Abstract
Angiokeratomas (AK) are a group of capillary vascular malformations encompassing several unrelated conditions, predominantly seen on the lower extremities. AK can be classified into localized and diffuse forms. The diffuse forms comprise Fabry's disease, which is the result of α-galactosidase deficiency. The cutaneous AK includes the Mibelli type, the Fordyce type, angiokeratoma circumscriptum (AC), and ‘solitary and multiple papular angiokeratoma’. We describe a case of AC with unusual features including late onset and palmar affection. Amongst the possible therapeutic options, cryotherapy was considered. However, the patient was lost to follow up.
Keywords: Angiokeratoma circumscriptum, late onset, palmar, solitary
INTRODUCTION
The term angiokeratoma (AK) is derived from three Greek words meaning vessels, horn, and tumor.[1] These lesions are not true angiomas but are merely telangiectasias of preexisting vessels.[1] The basic abnormality is dilatation of the papillary capillaries with resultant secondary epidermal changes of hyperkeratosis and acanthosis, as a means of preventing further dilatation and rupture.[1] Angiokeratoma circumscriptum (AC) is one of the types of localized angiokeratoma (LAK) and is a rare vascular malformation characterized by asymptomatic hyperkeratotic vascular skin lesions. LAK have a prevalence of 0.16%.[2] Lesions of AC are typically situated unilaterally on the lower legs or feet, but can occur on the thighs, buttocks, or occasionally elsewhere.[3] The age of onset of AC is generally at birth. Late onset AC has been reported, however this is rare.[4,5] Involvement of the palms by AC, as in this case, is also uncommon.
CASE REPORT
A 53-year-old female presented with a single, bluish-red, progressively increasing lesion, over the left palm with occasional bleeding, since 5 years. There was no history of trauma prior to occurrence of the lesion. On examination, there was a soft, tender, bluish-red minimally scaly, keratotic plaque measuring 2 × 2 cm on the thenar eminence. Telangiectatic vessels were visible on the surface [Figure 1]. On magnoscopic examination, yellow structureless areas, peripheral erythema, peripheral red streaks (representing telengiectasias), hemorrhagic crusts, and lacunae were seen [Figures 2 and 3]. Histopathology showed hyperkeratosis, parakeratosis, and acanthosis. Multiple dilated vascular spaces lined by thinned out endothelium and filled with blood were present mainly in the papillary dermis, with elongation of rete ridges [Figures 4 and 5]. Other laboratory investigations were within normal limits. General physical and systemic examination revealed no other abnormality. On the basis of morphological appearance of an erythematous bluish plaque with prominent telengiectasia and histological appearance, a diagnosis of late onset AC was made.
Figure 1.

Soft, tender, bluish-red minimally scaly, keratotic plaque over the thenar eminence with overlying telangiectasias
Figure 2.
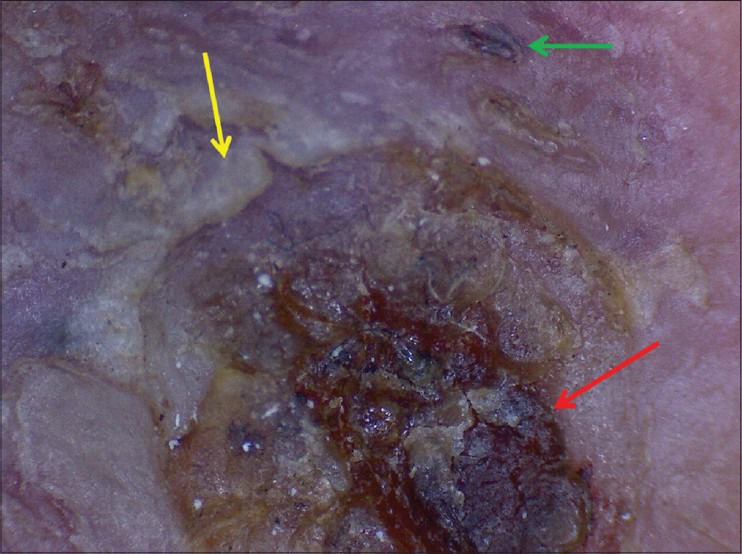
Magnoscopic image: Hemorrhagic crusts (red arrow), yellow structureless area (yellow arrow), and lacunae (green arrow)
Figure 3.
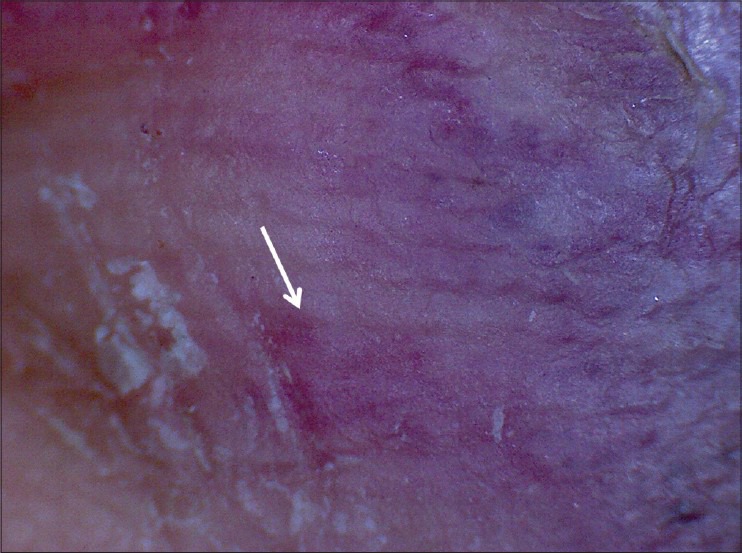
Magnoscopic image: Peripheral erythema and red peripheral streaks, representing telengiectasias (white arrow)
Figure 4.
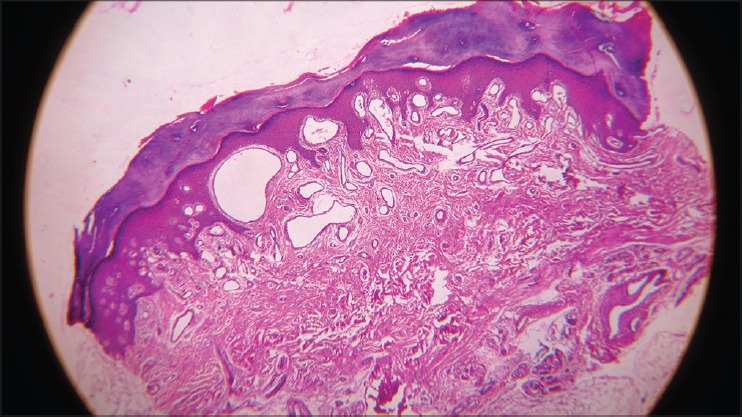
Epidermis showing hyperkeratosis, parakeratosis and acanthosis with elongation of rete ridges. Multiple dilated vascular spaces lined by thinned out endothelium and filled with blood are present mainly in the papillary dermis (H and E, ×10)
Figure 5.
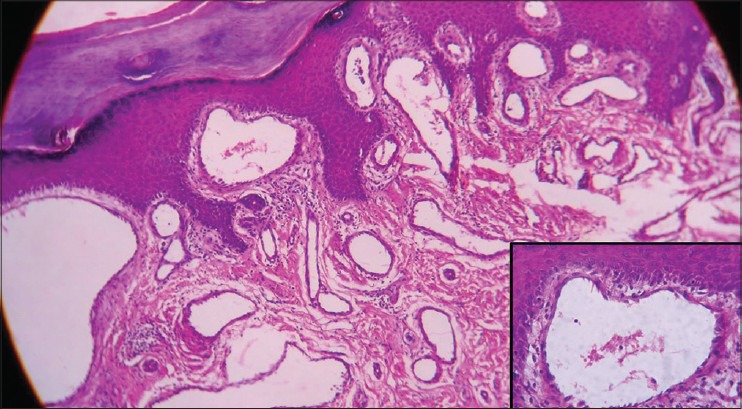
Papillary dermal dilated vascular channel with thinned out endothelium and elongated rete ridges (H and E, ×40). Inset: Thinned out endothelium is better appreciated (H and E, ×100)
DISCUSSION
On the basis of their historic aspects and clinical appearance, AK have been grouped traditionally into localized (purely cutaneous) or widespread types. The current division of LAK includes the following: (i) Bilateral form occurring on the dorsa of the fingers and toes-angiokeratoma of Mibelli, (ii) localized scrotal form-angiokeratoma of Fordyce, (iii) plaque form-AC, (iv) solitary papular angiokeratoma, and (v) localized vulval form-angiokeratoma of the vulva.[1] Most forms of LAK present during the first two decades of life. Among these five types of LAK, solitary AK is the most common while AC is the least frequent.[2] AC presents as unilateral localized hyperkeratotic vascular skin lesions, affecting females more often than males usually in infancy or early childhood. Late onset, as in this case has only been rarely reported.[4,5] The telengiectatic component and the plaque morphology in our case suggested a diagnosis of AC. Two subtypes of AC seem to be present. The first type consists of a plaque made up of small, grouped, discrete papules with only microscopic evidence of hyperkeratosis. In the second type papules and nodules vary in size, frequently become a confluent plaque, and show macroscopic hyperkeratosis.[6] Our patient appears to have the second subtype. In contrast, AK of Fabry typically presents before puberty and have a coexisting systemic affection. Solitary AK generally arises during the second to fourth decades or later. However, solitary AK consists of much a smaller lesion than AC and is a warty, black papule, rather than plaque, usually on the lower limbs. AK is usually asymptomatic, but with local trauma they may become irritated and can bleed, given their highly vascular nature. The pathogenesis and clinical presentation of the various AK are variable, but the histological features are similar in all the forms.[7] Histopathology shows ectatic, thin-walled vascular spaces in the papillary dermis intimately associated with, and variably encased by, acanthotic epidermis with elongated rete ridges and hyperkeratosis. Partial or virtually complete occlusion of these dilated vessels by intravascular fibrin thrombi in various degrees of organization is common. Clinically, when thrombosed and deeply pigmented, angiokeratoma can be mistaken for malignant melanoma and potentially result in unnecessary patient anxiety and inappropriate radical excision. Verrucous hemangiomas, first described by Imperial and Helwig in 1967[1] may mimic AC. However, verrucous hemangioma is congenital and characterized histologically by dilated capillaries and large cavernous, endothelial-lined, blood-filled spaces extending well into the reticular dermis and subcutaneous fat with hyperkeratosis. The deeper vascular component can be a reliable feature distinguishing verrucous hemangioma from AK.[8] It is thus important to obtain an adequate deep biopsy specimen for ruling out verrucous hemangioma. The pathogenesis of angiokeratoma is uncertain. The primary event is considered vascular ectasia within the papillary dermis, just beneath the basement membrane. The epidermal pathologic changes seem to be a secondary reaction. Increased proliferative capacity on the surface of vascular malformations and the close location of the vascular spaces with the epidermis could explain the reactive epidermal growth.[9] An acute or chronic trauma, chilblains, high venous pressure, or nevoid or vascular malformation are considered the causative factors in the LAK.[3] Although there was no overt history of trauma remembered by the patient, this could still be the plausible cause in our case. Local excision or electrocautery are the best treatments for smaller lesions, while the larger lesions require wide, deep excision, and grafting. It responds to the common means of physical therapy (diathermocoagulation, cryotherapy, and Argon laser) and recurrences are rare as opposed to verrucous hemangioma.[3] Our patient was offered cryotherapy; however, the patient was lost to follow up. This case has been presented due to the rare features of AC seen in this case in the form of late onset and palmar location.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Imperial R, Helwig EB. Angiokeratoma. A clinicopathological study. Arch Dermatol. 1967;95:166–75. doi: 10.1001/archderm.95.2.166. [DOI] [PubMed] [Google Scholar]
- 2.Ozdemir R, Karaaslan O, Tiftikcioglu YO, Kocer U. Angiokeratoma circumscriptum. Dermatol Surg. 2004;30:1364–6. doi: 10.1111/j.1524-4725.2004.30413.x. [DOI] [PubMed] [Google Scholar]
- 3.Mittal R, Aggarwal A, Srivastava G. Angiokeratoma circumscriptum: A case report and review of the literature. Int J Dermatol. 2005;44:1031–4. doi: 10.1111/j.1365-4632.2005.02252.x. [DOI] [PubMed] [Google Scholar]
- 4.Talwar S, Suresh MS, Jha PK. Angiokeratoma circumscriptum: Some unusual features. Indian J Dermatol Venereol Leprol. 1992;58:120–1. [Google Scholar]
- 5.Bruce DH. Angiokeratoma circumscriptum and angiokeratoma scroti. Arch Dermatol. 1960;81:388–93. doi: 10.1001/archderm.1960.03730030046007. [DOI] [PubMed] [Google Scholar]
- 6.Lynch PJ, Kosanovich M. Angiokeratoma circumscriptum. Arch Dermatol. 1967;96:665–8. [PubMed] [Google Scholar]
- 7.Requena L, Sangueza OP. Cutaneous vascular abnormalities. Part I. Hamartomas, malformations, and dilatation of preexisting vessels. J Am Acad Dermatol. 1997;37:523–49. doi: 10.1016/s0190-9622(97)70169-5. [DOI] [PubMed] [Google Scholar]
- 8.Clairwood MQ, Bruckner AL, Dadras SS. Verrucous hemangioma: A report of two cases and review of the literature. J Cutan Pathol. 2011;38:740–6. doi: 10.1111/j.1600-0560.2011.01733.x. [DOI] [PubMed] [Google Scholar]
- 9.Schiller PI, Itin PH. Angiokeratomas: An update. Dermatology. 1996;193:275–82. doi: 10.1159/000246270. [DOI] [PubMed] [Google Scholar]


