Abstract
Lateral periodontal cyst (LPC), originated from epithelial rests in the periodontal ligament, is a noninflammatory cyst on the lateral surface of the root of a vital tooth. LPC is generally asymptomatic and presents a round or oval uniform lucency with well-defined borders radiographically. In this case report, clinical, histological and radiographical findings and periodontal treatment of 32-year-old female patient, who was referred to Department of Periodontology Clinic of Faculty of Dentistry, Marmara University with a painless hyperplastic lesion on the distobuccal site of the tooth number 12, were presented. The tooth number 12 was vital and a well-defined round radiolucent area with corticated borders was determined radiographically. Preliminary diagnosis was LPC based on clinical and radiographical findings. Mechanical periodontal treatment consisted of oral hygiene instructions, scaling and root planing was applied and flap operation was performed to gain access to the lesion. Following enucleation of the lesion, alveolar bone destruction shaped as a tunnel from labial to palatinal site was observed. The bone cavity was grafted with bovine-derived xenograft, followed by placement of a resorbable collagen membrane. Tissues removed from of the lesion were examined histologically. Hematoxylen-eosin stained sections showed vasculature granulomatous structure underlying squamous epithelium, and destructed bone spaces, all of which were consisted with LPC. Acceptable clinical healing was achieved at 6 months follow-up period. Satisfactory clinical and radiographical outcome can be achieved in the treatment of LPC using regenerative periodontal approach.
Keywords: Guided tissue regeneration, periodontal cyst, surgical flaps
INTRODUCTION
Lateral periodontal cyst (LPC) is a noninflammatory cyst on the lateral surface of the root of a vital tooth.[1] The etiology of LPC is unclear and the cell rests of Malassez, reduced enamel epithelium or remnants of dental lamina were suggested to cause formation and development of LPC.[2,3] It is rare in young people under 30 years and affects individuals between the fifth and seventh decade of life. LPC was reported not to have a predilection for any race.[4] Although some studies report equal sex distribution,[4] others report male preponderance.[5] LPC occurs more often in the mandible, especially on the lateral aspect of premolar-canine root surfaces.[6]
The patients with LPC are generally asymptomatic and LPC is often identified during routine radiographical examination. It appears radiographically as a round or oval uniform lucency with well-defined borders <1 cm diameter.[5] The radiographic characteristics of LPC are not pathognomonic and can resemble an odontogenic keratocyst or lateral radicular cyst.[1]
Histologically, LPC is composed of a cystic cavity with a connective tissue wall with nonkeratinized squamous epithelial lining of 1-5 cell thickness and is generally without inflammation.[7]
Untreated odontogenic cysts may cause root resorption, tooth displacement, expansion, and pain.[3] Treatment of LPC includes removal of the lesion surgically by conservative enucleation and follow-up the patient radiographically to monitor for recurrence. During the healing period of 6 months to 1 year, bone regeneration will occur within the bony defect and recurrences are uncommon. On the other hand, different regenerative approaches, including guided tissue regeneration (GTR) technique combined with decalcified freeze-dried bone allograft (DFDBA)[8] and platelet rich plasma (PRP) technique[9] have been used in the treatment of intraosseous cystic cavities.
CASE REPORT
In this case report, clinical, histological and radiographical findings and periodontal treatment of a 32-year-old female patient, who was referred to the Department of Periodontology, Faculty of Dentistry, Marmara University with a painless hyperplastic inflamed lesion on the distobuccal side of the tooth number 12, were presented [Figure 1]. The patient was systemically healthy and wasn't taking any medicine or over the counter remedies, which may affect periodontal tissue metabolism. Clinical examination revealed slight plaque accumulation and mild gingival redness and edema with no radiographical bone loss. Plaque associated gingivitis was diagnosed based on the clinical and radiographical examination. Full mouth clinical periodontal parameters were as follows the mean plaque index (PI) 1.69 ± 0.34, gingival index (GI) 1.72 ± 0.42, and probing depth (PD) 2.45 ± 0.73 mm.
Figure 1.

Clinical appearance and radiographical image of the lesion
Dimension of the hyperplastic lesion on oral mucous membrane was recorded as 4.0 × 4.0 mm at intraoral examination. The tooth number 12 had no mobility and no response to horizontal and vertical percussion tests and was vital based on the results of electric pulp test. Radiographical examination revealed a well-defined round radiolucent area with corticated borders, which was <1 cm diameter [Figure 1]. The mean PI, GI, PD (mm) measured from six sites of the tooth number 12 was 1.1 ± 0.11, 1.09 ± 0.09, 2.83 ± 0.40, respectively and there was no access to the lesion area through periodontal sulcus. Preliminary diagnosis of the lesion was LPC based on clinical and radiographical findings.
Mechanical periodontal treatment consisted of oral hygiene instructions, scaling and root planing was applied and flap operation was performed to gain access to the lesion. First, the hyperplastic gingival lesion was removed [Figure 2]. Then, sulcular incisions from distal line angle of the tooth number 11 to mesial line angle of the tooth number 14 and vertical releasing incisions were carried out on the buccal site [Figure 2]. Similar sulcular incisions were performed palatinally without any vertical incision. Buccal and palatinal mucoperiostal flaps were reflected and all granulation tissues were removed. Tunnel shape alveolar bone cavity extending from buccal to palatinal site [Figure 2] was grafted with bovine-derived xenograft (Geistlich Bio-Oss® Spongious Bone Substitute Granules 0.25 mm−1 mm/0.5 g, Wolhusen, Switzerland) [Figure 2] followed by placement of a resorbable collagen membrane (Geistlich Bio-Gide® Membrane 16 mm × 22 mm, Wolhusen, Switzerland) to stabilize graft material [Figure 2]. Flaps were sutured with 5/0 polyglycolide-co-lactide braided absorbable suture material (Dogsan Pegelak® 5/0, 16 mm 3/8, cutting suture, Trabzon, Turkey) [Figure 2]. Amoxicillin/clavulanic acid 2 × 1 for 5 days (Augmentin-BID® 1000 mg 10 tablets, GlaxoSmithKline, London, England) and naproxen sodium 2 × 1 for 5 days (Apranax Fort® 550 mg 10 film tablets, Abdi İbrahim, İstanbul, Turkey) were prescribed to the patient to prevent any possible postoperative complication. Clinical healing was achieved without any postoperative complication such as pain, hemorrhage, swelling or recurrence and initial radiolucency disappeared at 6 months follow-up period [Figure 3].
Figure 2.

Surgical treatment of the lesion
Figure 3.

Clinical healing and radiographical image at the 6 months follow-up period
Removed tissue sample was fixated in 10% formaldehyde solution, sectioned and stained with hematoxylen-eosin. Histological examination under light microscope showed vasculature granulomatous structure and overlying squamous epithelium, all of which were consisted with LPC [Figure 4].
Figure 4.
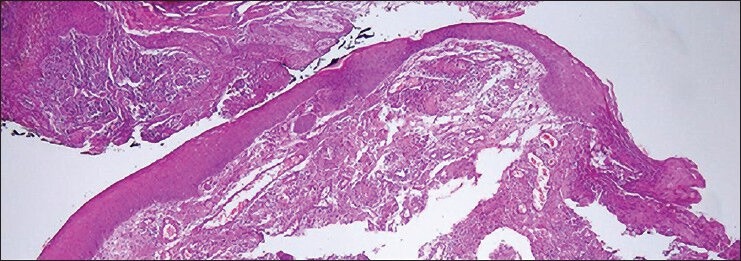
Histological section that shows epithelial lining of lateral periodontal cyst, mild chronic inflammation in the connective tissue
DISCUSSION
Lateral periodontal cyst, an uncommon noninflammatory lesion of the oral cavity, is an intraosseous cyst associated with the root of a vital tooth, which presents no signs or symptoms clinically. Occasionally, a small swelling of the gingiva or alveolar mucosa may be seen[7] and the diagnosis is generally established by means of a routine radiological examination as it was observed in our case.
In this case, the patient had a painless lesion, which was smaller than 1 cm, on the alveolar mucosa of distobuccal aspect of the tooth number 12. Electric pulp test findings confirmed over clinical examination that the tooth number 12 was vital. Radiographical examination revealed that a radiolucent area with corticated borders, that were smaller than 1 cm related with the tooth number 12.
Differential diagnosis is of importance, since misdiagnosis may lead to false or unnecessary treatment of the lesion.[7] It is important that the clinicians are aware of odontogenic keratocysts occupying a lateral periodontal position frequently. Keratocysts must be differentiated from the LPCs because of their aggressiveness and high potential for recurrence following surgical removal. In addition, gingival cyst, lateral radicular cyst, pseudocysts and radiolucent odontogenic tumors must also be considered in differential diagnosis of LPC.[10]
Histologically, LPC is composed of a cystic cavity with a noninflammatory[4]/inflammatory[7,11] connective tissue wall with fine nonkeratinized squamous epithelial lining. This case presented an epithelial lining of LPC, and the presence of mild chronic inflammation in the connective tissue.
Treatment approach of LPC is generally enucleation of the cyst, leaving the bone cavity to be filled spontaneously.[12] Any endodontic treatment or periapical surgery of the affected teeth was unnecessary, since all proved vital.[12] In our case, using the principles of GTR,[13] the bone cavity was grafted with bovine-derived xenograft covered by resorbable collagen membrane. Bovine-derived xenografts have osteoconductive properties that provide a scaffold for regenerative cells of patient in bone cavity. Collagen membrane is a physical barrier to prevent migration of cells without regenerative properties to bone cavity. Nart et al.[8] indicated the bone fill of the defect radiographically, which was demonstrated by re-entry after the treatment of an LPC using GTR, along with bone grafting 7 months postoperatively. In our case, because of ethical issues re-entry couldn't be performed. Even though, Nart et al.[8] had selected the DFDBA for grafting cystic cavity, we preferred the bovine-derived xenograft since its combined application with resorbable collagen membrane was reported excellent clinical and radiographical results in periodontal regeneration.[14] Subramaniam et al.[9] treated an intraosseous cystic cavity using PRP without grafting. Although this study showed promising results in the treatment of intraosseous cystic cavities, PRP still lacks consistent clinical outcome in periodontal regeneration.[15,16]
The patients are advised to be followed radiographically to monitor for recurrence and regeneration of bony defect.[17] In our case, clinical healing was acceptable without recurrence, except the scar formation because of vertical incisions of flap design, and radioopacity on the distobuccal site of the tooth number 12 was observed, due to stabilized graft material in the cystic cavity, after 6 months follow-up period.
Satisfactory clinical and radiographical outcome can be achieved in the treatment of LPC using the principles of GTR.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Kramer IR, Pindborg JJ, Shear M. 2nd ed. Geneva: Springer-Verlag; 1992. WHO Histological Typing of Odontogenic Tumours; pp. 34–118. [Google Scholar]
- 2.Wood K, Goaz P. 5th ed. St. Louis: Mosby; 1997. Differential Diagnosis of Oral and Maxillofacial Lesions; pp. 305–6. [Google Scholar]
- 3.Demirkol M, Ege B, Yanik S, Aras MH, Ay S. Clinicopathological study of jaw cysts in southeast region of Turkey. Eur J Dent. 2014;8:107–11. doi: 10.4103/1305-7456.126260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen DA, Neville BW, Damm DD, White DK. The lateral periodontal cyst. A report of 37 cases. J Periodontol. 1984;55:230–4. doi: 10.1902/jop.1984.55.4.230. [DOI] [PubMed] [Google Scholar]
- 5.Altini M, Shear M. The lateral periodontal cyst: An update. J Oral Pathol Med. 1992;21:245–50. doi: 10.1111/j.1600-0714.1992.tb01004.x. [DOI] [PubMed] [Google Scholar]
- 6.Soares de Lima AA, Naval Machado MÂ, Braga AM, De Souza MH. Lateral periodontal cyst: Aetiology, diagnosis and clinical significance. A review and report of case. Rev de Clín Pesqui Odontol. 2005;1:55–9. [Google Scholar]
- 7.Angelopoulou E, Angelopoulos AP. Lateral periodontal cyst. Review of the literature and report of a case. J Periodontol. 1990;61:126–31. doi: 10.1902/jop.1990.61.2.126. [DOI] [PubMed] [Google Scholar]
- 8.Nart J, Gagari E, Kahn MA, Griffin TJ. Use of guided tissue regeneration in the treatment of a lateral periodontal cyst with a 7-month reentry. J Periodontol. 2007;78:1360–4. doi: 10.1902/jop.2007.060483. [DOI] [PubMed] [Google Scholar]
- 9.Subramaniam P, Kumar K, Ramakrishna T, Bhadranna A. Bone regeneration with plasma-rich-protein following enucleation of traumatic bone cyst. Eur J Dent. 2013;7:377–81. doi: 10.4103/1305-7456.115427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Andrade M, Silva AP, de Moraes Ramos-Perez FM, Silva-Sousa YT, da Cruz Perez DE. Lateral periodontal cyst: Report of case and review of the literature. Oral Maxillofac Surg. 2012;16:83–7. doi: 10.1007/s10006-010-0257-2. [DOI] [PubMed] [Google Scholar]
- 11.Saygun I, Ozdemir A, Safali M. Lateral periodontal cyts. Turk J Med Sci. 2001;31:375–8. [Google Scholar]
- 12.Formoso Senande MF, Figueiredo R, Berini Aytés L, Gay Escoda C. Lateral periodontal cysts: A retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal. 2008;13:E313–7. [PubMed] [Google Scholar]
- 13.Sculean A, Stavropoulos A, Windisch P, Keglevich T, Karring T, Gera I. Healing of human intrabony defects following regenerative periodontal therapy with a bovine-derived xenograft and guided tissue regeneration. Clin Oral Investig. 2004;8:70–4. doi: 10.1007/s00784-004-0254-7. [DOI] [PubMed] [Google Scholar]
- 14.Gupta R, Pandit N, Malik R, Sood S. Clinical and radiological evaluation of an osseous xenograft for the treatment of infrabony defects. J Can Dent Assoc. 2007;73:513. [PubMed] [Google Scholar]
- 15.Ozdemir B, Okte E. Treatment of intrabony defects with beta-tricalciumphosphate alone and in combination with platelet-rich plasma. J Biomed Mater Res B Appl Biomater. 2012;100:976–83. doi: 10.1002/jbm.b.32660. [DOI] [PubMed] [Google Scholar]
- 16.Camargo PM, Lekovic V, Weinlaender M, Divnic-Resnik T, Pavlovic M, Kenney EB. A surgical reentry study on the influence of platelet-rich plasma in enhancing the regenerative effects of bovine porous bone mineral and guided tissue regeneration in the treatment of intrabony defects in humans. J Periodontol. 2009;80:915–23. doi: 10.1902/jop.2009.080600. [DOI] [PubMed] [Google Scholar]
- 17.Valério GM, Cury PR. Diagnosis and treatment of lateral periodontal cyst: Report of three clinical cases. Rev Odontol Cinc. 2009;24:213–7. [Google Scholar]


