Abstract
BACKGROUND:
Over the past half century the prevalence of childhood disability increased dramatically, coupled with notable increases in the prevalence of mental health and neurodevelopmental conditions. This study provides a detailed assessment of recent trends in childhood disability in relation to health conditions and sociodemographic factors.
METHODS:
Secondary data analysis of National Health Interview Survey (NHIS) datasets 2001–2002, 2004–2005, 2007–2008, and 2010–2011 (N = 198 888) was conducted to calculate the prevalence, rate of change, severity, and sociodemographic disparities of parent-reported childhood disability.
RESULTS:
The prevalence of childhood disability has continued to increase, growing by 15.6% between 2001–2002 and 2010–2011. Nearly 6 million children were considered disabled in 2010–2011. Children living in poverty experienced the highest rates of disability, 102.6 cases per 1000 population in 2010–2011, but unexpectedly, children living in households with incomes ≥400% above the federal poverty level experienced the largest increase (28.4%) over this 10-year period. The percentage of disability cases related to any physical health condition declined 11.8% during the decade, whereas cases related to any neurodevelopmental or mental health condition increased by 20.9%.
CONCLUSIONS:
Over the past decade, parent-reported childhood disability steadily increased. As childhood disability due to physical conditions declined, there was a large increase in disabilities due to neurodevelopmental or mental health problems. For the first time since the NHIS began tracking childhood disability in 1957, the rise in reported prevalence is disproportionately occurring among socially advantaged families. This unexpected finding highlights the need to better understand the social, medical, and environmental factors influencing parent reports of childhood disability.
Keywords: disability, sociodemographic, disparities, activity limitations, children
What’s Known on This Subject:
The prevalence of disability in childhood has been on the rise for the past several decades. Children living in poverty are more likely to have chronic health conditions and experience disabilities.
What This Study Adds:
The percentage of children with disabilities rose 16% between 2001 and 2011. Economically disadvantaged children had the highest rates of disability, but economically advantaged children experienced greater increases in disability. Disability due to neurodevelopmental or mental health conditions rose substantially.
A century of medical advances and public health improvements have dramatically altered the epidemiology of child health. Mortality rates for many pediatric conditions such as acute infectious diseases, prematurity, congenital heart disease, and cystic fibrosis have significantly declined.1–5 At the same time, the number of children with developmental, behavioral, and mental health conditions, such as autism, attention-deficit/hyperactivity disorder, and developmental disabilities, has increased.6,7 Advances in medical technology, health care delivery, and public health interventions do not explain why more children are diagnosed with neurodevelopmental and behavioral conditions and the resulting rise in disability.6
A recent study, using the National Longitudinal Survey of Youth, reported that the prevalence of behavioral and learning problems more than doubled between 1988 and 2006, and a statistically significant rise was noted for chronic conditions overall.8 Van Cleave et al8 also noted the fluctuating nature of chronic health conditions and highlighted the dynamic nature of illness trajectories and their health impacts on children. Analysis of National Health Interview Survey (NHIS) data between 1960 and 2010 shows that parentally reported rates of childhood disability, as defined by activity limitations due to chronic conditions, have increased from 2% to 8%.9 Although a growing body of evidence indicates that the face of disability in childhood is changing, no studies have undertaken a comprehensive evaluation of recent trends across all types of disabilities to elucidate these epidemiologic shifts. To address the gaps in the literature, we sought to examine trends in childhood disability over the past decade by using NHIS data collected between 2001 and 2011 and to assess changes in prevalence, severity, and composition of disability in relation to demographic and socioeconomic factors.
Methods
Study Design and Data Collection
We used the NHIS to conduct this analysis. The NHIS is the only continuing nationwide survey designed to collect information on the demographic characteristics, disability status, and health care use patterns of the US civilian noninstitutionalized population. The survey is conducted annually by the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) and has been the principal source of information for the Department of Health and Human Services to monitor health trends in the United States since 1957.10 The final response rates for the child samples varied from a low of 70.7% in 2010 to a high of 81.3% in 2002.11,12 Items were used from the Core Family and Child components of the survey and pooled 2 years of data at 4 points over the decade to increase statistical precision (2001–2002, 2004–2005, 2007–2008, and 2010–2011). The Core components are intended to be used for trend analyses and can be pooled because the questions remain largely unchanged from year to year. The Family component collects demographic information, health and functional status, health care service use and access, health insurance, and income data for people living in the home. In homes with children, 1 randomly selected child is the subject of the Child component, which gathers additional data on health behaviors, status, and service use. Responses for 198 888 separate children aged 0 to 17 years were included in this study. A knowledgeable adult (typically a parent or guardian) responded for children <17 years old. When present, adolescents 17 years old at the time of the interview responded for themselves. Key items used in this analysis, including the disability questions, remained unchanged during the 10-year period, except in 2011, when the term intellectual disability was added to the question about mental retardation.
Variable Construction
Disability is measured here using the NHIS limitation of activity approach. Under this method, a child was considered to be disabled if the survey respondent reported that the child experienced any of the following due to a chronic condition: limitations in the kinds or amounts of play activities done by other children (<5 years); needing help with personal care including bathing, dressing, eating, getting in and out of bed and chairs, using the toilet, and getting around the home (3+ years); difficulty walking without equipment (<18 years); difficulty remembering (<18 years); receipt of special education services or early intervention services (<18 years); or any other activity limitation (<18 years). Use of special education services was included as a marker of disability because children who receive special education services have been identified as having difficulty functioning in the academic environment. The NHIS approach used here is consistent with the International Classification of Functioning, Disability and Health framework for understanding disability.13
When a limitation was reported (Fig 1), the respondent was asked to identify the health problem or condition that caused it, choosing from a list contained on a flashcard provided by the interviewer. We classified the 14 possible responses into 3 categories based on the predominant features of the condition: primarily physical conditions, primarily neurodevelopmental or mental health conditions, and other conditions that could not be classified as primarily physical or neurodevelopmental or mental health. The list of problems in the NHIS intentionally allows respondents to categorize their child’s health condition without providing them an unwieldy exhaustive list of health conditions. Consequently, not all possible diagnoses were offered to respondents for categorization, and diagnoses were sometimes categorized in broad groups, such as “asthma/breathing problems.” We assigned developmental problems to the neurodevelopmental category, even though children may have substantial physical limitations associated with these conditions. Of note, the respondent could indicate that the child’s activity limitations were caused by >1 condition.
FIGURE 1.
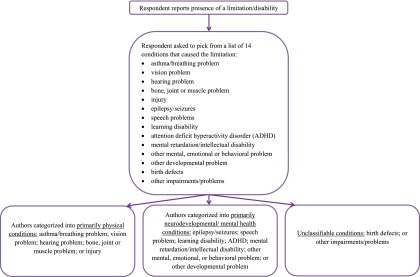
Classification of health conditions associated with childhood disability from the National Health Interview Survey.
Condition severity was described in terms of 2 proxy measures: the mean number of days of school missed due to illness or injury and overall health status as reported by the survey respondent. For young children, health status was the only measure of severity. The sociodemographic variables of interest were age (divided into 3 groups: <6 years, 6–11 years, and 12–17 years), gender, race or ethnicity, family income measured in terms of the federal poverty level (FPL), household composition, and highest educational level attained in the household.
Statistical Analysis
To calculate the prevalence of disability, survey weights provided by the NCHS were used. Design and ratio adjustments are made in the calculation of the person-level weights along with demographic adjustments from census data.14 Additional information about the design and operation of the NHIS, including the survey weights to adjust the data to be nationally representative, is available through the NCHS.15 The Taylor series linearization method was used to adjust the standard errors for the complex survey design. Wald tests of linear trend were used to determine differences in prevalence over the time series. We used multiply imputed income files provided by the NCHS.16 We conducted our analyses by using Stata version 12 (Stata Corp, College Station, TX) to accommodate the multiply imputed data.17 A P value cutoff of <.05 was set a priori as statistically significant. This study falls under the exempt category for human subjects research at the University of California.
Results
Changes in the Overall Prevalence of Disability
The overall rate of disability for noninstitutionalized children <18 years old increased 15.6% between 2001–2002 and 2010–2011 (Table 1). The estimated number of children with disabilities increased from 4 991 000 to 5 912 000, or from 6.87% to 7.94% of the population. An increase was found for all age groups, both genders, and Hispanics and non-Hispanic whites. Despite the statistically significant increase in disability rates among Hispanics, they repeatedly reported significantly lower rates of disability than non-Hispanics whites and blacks. Rates of disability significantly increased only among children living in households on the opposite ends of the income spectrum, with a much larger rise among children living in more financially advantaged households. Children living in households with incomes less than the FPL experienced a 10.7% rise in the rate of disability, compared with a 28.4% rise for children living in homes with ≥400% of the FPL. However, the inverse relationship between poverty status and disability remained: children from lower-income households continue to have higher rates of disability than children from higher-income families. Significant increases in disability prevalence also occurred for children of college-educated parents but not for children of parents with a high school education or less and for children in 2-parent homes or other family structures, but not for children of single parents.
TABLE 1.
Prevalence of Disabilities Due to Chronic Conditions by Sociodemographic Characteristics, US Children Ages 0–17, 2001–2011
| 2001–2002 | 2001–2002 (N = 54 651)a | 2004–2005 (N = 52 881)a | 2007–2008 (N = 40 569)a | 2010–2011 (N = 50 793)a | 2010–2011 | 2001–2011 | |
|---|---|---|---|---|---|---|---|
| Estimated Cases | Cases/1000 (SE) | Cases/1000 (SE) | Cases/1000 (SE) | Cases/1000 (SE) | Estimated Cases | % Change in Prevalence | |
| Overall | 4 991 000 | 68.7 (1.3) | 69.8 (1.4) | 72.3 (1.8) | 79.4 (1.6) | 5 912 000 | 15.6b |
| Child age | |||||||
| <6 y | 867 000 | 36.5 (1.7) | 42.7 (1.8) | 43.0 (2.3) | 51.7 (2.0) | 1 319 000 | 41.6b |
| 6–11 y | 2 047 000 | 83.6 (2.4) | 81.2 (2.3) | 86.8 (2.8) | 92.0 (2.8) | 2 279 000 | 10.0b |
| 12–17 y | 2 077 000 | 85.0 (2.6) | 84.6 (2.5) | 87.7 (3.3) | 95.7 (2.7) | 2 314 000 | 12.6b |
| Child gender | |||||||
| Male | 3 250 000 | 87.5 (2.0) | 88.8 (2.0) | 94.0 (2.5) | 101.2 (2.4) | 3 854 000 | 15.7b |
| Female | 1 741 000 | 49.0 (1.6) | 49.9 (1.7) | 49.7 (1.9) | 56.5 (1.8) | 2 058 000 | 15.3b |
| Race or ethnicity | |||||||
| White, non-Hispanic | 3 235 000 | 71.6 (1.8) | 73.4 (1.9) | 80.3 (2.6) | 86.7 (2.4) | 3 513 000 | 21.1b |
| Hispanic | 596 000 | 49.7 (2.1) | 53.1 (2.1) | 51.0 (2.5) | 61.1 (2.6) | 1 027 000 | 22.9b |
| Black, non-Hispanic | 856 000 | 82.2 (3.8) | 81.6 (3.9) | 77.6 (4.0) | 93.5 (3.9) | 966 000 | 13.4 |
| Multiple race or other | 304 000 | 59.9 (5.0) | 60.1 (4.7) | 62.6 (5.3) | 59.3 (3.6) | 407 000 | −1.0 |
| Family income | |||||||
| <100% FPL | 1 210 000 | 92.7 (3.7) | 90.9 (4.1) | 100.3 (5.1) | 102.6 (4.0) | 1 725 000 | 10.7b |
| 100%–199% FPL | 1 247 000 | 80.7 (3.4) | 77.8 (3.3) | 81.0 (3.8) | 86.1 (3.6) | 1 475 000 | 6.7 |
| 200%–299% FPL | 892 000 | 68.0 (3.2) | 68.5 (3.5) | 67.8 (4.0) | 72.3 (4.1) | 885 000 | 6.3 |
| 300%–399% FPL | 609 000 | 60.8 (4.1)) | 68.1 (4.1) | 65.3 (5.0) | 68.3 (4.5) | 604 000 | 12.3 |
| ≥400% FPL | 1 034 000 | 49.0 (2.4) | 51.8 (2.6) | 53.1 (3.1) | 62.9 (2.8) | 1 223 000 | 28.4b |
| Highest household education | |||||||
| Less than high school | 667 000 | 80.4 (4.2) | 69.5 (3.8) | 68.4 (4.7) | 88.0 (5.3) | 693 000 | 9.5 |
| High school diploma | 1 371 000 | 81.7 (3.2) | 76.2 (3.0) | 82.1 (4.0) | 82.5 (3.6) | 1 224 000 | 1.0 |
| Some college | 1 835 000 | 79.0 (2.5) | 81.2 (2.7) | 83.6 (3.4) | 89.9 (2.6) | 2 197 000 | 13.8b |
| College degree or higher | 1 089 000 | 47.6 (2.1) | 58.3 (2.2) | 59.6 (3.0) | 66.3 (2.3) | 1 783 000 | 39.3b |
| Family structure | |||||||
| 2 parents | 2 418 000 | 55.6 (1.6) | 58.6 (1.7) | 61.4 (2.2) | 65.4 (1.9) | 2 611 000 | 17.6b |
| Single parent | 1 084 000 | 101.9 (4.0) | 94.1 (4.1) | 95.0 (4.7) | 107.3 (4.1) | 1 270 000 | 5.3 |
| Other | 1 485 000 | 80.1 (2.9) | 78.9 (2.6) | 82.2 (3.4) | 89.5(3.1) | 2 028 000 | 11.7b |
Sample size is 2% lower for household education in 2001–2002, 2004–2005, and 2007–2008 and 1% lower in 2010–2011 because of missing data.
Wald trend test P < .05, percentage change values calculated between 2001–2002 and 2010–2011.
Changes in Disability Case Mix
As shown in Table 2, the overall increase in disability prevalence was driven by increases in health conditions that were classified as primarily neurodevelopmental or mental health. There was a commensurate decline in the proportion of disabilities caused by conditions classified as primarily physical over the same time period. There was 24.2% decrease in asthma as the cause of childhood disability, whereas there was marked increase in disability associated with speech problems (63.1% increase), mental retardation or intellectual impairment (63% increase), and other mental, emotional, or behavioral problems (64.7% increase).
TABLE 2.
Prevalence of Chronic Conditions Associated With Limitations in Usual Activities for US Children Aged <18, 2001–2011a
| 2001–2002 | 2001–2002 (N = 54 651) | 2004–2005 (N = 52 881) | 2007–2008 (N = 40 569) | 2010–2011 (N = 50 793) | 2010–2011 | 2001–2011 | |
|---|---|---|---|---|---|---|---|
| Estimated No. Cases | Cases per 100 000 (SE) | Cases per 100 000 (SE) | Cases per 100 000 (SE) | Cases per 100 000 (SE) | Estimated No. Cases | % Change in Prevalence | |
| Any physical health condition | 1 099 000 | 1512 (65) | 1265 (60) | 1229 (68) | 1333 (66) | 994 000 | −11.8 |
| Asthma or breathing problem | 586 000 | 807 (47) | 617 (44) | 589 (44) | 612 (40) | 456 000 | −24.2b |
| Hearing problem | 196 000 | 270 (24) | 279 (24) | 263 (31) | 312 (32) | 233 000 | 15.6 |
| Vision problem | 188 000 | 259 (27) | 195 (19) | 266 (33) | 295 (29) | 220 000 | 13.9 |
| Bone, joint, or muscle problem | 175 000 | 241 (23) | 227 (25) | 230 (29) | 269 (34) | 200 000 | 11.6 |
| Injuries | 62 000 | 86 (15) | 71 (13) | 73 (20) | 71 (16) | 53 000 | −17.4 |
| Any neurodevelopmental or mental health condition | 3 927 000 | 5404 (125) | 5543 (127) | 5977 (163) | 6531 (149) | 4 864 000 | 20.9b |
| Epilepsy or seizures | 162 000 | 223 (23) | 154 (20) | 212 (29) | 203 (23) | 151 000 | −9.0 |
| Speech problems | 835 000 | 1150 (59) | 1301 (54) | 1600 (82) | 1876 (80) | 1 397 000 | 63.1b |
| Learning disability | 1 590 000 | 2188 (72) | 1634 (75) | 1747 (87) | 1903 (80) | 1 417 000 | −13.0b |
| Attention-deficit/hyperactivity disorder | 1 071 000 | 1474 (67) | 1467 (67) | 1676 (77) | 1799 (83) | 1 400 000 | 22.0b |
| Mental retardation | 163 000 | 224 (23) | 262 (24) | 217 (31) | 365 (36) | 272 000 | 63.0b,c |
| Other mental, emotional, or behavioral problems | 695 000 | 956 (54) | 1038 (55) | 1314 (73) | 1575 (71) | 1 173 000 | 64.7b |
| Other developmental problem | 462 000 | 636 (40) | 785 (52) | 759 (56) | 873 (48) | 650 000 | 37.3b |
| Other, not classifiable | |||||||
| Other impairment or problem | 371 113 | 511 (39) | 480 (38) | 362 (36) | 480 (36) | 358 000 | −6.0 |
| Birth defect | 253 753 | 349 (29) | 345 (30) | 370 (34) | 434 (33) | 323 000 | 24.4b |
Parents could answer that their child had >1 condition contributing to activity limitation.
Wald trend test P < .05, percentage change values calculated between 2001–2002 and 2010–2011.
Wording for this item was altered in 2011 to intellectual disability, also known as mental retardation, contributes to activity limitation. Prevalence was 319 per 100 000 population in 2010 and 411 per 100 000 population in 2011.
To further illuminate the rise in disability related to neurodevelopmental or mental health conditions, we examined disability trends by the same sociodemographic characteristics presented in Table 1 (Table 3). We found the greatest rise in disability due to neurodevelopmental or mental health conditions among children <6 years old, who experienced a 62.1% change in prevalence (23.5 per 1000 population to 38.1 per 1000 population). Across all ages, prevalence of disability due to neurodevelopmental or mental health conditions increased for Hispanics (29.1%), non-Hispanic whites (27.2%), and non-Hispanic blacks (20.1%). All income groups, except children living in households with incomes between 100% and 299% of the FPL, experienced a statistically significant rise in the prevalence of disability-associated neurodevelopmental or mental health conditions.
TABLE 3.
Change in Prevalence of Neurodevelopmental or Mental Health Conditions by Sociodemographics, 2001–2011a
| Any Neurodevelopmental or Mental Health Condition,b No. Cases per 1000 (SE) | |||||
|---|---|---|---|---|---|
| 2001–2002 (N = 54 651)a | 2004–2005 (N = 52 881)a | 2007–2008 (N = 40 569)a | 2010–2011 (N = 50 793)a | % Change in Prevalence | |
| Overall | 54.0 (1.3) | 55.4 (1.3) | 59.8 (1.6) | 65.3 (1.5) | 20.9c |
| Child age | |||||
| <6 y | 23.5 (1.4) | 29.1 (1.6) | 30.2 (2.0) | 38.1 (1.9) | 62.1c |
| 6–11 y | 69.4 (2.2) | 67.8 (2.2) | 74.6 (2.6) | 80.2 (2.6) | 15.6c |
| 12–17 y | 68.3 (2.4) | 68.7 (2.3) | 74.8 (3.1) | 78.8 (2.6) | 15.4c |
| Child gender | |||||
| Male | 71.5 (1.9) | 73.1 (1.9) | 79.1 (2.3) | 86.1 (2.2) | 20.4c |
| Female | 35.8 (1.4) | 37.0 (1.4) | 39.6 (1.8) | 43.6 (1.5) | 21.8c |
| Race or ethnicity | |||||
| White, non-Hispanic | 56.7 (1.7) | 58.1 (1.6) | 66.8 (2.4) | 72.1 (2.3) | 27.2c |
| Hispanic | 39.2 (1.9) | 43.3 (2.0) | 42.3 (2.3) | 50.6 (2.3) | 29.1c |
| Black, non-Hispanic | 63.6 (3.5) | 64.0 (3.5) | 64.6 (3.7) | 76.4 (3.8) | 20.1c |
| Multiple race or other | 46.1 (4.4) | 48.1 (4.3) | 47.0 (4.2) | 44.4 (2.9) | −3.7 |
| Family income | |||||
| <100% FPL | 72.3 (3.3) | 69.2 (3.7) | 82.4 (4.9) | 82.9 (3.7) | 14.7c |
| 100%–199% FPL | 62.4 (3.1) | 61.8 (3.1) | 66.9 (3.5) | 69.7 (3.1) | 11.7 |
| 200%–299% FPL | 54.6 (3.0) | 56.8 (3.2) | 55.3 (3.6) | 58.4 (3.6) | 7.0 |
| 300%–399% FPL | 48.5 (3.7) | 54.0 (3.5) | 54.7 (4.6) | 58.3 (4.1) | 20.2c |
| ≥400% FPL | 38.9 (2.1) | 41.7 (2.4) | 44.2 (2.8) | 53.8 (2.6) | 38.3c |
| Highest household education | |||||
| Less than high school | 63.9 (3.7) | 53.7 (3.3) | 53.3 (4.7) | 70.4 (4.7) | 10.2 |
| High school diploma | 64.7 (2.9) | 59.6 (2.7) | 68.8 (3.7) | 64.8 (3.3) | 0.2 |
| Some college | 61.7 (2.2) | 64.9 (2.5) | 69.1 (3.2) | 74.2 (2.4) | 20.3c |
| College degree or higher | 37.7 (1.9) | 47.0 (2.0) | 49.5 (2.7) | 56.8 (2.1) | 50.7c |
| Family structure | |||||
| 2 parents | 43.7 (1.5) | 46.4 (1.6) | 50.1 (2.0) | 54.2 (1.7) | 24.0c |
| Single parent | 80.4 (3.7) | 74.5 (3.7) | 79.5 (4.3) | 86.4 (3.9) | 7.5 |
| Other | 62.9 (2.7) | 63.2 (2.4) | 68.5 (3.2) | 73.8 (3.0) | 17.3c |
Sample size is 2% lower for household education in 2001–2002, 2004–2005, and 2007–2008 and 1% lower in 2010–2011 because of missing data.
Parents could answer that their child had >1 condition contributing to activity limitation. Prevalence estimates reflect cases where the parent reported any neurodevelopmental or mental health condition.
Wald trend test P < .05, percent changes values calculated between 2001/2002 and 2010/2011
Changes in Severity of Disability
To assess whether a decline in severity coincided with the increase in disability prevalence over the study period, we examined changes in the proportion of children in fair or poor health and mean number of school absences due to illness or injury (Table 4). The percentage of children considered to be in fair or poor health in 2001–2002 (11.4%) was not statistically different from that in 2010–1011 (10.8%). On average, school-aged children with disabilities missed 7 days of school because of their health in both 2001–2002 and 2010–2011.
TABLE 4.
Severity of Chronic Conditions Associated With Limitations in Usual Activities Due to Chronic Conditions for US Children <Age 18, 2001–2002 and 2010–2011
| % in Fair or Poor Health (SE) | Mean No. of School Absences (SE) | |||||
|---|---|---|---|---|---|---|
| 2001–2002 (N = 3644) | 2010–2011 (N = 3867) | χ2 Pa | 2001–2002 (N = 1514) | 2010–2011 (N = 1555) | t Test Pa | |
| All conditions | 11.4 (0.6) | 10.8 (0.6) | NS | 7.1 (0.3) | 7.1 (0.6) | NS |
| Any physical health conditionb | 20.2 (1.5) | 24.3 (2.1) | NS | 9.3 (0.7) | 10.8 (1.9) | NS |
| Any neurodevelopmental or mental health conditionb | 9.5 (0.7) | 8.6 (0.6) | NS | 6.4 (0.3) | 6.1 (0.4) | NS |
| Other, not classifiable | 27.0 (2.3) | 27.8 (2.4) | NS | 13.2 (1.8) | 15.6 (3.8) | NS |
Statistical significance set at P < .05.
Parents could answer that their child had >1 condition contributing to activity limitation. Estimates reflect cases where the parent reported any physical health condition or any neurodevelopmental or mental health condition.
Discussion
This analysis of NHIS provides an up-to-date picture of child disability trends across condition and sociodemographic groups. Over the decade (2001–2011), the prevalence of parent-reported disability in childhood rose by >15%, with nearly a million more children reported as having disabilities. This analysis also documents 2 factors that contributed to the trends identified. First is the substantial rise in disabilities associated with neurodevelopmental or mental health conditions. Second is the unexpected finding that increasing rates were especially high among children from more advantaged households.
Partitioning the 15% overall increase in disability by diagnostic categories, we found a nearly 21% increase in disabilities related to neurodevelopmental or mental health conditions. The causes of the increases in neurodevelopmental or mental health problems are most certainly multifactorial, including biologic, familial, social, and cultural factors. For example, diagnostic shifts may partially explain why there was a decrease in learning disabilities but an increase in other neurodevelopmental or mental health problems.18 Data from the US Department of Education are consistent with this finding: A Thomas B. Fordham Institute study found that there have been substantial shifts over time in how children qualify for special education services.19 There have also been changes in diagnostic labeling and thresholds; for example, a child formerly considered distractible may now be seen as diagnosable by parents, teachers, and health professionals.20–22 Although cases of autism are not identifiable in the NHIS data, it is likely that the increasing prevalence of autism may explain some of the rise in neurodevelopmental or mental health problems.23,24 The relationship between autism and higher parental education and older maternal age25 may also help explain why the most pronounced increases in disability are among advantaged families. The increase in neurodevelopmental or mental health conditions was especially high among young children, a finding that may be attributed to increased awareness of these conditions and the need for a specific diagnosis to receive services such as early intervention.20,23
The divergence by sociodemographic status in the rate at which disability increased was not expected. During the first 40 years of the NHIS, disability rates increased at similar rates for all income groups, with a clear social gradient where children from lower-income families were reported to have higher levels of activity limitations.7 However, between 2001 and 2011 we found a differential increase among more advantaged groups of children. This trend held whether advantage is measured by family income, parental education, or family structure. Disadvantaged children continue to have higher absolute rates of disability, which is consistent with other studies and known risk factors.26–30 However, more advantaged children had a greater relative increases in the prevalence of disability over the study period. For example, disability rates among children in households at >400% of the poverty level rose 28% over the decade, more than twice the rate of growth seen for children in households living below the poverty line.
Several factors might explain why the rise in disability was more pronounced among advantaged families. Expanded use of diagnostic and treatment services may explain why more children are identified with disabilities. More advantaged families tend to have better access to care.31–34 Therefore, the differential growth in disability may be influenced in part by the connection between diagnosis and receipt of services or accommodations. Parent-identified need is associated with a greater likelihood of seeking out services.35,36 There may also be social differences that make seeking out a diagnosis, especially for mental health conditions, more acceptable among higher-income families.37,38
Furthermore, there may be undetected diagnostic biases contributing to the differential.39 Clinicians may be more inclined to label a child from a more advantaged background with a developmental or mental health diagnosis, or to provide a referral, despite the presence of symptoms or similar findings in the child from a disadvantaged household.40 Similarly, in the school setting providers may be influenced to provide more services by the higher-income parents, who tend to be more involved in the Individualized Education Program process than other parents.41 Greater acceptance of mental health diagnoses by more advantaged parents, coupled with persistent diagnostic biases, may help explain the trends identified by this research.
This article raises a number of important issues. There is a strong need to conduct research to determine how changes in the physical and social environments of children influence trends in health and disability and how children from different social and economic groups are differentially influenced by these trends. Such research should include examining children’s exposures to stress and other social and physical environmental threats that may especially affect neurodevelopmental health and function. There is also need for greater clarity on the concept of disability so that it can be measured and compared across studies and longitudinally. Without stability in diagnostic criteria (autism is a perfect example of shifting diagnostic criteria18) and agreement about the definition of disability, it is challenging to untangle the causes of the rise of disability. Additional research is necessary to assess the impacts of changing diagnostic labels and thresholds, evolving cultural views of health and disability, variable access to health services, the contribution of provider biases, and the incentive for a diagnosis to receive services. Cross-sectional surveys such as the NHIS are not suitable for addressing these causal questions. Mixed-method studies that combine the strengths of qualitative and quantitative research could improve our understanding of the factors influencing disability trends. Additionally, longitudinal cohort studies such as the National Children’s Study, which will follow a large sample of children from birth into adulthood,42 offer improved prospects for understanding these trends.
This study has several strengths, including a large, nationally representative sample, the ability to examine trends in disability and associated health conditions, an inclusive definition of disability, and multiple points of analysis over a decade. Despite these strengths, this research has notable limitations. First, the data on disability categories are limited to those that have been used in the NHIS, which does not encompass the full breadth of the disability experience and does not allow cross-survey comparisons. Second, results cannot be reliably compared with the NHIS before 2001 because the questionnaire items were changed in 2001. It is important to acknowledge a wording change in 2011 from mental retardation to intellectual disability (the now accepted term), which may have contributed to the rise in prevalence between 2010 and 2011, although eliminating the 2011 data from the analyses did not change the trends identified (data not shown). Third, the classification of conditions is limited by the 14 response options provided in the NHIS and is based on parent report, not clinical information. Our classification of these 14 options into physical health conditions versus neurodevelopmental or mental health conditions may oversimplify some conditions, especially those with both physical and neurodevelopment features. For example, we do not know how a parent with a child with complex condition such as cerebral palsy (not specified in the 14 options) would have responded.
Conclusions
The presence of parent-reported disability associated with chronic health conditions in childhood is on the rise. Between 2001 and 2011 there has been a decline in disability related to conditions that were classified as physical and a large increase in disability related to conditions that were classified as neurodevelopmental or mental health in nature, especially for children living in sociodemographically advantaged families. The consequences of these trends are profound and certainly affect how pediatricians and mental health professionals practice and prepare to address the needs of their patients. The health care system, including the payment structure for service delivery, must be nimble enough to accommodate the changing face of childhood disability and ensure access to high-quality care so that children are enabled to reach their full potential. Although additional research is necessary, documenting changes in the prevalence of childhood disability is an important step in developing better prevention and treatment strategies, refining how we study disability, and determining how to create and deliver services to best meet the needs of children.
Glossary
- CDC
Centers for Disease Control and Prevention
- FPL
federal poverty level
- NCHS
National Center for Health Statistics
- NHIS
National Health Interview Survey
Footnotes
Dr Houtrow participated in the conceptualization and analysis plan design, interpreting the results, drafting the manuscript, and revising per contributing authors’ recommendations; Dr Larson participated in the conceptualization and analysis plan design, conducting the analyses, interpreting the results, and editing the manuscript; Dr Olson participated in addressing methodologic concerns, interpreting the results, and editing the manuscript; Drs Newacheck and Halfon participated in the conceptualization and analysis plan design, interpreting the results, and editing the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Houtrow was funded by National Institutes of Health National Institute Child Health Development, Rehabilitation Medicine Scientists Training Program K12 H133B031102. Dr Halfon was funded by Department of Health and Human Services, Maternal and Child Health Bureau T76MC000141900. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Katz JA, Capua T, Bocchini JA, Jr. Update on child and adolescent immunizations: selected review of US recommendations and literature. Curr Opin Pediatr. 2012;24(3):407–421 [DOI] [PubMed] [Google Scholar]
- 2.Allen MC, Cristofalo EA, Kim C. Outcomes of preterm infants: morbidity replaces mortality. Clin Perinatol. 2011;38(3):441–454 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) . Ten great public health achievements: United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(19):619–623 [PubMed] [Google Scholar]
- 4.van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. 2011;8(1):50–60 [DOI] [PubMed] [Google Scholar]
- 5.Mogayzel PJ, Jr, Naureckas ET, Robinson KA, et al. Pulmonary Clinical Practice Guidelines Committee . Cystic fibrosis pulmonary guidelines. Chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2013;187(7):680–689 [DOI] [PubMed] [Google Scholar]
- 6.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127(6):1034–1042 [DOI] [PubMed] [Google Scholar]
- 7.Newacheck PW, Budetti PP, Halfon N. Trends in activity-limiting chronic conditions among children. Am J Public Health. 1986;76(2):178–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630 [DOI] [PubMed] [Google Scholar]
- 9.Halfon N, Houtrow A, Larson K, Newacheck PW. The changing landscape of disability in childhood. Future Child. 2012;22(1):13–42 [DOI] [PubMed] [Google Scholar]
- 10.National Health Interview Survey: The principle source of information on the health of the U.S. population. National Center for Health Statistics, Division of Health Interview Statistics. Hyattsville, MD. 2010. Available at: www.cdc.gov/nchs/data/nhis/brochure2010January.pdf. Accessed July 17, 2014
- 11.Bloom B, Cohen RA, Freeman G. Summary health statistics for US children: National Health Interview Survey. Vital Health Stat 10. 2010;247:1–80 [PubMed] [Google Scholar]
- 12.Dey AN, Schiller JS, Tai DA. Summary health statistics for U.S. children: National Health Interview Survey, 2002. National Center for Health Statistics. Vital Health Statistics 10 (221). 2004 [PubMed] [Google Scholar]
- 13.Simeonsson RJ, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. Applying the International Classification of Functioning, Disability and Health (ICF) to measure childhood disability. Disabil Rehabil. 2003;25(11–12):602–610 [DOI] [PubMed] [Google Scholar]
- 14.Division of Health Interview Statistics, National Center for Health Statistics 2004 National Health Interview Survey Public Use Data Release. Hyattsville, MD: Author; 2005 [Google Scholar]
- 15.Botman SL, Moore TF, Moriarity CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. National Center for Health Statistics 2000. Vital Health Stat 2. 2004;130:i–33 [Google Scholar]
- 16.Division of Health Interview Statistics of the National Center for Health Statistics. Questionnaires, datasets, and related documentation 1997 to the present. 2012. Available at: www.cdc.gov/NCHS/nhis/quest_data_related_1997_forward.htm
- 17.StataPress Stata Base Reference Manual. College Station, TX: Stata Press; 2009 [Google Scholar]
- 18.Halfon N, Kuo AA. What DSM-5 could mean to children with autism and their families. JAMA Pediatr. 2013;167(7):608–613 [DOI] [PubMed] [Google Scholar]
- 19.Scull J, Winkler AM. Shifting Trends in Special Education. Washington, DC: Thomas B. Fordham Institute; 2011 [Google Scholar]
- 20.Leonard H, Dixon G, Whitehouse AJO, et al. Unpacking the complex nature of the autism epidemic. Res Autism Spectr Disord. 2010;4(4):548–554 [Google Scholar]
- 21.Sclar DA, Robison LM, Bowen KA, Schmidt JM, Castillo LV, Oganov AM. Attention-deficit/hyperactivity disorder among children and adolescents in the United States: trend in diagnosis and use of pharmacotherapy by gender. Clin Pediatr (Phila). 2012;51(6):584–589 [DOI] [PubMed] [Google Scholar]
- 22.Robison LM, Skaer TL, Sclar DA, Galin RS. Is attention deficit hyperactivity disorder increasing among girls in the US? Trends in diagnosis and the prescribing of stimulants. CNS Drugs. 2002;16(2):129–137 [DOI] [PubMed] [Google Scholar]
- 23.Hertz-Picciotto I, Delwiche L. The rise in autism and the role of age at diagnosis. Epidemiology. 2009;20(1):84–90. doi:10.1097/EDE.0b013e3181902d15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schieve LA, Rice C, Yeargin-Allsopp M, et al. Parent-reported prevalence of autism spectrum disorders in US-born children: an assessment of changes within birth cohorts from the 2003 to the 2007 National Survey of Children’s Health. Matern Child Health J. 2012;16(Suppl 1):S151–S157 [DOI] [PubMed] [Google Scholar]
- 25.Windham GC, Anderson MC, Croen LA, Smith KS, Collins J, Grether JK. Birth prevalence of autism spectrum disorders in the San Francisco Bay area by demographic and ascertainment source characteristics. J Autism Dev Disord. 2011;41(10):1362–1372 [DOI] [PubMed] [Google Scholar]
- 26.Perou R, Bitsko RH, Blumberg SJ, et al. Centers for Disease Control and Prevention (CDC) . Mental health surveillance among children: United States, 2005–2011. MMWR Surveill Summ. 2013;62(suppl 2):1–35 [PubMed] [Google Scholar]
- 27.Blackburn CM, Spencer NJ, Read JM. Prevalence of childhood disability and the characteristics and circumstances of disabled children in the UK: secondary analysis of the Family Resources Survey. BMC Pediatr. 2010;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simkiss DE, Blackburn CM, Mukoro FO, Read JM, Spencer NJ. Childhood disability and socio-economic circumstances in low and middle income countries: systematic review. BMC Pediatr. 2011;11:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stein REK. Measurement of children’s health. Ambul Pediatr. 2004;4(4 suppl):365–370 [DOI] [PubMed] [Google Scholar]
- 30.Newacheck PW, Stein RE, Bauman L, Hung YY, Research Consortium on Children With Chronic Conditions . Disparities in the prevalence of disability between black and white children. Arch Pediatr Adolesc Med. 2003;157(3):244–248 [DOI] [PubMed] [Google Scholar]
- 31.Coker TR, Elliott MN, Kataoka S, et al. Racial/ethnic disparities in the mental health care utilization of fifth grade children. Acad Pediatr. 2009;9(2):89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Larson K, Halfon N. Family income gradients in the health and health care access of US children. Matern Child Health J. 2010;14(3):332–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Silver EJ, Stein RE. Access to care, unmet health needs, and poverty status among children with and without chronic conditions. Ambul Pediatr. 2001;1(6):314–320 [DOI] [PubMed] [Google Scholar]
- 34.Hambidge SJ, Emsermann CB, Federico S, Steiner JF. Disparities in pediatric preventive care in the United States, 1993–2002. Arch Pediatr Adolesc Med. 2007;161(1):30–36 [DOI] [PubMed] [Google Scholar]
- 35.Banta JE, James S, Haviland MG, Andersen RM. Race/ethnicity, parent-identified emotional difficulties, and mental health visits among California children. J Behav Health Serv Res. 2013;40(1):5–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller TW, Nigg JT, Miller RL. Attention deficit hyperactivity disorder in African American children: what can be concluded from the past ten years? Clin Psychol Rev. 2009;29(1):77–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zimmerman FJ. Social and economic determinants of disparities in professional help-seeking for child mental health problems: evidence from a national sample. Health Serv Res. 2005;40(5 pt 1):1514–1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bailey RK, Ali S, Jabeen S, et al. Attention-deficit/hyperactivity disorder in African American youth. Curr Psychiatry Rep. 2010;12(5):396–402 [DOI] [PubMed] [Google Scholar]
- 39.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 Suppl):I140–I151 [DOI] [PubMed] [Google Scholar]
- 40.Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2). Available at: www.pediatrics.org/cgi/content/full/115/2/e183 [DOI] [PubMed] [Google Scholar]
- 41.Wagner M, Newman L, Cameto R, Jarvitz H, Valdes K. A national picture of parent and youth participation in IEP and transition planning meetings. J Disabil Policy Stud. 2012;23:140–155 [Google Scholar]
- 42.Hirschfeld S, Kramer B, Guttmacher A. Current status of the National Children’s Study. Epidemiology. 2010;21(5):605–606 [DOI] [PubMed] [Google Scholar]


