Abstract
Autosomal recessive polycystic kidney disease (ARPKD) is an important cause of chronic kidney disease in children. The care of ARPKD patients has traditionally been the realm of pediatric nephrologists; however, the disease has multisystem effects, and a comprehensive care strategy often requires a multidisciplinary team. Most notably, ARPKD patients have congenital hepatic fibrosis, which can lead to portal hypertension, requiring close follow-up by pediatric gastroenterologists. In severely affected infants, the diagnosis is often first suspected by obstetricians detecting enlarged, echogenic kidneys and oligohydramnios on prenatal ultrasounds. Neonatologists are central to the care of these infants, who may have respiratory compromise due to pulmonary hypoplasia and massively enlarged kidneys. Surgical considerations can include the possibility of nephrectomy to relieve mass effect, placement of dialysis access, and kidney and/or liver transplantation. Families of patients with ARPKD also face decisions regarding genetic testing of affected children, testing of asymptomatic siblings, or consideration of preimplantation genetic diagnosis for future pregnancies. They may therefore interface with genetic counselors, geneticists, and reproductive endocrinologists. Children with ARPKD may also be at risk for neurocognitive dysfunction and may require neuropsychological referral. The care of patients and families affected by ARPKD is therefore a multidisciplinary effort, and the general pediatrician can play a central role in this complex web of care. In this review, we outline the spectrum of clinical manifestations of ARPKD and review genetics of the disease, clinical and genetic diagnosis, perinatal management, management of organ-specific complications, and future directions for disease monitoring and potential therapies.
Keywords: polycystic kidney disease, congenital hepatic fibrosis, genetic testing, preimplantation genetic diagnosis, dialysis, kidney transplantation, liver transplantation
Autosomal recessive polycystic kidney disease (ARPKD; MIM 263200) is an important inherited cause of chronic kidney disease (CKD), with an estimated incidence of 1 in 20 000 live births.1 The most typical disease expression occurs in neonates and includes a history of oligohydramnios, massively enlarged kidneys, and the “Potter” sequence with pulmonary hypoplasia that leads to respiratory insufficiency and perinatal death in ∼30% of affected newborns.2–4
Improved survival of infants resulting from advances in neonatal supportive care over recent decades has allowed recognition of a broader spectrum of disease manifestations. In addition, identification of the causative gene, PKHD1, has allowed clinicians to recognize that patients with disparate phenotypes all have defects in the same disease gene.5
The typical renal phenotype of ARPKD consists of enlarged, echogenic kidneys with fusiform dilatation of the collecting ducts. Patients can progress to end-stage renal disease (ESRD) at varying ages.5,6 ARPKD also has important effects on other organ systems. Notably, patients have liver disease consisting of dilated biliary ducts, congenital hepatic fibrosis, and portal hypertension (Caroli syndrome). Systemic hypertension is prevalent and can be severe.5–9 Children with ARPKD may also be at risk for neurocognitive dysfunction.
Families of children with ARPKD also face a number of challenges. As genetic testing technology has advanced, not only do families face decisions regarding testing of a symptomatic child, they must also confront issues such as testing of asymptomatic children and consideration of new reproductive technologies such as preimplantation genetic diagnosis (PGD). Many families will be confronted with decisions regarding dialysis and/or transplantation, kidney, liver, or sometimes both. It is essential that providers caring for these patients be well versed not only in the biology of the disease but also in its psychosocial implications.
In this article, we review the genetic basis of ARPKD, clinical and genetic diagnosis, perinatal management, management of organ-specific and systemic complications, and considerations of dialysis and transplantation and explore future directions for monitoring disease progression and potential therapies.
Genetics of ARPKD
Background of the Gene and Protein
ARPKD is caused by mutations in PKHD1, a large ∼500-kb gene10,11 with a complex splicing pattern12 located on chromosome 6p21.1-p12.
The product of PKHD1, fibrocystin/polyductin (FPC), is a single-membrane spanning protein with multiple isoforms.13 It is expressed predominantly in the kidney (mostly in collecting ducts and thick ascending loops of Henle), liver (in bile duct epithelia), and pancreas.11,13–15 In renal tubular and biliary epithelial cells, FPC localizes to apical membranes, the primary cilia/basal body,13,14,16–19 and mitotic spindle.20
The exact function of FPC remains unclear. However, numerous proteins associated with other hepatorenal fibrocystic diseases (Table 1) also localize to the primary cilia/basal body (Fig 1). This suggests a central role for the primary cilium in development and maintenance of renal tubular architecture and has led some to characterize these disorders collectively as “ciliopathies.”21–26 Through its interactions with the autosomal dominant polycystic kidney disease (ADPKD) protein polycystin-2,27–29 FPC may form part of a common signaling pathway that also includes polycystin-1.30–32
TABLE 1.
Hepatorenal Fibrocystic Diseases: Summary of Genetics and Clinical Features
| Disease | Gene(s) | Renal Disease | Hepatic Disease | Associated Features |
|---|---|---|---|---|
| ARPKD | PKHD1 | Collecting duct dilatation | CHF; Caroli disease | Growth retardation |
| ADPKD | PKD1, PKD2 | Cysts along entire nephron | Biliary cysts; CHF | Minimal in children |
| NPHP | NPHP1–NPHP15 | Cysts at the corticomedullary junction | CHF | Tapetoretinal degeneration, situs inversus |
| Joubert syndrome | JBTS1–JBTS20 | Cystic dysplasia; NPHP | CHF; Caroli disease | Cerebellar vermis hypo/aplasia with episodic hyperpnea, abnormal eye movements, intellectual disability |
| Bardet-Biedl syndrome | BBS1–BBS15 | Cystic dysplasia; NPHP | CHF | Retinal degeneration, obesity, postaxial polydactyly, hypogonadism in males, intellectual disability |
| Meckel-Gruber syndrome | MKS1–MKS10 | Cystic dysplasia | CHF | Occipital encephalocele, polydactyly |
| Oral-facial-digital syndrome, type I | OFD1 | Glomerular cysts | CHF (rare) | Malformations of the face, oral cavity, and digits |
| Glomerulocystic disease | PKD1, TCF2, UMOD | Enlarged; normal or hypoplastic kidneys | CHF (with PKD1 mutations) | Diabetes, hyperuricemia |
| Jeune syndrome (asphyxiating thoracic dystrophy) | IFT80 (ATD2) | Cystic dysplasia | CHF; Caroli disease | Short stature, skeletal dysplasia, small thorax, short limbs, polydactyly, hypoplastic pelvis |
| DYNC2H1 (ADT3) | ||||
| ADT1, ADT4, ADT5 | ||||
| Renal-hepatic-pancreatic dysplasia (Ivemark II syndrome) | NPHP3 | Cystic dysplasia | Intrahepatic biliary dysgenesis | Pancreatic cysts, dysplasia, and/or fibrosis; splenic abnormalities; situs inversus |
| Zellweger syndrome | PEX1-3, 5-6, 10-11, 13, 14, 16, 19, 26 | Renal cortical microcysts | Intrahepatic biliary dysgenesis | Hypotonia, seizures, agenesis/hypoplasia of corpus callosum, characteristic facies, skeletal abnormalities, neonatal death |
Adapted with permission from Somlo and Guay-Woodford.143 CHF, congenital hepatic fibrosis; NPHP, nephronophthisis.
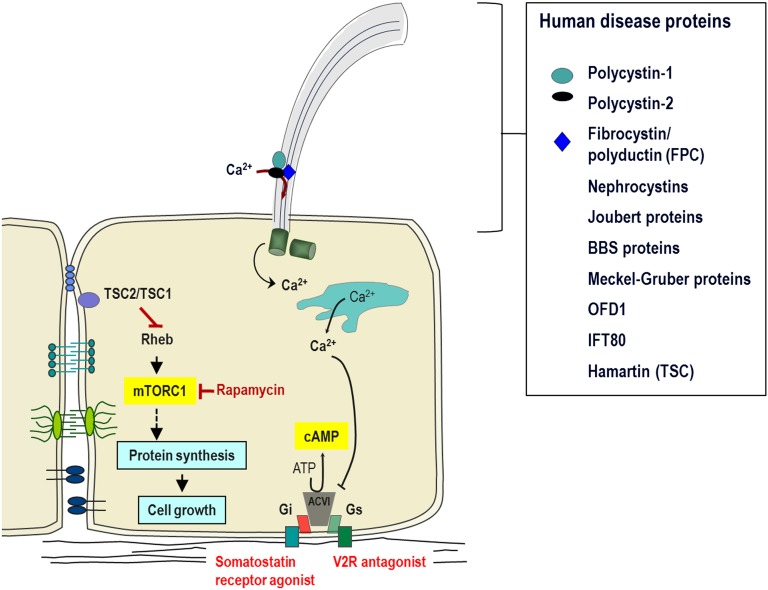
FIGURE 1.
The primary cilium and cystoproteins. The cilium concentrates and organizes a number of channels, receptors, and effectors, such as transcription factors and proteolytic fragments of cystoproteins. It therefore plays a critical role in transmitting information regarding the external milieu back into the cell and ultimately in regulating cellular and tubular differentiation and homeostasis. Cyst formation is characterized by deregulation of the balance between cell proliferation and differentiation. Cilia appear to play a role in maintaining this balance through sensing the extracellular milieu, responding to mechanical cues, and modulating different signaling cascades. Ciliary dysfunction contributes to increased intracellular accumulation of cAMP and activation of mammalian target of rapamycin (mTOR), features common to cystic epithelia in human and rodent models of renal cystic disease. Numerous groups have demonstrated that almost all cystoproteins, including polycystins; FPC; the nephrocystins; the Bardet Biedl syndrome (BBS) proteins; oral-facial-digital syndrome, type I (OFD1) protein; and the tuberous sclerosis type I (TSC1) protein Hamartin; all of these localize to the cilia/centrosome complex, providing compelling evidence that this complex is critical in the pathogenesis of renal cystic disease. mTORC1, mammalian target of rapamycin complex 1; V2R, V2 receptor.
Human Mutations
ARPKD mutations have been identified along the entire length of the PKHD1 gene, and multiple mutation types have been described as pathogenic. To date, >300 pathogenic mutations have been cataloged in the ARPKD Mutation Database (http://www.humgen.rwth-aachen.de),33 of which approximately half are missense changes. The most common mutation overall is a missense mutation in exon 3, c.107C>T (p.Thr36Met), which accounts for ∼20% of all mutated alleles.34 Aside from this mutation, which has been observed in a large number of unrelated patients,35 there do not appear to be any mutational hotspots. Indeed, a large proportion of mutations are unique to a single pedigree.35,36
Genotype-Phenotype Correlations
Multiple studies have attempted to elucidate genotype-phenotype correlations in ARPKD. Given the diversity of PKHD1 mutations, most patients are compound heterozygotes, that is they carry 2 different mutant alleles. The functional effect of any particular mutant allele can therefore be difficult to discern.
Nevertheless, some broad themes have emerged from these studies. Notably, patients with 2 truncating mutations typically have a severe phenotype leading to perinatal demise.35,37–40 However, not all missense mutations lead to a more benign outcome; indeed, a number of missense mutations result in severe phenotypes when present with a truncating mutation or in homozygous form.6,37,41
Numerous groups have attempted to categorize sequence variations based on likelihood of pathogenicity,6,37,42–44 many of which are cataloged in the ARPKD Mutation Database.33 However, because many patients will be found to have novel PKHD1 variants, interpretation of genetic testing results can be challenging.
Genetic modifiers likely also play a significant role in disease expression. This is illustrated by the presence of significant phenotypic variability in a subset of families; for example, in a study of 126 unrelated families, 20 sibships showed widely discordant phenotypes (perinatal lethality in 1 sibling and survival into childhood in the other).6
Genetic Testing
Mapping of the ARPKD locus to chromosome 6p21.1-p1245–47 in the mid-1990s allowed the use of haplotype (linkage) analysis for genetic confirmation of the diagnosis, including prenatally,1 provided DNA from a previously affected child and the parents was available.
Identification of PKHD1 has since allowed diagnosis by direct sequencing. In various cohort studies,5,10,11,34,35,37–39,42,43,48 mutation detection rates have ranged from 42% to 87% of tested alleles, and ∼95% of patients could be found to have at least 1 PKHD1 mutation. Generally, mutation detection rates are higher for patients with severe early-onset disease because they are more likely to have truncating mutations that are easier to detect.
A number of laboratories offer clinical genetic testing for ARPKD. These are summarized on the GeneTests Web site (www.genetests.org), and in the National Institutes of Health Genetic Testing Registry (http://www.ncbi.nlm.nih.gov/gtr). Most laboratories offer direct sequencing of the entire coding region, with expected mutation detection rates similar to recent studies of ∼80%. However, direct sequencing cannot detect all mutations (e.g., those in noncoding exons or in promoter or regulatory regions). Some laboratories also offer multiplex ligation-dependent probe amplification to detect large deletions or genomic rearrangements.49 In families with >1 affected child, haplotype analysis remains a valuable tool when only 1 or no PKHD1 mutations have been identified.50
Another challenge in establishing a molecular diagnosis is that several other diseases can mimic the clinical presentation of ARPKD. For example, patients with mutations in the ADPKD genes, PKD1 and PKD2, can present with early-onset renal cystic disease indistinguishable from ARPKD.51–53 In some cases, this can occur in families with a mild phenotype in previous generations51; in others, ARPKD-like phenotypes have been described when 2 incompletely penetrant PKD1/2 alleles are inherited in trans52,53 or when a PKD1/2 mutation is inherited in trans with a mutation in another cystic kidney disease gene such as HNF1β.53 In addition, it must be noted that the most common cause of hyperechoic fetal kidneys is reported to be HNF1β-related disease.54 A number of the other hepatorenal fibrocystic diseases listed in Table 1 can also have clinical manifestations that overlap with ARPKD.
Thus, mutational analysis of PKHD1 using current single-gene testing methodologies should not be considered as a first-line diagnostic approach for infants and children presenting with an ARPKD-like phenotype. It is expensive and potentially confounded by the existence of phenocopy disorders. Moreover, the high frequency of missense mutations makes pathogenicity predictions for single nucleotide variants challenging, and particular caution is required when only novel or rare missense changes are detected. The one clear exception to this guidance is in the context of planned PGD in which putative PKHD1 mutations transmitted from the mother and father, respectively, must be prospectively identified.
The need for the somewhat cumbersome single-gene testing approach may soon be obviated with advances in next-generation genetic sequencing. Using a massively parallel sequencing approach, it is now possible to evaluate dozens of genes of interest simultaneously in a single test. This will likely prove to be a particularly powerful approach for patients with cystic kidneys in whom the differential diagnosis can be broad.55
Perinatal Considerations
Prenatal Diagnosis of ARPKD
ARPKD is often first suspected based on routine prenatal ultrasound. Suggestive fetal features include symmetrically enlarged, echogenic kidneys (due to multiple microscopic cysts) with loss of corticomedullary differentiation due to medullary hyperechogenicity.56 Discrete cysts are sometimes observed.57 Oligohydramnios may be present due to poor fetal urine output.1,56 Many other hepatorenal fibrocystic diseases can have similar sonographic findings, however, so a definitive diagnosis is difficult based on imaging alone unless previous children have had a confirmed diagnosis of ARPKD. ADPKD can often be distinguished from ARPKD by the finding of increased corticomedullary differentiation in ADPKD (due to cortical hyperechogenicity with a relatively hypoechogenic medulla).58 It is important to note, however, that normal sonographic findings do not exclude a diagnosis of ARPKD because abnormalities may not be seen until late in the second trimester (or beyond), even in infants who later manifest a severe phenotype at birth.1,56,59 In addition, the presence or absence of oligohydramnios does not always correlate with the degree of pulmonary insufficiency.56
Prenatal genetic testing can be performed by using haplotype analysis1,50 or PKHD1 sequencing as previously described.40,60,61 However, as discussed earlier, providing clear prognostic information based on sequencing results remains a challenge; although the presence of 2 truncating mutations is generally incompatible with survival, clinical consequences of other mutation types can be difficult to predict. Next-generation sequencing methods will likely also prove useful to differentiate ARPKD from other phenotypically similar entities.55
PGD
In families with a previous child severely affected by ARPKD, PGD represents a valuable alternative to prenatal diagnosis.62 To carry out PGD, the transmitted PKHD1 mutations must be prospectively identified. Then, a couple must undergo in vitro fertilization; the resulting embryo is biopsied, with removal of 1 or 2 blastomeres for genetic testing.63 Two groups have recently reported the birth of healthy infants after PGD in families at risk for ARPKD.62,64
Postnatal Management
The estimated perinatal mortality rate in ARPKD patients is ∼30%, primarily due to respiratory compromise. One-year survival rates of 92% to 95%6,9 have been reported in patients who survive the first month of life.
Although pulmonary hypoplasia is a major cause of respiratory compromise,65,66 an additional impediment is the presence of massively enlarged kidneys limiting diaphragmatic excursion. The enlarged kidneys may also interfere with nutrition due to gastrointestinal tract compression. The proportion of infants requiring mechanical ventilation is not well established; in one cohort, it was required in 41% of neonates.9 Pneumothoraces also appear to be a relatively common complication.8,67
Aggressive management strategies for infants with severe ARPKD have been described, including unilateral68–70 or bilateral67,71,72 nephrectomy to improve ventilation and nutrition. The optimal approach, however, is not well established given that the evidence base consists only of limited case reports and case series. Several of these reports have described improvements in nutrition after either unilateral68,69 or bilateral67 nephrectomy. Potential respiratory benefits of nephrectomy are less clear, particularly given the significant surgical risks in infants with severe respiratory compromise.70,72 Although some authors have reported successful weaning of respiratory support after nephrectomy,67,71,72 some infants with massively enlarged kidneys can be weaned from mechanical ventilation even without nephrectomy.68,69 In addition, morbidity associated with the earlier need for renal replacement therapy after nephrectomy must be carefully considered. Therefore, decisions surrounding possible nephrectomy for infants with severe ARPKD must be highly individualized.
Despite advances in neonatal supportive care including respiratory support and dialysis, the prognosis of infants with severe ARPKD is often uncertain. Parents and care providers may need to make difficult decisions surrounding possible limitation or withdrawal of care. Palliative care providers and/or medical ethicists can be invaluable in facilitating the decision-making process.
Renal Manifestations
Most ARPKD patients progress to ESRD, but the age at onset is highly variable. The overall renal survival rate in one large cohort of neonatal survivors was 86% at age 5 years and decreased to 42% by 20 years of age.6 However, age at ESRD onset appears to depend on age at initial presentation. In one cohort, 25% of patients who presented in the perinatal period required renal replacement therapy by 11 years. In contrast, among those who presented after the perinatal period, the age at which 25% of patients required renal replacement therapy was 32 years.44 Similarly, in another cohort, renal survival rate 20 years after diagnosis was 36% in patients diagnosed before 1 year of age but was 80% in those diagnosed at age 1 to 20 years.5
Systemic hypertension is another important cause of morbidity in children with ARPKD, and its onset often precedes a decline in glomerular filtration rate.3,7 The prevalence of hypertension in various cohorts has been reported to range from 55% to 75%.2,3,7–9,73,74 Interestingly, some authors have noted that hypertension can sometimes normalize during the course of the disease.75,76
The mechanism underlying hypertension in ARPKD is unclear. Some studies have suggested a low-renin mechanism,3,9 possibly due to dysregulation in sodium absorption in the structurally abnormal collecting ducts. However, other studies suggest a role for renin-angiotensin-aldosterone system (RAS) activation. A study in the PCK rat model reported a significant increase in intrarenal, but not systemic, RAS activation.77 This finding may explain why previous studies did not detect increased plasma renin levels.3,78
Hypertension in children with ARPKD is often severe enough to require multiagent therapy.8,9 As in other causes of CKD, angiotensin converting enzyme inhibitors and angiotensin receptor blockers are therapeutic mainstays and may be particularly helpful given data suggesting intrarenal RAS activation.77 However, there are no studies to determine whether therapy with these agents can slow disease progression in ARPKD. Strict blood pressure control has been shown to slow CKD progression in children with other diseases79; thus it seems reasonable to also target blood pressures <90th percentile for children with ARPKD.
Hyponatremia has been reported to be common in early infancy; it was reported in 27% of patients in one cohort9 and in 79% of infants in another3 and may be due to an inability to maximally dilute the urine.3 However, other cohorts have reported much lower prevalences of hyponatremia.7,8
Children with ARPKD appear to be at higher risk for urinary tract infections, possibly due to urinary stasis within the cystic, dilated collecting ducts. Urinary tract infections have been reported at rates of ∼20% to 50% in various cohorts and are more common in girls.7–9,80
Renal calcifications have also been reported to be common in older children with ARPKD5,81 and may be related to hypocitraturia and a defect in urine acidification due to renal failure.81
Hepatobiliary Manifestations
Patients with ARPKD invariably have a developmental biliary defect termed the ductal plate malformation.82 The abnormal intrahepatic bile ducts become progressively dilated and sometimes develop overt cysts. Progressive portal tract fibrosis can lead to portal hypertension and associated complications of hypersplenism and varices.83
Although histologic biliary abnormalities are a universal feature, clinical expression varies widely. In 1 cohort, liver-related symptoms such as splenomegaly, cholangitis, or thrombocytopenia due to hypersplenism were presenting features in 26% of patients.84 Platelet counts were found to correlate well with spleen volume in this cohort.84 Liver transaminases are generally normal, and a fraction of patients have mild abnormalities in serum alkaline phosphatase, γ-glutamyltransferase, albumin, bilirubin, or prothrombin time.7,84
In various cohorts, the proportion of ARPKD patients with imaging findings of liver disease has ranged from 45% to 90%.2,7,84 However, relatively fewer develop serious clinical complications of portal hypertension. Occurrence of bleeding esophageal varices and/or the need for portosystemic shunting has ranged from 10% to 40% of patients in various reports.2,5,8,75,84 Ascending cholangitis is another important complication and is a leading cause of morbidity and mortality in ARPKD patients particularly after kidney and/or liver transplantation.85
In one cohort, about 7% of long-term survivors were reported to require liver transplantation, with primary indications being significant portal hypertension or recurrent cholangitis.9
The relationship between renal and hepatic disease severity in ARPKD is unclear. One study reported significant correlation between degree of renal dysfunction and portal hypertension.6 However, subsequent studies have documented no correlation between renal and hepatic disease severity.9,75 It appears that a subset of patients with ARPKD presenting later in life can have a liver-predominant phenotype with few or no manifestations of kidney disease.5
Radiologic Diagnosis and Monitoring
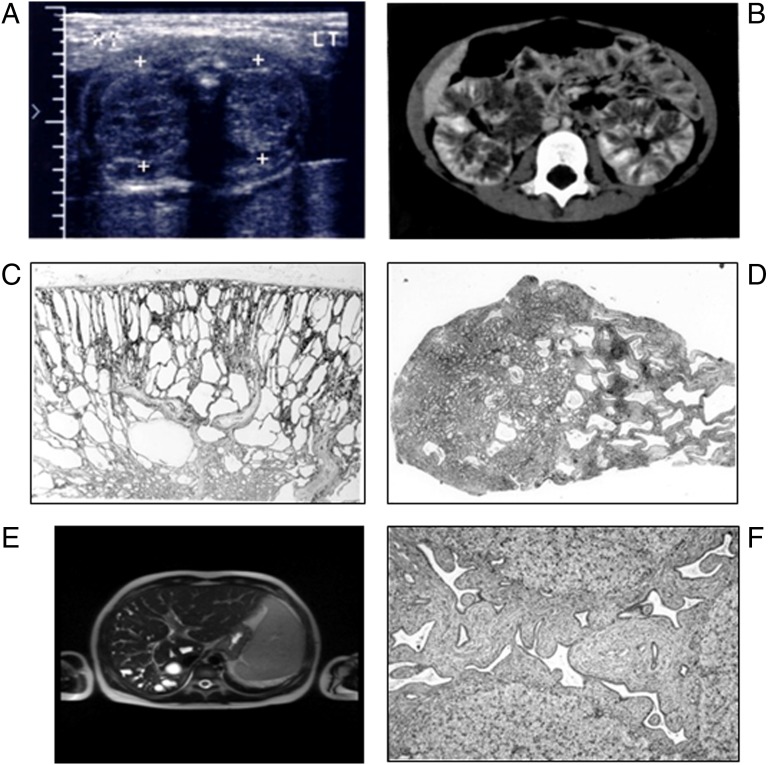
Although renal ultrasound is sometimes used to monitor children with ARPKD, the prognostic value of imaging findings is unclear (Fig 2). Unlike in ADPKD, in which decline in renal function clearly correlates with increasing total kidney and cyst volume,86,87 there is no clear relationship between kidney size and function in ARPKD. There was no correlation between kidney length and serum creatinine in one large cohort.7 Another study found a weak inverse correlation between kidney function and volume in ARPKD patients, but there was marked variability.44 This study also found that patients with cysts limited to the renal medulla fared better than those with cortical and medullary abnormalities.44 It is unclear, however, if these findings represent different stages of disease progression or simply inherent differences in disease expression. Longitudinal studies of ARPKD have shown that kidney size tends to either remain stable or decrease over time.7,88–91
FIGURE 2.
Radiologic findings and pathologic features associated with ARPKD. A, Neonatal sonography with nephromegaly and increased echogenicity. B, Contrast-enhanced computed tomography in a symptomatic 4-year-old girl reveals a striated nephrogram and prolonged corticomedullary contrast retention. C, Light microscopy: ARPKD kidney from a 1-year-old child reveals discrete medullary cysts and dilated collecting ducts, hematoxylin and eosin (H&E) ×10. D, Light microscopy: later-onset ARPKD kidney with prominent medullary ductal ectasia, H&E ×10. E, Coronal heavily T2-weighted image of the abdomen in an 8-year-old boy reveals marked cystic and fusiform dilatation of the intrahepatic biliary system. F, Light microscopy: congenital hepatic fibrosis with extensive fibrosis of the portal area; ectatic, tortuous bile ducts; and hypoplasia of the portal vein, H&E ×40.
Ultrasound can also be used to monitor sequelae of portal hypertension such as splenomegaly, presence of collateral vessels, and reversal of portal flow. However, these may be late findings in ARPKD and may not reflect underlying pathology such as progressive hepatic fibrosis.
MRI has been used for kidney and liver imaging in several studies44,84,92,93; however, MRI has not come into routine clinical use because of the unclear prognostic significance of findings. Transient elastography (FibroScan) is a method of assessing liver fibrosis that has been validated in other disease processes94 and has been studied in children with ARPKD.95 However, additional studies are needed to assess the clinical utility of this technique in this patient cohort.
Additional studies of new imaging modalities are clearly needed. New disease monitoring tools not only could provide useful prognostic information but also could help to define reliable biomarkers to evaluate the efficacy of any future potential therapies.
Dialysis and Transplantation
As discussed previously, some infants require dialysis in the newborn period after bilateral nephrectomy.67,71,72 Given the technical challenges of hemodialysis in young infants, peritoneal dialysis (PD) is generally preferred. However, PD in infants with ARPKD can be complicated by peritoneal leak caused by peritoneal disruption during nephrectomy and poor wound healing due to suboptimal nutrition.67,96
In patients who do not undergo nephrectomy in infancy, standard care for progressive CKD is generally adopted, including referral for dialysis or transplantation as indicated. There are, however, some unique considerations in children with ARPKD with significant dual-organ involvement. A subset of patients can require both kidney and liver transplantation, either simultaneously or sequentially. Decisions regarding timing and sequence of organ transplantation can be difficult, and Telega et al85 recently presented a clinical decision framework to help guide clinicians.
Special considerations after isolated kidney transplantation in ARPKD patients include the substantial risk of morbidity and mortality due to cholangitis/sepsis. Some authors have therefore advocated standard use of posttransplant antibiotic prophylaxis.97,98 Others have suggested earlier consideration of liver transplantation (LT) in ARPKD patients with severe liver disease who are being evaluated for kidney transplantation, even if they may not otherwise meet criteria for LT-based liver disease severity alone.85,98–100 In patients with liver-predominant disease who first undergo LT, acceleration of kidney disease progression is also a concern.101 Currently, the only guidelines regarding listing for combined kidney-liver transplantation (CKLT) are in the context of end-stage liver disease due to hepatocellular dysfunction, for which listing for CKLT is recommended when estimated glomerular filtration rate is ≤30 mL/min/1.73m2.101,102 That said, the corollary of these data for patients with ARPKD who typically have biliary-related disease is unclear. Studies in patients with ARPKD who underwent CKLT have reported patient survival rates of 70% to 100%.99,103
Systemic Manifestations
Growth Impairment
Growth impairment has been reported in children with ARPKD; in one cohort, growth delay was observed in ∼30% of patients.9 Some authors have postulated that growth retardation in ARPKD seems out of proportion to the degree of renal dysfunction, raising the question of whether there are disease-specific influences on growth.104 However, others have reported that growth impairment is indeed correlated with decreased renal function.105 Like children with other forms of CKD, children with ARPKD can successfully be treated with growth hormone.104
Neurocognitive Issues
Behavioral and neurocognitive difficulties have been recognized as important comorbidities in children with other forms of CKD,106 as well as in children with hypertension, both with107 and without108–111 coexisting CKD. Given that children with ARPKD often have both CKD and severe hypertension during critical early years of neurodevelopment, they may be at particular risk for worse neurocognitive outcomes. A study of neurocognitive function in children with ARPKD was recently completed.112 This study examined results of neurocognitive testing of ARPKD patients in the Chronic Kidney Disease in Children cohort study, which includes children with mild-to-moderate CKD due to a wide range of diagnoses. Children with ARPKD were compared with a control group with renal aplasia/hypoplasia/dysplasia, matched based on kidney function, age at diagnosis, and age at study entry. In both ARPKD and control groups, scores in all domains tested were within average range, but a larger than expected proportion of children demonstrated risk for neurocognitive dysfunction (scores worse than 1 SD below the mean). Although this study did not find evidence of disease-specific neurocognitive defects in this subset of ARPKD patients with mild-to-moderate CKD, these findings may not be generalizable to children with more severe disease manifestations. Additional studies are therefore needed in ARPKD patients with a broader range of CKD and other morbidities to fully characterize their neurocognitive and behavioral functioning. However, given the presence of multiple risk factors for neurocognitive dysfunction, clinicians should maintain a high index of suspicion for neurocognitive problems and provide referrals as appropriate.
Psychosocial Considerations
The psychosocial impact of ARPKD on patients, families, and care providers can be far-reaching. When a diagnosis of ARPKD is suspected based on prenatal ultrasound, families face many uncertainties. Families may choose to pursue genetic testing to help guide a decision about possible pregnancy termination. Yet, as discussed previously, genetic results may not provide definitive prognostic information. Care providers must be willing to help guide families through this difficult decision-making process and to provide appropriate referrals to genetic counselors, social workers, and other sources of psychosocial support.
Families may also need extra support if they are considering PGD for a future pregnancy. This can be a physically challenging procedure and can be especially emotion-laden for families who have previously faced the devastating loss of child with severe ARPKD.
Parents may also face the decision on whether to consider testing to determine the status of asymptomatic siblings. Given that there are currently no known therapies to prevent disease progression, no consensus exists on whether testing should be offered to siblings. Providers may be called on for advice as families navigate these decisions.
Impairments in health-related quality of life have been well documented in children with CKD113 and ESRD.114 Given that children with ARPKD may also be faced with additional stressors such as liver disease, they are likely to experience similarly decreased health-related quality of life. Care from a multidisciplinary team, including child life specialists and psychologists, can be particularly helpful.
Patient advocacy organizations can be extremely valuable sources of support and information for patients and families dealing with ARPKD; these include the PKD Foundation (www.pkdcure.org) and the ARPKD/CHF Alliance (www.arpkdchf.org).
Future Directions and Translational Considerations
To date, specific disease-targeting therapies to slow progression of ARPKD have remained elusive. However, a number of preclinical studies have defined several potential molecular targets for therapeutic intervention (Fig 1).
Studies in human ARPKD tissues have shown activation of the mammalian target of rapamycin (mTOR) pathway,115,116 suggesting a potential therapeutic role for mTOR inhibitors such as sirolimus. However, in the PCK rat model, sirolimus treatment did not slow disease progression.117 Studies of mTOR inhibitors in adult ADPKD patients have been disappointing118,119 despite promising results in animal studies.120–124 Thus, it seems unlikely that the current generation of mTOR inhibitors will prove effective in ARPKD.
Cyclic adenosine monophosphate (cAMP) signaling has been shown to be upregulated in ADPKD and ARPKD renal epithelia.125–130 Stimulation of the vasopressin V2 receptor (V2R) increases cAMP production,131 making V2R antagonists such as tolvaptan appealing as potential therapies. In the PCK rat model, V2R antagonists appear to slow renal disease progression.132 Additional evidence for the role of V2R signaling in ARPKD comes from experiments in which PCK rats were crossed with vasopressin knockout rats to generate double mutant progeny with varying levels of circulating vasopressin.133 PCK rats lacking vasopressin showed lower renal cAMP activity and almost complete inhibition of cystogenesis. Although tolvaptan has been studied in adults with ADPKD,134 there have been no studies in human ARPKD.
Somatostatin analogs have also been studied to reduce cAMP activation in PKD. A recent study of these analogs in the PCK rat showed reduced renal and hepatic cyst formation, with pasireotide showing greater benefit than octreotide.135 Somatostatin analogs have been studied in adults with ADPKD,136 but there are no published studies in human ARPKD.
The epidermal growth factor receptor (EGFR) axis may also play a role in cyst development in ARPKD and ADPKD.137 Inhibition of the EGFR axis has improved biliary and renal abnormalities in various murine models of ARPKD.138–141 Therapies directed at downstream targets of both the cAMP and EGFR pathways, such as Src, may prove especially helpful; a study of Src inhibition in ARPKD mice showed improvement in both biliary and renal abnormalities.142
The ultimate goal of these preclinical studies is, of course, to translate knowledge of disease mechanisms into effective therapy. However, the ability to track disease response is predicated on having defined end points, and in the case of animal studies, this has generally been serial histology. Human studies are currently hampered by the lack of defined imaging biomarkers to meaningfully track disease progression. It is therefore imperative that ongoing research efforts focus on developing reliable noninvasive biomarkers to be able to monitor the effectiveness of potential therapies.
Conclusions
ARPKD is a multifaceted genetic disorder that requires expert interdisciplinary management. Much has been learned in recent decades about the genetics and pathophysiology of this disorder, and the survival of patients has been improved by advances in supportive therapy, dialysis, and transplantation. However, many challenges remain in our understanding of the disease and in the care of affected patients. Advances in elucidating the function of the FPC protein will help to define additional therapeutic targets. Improvements in technologies for noninvasive disease monitoring will be invaluable in providing predictive/prognostic information and gauging the efficacy of any future potential therapies. The ultimate goal is to identify disease-specific therapies to stop or even reverse the inexorable progression of ARPKD-related morbidities.
Glossary
- ADPKD
autosomal dominant polycystic kidney disease
- ARPKD
autosomal recessive polycystic kidney disease
- cAMP
cyclic adenosine monophosphate
- CKD
chronic kidney disease
- CLKT
combined kidney-liver transplantation
- EGFR
epidermal growth factor receptor
- ESRD
end-stage renal disease
- FPC
fibrocystin/polyductin
- LT
liver transplantation
- mTOR
mammalian target of rapamycin
- PGD
preimplantation genetic diagnosis
- RAS
renin-angiotensin-aldosterone system
- V2R
vasopressin V2 receptor
Footnotes
Dr Hartung conceptualized the article, interpreted the data, and drafted and revised the article; Dr Guay-Woodford provided guidance with the content of the article and critically reviewed and revised the article; and both authors approved the final article as submitted.
FINANCIAL DISCLOSURE: Dr Guay-Woodford is a paid consultant for Otsuka Pharmaceuticals; and Dr Hartung has indicated she has no financial relationships relevant to this article to disclose.
FUNDING: Dr Hartung is supported by the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under award KL2TR000139. The content is solely the responsibility of the authors and does not necessarily represent the official view of NCATS or the NIH. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Zerres K, Mücher G, Becker J, et al. Prenatal diagnosis of autosomal recessive polycystic kidney disease (ARPKD): molecular genetics, clinical experience, and fetal morphology. Am J Med Genet. 1998;76(2):137–144 [PubMed] [Google Scholar]
- 2.Roy S, Dillon MJ, Trompeter RS, Barratt TM. Autosomal recessive polycystic kidney disease: long-term outcome of neonatal survivors. Pediatr Nephrol. 1997;11(3):302–306 [DOI] [PubMed] [Google Scholar]
- 3.Kaplan BS, Fay J, Shah V, Dillon MJ, Barratt TM. Autosomal recessive polycystic kidney disease. Pediatr Nephrol. 1989;3(1):43–49 [DOI] [PubMed] [Google Scholar]
- 4.Kääriäinen H, Jääskeläinen J, Kivisaari L, Koskimies O, Norio R. Dominant and recessive polycystic kidney disease in children: classification by intravenous pyelography, ultrasound, and computed tomography. Pediatr Radiol. 1988;18(1):45–50 [DOI] [PubMed] [Google Scholar]
- 5.Adeva M, El-Youssef M, Rossetti S, et al. Clinical and molecular characterization defines a broadened spectrum of autosomal recessive polycystic kidney disease (ARPKD). Medicine (Baltimore). 2006;85(1):1–21 doi:10.1097/01.md.0000200165.90373.9a [DOI] [PubMed] [Google Scholar]
- 6.Bergmann C, Senderek J, Windelen E, et al. APN (Arbeitsgemeinschaft für Pädiatrische Nephrologie) . Clinical consequences of PKHD1 mutations in 164 patients with autosomal-recessive polycystic kidney disease (ARPKD). Kidney Int. 2005;67(3):829–848 doi:10.1111/j.1523-1755.2005.00148.x [DOI] [PubMed] [Google Scholar]
- 7.Zerres K, Rudnik-Schoneborn S, Deget F, et al. Autosomal recessive polycystic kidney disease in 115 children: clinical presentation, course and influence of gender. Arbeitsgemeinschaft fur Padiatrische, Nephrologie. Acta Paediatr. 1996;85(4):437–445 [DOI] [PubMed]
- 8.Capisonda R, Phan V, Traubuci J, Daneman A, Balfe JW, Guay-Woodford LM. Autosomal recessive polycystic kidney disease: outcomes from a single-center experience. Pediatr Nephrol. 2003;18(2):119–126 doi:10.1007/s00467-002-1021-0 [DOI] [PubMed] [Google Scholar]
- 9.Guay-Woodford LM, Desmond RA. Autosomal recessive polycystic kidney disease: the clinical experience in North America. Pediatrics. 2003;111(5 pt 1):1072–1080 [DOI] [PubMed] [Google Scholar]
- 10.Onuchic LF, Furu L, Nagasawa Y, et al. PKHD1, the polycystic kidney and hepatic disease 1 gene, encodes a novel large protein containing multiple immunoglobulin-like plexin-transcription-factor domains and parallel beta-helix 1 repeats. Am J Hum Genet. 2002;70(5):1305–1317 doi:10.1086/340448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ward CJ, Hogan MC, Rossetti S, et al. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet. 2002;30(3):259–269 doi:10.1038/ng833 [DOI] [PubMed] [Google Scholar]
- 12.Bergmann C, Frank V, Küpper F, Schmidt C, Senderek J, Zerres K. Functional analysis of PKHD1 splicing in autosomal recessive polycystic kidney disease. J Hum Genet. 2006;51(9):788–793 doi:10.1007/s10038-006-0022-4 [DOI] [PubMed] [Google Scholar]
- 13.Menezes LFC, Cai Y, Nagasawa Y, et al. Polyductin, the PKHD1 gene product, comprises isoforms expressed in plasma membrane, primary cilium, and cytoplasm. Kidney Int. 2004;66(4):1345–1355 doi:10.1111/j.1523-1755.2004.00844.x [DOI] [PubMed] [Google Scholar]
- 14.Zhang MZ, Mai W, Li C, et al. PKHD1 protein encoded by the gene for autosomal recessive polycystic kidney disease associates with basal bodies and primary cilia in renal epithelial cells. Proc Natl Acad Sci USA. 2004;101(8):2311–2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagasawa Y, Matthiesen S, Onuchic LF, et al. Identification and characterization of Pkhd1, the mouse orthologue of the human ARPKD gene. J Am Soc Nephrol. 2002;13(9):2246–2258 doi:10.1097/01.ASN.0000030392.19694.9D [DOI] [PubMed] [Google Scholar]
- 16.Ward CJ, Yuan D, Masyuk TV, et al. Cellular and subcellular localization of the ARPKD protein; fibrocystin is expressed on primary cilia. Hum Mol Genet. 2003;12(20):2703–2710 doi:10.1093/hmg/ddg274 [DOI] [PubMed] [Google Scholar]
- 17.Wang S, Luo Y, Wilson PD, Witman GB, Zhou J. The autosomal recessive polycystic kidney disease protein is localized to primary cilia, with concentration in the basal body area. J Am Soc Nephrol. 2004;15(3):592–602 doi:10.1097/01.ASN.0000113793.12558.1D [DOI] [PubMed] [Google Scholar]
- 18.Bakeberg JL, Tammachote R, Woollard JR, et al. Epitope-tagged Pkhd1 tracks the processing, secretion, and localization of fibrocystin. J Am Soc Nephrol. 2011;22(12):2266–2277 doi:10.1681/ASN.2010111173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gallagher A-R, Esquivel EL, Briere TS, et al. Biliary and pancreatic dysgenesis in mice harboring a mutation in Pkhd1. Am J Pathol. 2008;172(2):417–429 doi:10.2353/ajpath.2008.070381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang J, Wu M, Wang S, Shah JV, Wilson PD, Zhou J. Polycystic kidney disease protein fibrocystin localizes to the mitotic spindle and regulates spindle bipolarity. Hum Mol Genet. 2010;19(17):3306–3319 doi:10.1093/hmg/ddq233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watnick T, Germino G. From cilia to cyst. Nat Genet. 2003;34(4):355–356 doi:10.1038/ng0803-355 [DOI] [PubMed] [Google Scholar]
- 22.Menezes LF, Germino GG. Polycystic kidney disease, cilia, and planar polarity. Methods Cell Biol. 2009;94(08):273–297 doi:10.1016/S0091-679X(08)94014-0 [DOI] [PubMed] [Google Scholar]
- 23.Kotsis F, Boehlke C, Kuehn EW. The ciliary flow sensor and polycystic kidney disease. Nephrol Dial Transplant. 2013;28(3):518–526 doi:10.1093/ndt/gfs524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pazour GJ. Intraflagellar transport and cilia-dependent renal disease: the ciliary hypothesis of polycystic kidney disease. J Am Soc Nephrol. 2004;15(10):2528–2536 doi:10.1097/01.ASN.0000141055.57643.E0 [DOI] [PubMed] [Google Scholar]
- 25.Yoder BK. Role of primary cilia in the pathogenesis of polycystic kidney disease. J Am Soc Nephrol. 2007;18(5):1381–1388 doi:10.1681/ASN.2006111215 [DOI] [PubMed] [Google Scholar]
- 26.Hildebrandt F, Benzing T, Katsanis N. Ciliopathies. N Engl J Med. 2011;364(16):1533–1543 doi:10.1056/NEJMra1010172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim I, Li C, Liang D, et al. Polycystin-2 expression is regulated by a PC2-binding domain in the intracellular portion of fibrocystin. J Biol Chem. 2008;283(46):31559–31566 doi:10.1074/jbc.M805452200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim I, Fu Y, Hui K, et al. Fibrocystin/polyductin modulates renal tubular formation by regulating polycystin-2 expression and function. J Am Soc Nephrol. 2008;19(3):455–468 doi:10.1681/ASN.2007070770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang S, Zhang J, Nauli SM, et al. Fibrocystin/polyductin, found in the same protein complex with polycystin-2, regulates calcium responses in kidney epithelia. Mol Cell Biol. 2007;27(8):3241–3252 doi:10.1128/MCB.00072-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qian F, Germino FJ, Cai Y, Zhang X, Somlo S, Germino GG. PKD1 interacts with PKD2 through a probable coiled-coil domain. Nat Genet. 1997;16(2):179–183 doi:10.1038/ng0697-179 [DOI] [PubMed] [Google Scholar]
- 31.Tsiokas L, Kim E, Arnould T, Sukhatme VP, Walz G. Homo- and heterodimeric interactions between the gene products of PKD1 and PKD2. Proc Natl Acad Sci USA. 1997;94(13):6965–6970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bertuccio CA, Caplan MJ. Polycystin-1C terminus cleavage and its relation with polycystin-2, two proteins involved in polycystic kidney disease. Medicina (B Aires). 2013;73(2):155–162 [PubMed] [Google Scholar]
- 33.Autosomal Recessive Polycystic Kidney Disease (ARPKD/PKHD1) Mutation Database. Available at: http://www.humgen.rwth-aachen.de. Accessed August 14, 2013
- 34.Bergmann C, Küpper F, Dornia C, Schneider F, Senderek J, Zerres K. Algorithm for efficient PKHD1 mutation screening in autosomal recessive polycystic kidney disease (ARPKD). Hum Mutat. 2005;25(3):225–231 doi:10.1002/humu.20145 [DOI] [PubMed] [Google Scholar]
- 35.Bergmann C, Senderek J, Küpper F, et al. PKHD1 mutations in autosomal recessive polycystic kidney disease (ARPKD). Hum Mutat. 2004;23(5):453–463 doi:10.1002/humu.20029 [DOI] [PubMed] [Google Scholar]
- 36.Rossetti S, Harris PC. Genotype-phenotype correlations in autosomal dominant and autosomal recessive polycystic kidney disease. J Am Soc Nephrol. 2007;18(5):1374–1380 doi:10.1681/ASN.2007010125 [DOI] [PubMed] [Google Scholar]
- 37.Bergmann C, Senderek J, Sedlacek B, et al. Spectrum of mutations in the gene for autosomal recessive polycystic kidney disease (ARPKD/PKHD1). J Am Soc Nephrol. 2003;14(1):76–89 doi:10.1136/jmg.2005.032318 [DOI] [PubMed] [Google Scholar]
- 38.Furu L, Onuchic LF, Gharavi A, et al. Milder presentation of recessive polycystic kidney disease requires presence of amino acid substitution mutations. J Am Soc Nephrol. 2003;14(8):2004–2014 [DOI] [PubMed] [Google Scholar]
- 39.Sharp AM, Messiaen LM, Page G, et al. Comprehensive genomic analysis of PKHD1 mutations in ARPKD cohorts. J Med Genet. 2005;42(4):336–349 doi:10.1136/jmg.2004.024489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bergmann C, Senderek J, Schneider F, et al. PKHD1 mutations in families requesting prenatal diagnosis for autosomal recessive polycystic kidney disease (ARPKD). Hum Mutat. 2004;23(5):487–495 doi:10.1002/humu.20019 [DOI] [PubMed] [Google Scholar]
- 41.Denamur E, Delezoide AL, Alberti C, et al. Société Française de Foetopathologie . Genotype-phenotype correlations in fetuses and neonates with autosomal recessive polycystic kidney disease. Kidney Int. 2010;77(4):350–358 doi:10.1038/ki.2009.440 [DOI] [PubMed] [Google Scholar]
- 42.Losekoot M, Haarloo C, Ruivenkamp C, White SJ, Breuning MH, Peters DJM. Analysis of missense variants in the PKHD1-gene in patients with autosomal recessive polycystic kidney disease (ARPKD). Hum Genet. 2005;118(2):185–206 doi:10.1007/s00439-005-0027-7 [DOI] [PubMed] [Google Scholar]
- 43.Gunay-Aygun M, Tuchman M, Font-Montgomery E, et al. PKHD1 sequence variations in 78 children and adults with autosomal recessive polycystic kidney disease and congenital hepatic fibrosis. Mol Genet Metab. 2010;99(2):160–173 doi:10.1016/j.ymgme.2009.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gunay-Aygun M, Font-Montgomery E, Lukose L, et al. Correlation of kidney function, volume and imaging findings, and PKHD1 mutations in 73 patients with autosomal recessive polycystic kidney disease. Clin J Am Soc Nephrol. 2010;5(6):972–984 doi:10.2215/CJN.07141009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zerres K, Mücher G, Bachner L, et al. Mapping of the gene for autosomal recessive polycystic kidney disease (ARPKD) to chromosome 6p21-cen. Nat Genet. 1994;7(3):429–432 doi:10.1038/ng0794-429 [DOI] [PubMed] [Google Scholar]
- 46.Mücher G, Wirth B, Zerres K. Refining the map and defining flanking markers of the gene for autosomal recessive polycystic kidney disease on chromosome 6p21.1-p12. Am J Hum Genet. 1994;55(6):1281–1284 [PMC free article] [PubMed] [Google Scholar]
- 47.Guay-Woodford LM, Muecher G, Hopkins SD, et al. The severe perinatal form of autosomal recessive polycystic kidney disease maps to chromosome 6p21.1-p12: implications for genetic counseling. Am J Hum Genet. 1995;56(5):1101–1107 [PMC free article] [PubMed] [Google Scholar]
- 48.Rossetti S, Torra R, Coto E, et al. A complete mutation screen of PKHD1 in autosomal-recessive polycystic kidney disease (ARPKD) pedigrees. Kidney Int. 2003;64(2):391–403 doi:10.1046/j.1523-1755.2003.00111.x [DOI] [PubMed] [Google Scholar]
- 49.Zvereff V, Yao S, Ramsey J, Mikhail FM, Vijzelaar R, Messiaen L. Identification of PKHD1 multiexon deletions using multiplex ligation-dependent probe amplification and quantitative polymerase chain reaction. Genet Test Mol Biomarkers. 2010;14(4):505–510 doi:10.1089/gtmb.2009.0188 [DOI] [PubMed] [Google Scholar]
- 50.Consugar MB, Anderson SA, Rossetti S, et al. Haplotype analysis improves molecular diagnostics of autosomal recessive polycystic kidney disease. Am J Kidney Dis. 2005;45(1):77–87 doi:10.1053/j.ajkd.2004.09.009 [DOI] [PubMed] [Google Scholar]
- 51.Bergmann C, Brüchle NO, Frank V, Rehder H, Zerres K. Perinatal deaths in a family with autosomal dominant polycystic kidney disease and a PKD2 mutation. N Engl J Med. 2008;359(3):318–319 doi:10.1056/NEJMc0801868 [DOI] [PubMed] [Google Scholar]
- 52.Vujic M, Heyer CM, Ars E, et al. Incompletely penetrant PKD1 alleles mimic the renal manifestations of ARPKD. J Am Soc Nephrol. 2010;21(7):1097–1102 doi:10.1681/ASN.2009101070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bergmann C, von Bothmer J, Ortiz Brüchle N, et al. Mutations in multiple PKD genes may explain early and severe polycystic kidney disease. J Am Soc Nephrol. 2011;22(11):2047–2056 doi:10.1681/ASN.2010101080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Decramer S, Parant O, Beaufils S, et al. Anomalies of the TCF2 gene are the main cause of fetal bilateral hyperechogenic kidneys. J Am Soc Nephrol. 2007;18(3):923–933 doi:10.1681/ASN.2006091057 [DOI] [PubMed] [Google Scholar]
- 55.Bergmann C. Autosomal-recessive polycystic kidney disease gets more complex. Gastroenterology. 2013;144(5):1155–1156 doi:10.1053/j.gastro.2013.02.046 [DOI] [PubMed] [Google Scholar]
- 56.Reuss A, Wladimiroff JW, Niermeyer MF. Sonographic, clinical and genetic aspects of prenatal diagnosis of cystic kidney disease. Ultrasound Med Biol. 1991;17(7):687–694 [DOI] [PubMed] [Google Scholar]
- 57.Chaumoitre K, Brun M, Cassart M, et al. Differential diagnosis of fetal hyperechogenic cystic kidneys unrelated to renal tract anomalies: A multicenter study. Ultrasound Obstet Gynecol. 2006;28(7):911–917 doi:10.1002/uog.3856 [DOI] [PubMed] [Google Scholar]
- 58.Brun M, Maugey-Laulom B, Eurin D, Didier F, Avni EF. Prenatal sonographic patterns in autosomal dominant polycystic kidney disease: a multicenter study. Ultrasound Obstet Gynecol. 2004;24(1):55–61 doi:10.1002/uog.1098 [DOI] [PubMed] [Google Scholar]
- 59.Luthy DA, Hirsch JH. Infantile polycystic kidney disease: observations from attempts at prenatal diagnosis. Am J Med Genet. 1985;20(3):505–517 doi:10.1002/ajmg.1320200311 [DOI] [PubMed] [Google Scholar]
- 60.Zerres K, Senderek J, Rudnik-Schöneborn S, et al. New options for prenatal diagnosis in autosomal recessive polycystic kidney disease by mutation analysis of the PKHD1 gene. Clin Genet. 2004;66(1):53–57 doi:10.1111/j.0009-9163.2004.00259.x [DOI] [PubMed] [Google Scholar]
- 61.Gaspar H, Michel-Calemard L, Morel Y, Wisser J, Stallmach T, Schinzel A. Prenatal diagnosis of autosomal recessive polycystic kidney disease (ARPKD) without DNA from an index patient in a current pregnancy. Prenat Diagn. 2006;26(4):392–393 doi:10.1002/pd.1420 [DOI] [PubMed] [Google Scholar]
- 62.Gigarel N, Frydman N, Burlet P, et al. Preimplantation genetic diagnosis for autosomal recessive polycystic kidney disease. Reprod Biomed Online. 2008;16(1):152–158 [DOI] [PubMed] [Google Scholar]
- 63.Thornhill AR, deDie-Smulders CE, Geraedts JP, et al. ESHRE PGD Consortium . ESHRE PGD Consortium “Best practice guidelines for clinical preimplantation genetic diagnosis (PGD) and preimplantation genetic screening (PGS).” Hum Reprod. 2005;20(1):35–48 doi:10.1093/humrep/deh579 [DOI] [PubMed] [Google Scholar]
- 64.Lau EC, Janson MM, Roesler MR, Avner ED, Strawn EY, Bick DP. Birth of a healthy infant following preimplantation PKHD1 haplotyping for autosomal recessive polycystic kidney disease using multiple displacement amplification. J Assist Reprod Genet. 2010;27(7):397–407 doi:10.1007/s10815-010-9432-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mehler K, Beck BB, Kaul I, Rahimi G, Hoppe B, Kribs A. Respiratory and general outcome in neonates with renal oligohydramnios—a single-centre experience. Nephrol Dial Transplant. 2011;26(11)3514–3522. 10.1093/ndt/gfr046 [DOI] [PubMed]
- 66.Klaassen I, Neuhaus TJ, Mueller-Wiefel DE, Kemper MJ. Antenatal oligohydramnios of renal origin: long-term outcome. Nephrol Dial Transplant. 2007;22(2):432–439 doi:10.1093/ndt/gfl591 [DOI] [PubMed] [Google Scholar]
- 67.Beaunoyer M, Snehal M, Li L, Concepcion W, Salvatierra O, Jr, Sarwal M. Optimizing outcomes for neonatal ARPKD. Pediatr Transplant. 2007;11(3):267–271 doi:10.1111/j.1399-3046.2006.00644.x [DOI] [PubMed] [Google Scholar]
- 68.Bean SA, Bednarek FJ, Primack WA. Aggressive respiratory support and unilateral nephrectomy for infants with severe perinatal autosomal recessive polycystic kidney disease. J Pediatr. 1995;127(2):311–313 [DOI] [PubMed] [Google Scholar]
- 69.Shukla AR, Kiddoo DA, Canning DA. Unilateral nephrectomy as palliative therapy in an infant with autosomal recessive polycystic kidney disease. J Urol. 2004;172(5 pt 1):2000–2001 doi:10.1097/01.ju.0000142025.80132.2f [DOI] [PubMed] [Google Scholar]
- 70.Arbeiter A, Büscher R, Bonzel K-E, et al. Nephrectomy in an autosomal recessive polycystic kidney disease (ARPKD) patient with rapid kidney enlargement and increased expression of EGFR. Nephrol Dial Transplant. 2008;23(9):3026–3029 doi:10.1093/ndt/gfn288 [DOI] [PubMed] [Google Scholar]
- 71.Spechtenhauser B, Hochleitner BW, Ellemunter H, et al. Bilateral nephrectomy, peritoneal dialysis and subsequent cadaveric renal transplantation for treatment of renal failure due to polycystic kidney disease requiring continuous ventilation. Pediatr Transplant. 1999;3(3):246–248 [DOI] [PubMed] [Google Scholar]
- 72.Sumfest JM, Burns MW, Mitchell ME. Aggressive surgical and medical management of autosomal recessive polycystic kidney disease. Urology. 1993;42(3):309–312 [DOI] [PubMed] [Google Scholar]
- 73.Cole BR, Conley SB, Stapleton FB. Polycystic kidney disease in the first year of life. J Pediatr. 1987;111(5):693–699 [DOI] [PubMed] [Google Scholar]
- 74.Kääriäinen H, Koskimies O, Norio R. Dominant and recessive polycystic kidney disease in children: evaluation of clinical features and laboratory data. Pediatr Nephrol. 1988;2(3):296–302 [DOI] [PubMed] [Google Scholar]
- 75.Gagnadoux MF, Habib R, Levy M, Brunelle F, Broyer M. Cystic renal diseases in children. Adv Nephrol Necker Hosp. 1989;18:33–57 [PubMed] [Google Scholar]
- 76.Zerres K. Autosomal recessive polycystic kidney disease. Clin Investig. 1992;70(9):794–801 [DOI] [PubMed] [Google Scholar]
- 77.Goto M, Hoxha N, Osman R, Dell KM. The renin-angiotensin system and hypertension in autosomal recessive polycystic kidney disease. Pediatr Nephrol. 2010;25(12):2449–2457 doi:10.1007/s00467-010-1621-z [DOI] [PubMed] [Google Scholar]
- 78.Phillips JK, Hopwood D, Loxley RA, et al. Temporal relationship between renal cyst development, hypertension and cardiac hypertrophy in a new rat model of autosomal recessive polycystic kidney disease. Kidney Blood Press Res. 2007;30(3):129–144 doi:10.1159/000101828 [DOI] [PubMed] [Google Scholar]
- 79.Wühl E, Trivelli A, Picca S, et al. ESCAPE Trial Group . Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361(17):1639–1650 doi:10.1056/NEJMoa0902066 [DOI] [PubMed] [Google Scholar]
- 80.Dias NF, Lanzarini V, Onuchic LF, Koch VHK. Clinical aspects of autosomal recessive polycystic kidney disease. J Bras Neurol. 2010;32(3):263–267 [PubMed] [Google Scholar]
- 81.Lucaya J, Enriquez G, Nieto J, Callis L, Garcia Peña P, Dominguez C. Renal calcifications in patients with autosomal recessive polycystic kidney disease: prevalence and cause. AJR Am J Roentgenol. 1993;160(2):359–362 doi:10.2214/ajr.160.2.8424350 [DOI] [PubMed] [Google Scholar]
- 82.Wen J. Congenital hepatic fibrosis in autosomal recessive polycystic kidney disease. Clin Transl Sci. 2011;4(6):460–465 doi:10.1111/j.1752-8062.2011.00306.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Srinath A, Shneider BL. Congenital hepatic fibrosis and autosomal recessive polycystic kidney disease. J Pediatr Gastroenterol Nutr. 2012;54(5):580–587 doi:10.1097/MPG.0b013e31824711b7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gunay-Aygun M, Font-Montgomery E, Lukose L, et al. Characteristics of congenital hepatic fibrosis in a large cohort of patients with autosomal recessive polycystic kidney disease. Gastroenterology. 2013;144(1)112–121.e2 10.1053/j.gastro.2012.09.056 [DOI] [PMC free article] [PubMed]
- 85.Telega G, Cronin D, Avner ED. New approaches to the autosomal recessive polycystic kidney disease patient with dual kidney-liver complications. Pediatr Transplant. 2013;17(4):328–335 doi:10.1111/petr.12076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Higashihara E, Nutahara K, Okegawa T, et al. Kidney volume and function in autosomal dominant polycystic kidney disease. Clin Exp Nephrol. 2014;18(1)157–165 10.1007/s10157-013-0834-4 [DOI] [PMC free article] [PubMed]
- 87.Grantham JJ, Torres VE, Chapman AB, et al. CRISP Investigators . Volume progression in polycystic kidney disease. N Engl J Med. 2006;354(20):2122–2130 doi:10.1056/NEJMoa054341 [DOI] [PubMed] [Google Scholar]
- 88.Fonck C, Chauveau D, Gagnadoux MF, Pirson Y, Grünfeld JP. Autosomal recessive polycystic kidney disease in adulthood. Nephrol Dial Transplant. 2001;16(8):1648–1652 [DOI] [PubMed] [Google Scholar]
- 89.Blickman JG, Bramson RT, Herrin JT. Autosomal recessive polycystic kidney disease: long-term sonographic findings in patients surviving the neonatal period. AJR Am J Roentgenol. 1995;164(5):1247–1250 doi:10.2214/ajr.164.5.7717240 [DOI] [PubMed] [Google Scholar]
- 90.Lieberman E, Salinas-Madrigal L, Gwinn JL, Brennan LP, Fine RN, Landing BH. Infantile polycystic disease of the kidneys and liver: clinical, pathological and radiological correlations and comparison with congenital hepatic fibrosis. Medicine (Baltimore). 1971;50(4):277–318 [DOI] [PubMed] [Google Scholar]
- 91.Avni FE, Guissard G, Hall M, Janssen F, DeMaertelaer V, Rypens F. Hereditary polycystic kidney diseases in children: changing sonographic patterns through childhood. Pediatr Radiol. 2002;32(3):169–174 [DOI] [PubMed] [Google Scholar]
- 92.Cassart M, Massez A, Metens T, et al. Complementary role of MRI after sonography in assessing bilateral urinary tract anomalies in the fetus. AJR Am J Roentgenol. 2004;182(3):689–695 doi:10.2214/ajr.182.3.1820689 [DOI] [PubMed] [Google Scholar]
- 93.Kern S, Zimmerhackl LB, Hildebrandt F, Ermisch-Omran B, Uhl M. Appearance of autosomal recessive polycystic kidney disease in magnetic resonance imaging and RARE-MR-urography. Pediatr Radiol. 2000;30(3):156–160 [DOI] [PubMed] [Google Scholar]
- 94.Piscaglia F, Marinelli S, Bota S, et al. The role of ultrasound elastographic techniques in chronic liver disease: current status and future perspectives. Eur J Radiol. 2014;83450–455 10.1016/j.ejrad.2013.06.009 [DOI] [PubMed]
- 95.Kummer S, Sagir A, Pandey S, et al. Liver fibrosis in recessive multicystic kidney diseases: transient elastography for early detection. Pediatr Nephrol. 2011;26(5):725–731 doi:10.1007/s00467-011-1771-7 [DOI] [PubMed] [Google Scholar]
- 96.Beil S, Drube J, Gluer S, Lehner F, Ehrich JHH, Pape L. End-stage renal disease due to ARPKD in the first months of life: transplantation or dialysis?—two case reports. Pediatr Transplant. 2010;14(6):E75–E78 doi:10.1111/j.1399-3046.2009.01167.x [DOI] [PubMed] [Google Scholar]
- 97.Kashtan CE, Primack WA, Kainer G, Rosenberg AR, McDonald RA, Warady BA. Recurrent bacteremia with enteric pathogens in recessive polycystic kidney disease. Pediatr Nephrol. 1999;13(8):678–682 [DOI] [PubMed] [Google Scholar]
- 98.Davis ID, Ho M, Hupertz V, Avner ED. Survival of childhood polycystic kidney disease following renal transplantation: the impact of advanced hepatobiliary disease. Pediatr Transplant. 2003;7(5):364–369 [DOI] [PubMed] [Google Scholar]
- 99.Chapal M, Dufay A, Roussey G, et al. Kidney and liver transplantation in patients with autosomal recessive polycystic kidney disease: a multicentric study. Nephrol Dial Transplant. 2012;27(5)2083–2088 10.1093/ndt/gfr588 [DOI] [PubMed]
- 100.Khan K, Schwarzenberg SJ, Sharp HL, Matas AJ, Chavers BM. Morbidity from congenital hepatic fibrosis after renal transplantation for autosomal recessive polycystic kidney disease. Am J Transplant. 2002;2(4):360–365 [DOI] [PubMed] [Google Scholar]
- 101.Charlton MR, Wall WJ, Ojo AO, et al. International Liver Transplantation Society Expert Panel . Report of the first international liver transplantation society expert panel consensus conference on renal insufficiency in liver transplantation. Liver Transpl. 2009;15(11):S1–S34 doi:10.1002/lt.21877 [DOI] [PubMed] [Google Scholar]
- 102.Eason JD, Gonwa TA, Davis CL, Sung RS, Gerber D, Bloom RD. Proceedings of Consensus Conference on Simultaneous Liver Kidney Transplantation (SLK). Am J Transplant. 2008;8(11):2243–2251 doi:10.1111/j.1600-6143.2008.02416.x [DOI] [PubMed] [Google Scholar]
- 103.Brinkert F, Lehnhardt A, Montoya C, et al. Combined liver-kidney transplantation for children with autosomal recessive polycystic kidney disease (ARPKD): indication and outcome. Transpl Int. 2013;26(6):640–650 doi:10.1111/tri.12098 [DOI] [PubMed] [Google Scholar]
- 104.Lilova M, Kaplan BS, Meyers KE. Recombinant human growth hormone therapy in autosomal recessive polycystic kidney disease. Pediatr Nephrol. 2003;18(1):57–61 doi:10.1007/s00467-002-0986-z [DOI] [PubMed] [Google Scholar]
- 105.Konrad M, Zerres K, Wühl E, Rudnik-Schöneborn S, Holtkamp U, Schärer K. Body growth in children with polycystic kidney disease. Arbeitsgemeinschaft für Pädiatrische Nephrologie. Acta Paediatr. 1995;84(11):1227–1232 [DOI] [PubMed] [Google Scholar]
- 106.Hooper SR, Gerson AC, Butler RW, et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(8):1824–1830 doi:10.2215/CJN.09751110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lande MB, Gerson AC, Hooper SR, et al. Casual blood pressure and neurocognitive function in children with chronic kidney disease: a report of the children with chronic kidney disease cohort study. Clin J Am Soc Nephrol. 2011;6(8):1831–1837 doi:10.2215/CJN.00810111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kupferman JC, Lande MB, Adams HR, Pavlakis SG. Primary hypertension and neurocognitive and executive functioning in school-age children. Pediatr Nephrol. 2013;28(3):401–408 doi:10.1007/s00467-012-2215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lande MB, Kupferman JC, Adams HR. Neurocognitive alterations in hypertensive children and adolescents. J Clin Hypertens (Greenwich). 2012;14(6):353–359 doi:10.1111/j.1751-7176.2012.00661.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ostrovskaya MA, Rojas M, Kupferman JC, et al. Executive function and cerebrovascular reactivity in pediatric hypertension [published online ahead of print July 22, 2013]. J Child Neurol 10.1177/0883073813494264 [DOI] [PubMed]
- 111.Adams HR, Szilagyi PG, Gebhardt L, Lande MB. Learning and attention problems among children with pediatric primary hypertension. Pediatrics. 2010;126(6). Available at: www.pediatrics.org/cgi/content/full/126/6/e1425 doi:10.1542/peds.2010-1899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hartung EA, Matheson M, Lande MB, et al. Neurocognition in children with autosomal recessive polycystic kidney disease in the CKiD Cohort Study [published online ahead of print May 15, 2014]. Pediatr Nephrol. doi: 10.1007/s00467-014-2816-5. doi:10.1007/s00467-014-2816-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gerson AC, Wentz A, Abraham AG, et al. Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics. 2010;125(2). Available at: www.pediatrics.org/cgi/content/full/125/2/e349 doi:10.1542/peds.2009-0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Neul SK, Minard CG, Currier H, Goldstein SL. Health-related quality of life functioning over a 2-year period in children with end-stage renal disease. Pediatr Nephrol. 2013;28(2):285–293 doi:10.1007/s00467-012-2313-7 [DOI] [PubMed] [Google Scholar]
- 115.Becker JU, Opazo Saez A, Zerres K, et al. The mTOR pathway is activated in human autosomal-recessive polycystic kidney disease. Kidney Blood Press Res. 2010;33(2):129–138 doi:10.1159/000314380 [DOI] [PubMed] [Google Scholar]
- 116.Fischer D-C, Jacoby U, Pape L, et al. Activation of the AKT/mTOR pathway in autosomal recessive polycystic kidney disease (ARPKD). Nephrol Dial Transplant. 2009;24(6):1819–1827 doi:10.1093/ndt/gfn744 [DOI] [PubMed] [Google Scholar]
- 117.Renken C, Fischer DC, Kundt G, Gretz N, Haffner D. Inhibition of mTOR with sirolimus does not attenuate progression of liver and kidney disease in PCK rats. Nephrol Dial Transplant. 2011;26(1):92–100 doi:10.1093/ndt/gfq384 [DOI] [PubMed] [Google Scholar]
- 118.Serra AL, Poster D, Kistler AD, et al. Sirolimus and kidney growth in autosomal dominant polycystic kidney disease. N Engl J Med. 2010;363(9):820–829 doi:10.1056/NEJMoa0907419 [DOI] [PubMed] [Google Scholar]
- 119.Walz G, Budde K, Mannaa M, et al. Everolimus in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2010;363(9):830–840 doi:10.1056/NEJMoa1003491 [DOI] [PubMed] [Google Scholar]
- 120.Wahl PR, Serra AL, Le Hir M, Molle KD, Hall MN, Wüthrich RP. Inhibition of mTOR with sirolimus slows disease progression in Han:SPRD rats with autosomal dominant polycystic kidney disease (ADPKD). Nephrol Dial Transplant. 2006;21(3):598–604 doi:10.1093/ndt/gfi181 [DOI] [PubMed] [Google Scholar]
- 121.Berthier CC, Wahl PR, Le Hir M, et al. Sirolimus ameliorates the enhanced expression of metalloproteinases in a rat model of autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2008;23(3):880–889 doi:10.1093/ndt/gfm697 [DOI] [PubMed] [Google Scholar]
- 122.Shillingford JM, Piontek KB, Germino GG, Weimbs T. Rapamycin ameliorates PKD resulting from conditional inactivation of Pkd1. J Am Soc Nephrol. 2010;21(3):489–497 doi:10.1681/ASN.2009040421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shillingford JM, Murcia NS, Larson CH, et al. The mTOR pathway is regulated by polycystin-1, and its inhibition reverses renal cystogenesis in polycystic kidney disease. Proc Natl Acad Sci USA. 2006;103(14):5466–5471 doi:10.1073/pnas.0509694103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tao Y, Kim J, Schrier RW, Edelstein CL. Rapamycin markedly slows disease progression in a rat model of polycystic kidney disease. J Am Soc Nephrol. 2005;16(1):46–51 doi:10.1681/ASN.2004080660 [DOI] [PubMed] [Google Scholar]
- 125.Yamaguchi T, Pelling JC, Ramaswamy NT, et al. cAMP stimulates the in vitro proliferation of renal cyst epithelial cells by activating the extracellular signal-regulated kinase pathway. Kidney Int. 2000;57(4):1460–1471 doi:10.1046/j.1523-1755.2000.00991.x [DOI] [PubMed] [Google Scholar]
- 126.Hanaoka K, Guggino WB. cAMP regulates cell proliferation and cyst formation in autosomal polycystic kidney disease cells. J Am Soc Nephrol. 2000;11(7):1179–1187 [DOI] [PubMed] [Google Scholar]
- 127.Yamaguchi T, Nagao S, Wallace DP, et al. Cyclic AMP activates B-Raf and ERK in cyst epithelial cells from autosomal-dominant polycystic kidneys. Kidney Int. 2003;63(6):1983–1994 doi:10.1046/j.1523-1755.2003.00023.x [DOI] [PubMed] [Google Scholar]
- 128.Belibi FA, Reif G, Wallace DP, et al. Cyclic AMP promotes growth and secretion in human polycystic kidney epithelial cells. Kidney Int. 2004;66(3):964–973 doi:10.1111/j.1523-1755.2004.00843.x [DOI] [PubMed] [Google Scholar]
- 129.Yamaguchi T, Wallace DP, Magenheimer BS, Hempson SJ, Grantham JJ, Calvet JP. Calcium restriction allows cAMP activation of the B-Raf/ERK pathway, switching cells to a cAMP-dependent growth-stimulated phenotype. J Biol Chem. 2004;279(39):40419–40430 doi:10.1074/jbc.M405079200 [DOI] [PubMed] [Google Scholar]
- 130.Yamaguchi T, Hempson SJ, Reif GA, Hedge A-M, Wallace DP. Calcium restores a normal proliferation phenotype in human polycystic kidney disease epithelial cells. J Am Soc Nephrol. 2006;17(1):178–187 doi:10.1681/ASN.2005060645 [DOI] [PubMed] [Google Scholar]
- 131.Yasuda G, Jeffries WB. Regulation of cAMP production in initial and terminal inner medullary collecting ducts. Kidney Int. 1998;54(1):80–86 doi:10.1046/j.1523-1755.1998.00990.x [DOI] [PubMed] [Google Scholar]
- 132.Gattone VH, 2nd, Wang X, Harris PC, Torres VE. Inhibition of renal cystic disease development and progression by a vasopressin V2 receptor antagonist. Nat Med. 2003;9(10):1323–1326 doi:10.1038/nm935 [DOI] [PubMed] [Google Scholar]
- 133.Wang X, Wu Y, Ward CJ, Harris PC, Torres VE. Vasopressin directly regulates cyst growth in polycystic kidney disease. J Am Soc Nephrol. 2008;19(1):102–108 doi:10.1681/ASN.2007060688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Torres VE, Chapman AB, Devuyst O, et al. TEMPO 3:4 Trial Investigators . Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367(25):2407–2418 doi:10.1056/NEJMoa1205511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Masyuk TV, Radtke BN, Stroope AJ, et al. Pasireotide is more effective than octreotide in reducing hepatorenal cystogenesis in rodents with polycystic kidney and liver diseases. Hepatology. 2013;58(1):409–421 doi:10.1002/hep.26140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Caroli A, Perico N, Perna A, et al. ALADIN study group . Effect of longacting somatostatin analogue on kidney and cyst growth in autosomal dominant polycystic kidney disease (ALADIN): a randomised, placebo-controlled, multicentre trial. Lancet. 2013;382(9903):1485–1495 doi:10.1016/S0140-6736(13)61407-5 [DOI] [PubMed] [Google Scholar]
- 137.Sweeney WE, Jr, Avner ED. Molecular and cellular pathophysiology of autosomal recessive polycystic kidney disease (ARPKD). Cell Tissue Res. 2006;326(3):671–685 doi:10.1007/s00441-006-0226-0 [DOI] [PubMed] [Google Scholar]
- 138.Dell KM, Nemo R, Sweeney WE, Jr, Levin JI, Frost P, Avner ED. A novel inhibitor of tumor necrosis factor-alpha converting enzyme ameliorates polycystic kidney disease. Kidney Int. 2001;60(4):1240–1248 doi:10.1046/j.1523-1755.2001.00963.x [DOI] [PubMed] [Google Scholar]
- 139.Sweeney WE, Jr, Hamahira K, Sweeney J, Garcia-Gatrell M, Frost P, Avner ED. Combination treatment of PKD utilizing dual inhibition of EGF-receptor activity and ligand bioavailability. Kidney Int. 2003;64(4):1310–1319 doi:10.1046/j.1523-1755.2003.00232.x [DOI] [PubMed] [Google Scholar]
- 140.Sato Y, Harada K, Kizawa K, et al. Activation of the MEK5/ERK5 cascade is responsible for biliary dysgenesis in a rat model of Caroli’s disease. Am J Pathol. 2005;166(1):49–60 doi:10.1016/S0002-9440(10)62231-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sweeney WE, Chen Y, Nakanishi K, Frost P, Avner ED. Treatment of polycystic kidney disease with a novel tyrosine kinase inhibitor. Kidney Int. 2000;57(1):33–40 doi:10.1046/j.1523-1755.2000.00829.x [DOI] [PubMed] [Google Scholar]
- 142.Sweeney WE, Jr, von Vigier RO, Frost P, Avner ED. Src inhibition ameliorates polycystic kidney disease. J Am Soc Nephrol. 2008;19(7):1331–1341 doi:10.1681/ASN.2007060665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Somlo S, Guay-Woodford LM. Polycystic kidney disease. In: Lifton RP, Somlo S, Giebisch GH, Seldin DW, eds. Genetic Diseases of the Kidney. Burlington, MA: Elsevier; 2009:393–424 [Google Scholar]