRODUCTION
Hypertension is one of the most important risk factors for cardiovascular disease (CVD), which remains the leading cause of death in America [1]. In the United States (US), on average, the risk of developing hypertension over a lifetime is approximately 90% [2]. The short-term risk of incident hypertension is highest for blacks and lowest for whites up until 75 years of age [new 3]. An estimated 40% of CVD mortality is due to high blood pressure [1]. Thus, primary prevention of hypertension is an important public health goal [4]. Primary prevention of hypertension from a clinical standpoint consists of identifying patients who are “pre-hypertensive” and counseling them to lose weight if warranted, reduce sodium intake, adopt the DASH (Dietary Approaches to Stop Hypertension) eating plan [5], exercise, and limit alcohol intake [6]. While these lifestyle changes can help prevent or delay the onset of hypertension, clinical effectiveness at getting patients with “prehypertension” to adopt them is extremely limited [7-9].
In addition to the category of prehypertension itself [6], several risk scores for hypertension have been developed [10]. The underlying basis for developing such scores is that targeting people most at risk in the shorter term might increase the effectiveness of preventive interventions such as lifestyle recommendations. Identifying those at higher risk may also permit use of more aggressive interventions such as specialized weight loss or exercise programs. People whose short-term risk is increased can also be monitored more closely for development of hypertension. Not surprisingly, in all of the hypertension risk models, a person’s blood pressure (BP) level is one of the most important predictors [10].
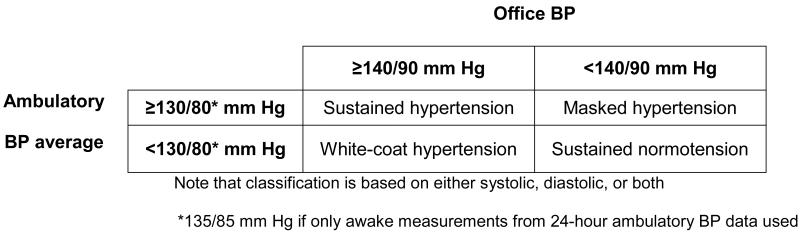
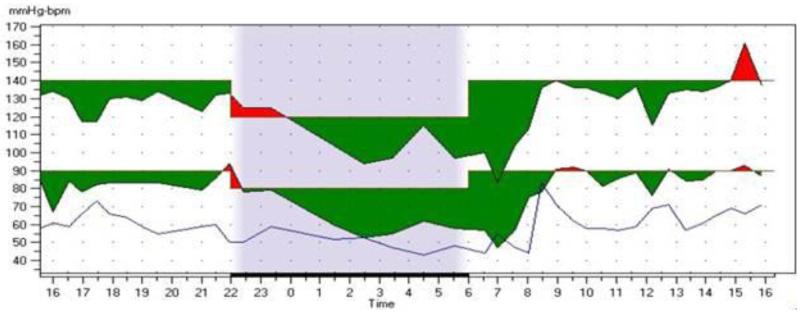
Through the use of 24-hour ambulatory BP monitoring [11], it has become evident that people exhibit several BP patterns (Table 1). The pairing of office BP measurement(s) with average BP derived from ambulatory BP data yields four major phenotypes of BP: sustained normotension, white-coat hypertension, masked hypertension, and sustained hypertension (Figure 1). Ambulatory BP monitoring also uniquely provides measures of BP during sleep which can be used to calculate mean sleep BP. Normally during sleep, BP decreases (“dips”) such that sleep BP average is lower than awake BP average (Figure 2). The “normal” dip is considered 10%-20% [12]. Individuals who dip <10% are said to exhibit the nondipper phenotype (although this category includes “mild dippers” who dip but do so less than 10%). Nondippers whose sleep BP average is actually greater than their awake BP average are described as “risers”, and dippers who exceed 20% are sometimes referred to as “extreme dippers”. Ambulatory BP measurements can also be used to derive other measures of variability such as standard deviation and average real variability [13]. Thus, “high ambulatory BP variability” represents another phenotype.
Table 1.
Major Ambulatory Blood Pressure Phenotypes
| Phenotype | Usual Definition |
|---|---|
| Sustained normotension | Office BP is not elevated AND 24-hour ambulatory BP average is <130/80 mm Hg |
| White-coat hypertension | Office BP is elevated BUT 24-hour ambulatory BP average is <130/80 mm Hg |
| Masked hypertension | Office BP is not elevated BUT 24-hour ambulatory BP average is ≥130/80 mm Hg (or awake average is ≥135/85 mm Hg) |
| Sustained hypertension | Office BP is elevated AND 24-hour ambulatory BP average is ≥130/80 mm Hg (or awake average is ≥135/85 mm Hg) |
| Nocturnal hypertension | Sleep BP average ≥120/70 mm Hg |
| Nondipping | Sleep BP average decreases less than 10% relative to awake ambulatory BP average |
| High (average real) variability |
Average absolute difference between consecutive readings over the 24 hours; “high” variability usually defined as the highest percentile (e.g., quartile) in the sample |
Figure 1.
Ambulatory Blood Pressure Phenotypes Based on Pairing Office and Ambulatory Measurements
Figure 2. A 24-Hour Ambulatory Blood Pressure Monitoring Graph.
The 24-hour period of monitoring is divided primarily into awake (often called “daytime”) and sleep (often called “nocturnal”) periods (shaded section in above graph). Sometimes, to improve tolerability of wearing the monitor, readings are taken at less frequent intervals during the sleep period. A diary is often used as the basis by which to define sleep time, although some studies use a specified period (e.g., midnight to 6am) to denote sleep time. Based on the time periods, a person’s awake (or daytime) BP average can be calculated, as can their sleep (or nocturnal) average. Shown above is the graph of a person whose awake average (based on 31 measurements) was 128/81 (±14/11) mm Hg and sleep average (based on 7 measurements) was 108/64 (±13/11) mm Hg. The nocturnal systolic dip is calculated as (128-108)/128, which is approximately 16%. The lowest line on the graph shows heart rate.
While we are aware of no risk score that incorporates ambulatory BP, people with abnormal BP phenotypes might be at greater risk of developing sustained hypertension than people whose BP pattern is considered normal or optimal. Herein, we summarize relevant literature examining the risk of developing sustained hypertension according to baseline ambulatory BP phenotype. Given the limited data available, we also included studies that categorized baseline BP phenotype using home BP monitoring.
DEFINING INCIDENT HYPERTENSION
For the purpose of this paper, we preferred studies that examined incident hypertension based on 24-hour ambulatory BP monitoring. Often, such studies would also include measurements of BP taken in the office setting. As shown in Figure 1, when office BP and ambulatory or home BP average are both elevated, the term “sustained” hypertension is used. Incident hypertension could also be based on office BP readings alone if 24-hour ambulatory BP or home BP was not available. However, in such instances it is impossible to know whether the incident hypertension is white-coat or sustained.
PHENOTYPES AND RISK FOR SUSTAINED HYPERTENSION
Sustained Normotension
Sustained normotension is defined as non-elevated office BP (<140/90 mm Hg) and normal ambulatory BP (i.e. daytime ambulatory BP average < 135/85 mm Hg or 24-hour ambulatory BP average <130/80 mm Hg) or home BP average < 135/85 mm Hg. Compared to persons with abnormal BP phenotypes discussed below, a person with sustained normotension, especially if office BP is optimal (i.e., <120/80 mm Hg) by conventional standards, has the lowest risk of developing hypertension, at least in the short-term. For example, one study showed that among people with sustained normotension at baseline, approximately 18% had sustained hypertension 10 years later [14]. In another study conducted in Japan that used home BP measurements for out-of-office assessments, 22% of adults 40 years and older who had sustained (home BP) normotension at baseline had developed sustained (home BP) hypertension (elevated office BP defined as ≥140/90 mm Hg, and elevated home BP defined as ≥ 135/85 mm Hg or start of treatment with antihypertensive medication) 8 years later [15].
White-Coat Hypertension
White-coat hypertension is said to be present when office BP is elevated (≥140/90 mm Hg) with normal ambulatory BP (i.e. daytime ambulatory BP < 135/85 mm Hg or 24-hour ambulatory BP <130/80 mm Hg) or home BP (< 135/85 mm Hg).
In the PAMELA study, Mancia and colleagues examined 1412 adults whose ages ranged from 25 to 74 years at baseline. Participants had office visit BP measurements and 24-hour ambulatory BP monitoring at baseline and 10 years later [14]. At baseline there were 758 participants categorized as sustained normotensive and 225 categorized as white-coat hypertensive. Of the participants with white-coat hypertension at baseline, 43% had sustained hypertension 10-years later compared to 18% among those with sustained normotension at baseline. After adjusting for age and sex, and excluding any participants on BP-lowering medications, the odds of developing sustained hypertension were approximately three times that of those with sustained normotension (aOR 3.25; 95% CI 2.08-5.07). A similar percentage was noted in the Japanese home BP measurement study mentioned above, in which 47% of those with white-coat hypertension at baseline had developed sustained (home BP) hypertension 8 years later [15]. After adjustment for multiple confounders, the odds ratio for development of sustained (home BP) hypertension was 2.9 (95% CI 1.9-4.3) [15].
Masked Hypertension
People whose office BP is <140/90 mm Hg but whose 24-hour ambulatory BP or home BP average is elevated (Table) are classified as having masked hypertension. In the PAMELA study described above, of the participants with masked hypertension at baseline (n=124), 47% had sustained hypertension 10-years later [14]. After adjusting for age and sex, and excluding any participants taking BP-lowering medications, the odds of developing sustained hypertension were approximately 1.7 times that of those with sustained normotension (aOR 1.65; 95% CI 1.27-2.15). In another study of 1669 white-collar workers, 232 had masked hypertension at baseline [16]. At three years, 26% of those with masked hypertension had sustained hypertension; and at five years, 35% had sustained hypertension. Another study with average follow-up of 6 to 7 years found a 42% incidence of sustained hypertension among adults with masked hypertension compared to a 17% incidence among those with sustained normotension [17].
Nondipping Pattern
As mentioned earlier, a nondipping pattern is defined as sleep BP average that decreases less than 10% relative to awake ambulatory BP average. It has been suggested that nondipping in younger adults might predate hypertension, possibly due to an early autonomic imbalance as a contributor [18]. In one analysis of 264 adults (mean age 30 years) who had ambulatory BP monitoring, 118 were nondippers [18]. Baseline office BP was 107/72 mm Hg. Over a follow-up of 15 years, the incidence of a change to office prehypertension or hypertension was 36/1000 person-years (64 out of 118) among non-dippers compared to 29/1000 person-years (64 out of 146) among dippers. When adjusted for race, age, baseline clinic BP, and other factors, the difference was not significant. However, the study was limited by a small sample size as well as office BP that was low at baseline. Additionally, participants did not have follow-up ambulatory BP monitoring, so it is not known whether participants with incident hypertension had sustained or white-coat hypertension.
Nocturnal Hypertension
Nocturnal hypertension is defined as sleep BP average of ≥120/70 mm Hg during ambulatory BP monitoring. It can occur with daytime (awake) hypertension or in isolation [19]. It can also occur in dippers or nondippers but appears superior to nondipping status as a predictor of cardiovascular disease risk [20]. We are aware of no studies that have examined the incidence of sustained hypertension according to baseline nocturnal hypertension status.
High Ambulatory BP Variability
Ambulatory BP variability can be reported as a standard deviation of the BP readings from the 24-hour period or as average real variability (ARV). ARV is calculated as the average absolute difference between consecutive readings over the 24 hours and therefore is sensitive to the order of BP measurements over the monitoring period. “High” variability is usually defined as the highest percentile (e.g., quartile) in the sample being studied. On ABPM, ARV is a better predictor of cardiovascular risk than the traditional SD [13,21]. While research shows that higher ARV is associated with cardiovascular disease [22], we are aware of no studies that have examined the incidence of hypertension according to levels of ARV.
DISCUSSION
While there are a number of studies that demonstrate the increased CVD-related risk associated with certain abnormal ambulatory BP phenotypes [22-27], few studies have examined the risk of hypertension according to these phenotypes. Despite relatively limited data, however, it does appear that people with white-coat or masked hypertension are at two to three times the risk of developing sustained hypertension over 5 to 10 years compared to those with sustained normotension. It also appears that people with normal ambulatory BP averages but a nondipping nocturnal BP pattern may be at increased risk of developing hypertension. We are aware of no studies that examined the risk of sustained hypertension associated with nocturnal hypertension or across strata of ambulatory BP variability. Studies that have used home BP instead of ambulatory BP monitoring have found similar results, although it is not certain that these methods are interchangeable for identifying out-of-office BP phenotypes [28].
In current US clinical practice, most people who have ambulatory BP do so for evaluation of possible white-coat effect. Most evidence demonstrates that people with white-coat hypertension have CVD risk similar to, or only slightly greater than, people with true normotension, and therefore do not need to be offered BP-lowering medications [27,29]. Given the increased short-term risk of sustained hypertension, it seems prudent to monitor such patients more closely for development of hypertension. Additionally, a push for more aggressive lifestyle modifications may be worthwhile. Masked hypertension poses a different challenge. If a person is identified as having masked hypertension, BP-lowering treatment might actually be warranted based on the fact that the CVD risk among such patients approaches that of those with sustained hypertension. However, there are currently no trials that have demonstrated a reduction in CVD events by treating masked hypertension. It seems clear at the very least such patients should be monitored closely for development of sustained hypertension.
In addition to the small number of studies that have examined the incidence of hypertension according to ambulatory BP phenotypes, the existing research has a number of limitations. Studies have been limited in terms of the population enrolled. For example, studies may have only included only Caucasions (PAMELA) [14]. Given that Blacks have a higher prevalence and severity of hypertension, the risk based on ambulatory BP phenotype may differ. We know, for instance, that Blacks have a higher prevalence of nondipping [18].
A systematic review of hypertension risk models is notable for the fact that no models include baseline ambulatory BP measures [10]. Risk prediction might be refined by including such measures. An additional important point to note about research on hypertension risk is that any study that categorizes incident hypertension solely by office BP is limited as it would not necessarily reflect sustained hypertension.
CONCLUSIONS
People with white-coat and masked hypertension are two to three times more likely to develop sustained hypertension over 5 to 10 years. It also appears that nondipping might be a harbinger of developing hypertension. We know of no studies examining whether nocturnal hypertension or high ambulatory BP variability among people with otherwise normal ambulatory BP average predict hypertension. In addition to its value in diagnosis and management of hypertension, ambulatory BP monitoring may be useful in identifying some groups at increased short-term risk of developing hypertension. Further research is needed to learn whether such use is clinically effective at preventing or delaying hypertension.
Acknowledgments
This article was partially supported by grants R01-HL098604 (Dr. Viera) and P01-HL047540 (Dr. Shimbo) from the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Anthony Viera has served on the medical advisory board for Suntech Medical, manufacturer of a brand of ambulatory blood pressure monitor, as well as the hypertension advisory board for Daiichi-Sankyo.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
* Of importance
**Of major importance
- 1.Go AS, Mozaffarian D, Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee.Executive summary: heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014 Jan 21;129(3):399–410. doi: 10.1161/01.cir.0000442015.53336.12. ⍰ . doi: 10.1161/01.cir.0000442015.53336.12. Presents the most recent statistics on cardiovascular disease including the contributions of hypertension. [DOI] [PubMed] [Google Scholar]
- 2.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the Multi-ethnic Study of Atherosclerosis. Hypertension. 2011;57:1101–07. doi: 10.1161/HYPERTENSIONAHA.110.168005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287(8):1003–10. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, He J, Appel LJ, et al. National High Blood Pressure Education Program Coordinating Committee. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002 Oct 16;288(15):1882–8. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 5.Sacks FM, Svetkey LP, Vollmer WM, et al. DASH-Sodium Collaborative Research Group.Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001 Jan 4;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee.. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 7.Viera AJ, Lingley K, Esserman D. Effects of labeling patients as prehypertensive. J Am Board Fam Med. 2010;23(5):571–83. doi: 10.3122/jabfm.2010.05.100047. [DOI] [PubMed] [Google Scholar]
- 8.Viera AJ, Bangura F, Mitchell CM, Cerna A, Sloane P. Do clinicians tell patients they have prehypertension? J Am Board Fam Med. 2011;24(1):117–8. doi: 10.3122/jabfm.2011.01.100206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spruill TM, Feltheimer SD, Harlapur M, et al. Are there consequences of labeling patients with prehypertension? An experimental study of effects on blood pressure and quality of life. J Psychosom Res. 2013 May;74(5):433–8. doi: 10.1016/j.jpsychores.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Echouffo-Tcheugui JB, Batty GD, Kivimäki M, Kengne AP. Risk models to predict hypertension: a systematic review. PLoS One. 2013 Jul 5;8(7):e67370. doi: 10.1371/journal.pone.0067370. ⍰ . This article provides a review of the available hypertension risk models and scores. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pickering TG, Shimbo D, Haas D. Ambulatory blood pressure monitoring. N Engl J Med. 2006;354:2368–74. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 12.O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013 Sep;31(9):1731–68. doi: 10.1097/HJH.0b013e328363e964. ⍰ . doi: 10.1097/HJH.0b013e328363e964. Presents comprehensive, up-to-date information on all aspects of ambulatory blood pressure monitoring. [DOI] [PubMed] [Google Scholar]
- 13.Pierdomenico SD, Di Nicola M, Esposito AL, et al. Prognostic value of different indices of blood pressure variability in hypertensive patients. Am J Hypertens. 2009;22(8):842–847. doi: 10.1038/ajh.2009.103. [DOI] [PubMed] [Google Scholar]
- 14.Mancia G, Bombelli M, Facchetti R, et al. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009 Aug;54(2):226–32. doi: 10.1161/HYPERTENSIONAHA.109.129882. ⍰ . This article provides some of the leading evidence of the risk of sustained hypertension for people with white-coat and masked hypertension. [DOI] [PubMed] [Google Scholar]
- 15.Ugajin T, Hozawa A, Okhubo T, et al. White-coat hypertension as a risk factor for the development of home hypertension. Arch Intern Med. 2005;165:1541–46. doi: 10.1001/archinte.165.13.1541. [DOI] [PubMed] [Google Scholar]
- 16.Trudel X, Milot A, Brisson C. Persistence and progression of masked hypertension: a 5-year prospective study. Int J Hypertens. 2013;2013:836387. doi: 10.1155/2013/836387. ⍰ . doi: 10.1155/2013/836387. This article examines what happens to blood pressure in people identified with masked hypertension 5 years later. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierdomenico SD, Pannarale G, Rabbia F, et al. Prognostic relevance of masked hypertension in subjects with prehypertension. Am J Hypertens. 2008;21(8):879–83. doi: 10.1038/ajh.2008.196. [DOI] [PubMed] [Google Scholar]
- 18.Viera AJ, Zhu S, Hinderliter AL, Shimbo D, Person SD, Jacobs DR., Jr Diurnal blood pressure pattern and development of prehypertension or hypertension in young adults: the CARDIA study. J Am Soc Hypertens. 2011;5(1):48–55. doi: 10.1016/j.jash.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y, Wang J. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013;61:278–83. doi: 10.1161/HYPERTENSIONAHA.111.00217. [DOI] [PubMed] [Google Scholar]
- 20.Tsioufis C, Andrikou I, Thomopoulos C, Syrseloudis D, Stergiou G, Stefanadis C. Increased nighttime blood pressure or nondipping profile for prediction of cardiovascular outcomes. J Hum Hypertens. 2011;25:281–293. doi: 10.1038/jhh.2010.113. [DOI] [PubMed] [Google Scholar]
- 21.Mena L, Pintos S, Queipo NV, JAizpúrua JA, Maestre G, Sulbarán T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23(3):505–511. doi: 10.1097/01.hjh.0000160205.81652.5a. T. [DOI] [PubMed] [Google Scholar]
- 22.Stolarz-Skrzypek K, Thijs L, Li Y, et al. Short-term blood pressure variability in relation to outcome in the International Database of Ambulatory blood pressure in relation to Cardiovascular Outcome (IDACO) Acta Cardiol. 2011 Dec;66(6):701–706. doi: 10.1080/ac.66.6.2136952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamaguchi Y, Wada M, Sato H, et al. Impact of Ambulatory Blood Pressure Variability on Cerebral Small Vessel Disease Progression and Cognitive Decline in Community-Based Elderly Japanese. Am J Hypertens. 2014 Mar 20; doi: 10.1093/ajh/hpu045. ⍰ . [Epub ahead of print] A recent study of the association of ambulatory blood pressure variability with cognitive outcomes. [DOI] [PubMed] [Google Scholar]
- 24.Verberk WJ, Kessesl AG, de Leeuw PW. Prevalence, causes, and consequences of masked hypertension: a meta-analysis. Am J Hypertens. 2008;21:969–975. doi: 10.1038/ajh.2008.221. [DOI] [PubMed] [Google Scholar]
- 25.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–2198. doi: 10.1097/HJH.0b013e3282ef6185. [DOI] [PubMed] [Google Scholar]
- 26.Brguljan-Hitij J, Thijs L, Li Y, Hansen TW, et al. Risk Stratification by Ambulatory Blood Pressure Monitoring Across JNC Classes of Conventional Blood Pressure. Am J Hypertens. 2014 Feb 26; doi: 10.1093/ajh/hpu002. ⍰ . on behalf of the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcome Investigators. [Epub ahead of print] Uses the large IDACO database to examine outcomes across different BP phenotypes. [DOI] [PubMed] [Google Scholar]
- 27.Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of "masked" hypertension and "white-coat" hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005 Aug 2;46(3):508–15. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 28.Viera AJ, Lin FC, Tuttle LA, Olsson E, Stankevitz K, Girdler SS, Klein JL, Hinderliter AL. Reproducibility of masked hypertension among adults 30 years or older. Blood Press Monit. 2014 May 16; doi: 10.1097/MBP.0000000000000054. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891. doi:10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]