Abstract
Extensive intraosseous lesions represent a clinical challenge for the periodontist. Sites with bone defects have been shown to be at higher risk of periodontitis progression in patients who had not received periodontal therapy. Thus, the aim of this case report was to describe a novel approach for the treatment of 1-walled intraosseous defect by combining nonsurgical periodontal therapy and orthodontic movement toward the bone defect, avoiding regenerative and surgical procedures. A 47-year-old woman underwent the proposed procedures for the treatment of her left central incisor with 9 mm probing depth and 1-walled intraosseous defect in its mesial aspect. Initially, basic periodontal therapy with scaling and root planning was accomplished. Two months later, an orthodontic treatment was planned to eliminate the intraosseous lesion and to improve the interproximal papillary area. Orthodontic root movement toward the osseous defect was performed for 13 months with light forces. After 6 years postoperative it was concluded that combined basic periodontal therapy and orthodontic movement was capable of eliminating the intraosseous defect and improve the esthetics in the interproximal papillary area between the central incisors.
Keywords: Interproximal papillary area, intraosseous bone defect, periodontal treatment, periodontitis, tooth movement
INTRODUCTION
Periodontal disease is a chronic inflammatory condition induced by dental biofilm that results in pocket formation, alveolar bone destruction and tooth loss as evidenced by studies in animals[1,2] and humans.[3] Periodontal disease has been divided in two main categories: gingivitis (gingival inflammation without loss of connective tissue attachment) and periodontitis. Periodontitis is characterized by an apical migration of the junctional epithelium, which in most patients increased probing depths (PDs) or the formation of periodontal pockets accompany the development of periodontitis.[4] The majority of patients with periodontitis will have the chronic form of the disease (most prevalent in adults over 30 years of age, slow to moderate rate of progression, substantial deposits of subgingival calculus, periodontal pockets, and bone destruction) that are categorized in slight: 1-2 mm of clinical attachment loss (CAL); moderate: 3-4 mm CAL; or severe: >5 mm CAL, localized or generalized (>30% of sites involved).[4]
The final goal of periodontal therapy is to eliminate the inflammation and to achieve periodontal tissue regeneration, especially in intraosseous defect, destroyed by the disease process. Innumerous treatment modalities have been proposed to re-establishing periodontal health for patients with intraosseous defects associated to periodontitis, such as: proper plaque control,[5] open-flap debridement,[6,7] or single flap approach,[8] regenerative procedures with bone grafts,[6,9,10] guided tissue regeneration (GTR),[11] and orthodontic movement.[12,13] Albeit the treatment of these defects by surgical techniques are commonly used, there are significant benefits of treating intraosseous defects by means of conservative approaches, especially related to the cost-benefit outcome and absence of gingival flap that could result in delayed healing, wound dehiscence, loss of primary closure,[14] lower filling osseous defect and postsurgical infection.[15] In addition, esthetics may be compromised by gingival recession and loss of interproximal papillary tissue.[16]
For these reasons, new conservative techniques especially designed to optimize the elimination of intraosseous defect have been developed by means of orthodontic movement,[12,13] but at least in part, this protocol has not been validated in patients. Orthodontic treatment has been proposed to achieve a more favorable osseous contour, especially in 1-walled defects in which predictability of regenerative periodontal therapy is poor.[12,17] There are some possibilities to modify the osseous contour with orthodontic movement: intrusion,[7,13,18] extrusion,[9,19] movement of a tooth into an osseous defect,[13,20] alignment and leveling,[16] and moving a tooth in the opposite direction, away from the osseous defect.[12] Thus, orthodontic therapy can reduce or even eliminate the intraosseous 1-walled defect without the necessity of surgical procedures.[12,17]
Orthodontic movements in patients with reduced alveolar bone do not increase the damage to the periodontium if good plaque control and good oral hygiene is offered by the patient and the periodontist.[5] In the presence of active periodontal disease and inflammation, orthodontic forces may cause a more severe periodontal bone resorption.[5] In a study by Re et al.,[21] the periodontal-orthodontic combined treatment, in patients with reduced periodontium, was capable to maintain the long-term stability after 12 years follow-up in 276 patients. This result was corroborated by another study that showed the use of continuous and light orthodontic forces, without gingival inflammation, resulted in reduction of PD, clinical attachment gain and radiological bone fill.[13]
Here, we proposed a new therapy for the treatment of 1-walled intraosseous defect by means of orthodontic movement toward the osseous defect. To the best of our knowledge, this is the first long-term case report that describes an orthodontic movement to eliminate the periodontal bone defect without surgical or regenerative procedures in a patient with localized severe chronic periodontitis.
CASE REPORT
A 47-year-old Caucasian woman was referred to the Department of Periodontology for the treatment of her left maxillary central incisor. The patient was complaining of tooth sensitivity and spontaneous bleeding. She had no relevant medical history and denied smoking and use of alcohol. The periapical radiographs, standardized by means of parallel technique, showed a localized vertical bone defect on the mesial region her left central incisor [Figure 1a]. Periodontal examination with transgingival probing, under local anesthesia, revealed a 1-walled periodontal defect with 9 mm of PD, bleeding on probing (BOP), with signs of Class II tooth mobility, and normal fremitus position in this site [Figure 1b]. The patient had never been treated for periodontitis and based on clinical and radiographic examinations the diagnosis was severe localized chronic periodontitis. The initial treatment plan was nonsurgical basic periodontal therapy to control the disease and reduce PD.
Figure 1.
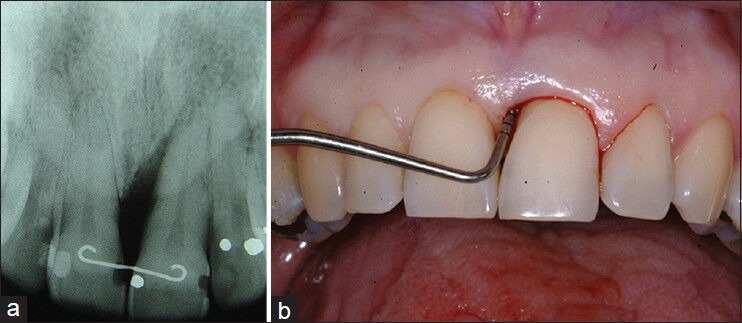
(a) Initial periapical radiographic showing the 1-walled intraosseous defect a in the mesial aspect of the central incisor. (b) Initial clinical appearance of the left central incisor, showing the 9 mm probing depth periodontal pocket. Note the bleeding on probe
Initially, a periodontal examination was performed including plaque scores, full-mouth bleeding, assessment of PD and CAL [Table 1]. To evaluate the qualitative changes in the gingival soft tissue, the gingival index was then accessed and scored at 3 (moderate inflammation and spontaneously bleeding), as described previously.[22] Then, the treatment involved oral hygiene instructions (OHI), supragingival and subgingival scaling followed by root planning with mini-Gracey curettes (Mini Five Gracey Curette, Hu-Friedy, Chicago, IL, USA) and chemistry control with 0.12% chlorhexidine. 2 months after the periodontal therapy, the patient exhibited good plaque control, healthy gingival tissues and 7 mm PD reduction, resulting in a final PD of 2 mm [Figure 2a and Table 1]. The patient was followed during 3 months and as an expected result of periodontal treatment, a “black triangle” between the central incisors was created due to the apical displacement of the gingival interproximal papilla, compromising the patient esthetics, and the CAL was 9 mm [Figure 2b].
Table 1.
The periodontal clinical indexes at the beginning of the therapy (baseline), at the end of the periodontal treatment, after orthodontic movement and after 6-year of follow-up
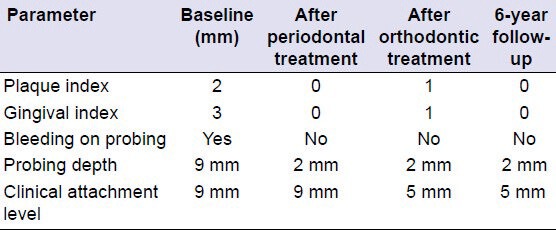
Figure 2.
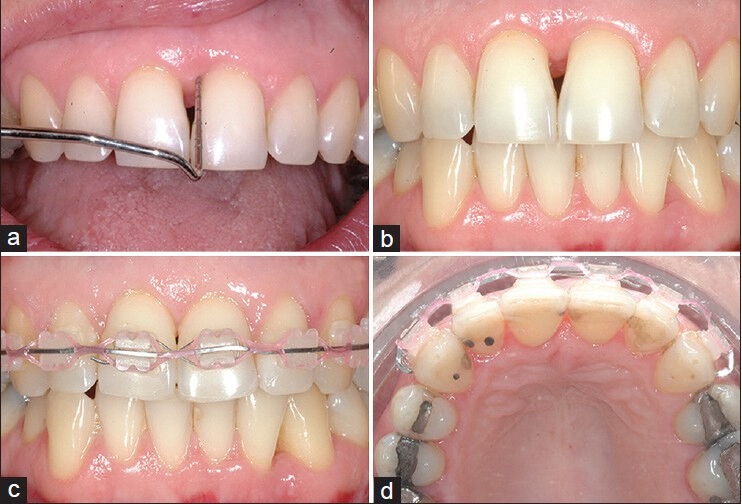
(a) 3 months after basic periodontal therapy with supra and subgingival scaling and root planning. The periodontal pocket was reduced about 7 mm but a black triangle was evident. (b) 3 months after basic periodontal therapy resulting in apical displacement of gingival margin leading to a compromised patient esthetics. (c and d) Initial orthodontic movement toward the intraosseous defect
To improve the esthetics of the gingival tissues between the central incisors and to achieve a more favorable osseous contour, orthodontic movement was proposed and accepted by the patient. The patient showed a Class I cephalometric pattern with good facial relationship and a normal profile without skeletal deviations. The orthodontic treatment began by the placement of fixed appliances in the maxillary arch with brackets and archwires. The maxillary right and left canine received a cuspid to cuspid titanium-molybdenum alloy 0.017’ × 0.025’ (3M Unitek, Monrovia, CA, USA) wire with progressively artistic bend incorporated, designed to produce a tipping root movement toward the intraosseous defect [Figure 2c and d]. The movement was accomplished by applying equal moments of approximately 15° in both central incisors. After 13 months of active orthodontic treatment, acceptable esthetics results were achieved, and the intraosseous defect was partially filled, as evidenced by a decrease in the CAL from 9 mm to 5 mm, resulting in 4 mm of bone gain [Figure 3a and b, Table 1]. At the end, the patient received a permanent retention apparatus, placed in her right and left central incisors, to prevent orthodontic relapse after treatment.
Figure 3.
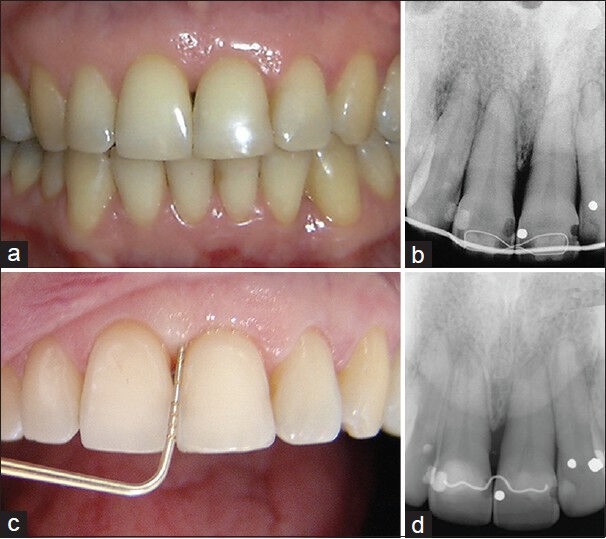
(a) 8 months after orthodontic movement by means of root movement toward the intraosseous defect. Note the partial filling of the papilla between the central incisors. (b) Periapical radiographic 8 months after active orthodontic therapy showing the partial intraosseous defect filling. (c) 6 years follow-up after periodontal and orthodontic therapy for the treatment of localized periodontal intraosseous defect. (d) Final radiographic result of an intraosseous defect treated with periodontal and orthodontic therapy. Compare with the initial radiography
Following the orthodontic treatment, the patient was seen monthly during the first 4 months to evaluate the periodontal status of the patient (gingival index, plaque scores, and BOP), followed by professional prophylaxis and OHI [Table 1]. Maintenance visits consisted of reinforcement of OHI and professional prophylaxis. Six years of follow-up showed normal PD, no BOP, no plaque scores, and the intraosseous defect was almost completely eliminated [Table 1]. The black triangle was reduced and the patient was rather pleased with the absence of sensitivity and spontaneous bleeding and good esthetics results. Clinical success was achieved in this case involving basic periodontal therapy and orthodontic treatment by means of root movement toward the intraosseous defect [Figure 3c and d].
DISCUSSION
New surgical approaches have been developed, in recent years, to optimize wound healing, to minimize the surgical trauma and to improve primary closure in the reconstructive procedures of periodontal intraosseous defects.[6,8,15,17,23] Commonly, treatments of intraosseous defect involve scaling and rooting planning with or without surgical flap.[17] In this last case, additional reconstructive procedures are indicated, such as: Bone grafts, GTR and biological agents to allow the intraosseous defect fill and periodontal tissue regeneration.[17] However, the predictability in these approaches only is found for 2- or 3-walled defects.[24]
On the other hand, orthodontic movement has been evaluated only in few cases for the treatment of deep intraosseous defect with open-flap surgery and orthodontic intrusion,[8,13,15,23] but not with orthodontic movement and basic periodontal therapy. Thus, we propose a novel approach to obtain periodontal regeneration of 1-walled intraosseous lesion by means of orthodontic movement toward the bone defect. The results of this clinical case indicate that orthodontic movement improve the healing process after basic periodontal therapy as demonstrated by reduction of PD, a significantly improve in the CAL, the new bone formation filling the periodontal defect evidenced by radiological examination, and for improvement in the esthetics of the interproximal papillary area. Besides, this approach can be beneficial because allow better clinical conditions to plaque control resulting in reduced inflammation, favors the incidence of occlusal forces, and enhances the osseous contour. Unlike the findings of a previous study in dogs,[12] where the authors observed small level of vertical bone apposition compared to the control group, using orthodontic movement in 1-walled bone defect, our results showed an increased bone gain, filling the intraosseous defect due to the movement of the root into the lesion.
The clinical results obtained in the present case can be attributed to the orthodontic movement that induced a slowly displacement of the root toward to the base of the osseous defect, allowing new bone formation, reduction of gingival recession and better tooth position, and could be stated that stretching the periodontal fibers resulted in reduction of the downgrowth of the epithelial cells. Moreover, orthodontic movement increased the periodontal ligament cells turnover enhancing the repopulating of the root surface.[13] In addition, good plaque control made by the patient and by the periodical visits to the periodontist, and due to a longer stabilization period of the orthodontic appliance were determining factors for achieving the results presented in this clinical report. Previous study[25] showed that proper oral hygiene maintenance during orthodontic therapy, no injury to the supporting teeth will occur. However, if periodontal inflammation is present, and if oral hygiene is poor controlled, orthodontic treatment will result in increased risk for bone resorption.[25] As stated by Corrente et al.,[13] absence of gingival inflammation are considered to be the most important factors related to the long-term success in patients with reduced periodontium.
Patients with periodontal disease commonly show interproximal bone loss, which result in papillary height defect.[16,26] An interesting finding of this clinical case is the significant esthetics improvement of the interproximal papillary area between the central incisors. This result can be explained by the intraosseous defect filling and apical displacement of the contact point between central incisors after the orthodontic movement, which provided an adequate distance from the contact point to the alveolar crest. According to Tarnow et al.,[27] when the distance from the base of the contact point to the bone crest was 3-5 mm, the papilla was present in 98% of cases. However, when the distance was >6 mm usually the interdental papilla was absent.[27] In this particular case, the distance from the contact point to the bone crest allowed the papilla filling of almost the entire space between the central incisors.
CONCLUSION
Basic periodontal therapy, good plaque control, light orthodontic forces, and root movement into the defect, can be a viable alternative for the treatment of intraosseous lesions in the esthetics region resulting in radiological bone fill, clinical attachment level gain, reduction of gingival recession, and PD. However, it should be stated that light orthodontic forces, good plaque control made by the patient, periodical maintenance visits to the periodontist, and a permanent retention orthodontic apparatus are necessary to achieve good results.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.de Molon RS, de Avila ED, Boas Nogueira AV, Chaves de Souza JA, Avila-Campos MJ, de Andrade CR, et al. Evaluation of the host response in various models of induced periodontal disease in mice. J Periodontol. 2014;85:465–77. doi: 10.1902/jop.2013.130225. [DOI] [PubMed] [Google Scholar]
- 2.de Molon RS, de Avila ED, Cirelli JA. Host responses induced by different animal models of periodontal disease: A literature review. J Investig Clin Dent. 2013;4:211–8. doi: 10.1111/jicd.12018. [DOI] [PubMed] [Google Scholar]
- 3.Haffajee AD, Socransky SS. Microbial etiological agents of destructive periodontal diseases. Periodontol 2000. 1994;5:78–111. doi: 10.1111/j.1600-0757.1994.tb00020.x. [DOI] [PubMed] [Google Scholar]
- 4.Armitage GC. Periodontal diagnoses and classification of periodontal diseases. Periodontol 2000. 2004;34:9–21. doi: 10.1046/j.0906-6713.2002.003421.x. [DOI] [PubMed] [Google Scholar]
- 5.Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93:143–8. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]
- 6.De Leonardis D, Paolantonio M. Enamel matrix derivative, alone or associated with a synthetic bone substitute, in the treatment of 1- to 2-wall periodontal defects. J Periodontol. 2013;84:444–55. doi: 10.1902/jop.2012.110656. [DOI] [PubMed] [Google Scholar]
- 7.Cardaropoli D, Re S, Corrente G, Abundo R. Intrusion of migrated incisors with infrabony defects in adult periodontal patients. Am J Orthod Dentofacial Orthop. 2001;120:671–5. doi: 10.1067/mod.2001.119385. [DOI] [PubMed] [Google Scholar]
- 8.Trombelli L, Simonelli A, Schincaglia GP, Cucchi A, Farina R. Single-flap approach for surgical debridement of deep intraosseous defects: A randomized controlled trial. J Periodontol. 2012;83:27–35. doi: 10.1902/jop.2011.110045. [DOI] [PubMed] [Google Scholar]
- 9.de Molon RS, de Avila ED, de Souza JA, Nogueira AV, Cirelli CC, Margonar R, et al. Forced orthodontic eruption for augmentation of soft and hard tissue prior to implant placement. Contemp Clin Dent. 2013;4:243–7. doi: 10.4103/0976-237X.114876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Molon RS, Avila ED, Cirelli JA, Mollo-Jr FD, Andrade MF, Barros-Filho LA, et al. A Combined approach for the treatment of resorbed fresh sockets allowing immediate implant restoration. A 2-year follow-up. J Oral Implantol. 2013 doi: 10.1563/AAID-JOI-D-13-00140. epub ahead of print. doi.10.1563/AAID.JOI.D.13.00140. [DOI] [PubMed] [Google Scholar]
- 11.Koylass JM, Valderrama P, Mellonig JT. Histologic evaluation of an allogeneic mineralized bone matrix in the treatment of periodontal osseous defects. Int J Periodontics Restorative Dent. 2012;32:405–11. [PubMed] [Google Scholar]
- 12.Cirelli CC, Cirelli JA, da Rosa Martins JC, Lia RC, Rossa C, Jr, Marcantonio E., Jr Orthodontic movement of teeth with intraosseous defects: Histologic and histometric study in dogs. Am J Orthod Dentofacial Orthop. 2003;123:666–73. doi: 10.1016/s0889-5406(03)00154-9. [DOI] [PubMed] [Google Scholar]
- 13.Corrente G, Abundo R, Re S, Cardaropoli D, Cardaropoli G. Orthodontic movement into infrabony defects in patients with advanced periodontal disease: A clinical and radiological study. J Periodontol. 2003;74:1104–9. doi: 10.1902/jop.2003.74.8.1104. [DOI] [PubMed] [Google Scholar]
- 14.Farina R, Simonelli A, Rizzi A, Pramstraller M, Cucchi A, Trombelli L. Early postoperative healing following buccal single flap approach to access intraosseous periodontal defects. Clin Oral Investig. 2013;17:1573–83. doi: 10.1007/s00784-012-0838-6. [DOI] [PubMed] [Google Scholar]
- 15.Trombelli L, Farina R, Franceschetti G, Calura G. Single-flap approach with buccal access in periodontal reconstructive procedures. J Periodontol. 2009;80:353–60. doi: 10.1902/jop.2009.080420. [DOI] [PubMed] [Google Scholar]
- 16.de Molon RS, de Avila ÉD, de Souza JA, Nogueira AV, Cirelli CC, Cirelli JA. Combination of orthodontic movement and periodontal therapy for full root coverage in a Miller class III recession: A case report with 12 years of follow-up. Braz Dent J. 2012;23:758–63. doi: 10.1590/s0103-64402012000600022. [DOI] [PubMed] [Google Scholar]
- 17.Trombelli L. Which reconstructive procedures are effective for treating the periodontal intraosseous defect? Periodontol 2000. 2005;37:88–105. doi: 10.1111/j.1600-0757.2004.03798.x. [DOI] [PubMed] [Google Scholar]
- 18.Fung K, Chandhoke TK, Uribe F, Schincaglia GP. Periodontal regeneration and orthodontic intrusion of a pathologically migrated central incisor adjacent to an infrabony defect. J Clin Orthod. 2012;46:417–23. [PubMed] [Google Scholar]
- 19.de Barros LA, de Almeida Cardoso M, de Avila ED, de Molon RS, Siqueira DF, Mollo-Junior Fde A, et al. Six-year follow-up of maxillary anterior rehabilitation with forced orthodontic extrusion: Achieving esthetic excellence with a multidisciplinary approach. Am J Orthod Dentofacial Orthop. 2013;144:607–15. doi: 10.1016/j.ajodo.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 20.Nemcovsky CE, Sasson M, Beny L, Weinreb M, Vardimon AD. Periodontal healing following orthodontic movement of rat molars with intact versus damaged periodontia towards a bony defect. Eur J Orthod. 2007;29:338–44. doi: 10.1093/ejo/cjm015. [DOI] [PubMed] [Google Scholar]
- 21.Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31–9. [PubMed] [Google Scholar]
- 22.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;(38 Suppl):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 23.Trombelli L, Simonelli A, Pramstraller M, Wikesjö UM, Farina R. Single flap approach with and without guided tissue regeneration and a hydroxyapatite biomaterial in the management of intraosseous periodontal defects. J Periodontol. 2010;81:1256–63. doi: 10.1902/jop.2010.100113. [DOI] [PubMed] [Google Scholar]
- 24.Pietruska M, Pietruski J, Nagy K, Brecx M, Arweiler NB, Sculean A. Four-year results following treatment of intrabony periodontal defects with an enamel matrix derivative alone or combined with a biphasic calcium phosphate. Clin Oral Investig. 2012;16:1191–7. doi: 10.1007/s00784-011-0611-2. [DOI] [PubMed] [Google Scholar]
- 25.Thilander B. Infrabony pockets and reduced alveolar bone height in relation to orthodontic therapy. Semin Orthod. 1996;2:55–61. doi: 10.1016/s1073-8746(96)80040-5. [DOI] [PubMed] [Google Scholar]
- 26.de Molon RS, de Avila ED, Cirelli JA, Cardoso Mde A, Capelozza-Filho L, Borelli Barros LA. Optimizing maxillary aesthetics of a severe compromised tooth through orthodontic movement and dental implants. Case Rep Dent 2014. 2014:103808. doi: 10.1155/2014/103808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]


