INTRODUCTION
Compression therapy is the mainstay of treatment of venous leg ulcers (VLU). Good wound care and compression therapy will heal majority of small venous ulcers of short duration.[1] Goals of compression therapy are ulcer healing, reduction of pain and edema, and prevention of recurrence.[2] Compression is used for VLU and narrows veins and restores valve competence and reduces ambulatory venous pressure, thus reducing venous reflux (VR). It also helps decrease inflammatory cytokines, accelerates capillary flow, and lowers capillary fluid leakage thereby alleviating limb edema. It also softens lipodermatosclerosis, improves lymphatic flow and function, and enhances fibrinolysis.[3]
Indications
The aim of compression therapy is to improve the venous function without compromising arterial function.
Contraindications
The contraindications of compression therapy are the following[4,5]
Advanced peripheral obstructive arterial disease (ankle brachial pressure index [ABPI] <0.8) (Evidence level A)
Systemic arterial pressure <80 mm Hg at ankle
Phlegmasia cerulea dolens
Uncontrolled congestive heart failure
Abscesses
Septic phlebitis
Advanced peripheral neuropathy.
CLASSIFICATION
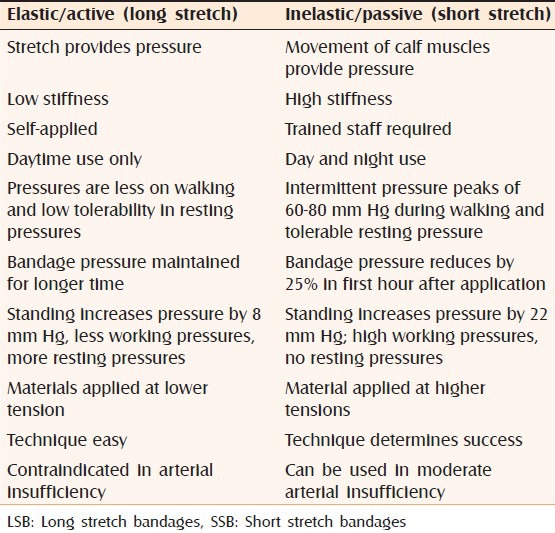
Compression can be broadly divided into bandages and compression stockings. The details are mentioned in Table 1.[6,7] The compression bandages can be classified as inelastic (short stretch bandages [SSB]) and elastic (long stretch bandages [LSB]). The differences between the two groups of bandages are elucidated in Table 2.
Table 1.
Types of compression therapy
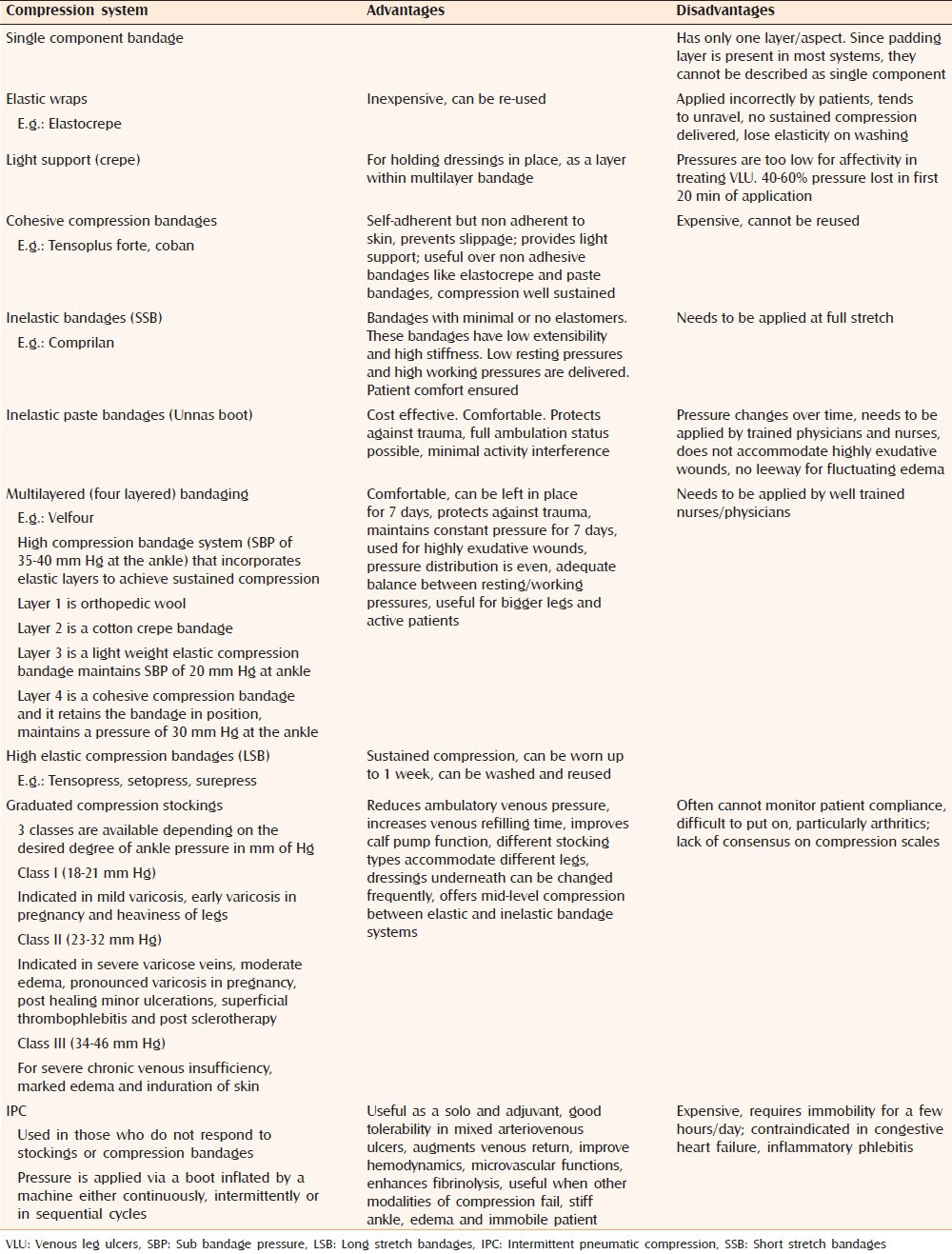
Table 2.
Comparison between elastic (LSB) and inelastic compression bandages (SSB)
COMPRESSION BANDAGES
All bandages used in compression must be applied on top of padding (subcompression wadding bandage) to prevent friction and pressure damage over bony prominences by spreading pressure across a greater area. Bandages should generally be applied toe to knee at 50% stretch and with 50% overlap but specific manufacturer's instructions should be followed for each bandage. Interface pressure peaks on the leg during walking exceeding 50-60 mm Hg reduce VR and increase venous pumping function. This may be achieved by stiff compression textiles like multicomponent bandages, especially when containing cohesive material or by zinc paste bandages. These compression types exert high stiffness which is characterized by a tolerable resting pressure and high pressure peaks during walking (“working pressure”), but need to be applied by well trained and experienced staff. Short stretch adjustable Velcro-wraps and (double) compression stockings may be promising alternatives allowing self-management.
INTERMITTENT PNEUMATIC COMPRESSION
Intermittent pneumatic compression constitutes inflating and deflating an airtight bag worn around leg. IPC controls edema in case compression bandage and stocking has failed. IPC upon compression therapy may accelerate ulcer healing.[8] It is particularly useful in patients with restricted mobility and when concomitant arterial disease is detected, where it helps reduce edema and enhance arterial blood flow.[9,10] IPC may improvement in hematologic, hemodynamic and endothelial effects which explains its role in healing of VLU.[11]
HEAD TO HEAD COMPARISON BETWEEN VARIOUS MODALITIES OF COMPRESSION
Compression versus no compression/usual care/simple dressings
Various guidelines have recommended that some compression is better than no compression[12,13] (evidence level A). A Cochrane review in 2009[4] (evidence level A) compared compression with either primary dressing, noncompressive bandages and usual care that always did not include compression and concluded that venous ulcers healed faster with compression and some form of compression is better than no compression in healing VLU.
High compression versus low compression
High compression bandages provide and maintain high levels of compression pressures in the range 25-35 mm Hg at the ankle. High compression is useful for bigger legs or more active patients. They can be used over padding on their own or as part of a layered system, and should be applied in a spiral according to manufacturer's instructions. Evidence exists that high compression is better than low compression in managing VLU[4,12,13,14,15] (evidence level A).
Single component versus multicomponent bandage systems and single layer versus multilayer
Studies have emphasized the fact that multi-layering increases stiffness of bandages and increases sub bandage pressure (SBP), thereby being inelastic practically. It ensures even distribution of SBP[4,12,16] (evidence level A). SBP of 30-40 mm Hg is recommended for healing of VLU (level of evidence A). Multicomponent multilayered compression is superior to a single component, single layer compression bandage systems.
Inelastic versus elastic bandages (long stretch bandages vs. short stretch bandages)
Two studies[17,18] demonstrated superiority of inelastic bandages in healing venous ulcers and reducing VR over elastic bandages. Short stretch compression (inelastic) and Unna's boot was found to support the pump function better than a long stretch compression (elastic)[19,20] (evidence level A).
Compression stockings
Use of a Class I or II stocking in patients with chronic venous insufficiency (CVI) led to reduction in the lower leg volume of 55-70 ml[14] (evidence level C).
Stockings (single layer/two-layer) versus bandages
A Cochrane review[4] identified two trials of compression bandages versus single layer compression stocking. No difference was detected among single layer stocking when compared to paste based bandages (Evidence level A). However healing outcome was better when a two layered stocking was compared to SSB (evidence level A). A meta-analysis of eight heterogenous randomized-controlled clinical trials (RCTs) concluded that stockings are better than compression bandages. There was better impact on pain, quicker healing by 3 weeks and increased ease of use with stockings[21] (level of evidence B). Pain scores were better for compression stockings than compression bandages[4,22] (level of evidence A). A well-chosen and correctly calibrated compression stocking exerting a pressure of 35 mm Hg or more is a good alternative to bandages in healing VLU[23,24] (level of evidence B).
Compression and surgery
Multiple sources and studies have shown that selective compression enhances sclerotherapy results[25,26] (level of evidence B). A RCT compared subfascial endoscopic perforator surgery with ambulatory compression and concluded that healing rates and recurrence rates in both modalities of treatment were same. However, the study recommended a combination of both for optimal results[27] (level of evidence B).
Intermittent pneumatic compression with or without compression versus compression alone
Berliner et al.[28] (evidence level A) reviewed eight studies, three of which showed that compression pumps could alleviate symptoms of CVI and assist with the healing of longstanding chronic ulcerations. A systematic Cochrane review identified four trials of IPC + Compression versus compression alone (Unnas boot/four layer dressing/stockings)[29] (evidence level A). Only one trial showed lesser time to heal and increased rate of reduction in ulcer area, although it could not identify any difference in ulcer healing between the two groups. Further studies are required to assess the status of IPC as alternative/adjuvant to compression and to optimize cycle times and IPC duration per day to effectively heal VLU.
Compression therapy modification in peripheral arterial disease
In patients with arterial occlusive disease (ABPI 0.6-0.8) modified compression using stiff material applied with reduced pressure (<40 mm Hg) under careful control may increase both arterial flow and venous pumping function. Compression decreases the elevated pressure within the venous system and may also increase arterial blood flow according to recent data in patients with mixed ulcers[30,31,32,33,34,35], (evidence level B).
Drawbacks of compression therapy
Correct application of compression bandages need expertise
Older debilitated patients with comorbidities find it difficult to use compression stockings
Peripheral vascular compromise in patients with mixed-arterial venous ulcers with low ABPI
Reduced compliance due to wearer discomfort.
CONCLUSION
Compression therapy is a highly effective treatment for VLU. Care should be taken while administering this therapeutic modality in case of mixed-arteriovenous ulcers. The minimum tolerable compression pressure tailored to the patient's requirement should be ensured so as to maximize compliance.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Phillips TJ. Current approaches to venous ulcers and compression. Dermatol Surg. 2001;27:611–21. doi: 10.1046/j.1524-4725.2001.00195.x. [DOI] [PubMed] [Google Scholar]
- 2.Abu-Own A, Scurr JH, Coleridge Smith PD. Effect of leg elevation on the skin microcirculation in chronic venous insufficiency. J Vasc Surg. 1994;20:705–10. doi: 10.1016/s0741-5214(94)70157-1. [DOI] [PubMed] [Google Scholar]
- 3.Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment of venous ulcers. Am J Surg. 2004;188:1–8. doi: 10.1016/S0002-9610(03)00284-8. [DOI] [PubMed] [Google Scholar]
- 4.O’Meara S, Cullum NA, Nelson EA. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2009:CD000265. doi: 10.1002/14651858.CD000265.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Nelson EA, Harper DR, Prescott RJ, Gibson B, Brown D, Ruckley CV. Prevention of recurrence of venous ulceration: Randomized controlled trial of class 2 and class 3 elastic compression. J Vasc Surg. 2006;44:803–8. doi: 10.1016/j.jvs.2006.05.051. [DOI] [PubMed] [Google Scholar]
- 6.Choucair M, Phillips TJ. Compression therapy. Dermatol Surg. 1998;24:141–8. doi: 10.1111/j.1524-4725.1998.tb04067.x. [DOI] [PubMed] [Google Scholar]
- 7.Morison MJ. London: Wolfe; 1992. A Colour Guide to the Nursing Management of Wounds. [Google Scholar]
- 8.Smith PC, Sarin S, Hasty J, Scurr JH. Sequential gradient pneumatic compression enhances venous ulcer healing: A randomized trial. Surgery. 1990;108:871–5. [PubMed] [Google Scholar]
- 9.Eze AR, Comerota AJ, Cisek PL, Holland BS, Kerr RP, Veeramasuneni R, et al. Intermittent calf and foot compression increases lower extremity blood flow. Am J Surg. 1996;172:130–4. doi: 10.1016/S0002-9610(96)00134-1. [DOI] [PubMed] [Google Scholar]
- 10.Delis KT, Nicolaides AN, Wolfe JH, Stansby G. Improving walking ability and ankle brachial pressure indices in symptomatic peripheral vascular disease with intermittent pneumatic foot compression: A prospective controlled study with 1-year follow-up. J Vasc Surg. 2000;31:650–61. doi: 10.1067/mva.2000.103969. [DOI] [PubMed] [Google Scholar]
- 11.Comerota AJ. Intermittent pneumatic compression: Physiologic and clinical basis to improve management of venous leg ulcers. J Vasc Surg. 2011;53:1121–9. doi: 10.1016/j.jvs.2010.08.059. [DOI] [PubMed] [Google Scholar]
- 12.Fletcher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. BMJ. 1997;315:576–80. doi: 10.1136/bmj.315.7108.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cullum N, Nelson EA, Fletcher AW, Sheldon TA. Compression bandages and stockings for venous leg ulcers. Cochrane Database Syst Rev. 2000:CD000265. doi: 10.1002/14651858.CD000265. [DOI] [PubMed] [Google Scholar]
- 14.Strolin A, Volkert B, Hafner HM, Junger M. Medical compression stockings in CVI-Patients. Phlebologie. 2005;34:34–41. [Google Scholar]
- 15.Amsler F, Blättler W. Compression therapy for occupational leg symptoms and chronic venous disorders-a meta-analysis of randomised controlled trials. Eur J Vasc Endovasc Surg. 2008;35:366–72. doi: 10.1016/j.ejvs.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 16.Moffatt CJ, Franks PJ, Oldroyd M, Bosanquet N, Brown P, Greenhalgh RM, et al. Community clinics for leg ulcers and impact on healing. BMJ. 1992;305:1389–92. doi: 10.1136/bmj.305.6866.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Partsch H, Menzinger G, Mostbeck A. Inelastic leg compression is more effective to reduce deep venous refluxes than elastic bandages. Dermatol Surg. 1999;25:695–700. doi: 10.1046/j.1524-4725.1999.98040.x. [DOI] [PubMed] [Google Scholar]
- 18.Moody M. Comparison of Rosidal K and SurePress in the treatment of venous leg ulcers. Br J Nurs. 1999;8:345–55. doi: 10.12968/bjon.1999.8.6.6660. [DOI] [PubMed] [Google Scholar]
- 19.Partsch H. The static stiffness index: A simple method to assess the elastic property of compression material in vivo. Dermatol Surg. 2005;31:625–30. doi: 10.1111/j.1524-4725.2005.31604. [DOI] [PubMed] [Google Scholar]
- 20.Polignano R, Bonadeo P, Gasbarro S, Allegra C. A randomised controlled study of four-layer compression versus Unna's Boot for venous ulcers. J Wound Care. 2004;13:21–4. doi: 10.12968/jowc.2004.13.1.26563. [DOI] [PubMed] [Google Scholar]
- 21.Amsler F, Willenberg T, Blättler W. In search of optimal compression therapy for venous leg ulcers: A meta-analysis of studies comparing diverse [corrected] bandages with specifically designed stockings. J Vasc Surg. 2009;50:668–74. doi: 10.1016/j.jvs.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 22.Scriven JM, Taylor LE, Wood AJ, Bell PR, Naylor AR, London NJ. A prospective randomised trial of four-layer versus short stretch compression bandages for the treatment of venous leg ulcers. Ann R Coll Surg Engl. 1998;80:215–20. [PMC free article] [PubMed] [Google Scholar]
- 23.Kurz X, Kahn SR, Abenhaim L, Clement D, Norgren L, Baccaglini U, et al. Chronic venous disorders of the leg: Epidemiology, outcomes, diagnosis and management. Summary of an evidence-based report of the VEINES task force. Venous insufficiency epidemiologic and economic studies. Int Angiol. 1999;18:83–102. [PubMed] [Google Scholar]
- 24.Partsch H, Horakova MA. Compression stockings in treatment of lower leg venous ulcer. Wien Med Wochenschr. 1994;144:242–9. [PubMed] [Google Scholar]
- 25.Weiss RA, Sadick NS, Goldman MP, Weiss MA. Post-sclerotherapy compression: Controlled comparative study of duration of compression and its effects on clinical outcome. Dermatol Surg. 1999;25:105–8. doi: 10.1046/j.1524-4725.1999.08180.x. [DOI] [PubMed] [Google Scholar]
- 26.Tazelaar DJ, Neumann HA, De Roos KP. Long cotton wool rolls as compression enhancers in macrosclerotherapy for varicose veins. Dermatol Surg. 1999;25:38–40. doi: 10.1046/j.1524-4725.1999.08005.x. [DOI] [PubMed] [Google Scholar]
- 27.van Gent WB, Hop WC, van Praag MC, Mackaay AJ, de Boer EM, Wittens CH. Conservative versus surgical treatment of venous leg ulcers: A prospective, randomized, multicenter trial. J Vasc Surg. 2006;44:563–71. doi: 10.1016/j.jvs.2006.04.053. [DOI] [PubMed] [Google Scholar]
- 28.Berliner E, Ozbilgin B, Zarin DA. A systematic review of pneumatic compression for treatment of chronic venous insufficiency and venous ulcers. J Vasc Surg. 2003;37:539–44. doi: 10.1067/mva.2003.103. [DOI] [PubMed] [Google Scholar]
- 29.Nelson EA, Mani R, Thomas K, Vowden K. Intermittent pneumatic compression for treating venous leg ulcers. Cochrane Database Syst Rev. 2011:CD001899. doi: 10.1002/14651858.CD001899.pub3. [DOI] [PubMed] [Google Scholar]
- 30.Mosti G, Iabichella ML, Partsch H. Compression therapy in mixed ulcers increases venous output and arterial perfusion. J Vasc Surg. 2012;55:122–8. doi: 10.1016/j.jvs.2011.07.071. [DOI] [PubMed] [Google Scholar]
- 31.Humphreys ML, Stewart AH, Gohel MS, Taylor M, Whyman MR, Poskitt KR. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007;94:1104–7. doi: 10.1002/bjs.5757. [DOI] [PubMed] [Google Scholar]
- 32.Grey JE, Harding KG, Enoch S. Venous and arterial leg ulcers. BMJ. 2006;332:347–50. doi: 10.1136/bmj.332.7537.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.A consensus document. London: MEP Ltd; 2008. World Union of Wound Healing Societies Initiative (WUWHS) compression in venous leg ulcers. [Google Scholar]
- 34.Hopf HW, Ueno C, Aslam R, Burnand K, Fife C, Grant L, et al. Guidelines for the treatment of arterial insufficiency ulcers. Wound Repair Regen. 2006;14:693–710. doi: 10.1111/j.1524-475X.2006.00177.x. [DOI] [PubMed] [Google Scholar]
- 35.Obermayer A, Göstl K, Partsch H, Benesch T. Venous reflux surgery promotes venous leg ulcer healing despite reduced ankle brachial pressure index. Int Angiol. 2008;27:239–46. [PubMed] [Google Scholar]


