ASSESSMENT
Management of venous leg ulcers (VLUs) should include a comprehensive assessment of all patients presenting with a leg ulcer.
This should include:
Leg ulcer history
Examination of the leg and ulcer
Investigations to support diagnosis
Comprehensive assessment should be made on initial presentation and at regular intervals thereafter to guide on-going management.
The surface area of the ulcer should be measured serially over time (Evidence level C).
Clinical grade, etiology, anatomy, pathophysiology classification can be used for assessment (Evidence level E).
Digital image measurement was significantly quicker and offered number advantages than contact tracing (Evidence level C).
Venous color flow Doppler imaging: Is a gold standard investigation for the assessment of the venous system of lower limb + Evidence level B.
All patients with chronic VLU should have an ankle brachial pressure index (ABPI) performed prior to treatment (Evidence level D).
Compression therapy is usually considered to be contraindicated with an ankle brachial index <0.8).
Ankle brachial pressure index should also be conducted when the ulcer is deteriorating, ulcer not healed fully by 12 weeks or there is recurrence of ulcer (Evidence level B).
Pulse oximetry is not routinely recommended, but may be a useful adjunctive investigative tool in specialist leg ulcer clinics.
Apparent venous ulcers that have been open continuously without signs of healing for 3 months and do not respond to treatment in 3 months should undergo biopsy (Evidence level C).
Leg ulcer patients with dermatitis/eczema should be considered for patch-testing using a leg ulcer series (Evidence level C).
Bacteriological swabbing is unnecessary unless there is evidence of clinical infections Grade B.
MANAGEMENT OF PATIENT
Dressings
Irrigation of wound with tap water and saline is sufficient (Evidence level E).
Dressing technique should be clean and aimed at preventing cross-infection (Evidence level E).
Dressing should be simple, low or nonadherent, low cost and acceptable to the patient (Evidence level A).
No single dressing material is favored (Evidence level C).
Use dressings or bandages impregnated with zinc oxide to provide comfort and promote epithelialization of a healthy granulated superficial VLU (Evidence level E).
Topicals
Antibiotics are indicated in cases of overt wound infection where the classical signs of infection are Evidence level C.
Iodine reduces bacterial load, decreases infection rates, and promotes healing (Evidence level C).
Cadexomer iodine: Leads to reduction of methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa with evidence from clinical reports of efficacy in stimulating healing (Evidence level C).
There is insufficient evidence on which to base a recommendation for mupirocin.
Debridement
Mechanical debridement should be carried out by appropriately trained practitioners (Evidence level C).
SYSTEMIC THERAPY
Systemic antibiotic should only be used in cases of clinical infection and not for bacterial colonization (Evidence level C).
Use of pentoxifylline (400 mg 3 times daily for up to 6 months) to improve healing should be considered in patients with VLUs (Evidence level A).
Zinc did not show any significant difference in the healing of VLU (Evidence level A).
There is insufficient good quality evidence on which to base a recommendation for micronized purified flavonoid fraction and phlebotonic drugs in chronic VLU.
The role of eicosanoids (prostaglandins) or prostaglandin antagonists in the treatment of venous ulcers lacks sufficient data to allow a recommendation.
Calcium dobesilate – No evidence exists to demonstrate efficacy of calcium dobesilate in healing VLU.
Fibrinolytic enhancement with an anabolic steroid such as stanozolol in conjunction with compression therapy may be useful in treating lipodermatosclerosis associated with venous ulcers (Evidence level B) but no evidence to support its use routinely in VLU sildenafil. cilostazole, iloprost. There is no good quality evidence currently to recommend these medications in routine therapy of VLU.
COMPRESSION THERAPY
Compression therapy has been proven beneficial for venous ulcer treatment and is the standard of care (Evidence level A).
Graduated, multi-layered high compression system with adequate padding should be the first line of treatment for uncomplicated VLUs with ABPI ≥ 0.8 in all settings (Evidence level A).
High compression achieved better healing rates than low compression (Evidence level A).
Insufficient evidence to recommend intermittent pneumatic therapy with or without compression for VLU.
Short stretch compression (inelastic) and Unna's boot was found to support the pump function better than a long stretch compression (elastic) (Evidence level A).
A well-chosen and correctly calibrated compression stocking exerting a pressure of 35 mmHg or more is a good alternative to bandages in healing VLU (Evidence level B).
Pentoxifylline is effective when used with compression therapy for venous ulcers, and may be useful (Evidence level A).
OTHER SUPPORTIVE MEASURE
Elevate the patient's leg to promote changes in microcirculation and decrease lower limb edema (Evidence level C).
Calf muscle exercises are recommended to improve calf muscle function (Evidence level B).
Patient of leg ulcer with suspected malnourishment should be assessed by a nutritionist and dietician (Evidence level E).
Optimize the patient's nutrition and hydration to promote healing in patients with VLUs and increase protein intake in highly exuding wounds (Evidence level E).
Large ulcers (>10 cm2) and long duration of ulcer leads to poorer health related quality of life (HRQoL) index (Evidence level D).
Electrical stimulation therapy can be used as an adjunctive treatment of venous ulcers (Evidence level B).
Hyperbaric oxygen can only be recommended as an adjunctive treatment in selected refractory cases of VLUs (Evidence level C).
There is insufficient evidence on which to base a recommendation for vacuum assisted closure in chronic VLU.
No benefit of low-level laser therapy on leg ulcer healing (Evidence level A).
Large ulcers (>10 cm2) and long duration of ulcer leads to poorer HRQoL index (Evidence level D).
RECOMMENDATIONS FOR SURGERY
Patient with chronic VLU and superficial venous reflux should be considered for surgery to promote ulcer healing and to prevent recurrence of the ulcer (Evidence level B).
Closing the venous ulcer with an autologous skin graft may provide a short-term goal of found closure, but does not address the increased ambulatory venous pressure (Evidence level E).
SCLEROTHERAPY
Sclerotherapy is indicated for the superficial varicosities and incompetent perforators surrounding the ulcer this also helps in fast healing of ulcers (Evidence level D).
Compression improves the results of sclerotherapy Grade B.
PREVENTION OF RECURRENCE
Diet modifications, nutritional supplements, cessation of smoking, weight reduction, maintaining a healthy cardiac status, and strong psychosocial supports can be practiced to prevent leg ulcers (Evidence level E).
Elevation of lower limb may reduce recurrence of venous ulcer (Evidence level D).
Progressive resistance exercise can be considered in patients as a measure to prevent recurrences (Evidence level D).
Below-knee graduated compression hosiery is recommended to prevent recurrence of VLU in patients where leg ulcer healing has been achieved Grade A.
Continued use of compression therapy reduces the risk of venous ulcer recurrence (Evidence level B).
Surgical correction of superficial venous reflux in addition to compression bandaging on long term follow-up has contributed significantly to bringing down rates of ulcer recurrence Grade B.
Sclerotherapy may reduce the risk of venous ulcer recurrence (Evidence level C).
CONCLUSION
The treatment of chronic venous ulcers is a therapeutic challenge. A comprehensive diagnostic evaluation is therefore essential at the start of treatment. For venous ulcers apart from conservative treatment reduction of venous hypertension is critical, with compression therapy occupying an important place in achieving this. Patients with nonhealing venous ulcers who have had compression therapy and have no deep vein incompetence are recommended for superficial venous surgery, foam sclerotherapy or ligation of the affected vein as an important aspect of the overall treatment plan. Prevention of recurrences includes regular clinical evaluations, patient education about skin care, elevation, exercise and life-long compression therapy.Figure 1 summarizes these recommendations.
Figure 1.
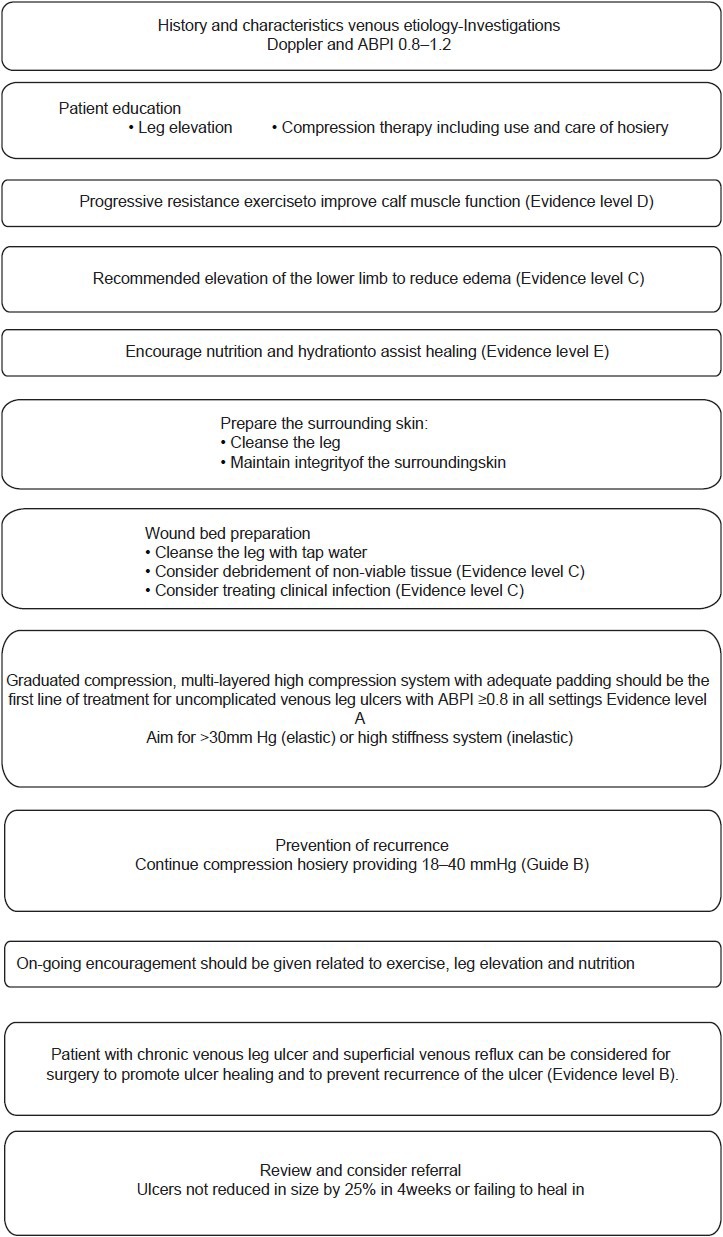
Management of leg ulcers
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.


