Abstract
Objective:
This study was aimed to evaluate and to compare the push-out bond strength of different brands of mineral trioxide aggregate (MTA) with a calcium enriched mixture cement (CEM).
Materials and Methods:
Fifteen extracted, single-rooted human teeth were used. The middle-third of the roots were sliced perpendicular to the long axis into 1.00 ± 0.05 mm thick serial slices (15 root × 4 slice = 60 specimen). The specimens were then divided into three groups (n = 20). The standardized root discs were filled with white CEM, ProRoot MTA, MTA-Angelus and wrapped in a serum-soaked gauze. After 3 days at relative humidity, the push-out bond strengths were measured with a universal testing machine. Data were analyzed using one-way analysis of variance and post hoc Tukey tests.
Results:
The mean push-out bond strength value of the ProRoot MTA group (12.7 ± 2.5 MPa) was the highest and statistically significant difference was recorded between ProRoot MTA and other groups (P < 0.001). There was no significant difference between the mean bond strength of CEM cement (4.6 ± 1.1 MPa) and MTA-Angelus (4.5 ± 1.5 MPa) (P = 0.982).
Conclusion:
The push-out bond strength of MTA was changed with the brands and ProRoot MTA had the highest push-out bond strength.
Keywords: Calcium enriched mixture cement, mineral trioxide aggregate-angelus, ProRoot mineral trioxide aggregate, push-out bond strength
INTRODUCTION
Marginal adaptation and bond strength of root-end filling materials are among crucial factors for endodontic success, because most endodontic failures arise from leakage of irritants into the periapical tissues.[1,2,3,4] Calcium silicate cement, e.g. mineral trioxide aggregate (MTA) is an endodontic cement that is extremely biocompatible, capable of stimulating healing and osteogenesis and has been widely used for pulp capping,[5] treatment of root perforations,[6,7] root-end filling material during apical surgery,[8] orthograde root canal filling before apical surgery,[9] apical barrier formations on nonvital teeth with open apices,[10] treatment of large periapical lesion,[11] and root canal filling material.[12] Despite the favorable results that support its clinical use, there are some disadvantages when using calcium silicate cements so new and more useful material need is continuing. MTA-Angelus and calcium enriched mixture (CEM)[13,14] cement are two of these materials. MTA-Angelus is composed of calcium carbonate, calcium silicate, calcium aluminate, and barium zinc phosphate than conventional MTA, which contribute to improve setting time and workability.[15,16] Recently, a new calcium silicate cements (CSS) material, CEM cement has been introduced. CEM cement is a new product and contains different chemical components. The major components of the powder are 51.75% wt. calcium oxide (CaO), 9.53% wt. SO3, 8.49% wt. P2O5, 6.32% wt. SiO2, and minor components are Al2O3 > Na2O > MgO > Cl,[14] CEM has similar clinical uses to MTA as well as similar pH, working time and dimensional changes. According to manufacturer description CEM is composed of different chemicals and has the advantage of shorter setting time, increased flow, and decreased film thickness.[17]
Researches on the physicochemical interaction between MTA-based products and root canal walls indicated that MTA was a bioactive material[18,19] and appeared to chemically bond to dentin through a diffusion-controlled reaction between its apatitic surface and dentin.[19,20]
There are various several methods for evaluating the adhesion of dental material to dentin. These are tensile, shear, and push-out strength tests.[21,22,23,24] The push-out test is based on shear stresses, which occur in clinical conditions and can be imitated by this test method.[25] As the push-out test generates parallel fractures in the interfacial area of the dentin-bonding, it presents a better method to evaluate bond strength than conventional tests.[26]
Few studies in the literature have evaluated the bond strength of MTA-based materials. ProRoot MTA and MTA-Angelus are the preferred products on the market, whereas CEM cement[13] is a new product and contains different chemical components. In the light of these information's the aim of this study was to evaluate and compare the push-out bond strengths of ProRoot MTA, MTA-Angelus, and CEM cement.
MATERIALS AND METHODS
Preparation of specimens
Fifteen single-rooted, freshly extracted human teeth with mature apices were selected for this study. The middle-third of the roots were sectioned perpendicular to the long axis into 1.00 ± 0.05 mm thick serial slices (15 root × 4 slice = 60 specimen) using a water-cooled diamond blade on a cutting machine (Isomet, Buhler, Lake Bluff, NY, USA). The root slices were drilled with post drills (Exacto, Angelus, Londrina, PR, Brazil) perpendicular to the root slice to obtain 1.3-mm diameter standardized cavities. The specimens were then randomly divided into three groups (n = 20). The standardized root slices were filled with white ProRoot MTA (Dentsply/Tulsa Dental, Tulsa, OK, USA-04.2015, lot12001879), MTA - Angelus (Angelus, Londrina, PR, Brazil-04.2014, lot 17975), and CEM (BioniqueDent, Tehran, Iran-01.2014, lot C100501) cement. The specimens wrapped in pieces of gauze soaked in serum and were kept for 3 days at 37°C to set.
Each group was placed in a separate closed plastic container. Saline-soaked pieces of jaconet were replaced daily to maintain a sufficient moist environment within the closed plastic container.
Push-out test
The push-out bond strengths were measured using a universal testing machine (Instron, Norwood, USA). The fillings were loaded with a 1-mm diameter cylindrical stainless steel plunger at a speed of 1 mm/min [Figure 1]. When dislodgement occurred, the maximum load applied to the fillings was recorded in Newtons. The recorded value was converted to Mpa using the following formula: Newtons/(2 prh), where P is the constant π, r is the root canal radius, and h is the thickness of the root slice in millimeters.
Figure 1.
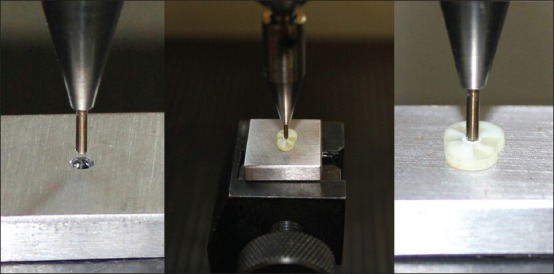
Push-out test design
The slices were then examined under a light microscope at ×25 magnification to determine the mode of the bond failure. Each sample was recorded in one of three failure modes: Adhesive failure that occurred at the cement and dentin interface, cohesive failure that occurred within the cement, and mixed failure. Data were analyzed using one-way analysis of variance (ANOVA) and post hoc Tukey tests. The differences between modes of failure were analyzed using Fisher's exact test.
RESULTS
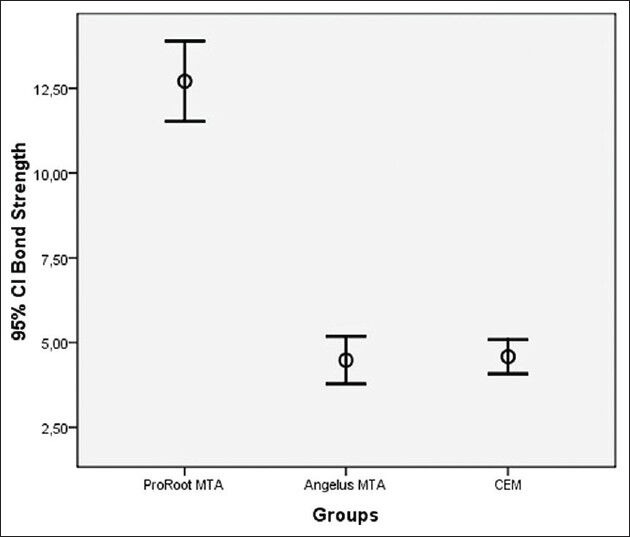
One-way ANOVA test showed significant differences between the groups (P < 0.001). Mean bond strengths and standard deviations of groups were: 12.7 ± 2.5 for ProRoot MTA, 4.6 ± 1.1 for CEM cement, and 4.5 ± 1.5 for MTA-Angelus [Table 1]. The mean push-out bond strength value of the ProRoot MTA group was a higher than the other groups (P < 0.001). There was no significant difference between the mean bond strength of the CEM cement and MTA-Angelus (P = 0.982) [Figure 2]. Fisher's exact test revealed that the bond failure modes were not significantly different for all experimental groups (P > 0.001).
Table 1.
Means and SD of groups
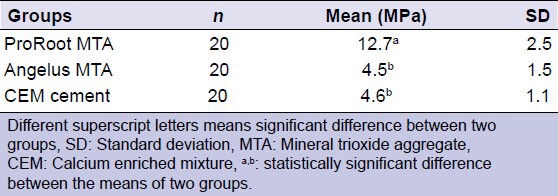
Figure 2.
Error bar chart of the group means with the 95% confidence interval
DISCUSSION
An ideal orthograde or retrograde filling material should seal to the root-end cavity wall and surrounding tissue, be able to prevent bacterial leakage from the periradicular tissues, and resist dislodging forces. MTA possesses most of these properties, and is the “golden” standard for root-end filling[27] and perforation repair material due to its sealing ability.[28] In addition, bond strength of MTA is important, as normal tooth functioning can dislodge the material. Although, there are various methods to evaluate the adhesion of MTA, the push-out test gives efficient and reliable results.[29] In our study, the push-out test method was used to test the bond strength of the materials.
Moistening MTA during setting is particularly important.[30] MTA has greater comprehensive strength when kept in a moist environment for 2-7 days, rather than only 4 h.[15] In addition, the retention characteristic and push-out strength of MTA increases by the time if kept under moist conditions.[30] And also moistening of MTA at least the first 3 days is more important for dislodging forces.[30] We incubated all samples in a moist environment for 72 h.
In the present study, the push-out strength of three brands of white MTA was evaluated for the first time. The analysis of the mean push-out strength values of each brand revealed that there were significant differences between the groups (P < 0.001). In this study, the ProRoot MTA group showed the highest bond strength among groups.
The setting reaction of MTA requires wet environment.[31] The sealing ability of MTA may be raised by its bioactivity and apatite-formation capacity.[31] Gandolfi et al.[32] demonstrated that the kinetics of the apatite-formation on MTA cements when in contact with P-containing fluids and that such property is improved if the cement contains phosphorous.[32] Alpha-tricalcium phosphate (TCP) improves the apatite-formation ability of calcium silicate hydraulic cement soaked in phosphate solutions.[33]
It has been demonstrated that the presence of phosphorous in MTA cements improve the ability to form apatite.[32] However, the phosphorus is 0.22% in MTA, 8.52% in CEM.[14] We might say the phosphorus is lower in MTA than CEM. And also fluoride delays the setting time, increases the expansion and adhesion of MTA.[31,34] These components may be related to the increase of the push-out bond strength of the ProRoot MTA.
Mineral trioxide aggregate cements, which are used as root-end filling materials, are directly in contact with alveolar bone.[31] The osteoconductive activity is important for new bone tissue formation.[35] Sodium fluoride was introduced into the formulation of MTA cements to improve their biological behavior due to its good biological activity on osteoblast cells.[31] It has been demonstrated that the presence of fluoride in MTA cements improves the expansion of MTA cements[31,34] and that the presence of phosphorous improves the ability to form apatite.[32] Alpha-TCP improves the apatite-formation ability of calcium silicate hydraulic cement soaked in phosphate solutions.[33]
It is important to understand that the physical and chemical components in MTA can adversely affect setting time and the compressive strength of the material.[36,37] ProRoot MTA contains tricalcium silicate, bismuth oxide (Bi2O3), dicalcium silicate, tricalcium aluminate, tetracalcium aluminoferrite, and calcium sulfate dihydrate. MTA-Angelus contains 80% Portland cement and 20% Bi2O3. MTA-Angelus does not contain calcium sulfate, TiO2, P2O5, FeO. The results of the MTA-Angelus were found lower than ProRoot MTA in the present study. It might be explained by some distribution differences between the heavy metals content of two materials [Table 2].[38] It should be studied with other studies with environmental scanning electron microscopy with energy dispersive X-ray and micro-Raman spectroscopy before clinical application.
Table 2.
Composition of ProRoot MTA, MTA-Angelus and CEM cement
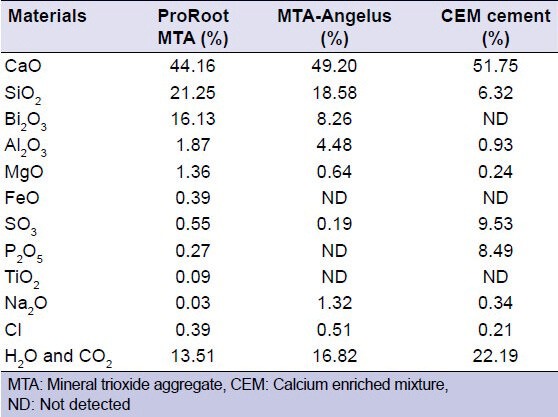
Calcium enriched mixture cement contains CaO, calcium phosphate, calcium carbonate, calcium silicate, calcium sulfate, calcium hydroxide, and calcium chloride. Asgary et al.[14] compared the main components of ProRoot MTA with CEM cement and found the proportion of the ingredients was different and TiO2 and Bi2O3 was not detected in CEM. And also the predominant elements of ProRoot MTA were calcium, silicon, and bismuth but the predominant elements of CEM cement were calcium, sulfur, phosphorus, and silicon.[14] They indicated that CEM has similar clinical applications as MTAs, but different chemical compositions and distribution.[14] These chemical compositions and distribution difference between CEM and MTA might explain the result of the difference between CEM cement and ProRoot MTA in this study.
CONCLUSION
ProRoot MTA had higher push-out bond strength than MTA-Angelus and CEM cement.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: Systematic review of the literature - Part 2. Influence of clinical factors. Int Endod J. 2008;41:6–31. doi: 10.1111/j.1365-2591.2007.01323.x. [DOI] [PubMed] [Google Scholar]
- 2.Hoen MM, Pink FE. Contemporary endodontic retreatments: An analysis based on clinical treatment findings. J Endod. 2002;28:834–6. doi: 10.1097/00004770-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Siqueira JF, Jr, Rôças IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod. 2008;34:1291–13013. doi: 10.1016/j.joen.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 4.Torabinejad M, Pitt Ford TR. Root end filling materials: A review. Endod Dent Traumatol. 1996;12:161–78. doi: 10.1111/j.1600-9657.1996.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 5.Petrou MA, Alhamoui FA, Welk A, Altarabulsi MB, Alkilzy M, H, Splieth C. randomized clinical trial on the use of medical Portland cement, MTA and calcium hydroxide in indirect pulp treatment. J Clin Oral Invest. 2013 doi: 10.1007/s00784-013-1107-z. doi: 10.1007/s00784-013-1107-z. [DOI] [PubMed] [Google Scholar]
- 6.Main C, Mirzayan N, Shabahang S, Torabinejad M. Repair of root perforations using mineral trioxide aggregate: A long-term study. J Endod. 2004;30:80–3. doi: 10.1097/00004770-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Unal GC, Maden M, Isidan T. Repair of furcal iatrogenic perforation with mineral trioxide aggregate: Two years follow-up of two cases. Eur J Dent. 2010;4:475–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Torabinejad M, Hong CU, Lee SJ, Monsef M, Pitt Ford TR. Investigation of mineral trioxide aggregate for root-end filling in dogs. J Endod. 1995;21:603–8. doi: 10.1016/S0099-2399(06)81112-X. [DOI] [PubMed] [Google Scholar]
- 9.Habibi M, Ghoddusi J, Habibi A, Mohtasham N. Healing process following application of set or fresh mineral trioxide aggregate as a root-end filling material. Eur J Dent. 2011;5:19–23. [PMC free article] [PubMed] [Google Scholar]
- 10.Camp JH. Diagnosis dilemmas in vital pulp therapy: Treatment for the toothache is changing, especially in young, immature teeth. J Endod. 2008;34:S6–12. doi: 10.1016/j.joen.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Yildirim T, Gencoglu N. Use of mineral trioxide aggregate in the treatment of large periapical lesions: Reports of three cases. Eur J Dent. 2010;4:468–74. [PMC free article] [PubMed] [Google Scholar]
- 12.Hayashi M, Shimizu A, Ebisu S. MTA for obturation of mandibular central incisors with open apices: Case report. J Endod. 2004;30:120–2. doi: 10.1097/00004770-200402000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Asgary patent. Endodontic filling material. US2008/0206716. 2008 [Google Scholar]
- 14.Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S. The properties of a new endodontic material. J Endod. 2008;34:990–3. doi: 10.1016/j.joen.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature review - Part I: Chemical, physical, and antibacterial properties. J Endod. 2010;36:16–27. doi: 10.1016/j.joen.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature review - Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36:400–13. doi: 10.1016/j.joen.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J. 2009;35:147–52. doi: 10.1111/j.1747-4477.2008.00137.x. [DOI] [PubMed] [Google Scholar]
- 18.Gandolfi MG, Taddei P, Tinti A, Prati C. Apatite-forming ability (bioactivity) of ProRoot MTA. Int Endod J. 2010;43:917–29. doi: 10.1111/j.1365-2591.2010.01768.x. [DOI] [PubMed] [Google Scholar]
- 19.Gandolfi MG, Taddei P, Modena E, Siboni F, Prati C. Biointeractivity-related versus chemi/physisorption-related apatite precursor-forming ability of current root end filling materials. J Biomed Mater Res B Appl Biomater. 2013;101:1107–23. doi: 10.1002/jbm.b.32920. [DOI] [PubMed] [Google Scholar]
- 20.Gandolfi MG, Taddei P, Siboni F, Modena E, Ciapetti G, Prati C. Development of the foremost light-curable calcium-silicate MTA cement as root-end in oral surgery. Chemical-physical properties, bioactivity and biological behavior. Dent Mater. 2011;27:e134–57. doi: 10.1016/j.dental.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Shokouhinejad N, Nekoofar MH, Iravani A, Kharrazifard MJ, Dummer PM. Effect of acidic environment on the push-out bond strength of mineral trioxide aggregate. J Endod. 2010;36:871–4. doi: 10.1016/j.joen.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 22.Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod. 2010;36:286–91. doi: 10.1016/j.joen.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Huffman BP, Mai S, Pinna L, Weller RN, Primus CM, Gutmann JL, et al. Dislocation resistance of ProRoot Endo Sealer, a calcium silicate-based root canal sealer, from radicular dentine. Int Endod J. 2009;42:34–46. doi: 10.1111/j.1365-2591.2008.01490.x. [DOI] [PubMed] [Google Scholar]
- 24.Iacono F, Gandolfi MG, Huffman B, Sword J, Agee K, Siboni F, et al. Push-out strength of modified Portland cements and resins. Am J Dent. 2010;23:43–6. [PubMed] [Google Scholar]
- 25.Sudsangiam S, van Noort R. Do dentin bond strength tests serve a useful purpose? J Adhes Dent. 1999;1:57–67. [PubMed] [Google Scholar]
- 26.Drummond JL, Sakaguchi RL, Racean DC, Wozny J, Steinberg AD. Testing mode and surface treatment effects on dentin bonding. J Biomed Mater Res. 1996;32:533–41. doi: 10.1002/(SICI)1097-4636(199612)32:4<533::AID-JBM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 27.Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25:197–205. doi: 10.1016/S0099-2399(99)80142-3. [DOI] [PubMed] [Google Scholar]
- 28.Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008;34:660–5. doi: 10.1016/j.joen.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, et al. The adhesion between fiber posts and root canal walls: Comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112:353–61. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 30.Gancedo-Caravia L, Garcia-Barbero E. Influence of humidity and setting time on the push-out strength of mineral trioxide aggregate obturations. J Endod. 2006;32:894–6. doi: 10.1016/j.joen.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Gandolfi MG, Taddei P, Siboni F, Modena E, Ginebra MP, Prati C. Fluoride-containing nanoporous calcium-silicate MTA cements for endodontics and oral surgery: Early fluorapatite formation in a phosphate-containing solution. Int Endod J. 2011;44:938–49. doi: 10.1111/j.1365-2591.2011.01907.x. [DOI] [PubMed] [Google Scholar]
- 32.Gandolfi MG, Taddei P, Tinti A, De Stefano Dorigo E, Rossi PL, Prati C. Kinetics of apatite formation on a calcium-silicate cement for root-end filling during ageing in physiological-like phosphate solutions. Clin Oral Investig. 2010;14:659–68. doi: 10.1007/s00784-009-0356-3. [DOI] [PubMed] [Google Scholar]
- 33.Gandolfi MG, Taddei P, Tinti A, De Stefano Dorigo E, Prati C. Alpha-TCP improves the apatite-formation ability of calcium-silicate hydraulic cement soaked in phosphate solutions. Mater Sci Eng C Mater Biol Appl. 2011;31:1412–22. [Google Scholar]
- 34.Gandolfi MG, Iacono F, Agee K, Siboni F, Tay F, Pashley DH, et al. Setting time and expansion in different soaking media of experimental accelerated calcium-silicate cements and ProRoot MTA. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e39–45. doi: 10.1016/j.tripleo.2009.07.039. [DOI] [PubMed] [Google Scholar]
- 35.Lau KH, Baylink DJ. Molecular mechanism of action of fluoride on bone cells. J Bone Miner Res. 1998;13:1660–7. doi: 10.1359/jbmr.1998.13.11.1660. [DOI] [PubMed] [Google Scholar]
- 36.Watts JD, Holt DM, Beeson TJ, Kirkpatrick TC, Rutledge RE. Effects of pH and mixing agents on the temporal setting of tooth-colored and gray mineral trioxide aggregate. J Endod. 2007;33:970–3. doi: 10.1016/j.joen.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 37.Kogan P, He J, Glickman GN, Watanabe I. The effects of various additives on setting properties of MTA. J Endod. 2006;32:569–72. doi: 10.1016/j.joen.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 38.Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J, Kheirieh S, Brink F. Comparison of mineral trioxide aggregate's composition with Portland cements and a new endodontic cement. J Endod. 2009;35:243–50. doi: 10.1016/j.joen.2008.10.026. [DOI] [PubMed] [Google Scholar]


