Abstract
Objective:
The aim of this study was to compare the anti-plaque efficacy of a low and high cost commercially available tooth paste among 13-20 years old adolescents in a Residential Home, Bhopal, India.
Materials and Methods:
The study was randomized double-blind parallel clinical trial conducted in a Residential Home, Bhopal, India. A total of 65 patients with established dental plaque and gingivitis were randomly assigned to either low cost or high cost dentifrice group for 4 weeks. The plaque and gingival scores at baseline and post-intervention were assessed and compared. Statistical analysis was performed using paired t-test and the independent sample t-test. The statistical significance was fixed at 0.05.
Results:
Results indicated a significant reduction in plaque and gingival scores in both groups post-intervention compared with the baseline. Difference between the groups was not significant. No adverse events were reported and both the dentifrices were well-tolerated.
Conclusion:
Low cost dentifrice is equally effective to the high cost dentifrice in reducing plaque and gingival inflammation.
Keywords: Cost, dentifrices, gingivitis, plaque, toothpastes
INTRODUCTION
Dental plaque is defined as “the diverse microbial community embedded in a matrix of host and bacterial polymers, growing on teeth as a biofilm.” The microflora in the dental plaque are mainly responsible for the two most common dental diseases (dental caries and periodontal diseases) afflicting mankind.[1] It is estimated that over 75% of today's adults have gingivitis.[2] According to a World Health Organization report, majority of the children and adolescents exhibit signs of gingivitis while 5-20% of the adults have severe periodontitis. Moreover, periodontitis remains a major cause of tooth loss among adults in both developed and developing countries.[3]
According to a survey by National Commission on Macroeconomics and Health in the year 2000, nearly 45% (2957.6 lakhs) of Indian population aged 15 years or more had periodontitis. The study predicted that the number may rise up to 3413.8 lakhs by 2010 and 3624.8 lakhs by 2015. The survey projected that the proportion could reach even 80-90% when minor periodontal diseases are included.[4] Majority of the Indian population resides in rural areas and the high prevalence of dental diseases are primarily attributed to lack of knowledge on oral health, inadequate use of fluorides and infrastructure deficiencies leading to inadequate dental care.[5] Besides, the prevalence of oral diseases is especially high among the population in lower socio-economic status group.[6]
Traditional treatment of oral diseases is extremely costly and not a realistic option for the poor. Traditional curative dental care is a significant economic burden for many industrialized countries where 5-10% of public health expenditure relates to oral health. In most developing countries, investment in oral health care is low. The strategy that suits the developing countries such as India is to focus on primary prevention.[7] Good oral hygiene is an important primary preventive procedure that can prevent many oral diseases.[8]
Plaque removal by way of a daily home care regimen has long been emphasized by the dental professionals and is considered as an important element of oral health. Currently, many products are designed and promoted to achieve improved oral health. The most common being the use of toothbrushes, rinses, floss, and dentifrices.[9] Throughout the ages, dentifrices have been used as a major oral cleansing device. It had been used in ancient Greek and Roman civilizations as a powder formulation for esthetics, removing objectionable odors from the mouth, strengthening the teeth, relieving the dental pain and as a prophylactic paste.[10] The use of dentifrices containing anti-plaque agents has been found to be effective in preventing periodontal diseases.[11] Today, toothpastes represent the most commonly manufactured product intended to be used, along with the toothbrush, to prevent the accumulation, removal, and the metabolic activities of dental plaque. Realizing the importance of dentifrices in oral health care, toothpaste quality has been improvised on a regular basis by refining, substituting, and reformulating the toothpaste ingredients. The effectiveness and functionality of toothpaste is enhanced by adding a variety of safe and compatible ingredients that may reduce demineralization, interfere with bacterial adhesion, provide antibacterial action, prevent the formation of supragingival calculus, promote remineralization, and reduce dentinal hypersensitivity.[12] With the evolution in the composition of various toothpastes, the cost of the product also increases.[1] Currently, many oral health care products with varying costs are marketed and sold over the counter. The high risk population in lower social strata and rural areas in developing countries such as India will most often rely on products of lower cost, irrespective of the potential benefits of high cost dentifrices. Literature suggests that nearly 80% of the rural populations in India still start their day with the datun of Neem, Babul, Mango, Guava, Dandarasa or roots of Pilu.[13]
According to planning commission report, total number of people below the poverty line in the country is estimated to be around 35.46 crore.[14] The ever increasing cost in dentifrices may play an important role in determining the acceptance of the product amongst this population. It becomes vital for the dental profession to evaluate whether the high cost dentifrices have potential benefits (as claimed) in reducing plaque formation in comparison with low cost dentifrices. The literature comparing the plaque removing efficacy between high and low cost dentifrices is almost nonexistent. The research in this area to generate necessary evidence is the need of the hour especially in developing countries like India. In the background stated above the present study evaluated and compared the anti-plaque efficacy between a low and high cost commercially available dentifrice among 13-20 years old adolescents in a Residential Home, Bhopal, India.
MATERIALS AND METHODS
Selection of the study participants
This was a double-blind randomized parallel study conducted over a period of 2 months from September to October 2012 among 13-20 years old adolescents selected from a residential school in Bhopal city. The permission to conduct the study was obtained from the head master of the concerned school and the ethical clearance was obtained from the Institutional Ethics Committee. A tentative list of 93 adolescents in the age range of 13-20 years was initially prepared. The relevant information facilitating the inclusion and exclusion of study participants was collected from all these participants using the checklist and a data collection sheet. The checklist had 16 questions that specifically elicited the information on oral hygiene practices (method of cleaning, frequency, direction, duration of brushing, frequency of discarding tooth brush, use of mouth rinse, and inter-dental aids) medical history (history of systemic diseases, use of antimicrobials in the last 1 month, history of oral prophylaxis in last 3 months) and tobacco related habits. The checklist was filled by one investigator by means of face-to-face interview with the study participants. The oral examination among these participants was carried out by one trained and calibrated investigator. Plaque score was recorded using full mouth Turesky modification of Quigley Hein index[15] and gingivitis was scored using full mouth Loe and Silness gingival index.[16] The training and calibration of the investigator in the application of plaque and gingival indices was carried out on a group of 20 subjects. The assessment of plaque (Cronbach's α = 0.985) and gingiva (Cronbach's α = 0.989) showed good intra-examiner reliability. Autoclaved set of instruments were used for oral examination of the study participants.
The selection of participants into the study was based on the following inclusion and exclusion criteria.
Inclusion criteria
Those who give the written informed consent to participate in the study
Aged between 13 and 20 years
Having a minimum of 20 natural teeth which are not indicated for extraction
Whose baseline mean plaque score was more than 1.5 (Turesky modification of Quigley Hein index)
Whose baseline mean gingival index was more than 1.0 (Loe and Silness gingival index)
Who will be staying in the residential home for duration of at least 2 months from the date of screening.
Exclusion criteria
Presence of advanced periodontal disease (periodontal pockets, mobility, gingival recession, furcation involvement, etc.)
Presence of dental appliances (removable or fixed)
History of antibiotic use in previous 3 months
Those using mouth rinses containing chemical agents or inter-dental cleaning aids on a regular basis
Presence of any systemic diseases
Presence of malocclusion traits
Deleterious habits like smoking or use of other tobacco related habits
Individuals failing to offer written informed consent.
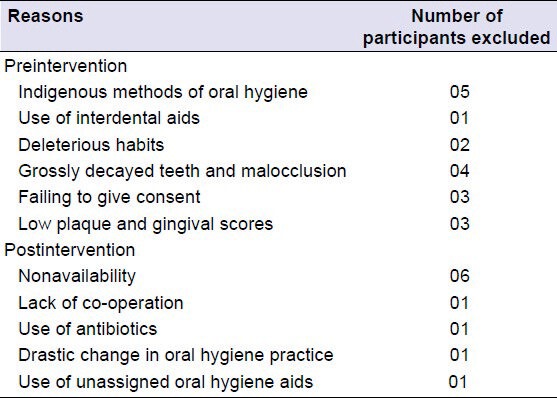
Eighteen participants were excluded from the initial list based on the inclusion and exclusion criteria. The reasons for exclusion are summarized in Table 1.
Table 1.
Summary of the reasons for exclusion and dropout of the study participants
Procedure of randomization
A total of 75 participants fulfilled the inclusion and exclusion criteria. These eligible participants were then randomly assigned to either Group A or Group B using a random allocation sequence by one of the faculty members. The staff member who carried out the process of randomization was not involved in the data collection and statistical analysis. The information on the group allocation and the sequence of random allocation was concealed from the main investigator and the statistician to ensure double blinding in the study. Each participant was offered a coded oral hygiene kit containing the assigned dentifrice and a toothbrush. The soft bristled toothbrush with uniform make was distributed to all participants to ensure uniformity with regards to mechanical cleaning aid. Oral hygiene kit for Group A contained a high cost dentifrice whose unit cost was 1.4 international normalized ratio (INR) (Indian rupee)/g (100 g for 140 INR). The kit assigned to Group B contained a low cost dentifrice whose unit cost was 0.21 INR/g (100 g for 21 INR). The details of the commercial name or the ingredients in the dentifrice were not revealed to the participants and the investigator. The participants were instructed to refrain from all other unassigned forms of oral hygiene, including nonstudy toothbrushes or toothpastes, dental floss, chewing gum or oral rinses for 1 month following the intervention. The study participants were instructed to continue with their existing oral hygiene habits (frequency and method of brushing) with no specific instructions to modify their routine habits owing to the difficulties anticipated in adopting to new oral hygiene instructions overnight. The oral hygiene aids used by the study participants prior to intervention were collected in an effort to maximize the compliance for the study. Adverse effects during the intervention period, if any, were recorded. The comparison of the distribution of the study participants based on frequency of brushing, duration of brushing (in each brushing) at pre- and post-intervention examinations between the participants in two groups was done to assess the confounding effect of oral hygiene practices.
Postintervention examination
At the end of 4 weeks following the intervention, all the participants were assembled in a waiting room. Then, each participant was examined by the same investigator who carried out the baseline examination for plaque and gingival scores employing the same indices which were used at baseline. The unique ID of the participant was entered after completion of oral examination. The information on the oral hygiene practices, use of antimicrobials, etc., during the intervention was collected using the same checklist that was used at baseline. The final analysis included only 65 participants. The dropout rate was 13.3%.
Statistical analysis
Data were entered onto a personal computer and statistical analysis was performed using SPSS version 19 (IBM, Chicago, IL, USA). Paired t-test was used for comparing the mean plaque and gingival index scores between baseline and postintervention in each group. The independent sample t-test was used for comparing the difference in the mean plaque and gingival scores between the groups. The statistical significance was fixed at 0.05.
RESULTS
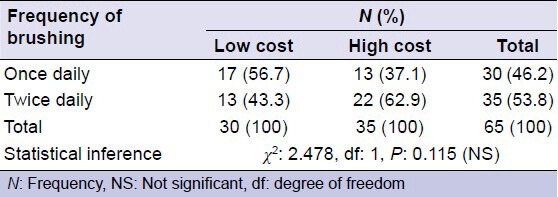
A total of 65 participants were considered for the final analysis. 35 participants were in the high cost dentifrice group and 30 participants were in the low cost dentifrice group. There was no significant difference in the distribution of study participants based on frequency of brushing between the intervention groups [P = 0.115, Table 2]. The statistical power was found to be 80% for an effect size of 0.67 and 5% α error.
Table 2.
Distribution of the study population according to frequency of brushing in different intervention groups
Baseline plaque and gingival scores between the intervention groups
The mean plaque score for the study population at baseline was 2.80 with a standard deviation (SD) of 0.46. The mean plaque score at baseline in the low and high cost dentifrice groups were 2.89 ± 0.37 (mean ± SD) and 2.74 ± 0.52, respectively. There was no statistically significant difference in the mean plaque scores between low and high cost dentifrices at baseline (P = 0.181). The mean plaque scores at baseline, among the participants brushing once was less in the high cost group (2.46 ± 0.32) compared to low cost group (2.83 ± 0.34) (P = 0.005). However, there was no significant difference in the mean plaque score at baseline among participants bushing twice daily between the low (2.97 ± 0.41) and high cost (2.90 ± 0.55) dentifrice groups (P = 0.693) [Table 3].
Table 3.
Comparison of baseline plaque and gingival scores in different intervention groups
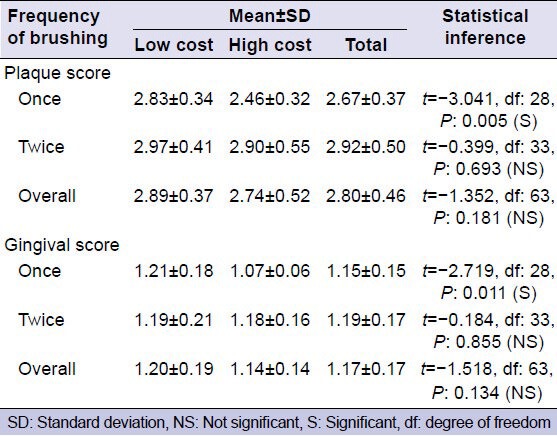
The mean gingival score for the study population at baseline was 1.17 with a SD of 0.17. The mean gingival scores at baseline, in the low and high cost dentifrice groups were 1.20 ± 0.19 and 1.14 ± 0.14, respectively. There was no statistically significant difference in the mean gingival scores between the groups at baseline (P = 0.134). The mean gingival score at baseline, among the participants brushing once was less in the high cost group (1.07 ± 0.06) compared with low cost group (1.21 ± 0.18) (P = 0.011). However, there was no significant difference in the mean gingival score at baseline among participants bushing twice daily between the low (1.19 ± 0.21) and high cost (1.18 ± 0.16) dentifrice groups (P = 0.855) [Table 3].
Postintervention plaque and gingival scores between the groups
The mean postintervention plaque score for the study population was 2.48 with a SD of 0.30. The mean plaque score at baseline in the low and high cost dentifrice groups were 2.52 ± 0.29 and 2.46 ± 0.26, respectively. There was no statistically significant difference in the mean postintervention plaque scores between low and high cost dentifrices (P = 0.417). The results were true even when a separate comparison was made among the study participants brushing once (P = 0.072) and twice daily (P = 0.915) between the two groups [Table 4].
Table 4.
Comparison of postintervention plaque and gingival scores between high and low cost groups
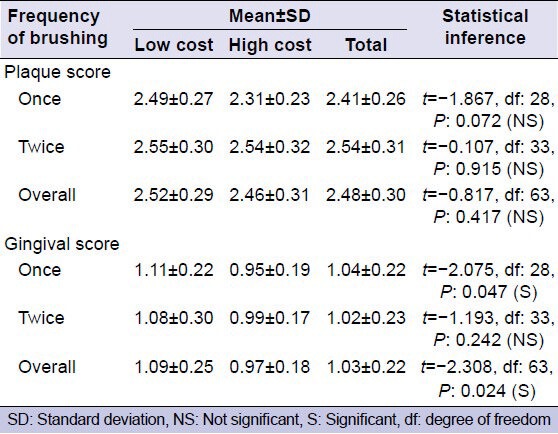
The mean postintervention gingival score for the study population was 1.03 with a SD of 0.22. The mean postintervention gingival score was significantly less in the high cost dentifrice group (0.97 ± 0.18) compared to low cost dentifrice group (1.09 ± 0.25) (P = 0.024). The mean postintervention gingival score, when compared separately among the participants brushing once daily was significantly less (P = 0.047) in the high cost group (0.95 ± 0.19) compared with the low cost group (1.11 ± 0.22). However, this difference was not statistically significant (P = 0.242) when the comparison was made separately among the participants brushing twice daily [P = 0.242, Table 4].
Pre- and post-intervention plaque and gingival scores in the each intervention groups
There was a significant reduction in the postintervention plaque score compared to preintervention levels in both the low (P < 0.001) and high cost dentifrice groups (P < 0.001). The results were true even when a separate comparison was made between pre- and post-intervention levels among the participants brushing once and twice daily [Table 5].
Table 5.
Results of paired t-test comparing the plaque and gingival score between baseline and postintervention in each intervention group
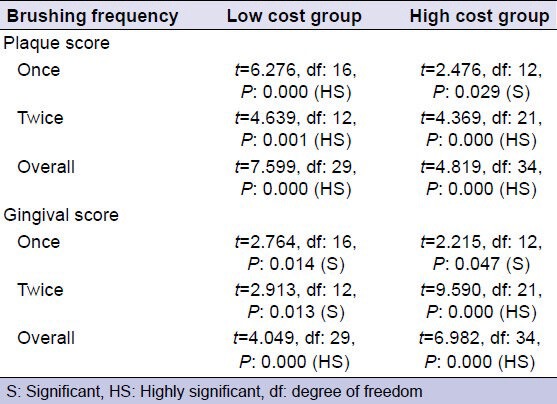
There was a significant reduction in the postintervention gingival score compared to preintervention levels in both the low (P < 0.001) and high cost dentifrice groups (P < 0.001). The results were true even when a separate comparison was made between pre- and post-intervention levels among the participants brushing once and twice daily [Table 5].
Comparison of the mean reduction in the plaque and gingival scores
The mean reduction in plaque and gingival scores was determined by noting the difference in these scores at baseline and postintervention. The comparison of the mean reduction in the plaque scores between the intervention groups revealed no statistically significant difference (P = 0.086). The results were true even when a separate comparison was made among the participants brushing once and twice daily [Table 6].
Table 6.
Comparison of the mean difference in plaque and gingival scores between the intervention groups
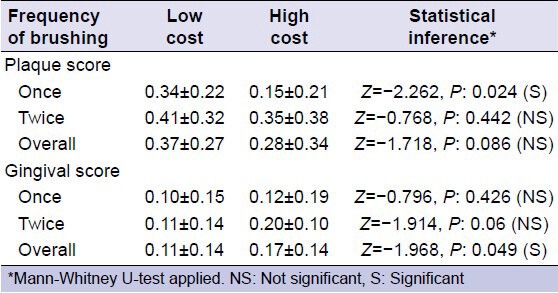
The mean reduction in the gingival score was significantly high in the high cost group (0.17 ± 0.14) compared to low cost (0.11 ± 0.14) group (P = 0.049). However, there was no significant difference in the mean reduction in gingival score among the participants brushing once (P = 0.426) and twice daily [P = 0.06, Table 6], when a separate comparison was made.
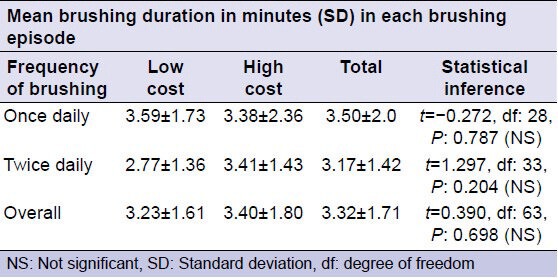
Comparison of brushing duration between the groups
The brushing duration was the approximate time spent for brushing the teeth at each episode of brushing. The study found no significant difference in the mean brushing duration among the participants assigned to the two intervention groups (P = 0.698). The results were true even when a separate comparison was made among the participants brushing once and twice daily [Table 7].
Table 7.
Comparison of the brushing duration among study population in different intervention groups
DISCUSSION
Oral hygiene maintenance is the key to prevention of dental diseases. Dental plaque remains the primary etiological factor for most of the dental diseases. Among all the methods of plaque removal, the most accepted method of oral hygiene maintenance is brushing of teeth. For proper brushing, a safe and effective cream is required to help the removal of dental plaque.[17] There is a wide variety of toothpastes which are marketed such as anti-cavity, extra-whitening and toothpaste for sensitive teeth, toothpastes with stripes or clear toothpastes.[18] Most of the dentifrices uses words such as “protects,” “cleans,” “freshens breath,” “fights bacteria,” “whitens” or “fights tartar” for their promotion. These claims are mostly cosmetic.[19] Toothpastes that contain up to 1500 ppm fluoride can make claims such as, “cavity protection,” “helps prevent tooth decay” and “fights tooth decay” all of which are also considered as cosmetic claims.[19] A major disadvantage is that cosmetic products can be marketed without clearance from any regulatory body. Only the manufacturer needs to ensure that such products are safe and under normal conditions of use do not cause any damage to health.[19]
Like all other cosmetic products, toothpastes also are in a race to be the best. In the race to enhance marketing, chemical composition of dentifrices is constantly changed and the multi-function toothpastes containing a wide range of ingredients have been evolved. These multi-function toothpastes provide both advantages (comprehensive oral health benefits in one package) and challenges for the consumers (higher price).[12] While multiple oral health benefits may be an advantage for those who can afford, many potential users will turn to their dental professional and may ask three simple questions:
Are these new multi-function toothpastes working in the manner as claimed in their advertisement?
Are the benefits they claim worth the additional cost burden?
Are you yourself using a multi-function paste, and if yes, which one?
It can be easy for a dental professional to answer the third question very easily. However, for many dentists, it is quite difficult to answer the first two questions that focus on the efficacy and value of the newer, multi-function toothpastes.[12]
This study was undertaken to compare the anti-plaque efficacy of a low and high cost commercially available tooth pastes and to address the questions raised above. A residential home was selected as the investigators felt the supervision of the oral hygiene practices was relatively easy and compliance with the use of oral hygiene could be monitored better in a residential home setting than in the individual houses of the participants.
The anti-plaque efficacy of a low and high cost commercially available tooth paste was assessed on the basis of reduction in plaque score and gingival score. Our study found no statistically significant difference in the mean postintervention plaque scores between low and high cost dentifrices. The results were true even when a separate comparison was made among the study participants brushing once and twice daily between the low and high cost dentifrice groups.
Prasad et al.[1] in their clinical trial comparing the anti-plaque efficacy of Anchor and Pepsodent toothpastes found no statistically significant difference in plaque status between the groups. They concluded that both toothpastes were equally effective in reducing the plaque scores over 8 week's duration similar to our findings.
Although, the chemical ingredients of different dentifrices offer an additional benefit to gingival health, the mechanical plaque removal is not always performed to an adequate standard. Further, the effectiveness of most of the benchmark dentifrices is close to test products because of similarity in majority of the chemical constituents.[18] The results our study were consistent with other studies which indicated no significant postintervention effects on plaque and gingival scores at the end of 18 week trial.[6]
We found the postintervention gingival score to be less in high cost dentifrice group compared to low cost group. Although, there was no statistically significant difference in gingival score between the groups as a whole at baseline, the gingival score was significantly less in the high cost group compared to low cost group among participants brushing once daily. This initial difference in gingival scores between the groups at baseline might be a reason for difference observed postintervention. When mean reduction in plaque and gingival scores was compared between the groups, no significant difference was observed. This strongly supports the claim that the initial difference in the gingival scores might be responsible for a relatively less postintervention gingival score in high cost group compared to low cost group.
The study found a statistically significant reduction in the postintervention plaque and gingival scores compared to baseline in both dentifrice groups. The study found no significant difference in the brushing frequency and brushing duration between pre- and post-intervention in both groups. However, we could not assess and compare the brushing method and force of brushing before and after intervention. The postintervention reduction in plaque and gingival scores in both the dentifrice groups may be attributed to free supply of oral hygiene kits and the fact that the participants might have brushed with more force than before since they were aware that they are participating in a study which involves their oral examination for plaque scores (Hawthorne effect).[9] The results of our study were consistent with the findings of study by Van der Weijden et al.[20] The results of our study could not be compared with any previous literature involving dentifrices of high and low cost as this was the first of its kind. The assessment of plaque using other indices such as Modified gingival margin plaque index[21] could help in precisely judging the anti-plaque efficacy for clinical decision.
SUMMARY AND CONCLUSION
The present study emphasizes the need to evaluate the claims of emerging oral health care products, marketed as being superior to other existing products. The intervention in the present study was offered for 4 weeks. The short duration of intervention, small sample and lack of uniform oral hygiene practices among the participants assigned to the intervention groups, are some potential limitations in the present study. Although, the results of the present study found no significant benefit in the plaque removing efficacy of high cost dentifrice compared to low cost dentifrice, we recommend further long term studies with larger samples to validate our results. The studies of this kind are more relevant and needs to be conducted in developing countries like India where an extensive population resides in rural areas and a bulk of them is living below the poverty line.
ACKNOWLEDGMENTS
First and foremost I offer my sincerest gratitude to my supervisor, Resp. Dr. Chandrashekar BR, who has supported me throughout my work with his patience and knowledge. The good advice and support of Resp. Dr. Pankaj Goel, Professor and Head of the Department of Public Health Dentistry, has been invaluable on both an academic and a personal level, for which I am extremely grateful. I am also thankful to Resp. Dr. Sudheer Hongal and Resp. Dr. Manish Jain who showed their kind concern and consideration regarding my academic requirements. I would also thank my colleague Dr. Ruchika Gupta for her kind support.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Prasad KV, Sohani R, Tikare S, Yelamalli M, Rajesh G, Javali SB. Anti-plaque efficacy of two commercially available dentifrices. J Indian Assoc Public Health Dent. 2009;1:12–7. doi: 10.4103/0970-9290.66639. [DOI] [PubMed] [Google Scholar]
- 2.Singh S, Chaknis P, DeVizio W, Petrone M, Panagakos FS, Proskin HM. A clinical investigation of the efficacy of three commercially available dentifrices for controlling established gingivitis and supragingival plaque. J Clin Dent. 2010;21:105–10. [PubMed] [Google Scholar]
- 3.Jin LJ, Armitage GC, Klinge B, Lang NP, Tonetti M, Williams RC. Global oral health inequalities: Task group - Periodontal disease. Adv Dent Res. 2011;23:221–6. doi: 10.1177/0022034511402080. [DOI] [PubMed] [Google Scholar]
- 4.Shaju JP, Zade RM, Das M. Prevalence of periodontitis in the Indian population: A literature review. J Indian Soc Periodontol. 2011;15:29–34. doi: 10.4103/0972-124X.82261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin S, Mauk A. Raghavan R, Johar Z, editors. Oral Health: Addressing Dental Diseases in Rural India. Implementing public health interventions in developing countries. ICTPH, Thanjavur, India. IKP Centre for Technologies in Public Health. 2011;(Ch 4):105–29. [Google Scholar]
- 6.Chandra Shekar BR, Reddy C. Oral health status in relation to socioeconomic factors among the municipal employees of Mysore city. Indian J Dent Res. 2011;22:410–8. doi: 10.4103/0970-9290.87063. [DOI] [PubMed] [Google Scholar]
- 7.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Sharda AJ, Shetty S. Relationship of periodontal status and dental caries status with oral health knowledge, attitude and behavior among professional students in India. Int J Oral Sci. 2009;1:196–206. doi: 10.4248/IJOS09061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnes VM, Richter R, DeVizio W. Comparison of the short-term antiplaque/antibacterial efficacy of two commercial dentifrices. J Clin Dent. 2010;21:101–4. [PubMed] [Google Scholar]
- 10.Fischman SL. The history of oral hygiene products: How far have we come in 6000 years? Periodontol. 2000;1997(15):7–14. doi: 10.1111/j.1600-0757.1997.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 11.Garcia RI. Mouthrinses and dentifrices are effective antigingivitis and antiplaque agents. J Evid Based Dent Pract. 2008;8:13–4. doi: 10.1016/j.jebdp.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stamm JW. Multi-function toothpastes for better oral health: A behavioural perspective. Int Dent J. 2007;57:351–363. [Google Scholar]
- 13.Bhambal A, Kothari S, Saxena S, Jain M. Comparative effect of neemstick and toothbrush on plaque removal and gingival health – A clinical trial. J Adv Oral Res. 2011;2:51–5. [Google Scholar]
- 14.Press Note on Poverty Estimates 2009. 10. Government of India, Planning Commission. 2012 Mar [Google Scholar]
- 15.Cugini M, Thompson M, Warren PR. Correlations between two plaque indices in assessment of toothbrush effectiveness. J Contemp Dent Pract. 2006;7:1–9. [PubMed] [Google Scholar]
- 16.Benamghar L, Penaud J, Kaminsky P, Abt F, Martin J. Comparison of gingival index and sulcus bleeding index as indicators of periodontal status. Bull World Health Organ. 1982;60:147–51. [PMC free article] [PubMed] [Google Scholar]
- 17.Amrutesh S, Malini J, Tandur PS, Patki PS. Clinical evaluation of a novel herbal dental cream in plaque formation: A double-blind, randomized, controlled clinical trial. J Exp Pharmacol. 2010;2:105–9. doi: 10.2147/jep.s10957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iqbal K, Asmat M, Jawed S, Mushtaque A, Mohsin F, Hanif S, et al. Role of different ingredients of tooth pastes and mouthwashes in oral health. JPDA. 2011;20:163–70. [Google Scholar]
- 19.Davies R, Scully C, Preston AJ. Dentifrices – An update. Med Oral Patol Oral Cir Bucal. 2010;15:e976–82. doi: 10.4317/medoral.15.e976. [DOI] [PubMed] [Google Scholar]
- 20.Van der Weijden GA, Timmerman MF, Danser MM, Van der Velden U. Relationship between the plaque removal efficacy of a manual toothbrush and brushing force. J Clin Periodontol. 1998;25:413–6. doi: 10.1111/j.1600-051x.1998.tb02464.x. [DOI] [PubMed] [Google Scholar]
- 21.Barnes VM, Vandeven M, Richter R, Xu T. The modified gingival margin plaque index: A predictable clinical method. J Clin Dent. 2008;19:131–3. [PubMed] [Google Scholar]


