Abstract
Objectives:
The objective of the following study is to evaluate the interaction between the resin materials used in immediate dentin sealing (IDS) techniques and impression materials with two different techniques to eliminate the oxygen-inhibition layer.
Materials and Methods:
The occlusal dentin surface of 35 human molars was exposed. The teeth were used in two Groups: Group 1 – Impression with Express XT; Group 2 – Impression with Impregum. Groups 1 and 2 were divided into 14 subgroups: Groups 1a and 2a – Control groups; 1b and 2b – IDS with Clearfil SE Bond (CSE); 1c and 2c – IDS with CSE + additional polymerization with glycerin jelly; 1d and 2d – IDS with CSE + alcohol; 1e and 2e – IDS with CSE and Protect Liner F (PLF); 1f and 2f – IDS with CSE and PLF + additional polymerization with glycerin jelly; and 1g and 2g – IDS with CSE and PLF + alcohol. Five teeth were used in each experimental group, and the tooth surface was photographed using a digital camera.
Results:
Small quantity of unpolymerized impression material remained attached to the CSE or to the PLF in Groups 1b and 1e. Groups 1c and 1d prevented the interaction. Small quantity of polymerized impression material remained attached to the CSE or to the PLF for Groups 2b and 2e. The same interaction was observed for Groups 2c and 2d. For Groups 2c and 2f, no interactions were observed.
Conclusion:
Resin materials interacted with impression materials. The application of glycerin jelly and alcohol prevented the interaction of CSE with Express XT and PLF with Impregum; however, these treatments were not completely effective in preventing the interaction of CSE with Impregum and PLF with Express XT.
Keywords: Immediate dentin sealing, impression materials, oxygen-inhibition layer
INTRODUCTION
During tooth preparation for indirect restorations such as inlays, onlays, veneers, and crowns, a significant area of dentin is exposed. To avoid problems such as dentin contamination by provisionalization[1,2] and hybridization failure sensitivity,[3] a technique called immediate dentin sealing (IDS) was suggested in the early 1990s.[4] This technique consists of the application of an adhesive system immediately after tooth preparation and before taking the impression. Another IDS technique was developed in which a sealing film is applied to the dentin surface immediately after tooth preparation using an adhesive system and a low-viscosity composite resin.[5,6] It is believed that this layer of low-viscosity composite resin isolates the underlying hybrid layer and consequently, aids in preserving the dentin seal.[7] Therefore, IDS techniques are based on the principle that adhesive systems bond better to freshly prepared dentin,[1,2] thus protecting the dentin – pulp complex and preventing or decreasing sensitivity and bacterial leakage during the provisional stage.[8,9]
When using the IDS techniques, the impression is taken after the application of the resin material on the dental substrate. This step is critical because the impression material can interact with the outer resin layer,[3] which is unpolymerized due to the oxygen-inhibition of the radicals that initiate the polymerization reaction.[10,11] Different techniques have been suggested to reduce or eliminate the oxygen-inhibition layer (OIL), such as the application of glycerin jelly followed by an additional light cure[12] or the use of a cotton pellet soaked in alcohol.[13] However, no study has compared these two techniques before an impression with vinyl polysiloxane and polyether.
The aim of this study was to qualitatively evaluate the interaction between the resin materials used in the IDS techniques and impression materials when two different techniques to reduce/eliminate the OIL are applied. This study was based on the hypothesis that these techniques do not eliminate the interaction between impression materials and resin materials.
MATERIALS AND METHODS
Thirty-five unerupted human third molars, which were extracted for therapeutic reasons, were obtained from the tooth bank after the approval of the Ethics Committee of the Pontifical Catholic University of Rio Grande do Sul. The teeth were cleaned of gross debris and stored in distilled water at 4°C. The water was changed every week, and the teeth were used in the study within 6 months. The roots were mounted in self-cured acrylic resin, and the occlusal enamel surface was removed with a diamond disc mounted in a low-speed laboratory cutting machine (Labcut 1010, Extec Corp., London, UK) under cooling conditions. The rest of the enamel was removed with 400-grit silicon carbide abrasive paper in a polishing machine (DPU-10, Panambra, São Paulo, SP, Brazil) under water. The superficial dentin was exposed and finished with 600-grit silicon carbide abrasive paper in the polishing machine, and a flat dentin surface was obtained.
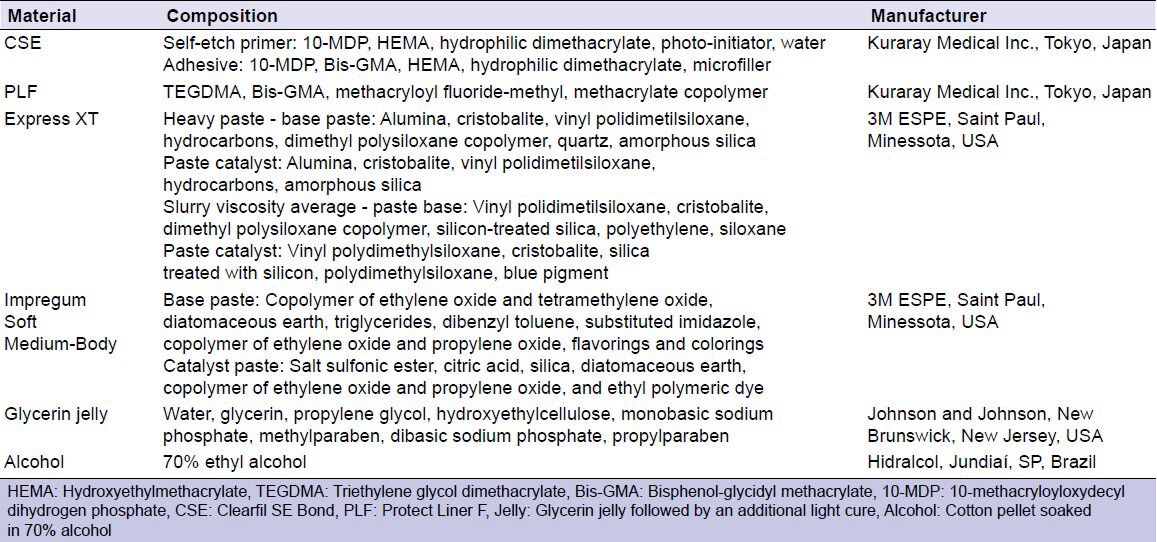
After polishing, the teeth were randomly divided into seven Groups (n = 5) to be used in Group 1 (Impression with Express XT). The teeth were used again for Group 2 (Impression with Impregum) after remotion of the resin material with 600-grit silicon carbide abrasive paper. Table 1 shows the materials used in the present study.
Table 1.
Materials used in the study
Express XT vinyl polysiloxane impression material was used in Group 1, and the following subgroups were assigned [Figure 1]:
Figure 1.
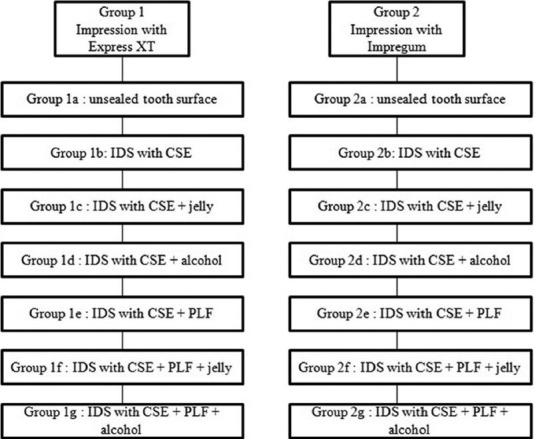
Schematic design of the experimental groups
Group 1a: Unsealed tooth surface
Group 1b: IDS with Clearfil SE Bond (CSE). SE Primer was first applied to the tooth surface for 20 s and gently air dried. SE Bond was then applied, mildly air dried, and light cured for 10 s using a conventional halogen light curing unit
Group 1c: IDS with CSE and glycerin jelly. The adhesive system was applied as described for Group 1b. The polymerization of the adhesive was followed by the application of an air-blocking barrier with glycerin jelly and was then light cured for an additional 10 s. The glycerin jelly was rinsed under running tap water
Group 1d: IDS with CSE and alcohol. The adhesive system was applied as described for Group 1b. The surface of the adhesive system was wiped with a cotton pellet soaked in 70% alcohol for 10 s
Group 1e: IDS with CSE and Protect Liner F (PLF). The adhesive system was applied as described for Group 1b. After application of the adhesive, PLF was placed on the adhesive surface using a brush-on technique and was then light cured for 20 s
Group 1f: IDS with CSE and PLF + glycerin jelly. Both materials were applied as described for Group 1e. The polymerization of the cured low-viscosity composite resin was followed by the application of an air-blocking barrier with glycerin jelly and light curing for an additional 10 s. The glycerin jelly was rinsed under running tap water
Group 1g: IDS with CSE and PLF + alcohol. Both materials were applied as described for Group 1e. The surface of the cured low-viscosity composite resin was wiped with a cotton pellet soaked in 70% alcohol for 10 s.
A monophase polyether Impregum was used in Group 2, and subgroups similar to Group 1 (2a, 2b, 2c, 2d, 2e, 2f, 2g) were assigned based on the materials and techniques used [Figure 1].
Individual trays with self-cured acrylic resin (JET – Clássico, São Paulo, SP, Brazil) were prepared. The adhesive was applied to the tray and was permitted to dry for 10 min. In Groups 1a to 1g, the putty/wash one-step technique was applied using Express XT. The light-body material was injected over the tooth surface. The tray was filled with the heavy-body material, and then the tray was placed over the tooth. In Groups 2a to 2g, the one-step technique was applied using Impregum. The medium-body material was injected over the tooth and in the tray, and the tray was placed over the tooth. The impression materials were allowed to set for 10 min before being removed from the tooth. Five impressions were taken for each group.
Each tooth surface was photographed using a digital camera Nikon Coolpix P100 (Nikon, Melville, NY, USA) with a TL3 model light source (Olympus, Center Valley, PA, USA). The images were saved in JPEG format and were used to examine the presence of unpolymerized and/or residual impression materials left on the treated tooth surface.
RESULTS
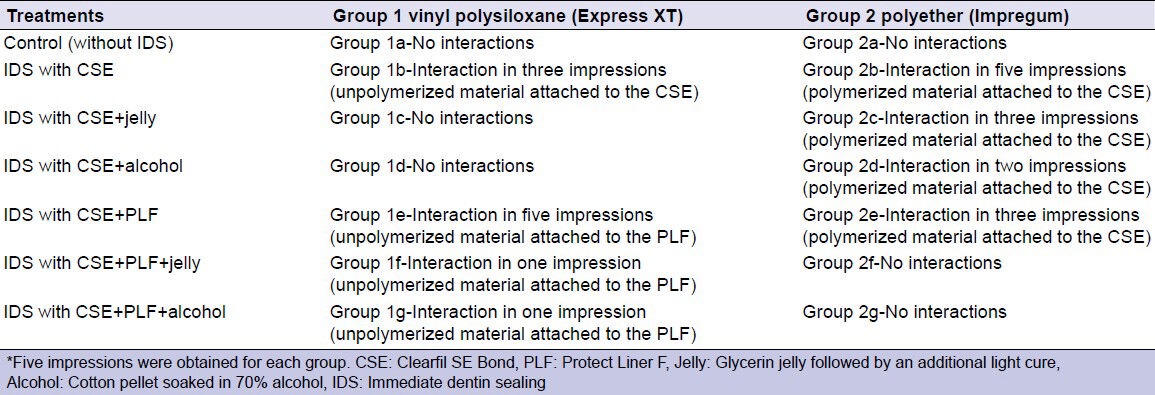
The interactions between the impression materials and the resin materials are described in Table 2.
Table 2.
Interactions between the impression materials and the resin materials
In the control groups (Groups 1a and 2a), no interaction was observed between the impression materials and the tooth structure [Figure 2].
Figure 2.
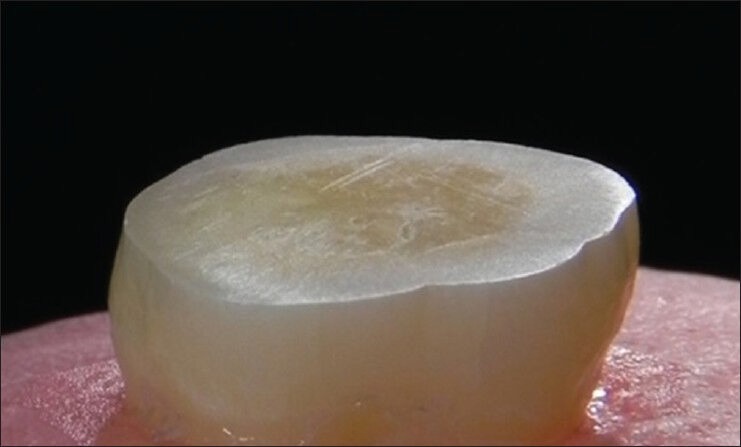
Photo of the tooth surface-Control group (without immediate dentin sealing) and impression with vinyl polysiloxane: There is no impression material attached to the dentin surface. The same was observed for polyether
For the vinyl polysiloxane impression material, the group that received IDS with the CSE (Group 1b) and the group with PLF (Group 1e) had observable interactions in three and five impressions, respectively. A small quantity of unpolymerized impression material remained attached to the adhesive system [Figure 3] or to the low-viscosity composite resin. The application of glycerin jelly followed by an additional light cure (Group 1c) and the use of cotton pellet soaked in alcohol (Group 1d) prevented the interaction between the vinyl polysiloxane and the adhesive system [Figure 4]. However, neither treatment was completely effective with the low-viscosity composite resin, as a small quantity of unpolymerized impression material remained attached to the PLF in one impression.
Figure 3.
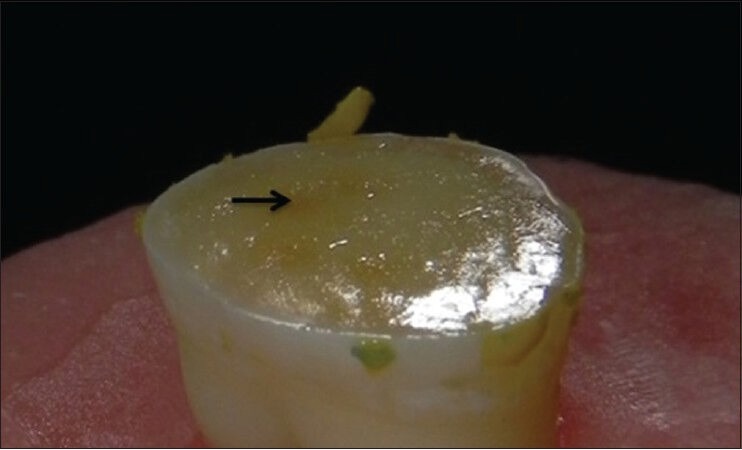
Photo of the tooth surface-immediate dentin sealing with Clearfil SE Bond and impression with vinyl polysiloxane: Small areas of unpolymerized impression material (arrow) are attached to the surface of the resin material. The same was observed for Protect Liner F
Figure 4.
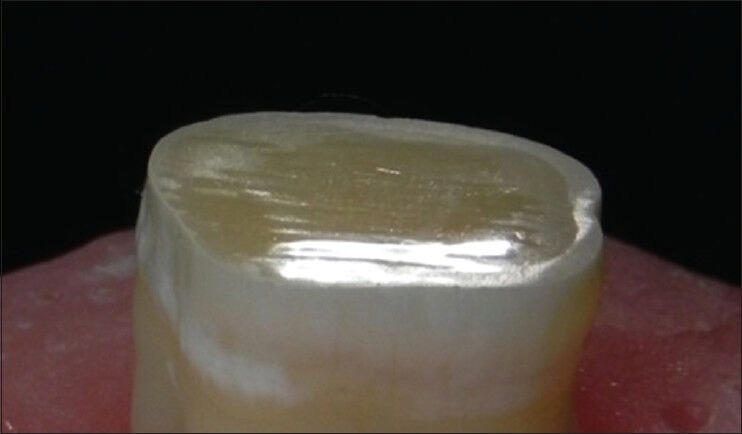
Photo of the tooth surface-immediate dentin sealing with Clearfil SE Bond, alcohol application and impression with vinyl polysiloxane: There is no interaction between the impression material and the resin material. The same was observed for glycerin jelly application, as well as for IDS with Protect Liner F and impression with polyether after glycerin jelly or alcohol application
For the polyether impression material, the group that received IDS with CSE (Group 2b) and the group with PLF (Group 2e) had observable interactions in five and three impressions, respectively. A small quantity of polymerized impression material remained attached to the adhesive system or to the low-viscosity composite resin [Figure 5]. The same interaction was observed for the groups that received IDS with CSE and the application of glycerin jelly (Group 2c) and a cotton pellet soaked in alcohol (Group 2d), occurring in three and two impressions, respectively. When both treatments were applied to the low-viscosity composite resin (Groups 2f and 2g), no interactions were observed.
Figure 5.

Photo of the tooth surface-immediate dentin sealing with Clearfil SE Bond, glycerin jelly application and impression with polyether: Polymerized impression material is attached to the CSE. The same was observed for alcohol application
DISCUSSION
The hypothesis of this study was partially rejected, as the prevention of interactions following the proposed treatments depended on the impression material and the resin materials employed.
In the control groups, in which the IDS was not applied, there was no interaction between the impression material and the tooth structure. However, in the groups in which the IDS was applied, there was an observable interaction of vinyl polysiloxane and the polyether with the resin materials, either with the adhesive systems or the low-viscosity composite resin. This finding is related to the presence of the OIL.[3] The CSE adhesive system and the PLF low-viscosity composite resin are composed of methacrylates[14] and when light cured, these materials present a superficial layer of approximately 40 μm that does not polymerize with air-oxygen contact.[11,15] The OIL has a jelly-like consistency and is composed mainly of residual monomers that do not react after the polymerization of the resin material.[16] These nonreacting monomers may go on to interact with the impression materials.[17,18]
Different interaction types occurred between the resin materials and the impression materials. For the vinyl polysiloxane, unpolymerized impression material remained over the resin materials. For the polyether, polymerized impression material remained joined to the resin materials. It is likely that the difference between the chemical composition of the vinyl polysiloxane and the polyether caused the impression materials to react in the different ways to the resin materials.
The permanence of the unpolymerized vinyl polysiloxane over the CSE adhesive system was observed in three impressions and was also observed in every impression with the PLF low-viscosity composite resin. It is speculated that the monomers presented in the OIL may have reacted with the platinum salt, which is the catalyst in the reaction of polymerization of the vinyl polysiloxane,[19] and a small portion of the light impression material remained unpolymerized over the resin materials. However, the amount of unpolymerized material is negligible and is likely functionally irrelevant; therefore, it is believed that this interaction does not render the use of the impressions impractical.
For the polyether, the polymerized material remained joined to the resin materials in all the impressions with CSE and in three impressions with PLF. This interaction may have occurred due to the polymerization reaction of the polyether (ionic polymerization), in which the initiator agent of the reaction is an ion (cation) that can react with the free radicals of the monomers from the resin materials on the surface. Moreover, the hydrophilicity, as well as the higher stiffness and the low resistance to the tearing of the polyether when compared to the vinyl polysiloxane, may have favored the superficial adhesion and the tearing of the impression material.[20] This type of interaction renders the use of the impressions impractical.
Taking into account the principles of molecular interaction, it is believed that the OIL was critical for the adhesion between the increments of composite resin and with the adhesive system.[16] However, currently, it is known that OIL is not essential for the chemical adhesion of the layers of the composite resin.[16,21]
Additional polymerization with glycerin jelly over the layer of resin material,[12] as well as the use of alcohol,[22,23] is aimed at reducing or eliminating the OIL. Both procedures were effective when applied over the CSE adhesive system and the impression was made with vinyl polysiloxane, as no interaction was observed between the adhesive and impression material. However, it is speculated that there is a certain amount of residual unpolymerized monomers on the surface of the adhesive after the application of glycerin jelly or alcohol because the polyether remained joined to the adhesive surface, subsequently tearing and rendering the impression unusable. These findings agree with the results of a study by Magne and Nielsen.[24]
Protect Liner F has a higher percentage of filler than CSE and consequently, should present fewer residual monomers after the light curing. Therefore, the application of glycerin jelly and alcohol were effective in preventing interactions with PLF when the polyether was used, as there was no interaction of this impression material with the low-viscosity composite resin. The application of glycerin jelly and alcohol on the low-viscosity composite resin was effective in four impressions with vinyl polysiloxane, and an interaction was observed only in one impression. The interaction was characterized by incomplete polymerization and the permanence of unpolymerized impression material adhering to the surface of the PLF. However, the amount of unpolymerized material was insignificant, and therefore the resulting impressions remain usable. Despite using standardized procedures, small variations, such as the final thickness of the low-viscosity composite resin, the thickness of the glycerin jelly applied on the low-viscosity composite resin, and the application pressure of the cotton pellet soaked in alcohol, likely contributed to the lack of effectiveness when removing or eliminating the OIL in the sample in which the interaction was observed.
Both the application of glycerin jelly and alcohol affected the OIL, as the results were similar for the same impression material when comparing the two techniques. This result indicates that professional discretion must be used when selecting a technique.
This in vitro study presents some limitations, such as the shape of the samples. The application of IDS was evaluated using flat dental surfaces. However, the preparations for indirect restorations are geometric and irregular, making it difficult to apply resin materials and remove OIL. Thus, additional studies are necessary to determine the nature of the interactions between the resin materials and the impression materials and to solve this potential clinical problem.
CONCLUSIONS
Despite the limitations of this in vitro study, the following conclusions can be drawn:
The IDS using the CSE adhesive system or the PLF low-viscosity composite resin produces interactions with the Express XT vinyl polysiloxane and with the Impregum polyether
The application of glycerin jelly and alcohol prevented the interactions between the CSE and the Express XT and between the PLF and the Impregum. However, these treatments were not completely effective in preventing the interactions of CSE with the Impregum or the interactions of the PLF with the Express XT.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Terata R. Characterization of enamel and dentin surfaces after removal of temporary cement – Study on removal of temporary cement. Dent Mater J. 1993;12:18–28. doi: 10.4012/dmj.12.18. [DOI] [PubMed] [Google Scholar]
- 2.Watanabe EK, Yamashita A, Imai M, Yatani H, Suzuki K. Temporary cement remnants as an adhesion inhibiting factor in the interface between resin cements and bovine dentin. Int J Prosthodont. 1997;10:440–52. [PubMed] [Google Scholar]
- 3.Paul SJ, Schärer P. The dual bonding technique: A modified method to improve adhesive luting procedures. Int J Periodontics Restorative Dent. 1997;17:536–45. [PubMed] [Google Scholar]
- 4.Pashley EL, Comer RW, Simpson MD, Horner JA, Pashley DH, Caughman WF. Dentin permeability: Sealing the dentin in crown preparations. Oper Dent. 1992;17:13–20. [PubMed] [Google Scholar]
- 5.Medina AD, de Paula AB, de Fucio SB, Puppin-Rontani RM, Correr-Sobrinho L, Sinhoreti MA. Marginal adaptation of indirect restorations using different resin coating protocols. Braz Dent J. 2012;23:672–8. doi: 10.1590/s0103-64402012000600008. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira L, Mota EG, Borges GA, Burnett LH, Jr, Spohr AM. Influence of immediate dentin sealing techniques on cuspal deflection and fracture resistance of teeth restored with composite resin inlays. Oper Dent. 2014;39:72–80. doi: 10.2341/12-100-L. [DOI] [PubMed] [Google Scholar]
- 7.Duarte RM, de Goes MF, Montes MA. Effect of time on tensile bond strength of resin cement bonded to dentine and low-viscosity composite. J Dent. 2006;34:52–61. doi: 10.1016/j.jdent.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Hu J, Zhu Q. Effect of immediate dentin sealing on preventive treatment for postcementation hypersensitivity. Int J Prosthodont. 2010;23:49–52. [PubMed] [Google Scholar]
- 9.Perugia C, Ferraro E, Docimo R. Immediate dentin sealing in indirect restorations of dental fractures in paediatric dentistry. Eur J Paediatr Dent. 2013;14:146–9. [PubMed] [Google Scholar]
- 10.Eliades GC, Caputo AA. The strength of layering technique in visible light-cured composites. J Prosthet Dent. 1989;61:31–8. doi: 10.1016/0022-3913(89)90104-2. [DOI] [PubMed] [Google Scholar]
- 11.Rueggeberg FA, Margeson DH. The effect of oxygen inhibition on an unfilled/filled composite system. J Dent Res. 1990;69:1652–8. doi: 10.1177/00220345900690100501. [DOI] [PubMed] [Google Scholar]
- 12.Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94:511–9. doi: 10.1016/j.prosdent.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Udo T, Nikaido T, Ikeda M, Weerasinghe DS, Harada N, Foxton RM, et al. Enhancement of adhesion between resin coating materials and resin cements. Dent Mater J. 2007;26:519–25. doi: 10.4012/dmj.26.519. [DOI] [PubMed] [Google Scholar]
- 14.Gauthier MA, Stangel I, Ellis TH, Zhu XX. Oxygen inhibition in dental resins. J Dent Res. 2005;84:725–9. doi: 10.1177/154405910508400808. [DOI] [PubMed] [Google Scholar]
- 15.Stansbury JW. Curing dental resins and composites by photopolymerization. J Esthet Dent. 2000;12:300–8. doi: 10.1111/j.1708-8240.2000.tb00239.x. [DOI] [PubMed] [Google Scholar]
- 16.Suh BI. Oxygen-inhibited layer in adhesion dentistry. J Esthet Restor Dent. 2004;16:316–23. doi: 10.1111/j.1708-8240.2004.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 17.Hannig C, Laubach S, Hahn P, Attin T. Shear bond strength of repaired adhesive filling materials using different repair procedures. J Adhes Dent. 2006;8:35–40. [PubMed] [Google Scholar]
- 18.Magne P, So WS, Cascione D. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007;98:166–74. doi: 10.1016/S0022-3913(07)60052-3. [DOI] [PubMed] [Google Scholar]
- 19.Anusavice KJ. 10th ed. Guanabara Koogan: 1998. Phillips – Dental Materials. [Google Scholar]
- 20.Lawson NC, Burgess JO, Litaker M. Tear strength of five elastomeric impression materials at two setting times and two tearing rates. J Esthet Restor Dent. 2008;20:186–93. doi: 10.1111/j.1708-8240.2008.00176.x. [DOI] [PubMed] [Google Scholar]
- 21.Papacchini F, Dall’Oca S, Chieffi N, Goracci C, Sadek FT, Suh BI, et al. Composite-to-composite microtensile bond strength in the repair of a microfilled hybrid resin: Effect of surface treatment and oxygen inhibition. J Adhes Dent. 2007;9:25–31. [PubMed] [Google Scholar]
- 22.Nikaido T, Cho E, Nakajima M, Tashiro H, Toba S, Burrow MF, et al. Tensile bond strengths of resin cements to bovine dentin using resin coating. Am J Dent. 2003;16(Spec No):41A–6. [PubMed] [Google Scholar]
- 23.Sultana S, Nikaido T, Matin K, Ogata M, Foxton RM, Tagami J. Effect of resin coating on dentin bonding of resin cement in Class II cavities. Dent Mater J. 2007;26:506–13. doi: 10.4012/dmj.26.506. [DOI] [PubMed] [Google Scholar]
- 24.Magne P, Nielsen B. Interactions between impression materials and immediate dentin sealing. J Prosthet Dent. 2009;102:298–305. doi: 10.1016/S0022-3913(09)60178-5. [DOI] [PubMed] [Google Scholar]


