Abstract
Background:
Dental products are widely used by patients and dental personnel alike and may cause problems for both. Dental materials could cause contact allergy with varying manifestations such as burning, pain, stomatitis, cheilitis, ulcers, lichenoid reactions localized to the oral mucosa in patients, and hand dermatitis in dental personnel. Patch testing with the dental series comprising commonly used materials can be used to detect contact allergies to dental materials.
Aim:
This study aimed to identify contact allergy among patients who have oral mucosal lesions after dental treatment and among dental personnel who came in contact with these materials.
Materials and Methods:
Twenty patients who had undergone dental procedures with symptoms of oral lichen planus, oral stomatitis, burning mouth, and recurrent aphthosis, were included in the study. Dental personnel with history of hand dermatitis were also included in the study. Patch testing was performed using Chemotechnique Dental Series and results interpreted as recommended by the International Contact Dermatitis Research Group (ICDRG).
Results:
Out of 13 patients who had undergone dental treatment/with oral symptoms, six patients with stomatitis, lichenoid lesions, and oral ulcers showed positive patch tests to a variety of dental materials, seven patients with ulcers had negative patch tests, seven dental personnel with hand dermatitis showed multiple allergies to various dental materials, and most had multiple positivities.
Conclusion:
The patch test is a useful, simple, noninvasive method to detect contact allergies among patients and among dental personnel dealing with these products. Long term studies are necessary to establish the relevance of these positive patch tests by eliminating the allergic substances, identifying clinical improvement, and substituting with nonallergenic materials.
Keywords: Contact allergy, dental series, patch test
INTRODUCTION
Dental products are widely used by patients, dentists, and dental technicians. They may cause problems both for patients undergoing dental treatment and for dental personnel because of occupational exposure. The relevance of allergic reactions to dental materials is poorly understood.[1] The oral mucosa, including the lips, is constantly exposed to a large number of potentially irritating and sensitizing substances. Hand dermatitis characterized by itching, burning, erythema, fissuring, and scaling due to dental products can occur in dental personnel dealing with dental materials. However, most dental materials are intended for long term use and this exposure may sensitize patients, resulting in contact allergies. The clinical manifestations of contact allergy to dental materials are not uniform. Patients may present with subjective complaints affecting the oral mucosa, including burning and pain and more objective manifestations such as stomatitis, cheilitis, and lichenoid reactions localized to the buccal mucosa, tongue, and lips.[2] Removal of these offending agents and replacement with nonallergenic material may have a beneficial effect for the patient. Patch testing with dental series containing the commonly used materials can be used to detect contact allergies to these dental materials.[3,4] This study is aimed at identifying the allergens causing allergy and to analyze positive patch test reactions in patients who have oral mucosal lesions after dental treatment and in dental personnel who are in contact with these materials.
MATERIALS AND METHODS
This study was carried out among 20 people, all females; 13 were patients with oral symptoms after dental treatment and seven were dental personnel including dental technicians with dermatitis of hands. After obtaining informed consent, patients who had undergone dental procedures with symptoms of oral lichen planus, oral stomatitis, recurrent aphthosis, and burning mouth/tongue were included in the study. Dental personnel with a history of hand dermatitis were also included in the study. Pregnant, lactating mothers, and patients on corticosteroids and immunosuppressives and were excluded from the study. After filling the case record form, patch testing was performed using Chemotechnique Dental Series [Table 1]. It is a standardized series of 30 materials commonly used in dentistry. Using Finn Chambers, the allergens present in the dental series were placed and then strapped to the patient's back. After 48 hours, the chambers were removed and the areas where the chambers were placed were outlined and marked with a marker pen. The readings were recorded on day 2 (after 48 hours), day 3 (72 hours), and day 4 (96 hours). Positive patch test was identified by the presence of erythema, papules, and vesicles and the results interpreted as recommended by the International Contact Dermatitis Research Group (ICDRG).
Table 1.
Dental series

The positive patch test was recorded and correlated with the clinical symptoms. Clinical relevance is defined by specific morphological symptoms in the oral cavity or hands together with a positive patch test reaction to dental materials containing the suspected contact allergen.
RESULTS
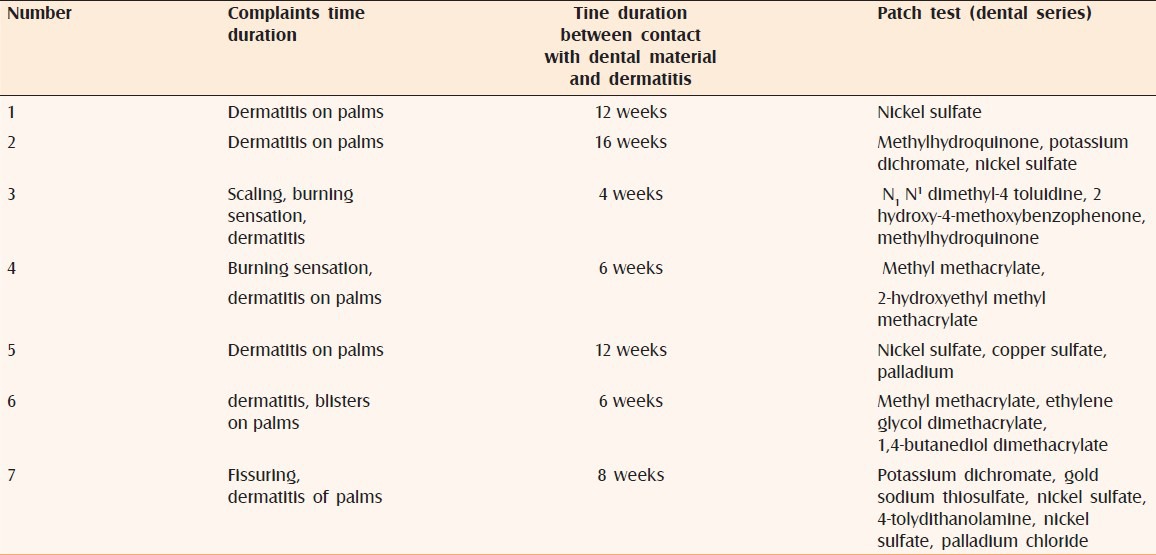
Of 13 patients who had undergone dental treatment/with oral symptoms, three had oral lichenoid lesions with positive patch tests to metals, including nickel, potassium chromate, copper sulfate, and amalgam; two had stomatitis with positive reactions to methylhydroquinone; one had stomatitis with a positive reaction to potassium chromate, nickel, and palladium, and seven patients with dentures had ulcers with a negative patch test. The onset of oral symptoms was between 1 and 12 weeks after dental treatment [Table 2]. Seven dental personnel with hand dermatitis showed multiple allergies to various dental materials which included N1 N1 dimethyl-4 toluidine, 2 hydroxy-4-methoxybenzophenone, methylhydroquinone, nickel sulfate, copper sulfate, palladium, methyl methacrylate, ethylene glycol dimethacrylate, and 1,4-butanediol dimethacrylate. The duration of onset of dermatitis varied from 4 to 16 weeks [Table 3].
Table 2.
Positive patch in relation to clinical presentation in patients
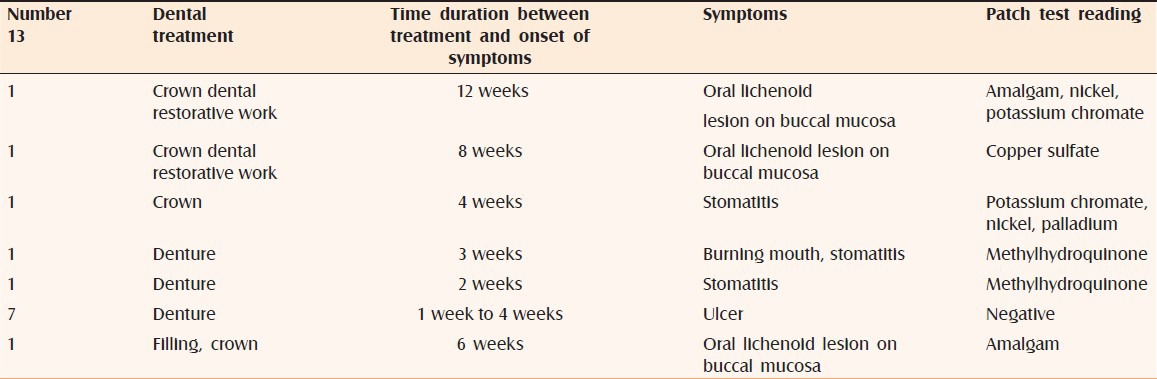
Table 3.
Positive patch in relation to clinical presentation in dental personnel
DISCUSSION
Contact allergy is not uncommon among dental professionals and patients. Patch testing is a reliable, easy, noninvasive test to detect contact allergies. A dental screening series from the beginning of the 1980s[5] was originally used for both stomatitis patients and those handling dental products, but since 1997, the addition of a dental series for dental personnel was started.
In a study by Khamaysi et al. in patients with oral symptoms, who had undergone dental treatment, the common allergens detected included gold sodium thiosulfate (14.0%), nickel sulfate (13.2%), mercury (9.9%), palladium chloride (7.4%), cobalt chloride (5.0%), and 2-hydroxyethyl methacrylate (5.8%).[4] In another study by Goon et al.,[6] the most common allergens in this group were the (meth) acrylate monomers and elemental mercury.
Contact allergy to (meth) acrylates among dental professionals has been well studied[7] and there are numerous epidemiologic studies available in the medical literature. In contrast, published information on contact allergy to (meth) acrylates among dental patients has mainly been case reports.[8,9] In dentistry, acrylics are used to make dentures and other prostheses, for the repair of fractured prostheses. Acrylics are strong occupational sensitizers, especially for dental personnel,[10] but sensitization of patients from dental acrylics other than dental prostheses is rare.[11]
Dental composite resins (DCRs) are used for restoration work include filling, bridges, and crowns, and many other aspects of cosmetic dentistry. Both dentists and dental technicians handle DCRs. Allergic contact dermatitis to DCRs has been reported to occur in dental personnel but it is less common than acrylate allergy.[12] Allergic reactions to an ethylene amine activator used in several polymeric materials, including impression materials and temporary crown materials, are one of two most commonly reported adverse effects to dental materials.[13] About one in four reactions to materials used in dental treatments are related to metals, especially chromium, cobalt, nickel, and gold alloys used for metal–ceramic restorations.[14] The literature indicates that allergic reactions to gold-based restorations were more common than to nickel-containing alloys.[15] Hildebrand et al. reviewed 139 published cases of allergy to base metal alloys in removable partial dentures.[16] Gingivitis and stomatitis were the most common clinical symptoms, but remote reactions occurred in almost 25% patients. However, mucosal reactions to metal-based partial dentures are rare.
Prosthodontic restorations and appliances consist of many designs including conventional and implant-supported crowns, fixed prostheses (dental bridges), and removable prostheses or dentures. Various prosthetic treatments are known to cause allergic reactions both in patients and dental personnel.[4]
Resin-based materials comprising liquid methyl methacrylate (MMA) monomers and poly-methyl--meth-acrylate (PMMA) powder are the most commonly used polymers in dental prostheses. MMA monomer may result in toxic reactions and allergic responses in previously sensitized individuals, especially if undercured.
The acrylic monomer usually contains an inhibitor or stabilizer, such as hydroquinone, and a polymer, an initiator such as benzoyl peroxide or dimethyl-p-toluidine (or a tertiary amine). When the monomer and polymer are mixed, the benzoyl peroxide initiates the reaction, and a hard, solid, high-molecular-weight polymer is produced. In the heat cure, the reaction is essentially complete, but after cold cure, it is likely that very small amounts of the residual monomer will be left unpolymerized. This residual monomer is capable of inducing stomatitis and angular cheilitis in sensitized individuals. Kaaber et al. have published 12 cases of allergic reactions to dental acrylic materials resulting in burning mouth syndrome and stomatitis.[17] Symptoms of patients sensitized to dental acrylates include lichenoid reactions, stomatitis, burning mouth, perioral eczema, and urticaria-like complaints. The mechanism behind those reactions is not yet clear.
Certain additives in acrylic denture material may also be sensitizers. Thus hydroquinone, the inhibitor in the monomer, may sensitize and can cause cheilitis and stomatitis.[18] In our study, two patients with stomatitis and one dental personnel with dermatitis had positive patch tests to methylhydroquinone. Crissey cited four instances in which hypersensitivity stomatitis resulted from acrylic dentures. The onset of symptoms followed fitting of the acrylic dentures by periods varying from one week to four years.[19] In a report from India, two patients with oral lesions reacted to triethylene glycol dimethacrylate.[20] Our patient who had stomatitis due to dentures had a positive patch test to methylhydroquinone and not acrylates and two dental personnel developed dermatitis due to acrylates.
Tosti et al. reported one case of contact stomatitis in a woman traced to N1 N1 dimethyl-para-toluidine used as an accelerator for the acrylic reaction.[21] In our study, one dental personnel who had dermatitis had a positive patch test to N1 N1 dimethyl-para-toluidine.
Palladium is becoming well recognized as an allergen usually in combination with nickel sensitivity.[22] It is used in dental alloys and therefore may be expected to cause stomatitis occasionally. In our study, one dental personnel and one patient with oral lichenoid lesions had positive patch tests to palladium and nickel.
Allergic sensitivity to copper is rare. One patient had oral lichenoid lesions and showed a positive patch test to copper. Frykholm et al. reported that allergy to copper derived from dental alloys may produce oral lesions of lichen planus.[23]
Allergy to dental materials has been implicated as a causative factor in cutaneous as well as oral lichen planus, burning mouth syndrome, aphthae, and stomatitis. Some have proposed a ‘dental restoration metal intolerance syndrome based on correlations between positive patch tests to elements present in the patient's restorations and clinical improvement of symptoms with the removal of restorations. Although mercury is the most commonly studied and reported allergen, oral mucosal diseases have been reported in association with allergies to a range of metals including copper, chromate, nickel, palladium, and gold.[24] Out of three patients who had oral lichenoid lesions, one had a positive patch test to amalgam and nickel, chromate, and gold, and one patient was positive to palladium, in addition to these metals. Only one patient had a positive patch test to amalgam alone.
Several studies of contact allergy to acrylates in dental professionals have been published.[6,25] Two of our dental personnel had positive reactions to various forms of acrylate. It is common that methacrylate-allergic patients have simultaneous allergic reactions to several acrylate test substances although they have probably not been exposed to all of the positive compounds. Some of the multiple reactions probably derive from cross-allergy between acrylic monomers. However, it is difficult to establish an individual's history of exposure to various acrylic monomers in dental materials because the patients will have used various different products during their working life, and dental products often contain many undeclared acrylic monomers.[26] Occupational allergies from dental personnel have been reported more commonly than mucosal allergies in dental patients as mucosal allergy develops less commonly than via the cutaneous route. This is because it is postulated that the action of saliva and increased absorption of haptens reduces the amount of contact between allergen and antigen-presenting cells of the mucosa.[14] This study highlights the importance of patch testing to detect allergens in patients with oral mucosal lesions and dental personnel with dermatitis. The relevance of these positive reactions can be established only after elimination of these allergenic materials, detecting clinical improvement, and substituting with nonallergenic materials. Long term studies are necessary to establish the relevance. Protective nonallergenic gloves will be necessary for dental personnel dealing with these allergic products.
CONCLUSION
Various contact allergies due to dental materials are known to occur. The patch test is a useful, simple, noninvasive method to detect contact allergies in patients and in dental personnel dealing with these products. Eliminating the offending agent and substituting with nonallergenic material may bring relief to the patients. Further long term research is needed to establish the relevance of the causative allergens to the allergies, by eliminating them and providing alternative materials which are nonallergic.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.De Rossi SS, Greenberg MS. Intraoral contact allergy: A literature review and case reports. J Am Dent Assoc. 1998;129:1435–41. doi: 10.14219/jada.archive.1998.0078. [DOI] [PubMed] [Google Scholar]
- 2.Reap U, Stiesch M, Reh M, Kapp A, Werfel T. Investigation of contact allergy to dental metals in 206 patients. Contact Dermatitis. 2009;60:339–43. doi: 10.1111/j.1600-0536.2009.01524.x. [DOI] [PubMed] [Google Scholar]
- 3.Alanko K, Kanerva L, Jolanki R, Kannas L, Estlander T. Oral mucosal diseases investigated by patch testing with a dental screening series. Contact Dermatitis. 1996;34:263–7. doi: 10.1111/j.1600-0536.1996.tb02197.x. [DOI] [PubMed] [Google Scholar]
- 4.Khamaysi Z, Bergman R, Weltfriend S. Positive patch test reactions to allergens of the dental series and the relation to the clinical presentations. Contact Dermatitis. 2006;55:216–8. doi: 10.1111/j.1600-0536.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 5.Axell T, Bjorkner B, Fregert S, Niklasson B. Standard patch test series for screening of contact allergy to dental materials. Contact Dermatitis. 1983;9:82–4. doi: 10.1111/j.1600-0536.1983.tb04640.x. [DOI] [PubMed] [Google Scholar]
- 6.Goon AT, Isaksson M, Zimerson E, Goh CL, Bruze M. Contact allergy to (meth) acrylates in the dental series in southern Sweden: Simultaneous positive patch test reaction patterns and possible screening allergens. Contact Dermatitis. 2006;55:219–26. doi: 10.1111/j.1600-0536.2006.00922.x. [DOI] [PubMed] [Google Scholar]
- 7.Wrangsjo K, Swartling C, Meding B. Occupational dermatitis in dental personnel: Contact dermatitis with special reference to (meth) acrylates in 174 patients. Contact Dermatitis. 2001;45:158–63. doi: 10.1034/j.1600-0536.2001.045003158.x. [DOI] [PubMed] [Google Scholar]
- 8.Koutis D, Freeman S. Allergic contact stomatitis caused by acrylic monomer in a denture. Australas J Dermatol. 2001;42:203–6. doi: 10.1046/j.1440-0960.2001.00517.x. [DOI] [PubMed] [Google Scholar]
- 9.Kanerva L, Alanko K, Estlander T. Allergic contact gingivo stomatitis from a temporary crown made of methacrylates and epoxy diacrylates. Allergy. 1999;54:1316–21. doi: 10.1034/j.1398-9995.1999.00074.x. [DOI] [PubMed] [Google Scholar]
- 10.Kanerva L, Estlander T, Jolanki R. Occupational skin allergy in the dental profession. Dermatol Clin. 1994;12:517–32. [PubMed] [Google Scholar]
- 11.Kanerva L, Estlander T, Jolanki R, Tarvainen K. Occupational allergic contact dermatitis caused by work with dental prostheses. Contact Dermatitis. 1993;28:268–75. doi: 10.1111/j.1600-0536.1993.tb03430.x. [DOI] [PubMed] [Google Scholar]
- 12.Kanerva L, Estlander T, Jolanki R. Allergic contact dermatitis from dental composite resins due to aromatic epoxy acrylates and aliphatic acrylates. Contact Dermatitis. 1989;20:201–11. doi: 10.1111/j.1600-0536.1989.tb04657.x. [DOI] [PubMed] [Google Scholar]
- 13.Churgin LS, Payne JC. Sensitized tissue response to an ethylene imines derivative transitional crown material. J Prosthetic Dent. 1981;46:179–80. doi: 10.1016/0022-3913(81)90305-x. [DOI] [PubMed] [Google Scholar]
- 14.Moee F, Hayat Khan Y, Ghani F. Safety and hazards of materials used in the fabrication of dental prostheses. J Pak Mater Soc. 2008;20:2–1. [Google Scholar]
- 15.Hensten-Pettersen A. Casting alloys: Side effects. Adv Dent Res. 1992;6:38–43. doi: 10.1177/08959374920060011401. [DOI] [PubMed] [Google Scholar]
- 16.Hildebrand HF, Veron C, Martin P. Nonprecious metal dental alloys and allergy. J Biol Buccale. 1989;17:227–43. [PubMed] [Google Scholar]
- 17.Kaaber S, Thulin H, Nielsen E. Skin sensitivity to denture base materials in the burning mouth syndrome. Contact Dermatitis. 1979;5:90–6. doi: 10.1111/j.1600-0536.1979.tb04805.x. [DOI] [PubMed] [Google Scholar]
- 18.Torres V, Mano-Azul AC, Correia T, Soares AP. Allergic contact cheilitis and stomatitis from hydroquinone in an acrylic dental prosthesis. Contact Dermatitis. 1993;29:102–3. doi: 10.1111/j.1600-0536.1993.tb03499.x. [DOI] [PubMed] [Google Scholar]
- 19.Crissey JT. Stomatitis, dermatitis and denture materials. Arch Dermatol. 1965;92:45–8. [PubMed] [Google Scholar]
- 20.Santosh V, Ranjith K, Shenoi SD, Sachin V, Balachandran C. Results of patch testing with dental materials. Contact Dermatitis. 1999;40:50–1. doi: 10.1111/j.1600-0536.1999.tb05980.x. [DOI] [PubMed] [Google Scholar]
- 21.Tosti A, Bardazzi F, Piancastelli E, Brasile GP. Contact stomatitis due to N N-dimethyl-para-toludine. Contact Dermatitis. 1990;22:113. doi: 10.1111/j.1600-0536.1990.tb01533.x. [DOI] [PubMed] [Google Scholar]
- 22.Fowler JF. Allergic contact dermatitis to metals. Am J Contact Dermatitis. 1990;1:212. [Google Scholar]
- 23.Frykholm KO, Frithiof L, Fernström AI, Moberger G, Blohm SG, Björn E. Allergy to copper derived from dental alloys as a possible cause of oral lesions of lichen planus. Acta Derm Venereol. 1969;49:268–81. [PubMed] [Google Scholar]
- 24.Koch P, Bahmer FA. Oral lichenoid lesions, mercury hypersensitivity and combined hypersensitivity to mercury and other metals: Histologically-proven reproduction of the reaction by patch testing with metal salts. Contact Dermatitis. 1995;33:323–8. doi: 10.1111/j.1600-0536.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- 25.Geukens S, Goossens A. Occupational contact allergy to (meth) acrylates. Contact Dermatitis. 2001;44:153–9. doi: 10.1034/j.1600-0536.2001.044003153.x. [DOI] [PubMed] [Google Scholar]
- 26.Kanerva L. Cross-reactions of multifunctional methacrylates and acrylates. Acta Odontol Scand. 2001;59:320–9. doi: 10.1080/000163501750541200. [DOI] [PubMed] [Google Scholar]


