Abstract
BACKGROUND
Cardiovascular mortality is high among diabetic patients due to abnormalities in the plasma lipid and lipoprotein metabolism, and increased oxidative stress. This study aimed to investigate the effects of active vitamin D on serum lipids and oxidative stress markers in type 2 diabetic patients.
METHODS
A double-blind randomized placebo-controlled trial was carried out in 70 participants with type 2 diabetes, aged 30-75 years of age. The participants were randomly assigned to two groups. One group received two capsules of calcitriol (0.25 µg 1,25-dihydroxycholecalciferol per capsule) per day. The second group received placebo tablets. All participants received their oral hypoglycemic drugs as prescribed by the endocrinologist. At the beginning, after 6 weeks, and at the end of the 12-week supplementation trial, serum total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglyceride (TG), and serum malondialdehyde (MDA) levels were measured.
RESULTS
There was a significant reduction in total cholesterol, LDL-cholesterol, TG, and MDA levels in both treatment and placebo groups (P < 0.05). Serum HDL-cholesterol level decreased significantly in the placebo group (P < 0.05), while it remained unchanged in the treatment group. However, the P values related to the between group’s comparisons were not significant for any variables.
CONCLUSION
Active vitamin D reduced lipid profile and oxidative stress markers in diabetic patients compared to the control group, but these alterations were not statistically significant
Keywords: Diabetes Mellitus, Lipoproteins, Oxidative Stress, Vitamin D
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity in the world. In 2005, CVD accounted for approximately 30% of deaths worldwide.1,2 In diabetic patients, coronary atherosclerosis risk is 3-5 times greater than non-diabetics, despite controlling other risk factors.3 The high cardiovascular mortality rate in diabetics could be attributed to abnormalities in lipid and lipoprotein metabolism and up-regulated oxidative stress.4,5
The classic role of vitamin D is maintaining calcium homeostasis and bone health.6,7 However, in recent years, new functions are proposed for this vitamin such as prevention of certain types of cancer, diabetes mellitus, auto-immune disorders, and CVD.8
Low serum level of 25-hydroxycholecalciferol (25(OH)D) is associated with CVD, diabetes, obesity, hypertension, and dyslipidemia.9 In a meta-analysis of cross-sectional and observational studies, Parker et al. have reported a 43% reduction in cardiometabolic disorders in those with the highest serum concentration of 25(OH)D.10,11 Several mechanisms could be involved in this association such as controlling blood pressure, glycemia, body fat percent, and serum lipids by vitamin D.8,12-15
Glucose tolerance abnormalities negatively affect the lipid profile.16 In addition to lipid abnormalities, increased oxidative stress is an obvious feature of diabetes mellitus, which is related to cardiovascular risk.17 The results of experimental studies approved the role of active vitamin D in lipid metabolism.18
On the other hand, it is reported in some studies that diabetes mellitus can reduce serum concentration of 25(OH)D.16
There are limited data on antioxidant properties of vitamin D, but in some studies, its antioxidant potential was considered to be even stronger than vitamin E and melatonin.19,20
Regarding increased prevalence of CVD in diabetic patients, and with respect to the role of vitamin D in lipid and lipoprotein metabolism and oxidative stress reduction, this study aimed to investigate the effects of active vitamin D on serum lipids and oxidative stress marker in type 2 diabetic patients.
Materials and Methods
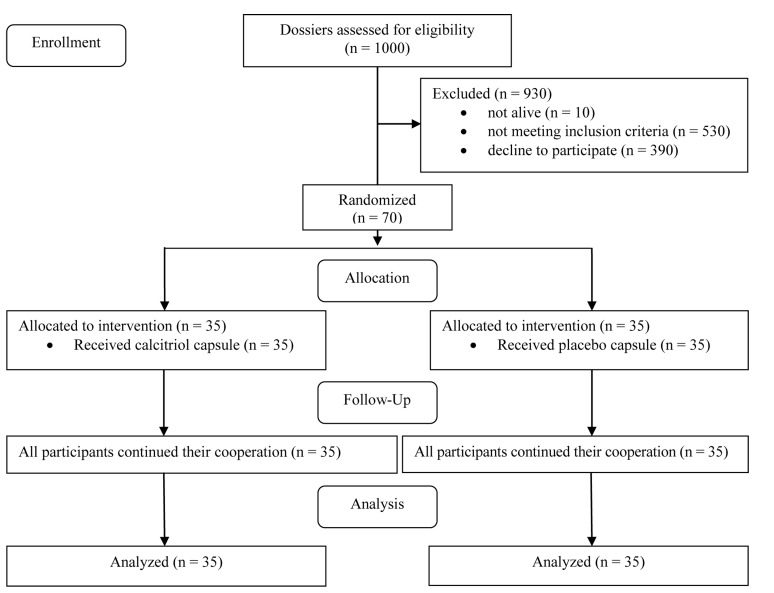
This study is a part of a larger study conducted in 2011.21Figure 1 shows the flow diagram of the trial.
Figure 1.
Flow diagram of the trial
Study participants
In this double-blind randomized placebo-controlled trial, 70 participants of which 35 males and 35 females with type 2 diabetes and hyperlipidemia, aged 30-75 years, on treatment with oral hypoglycemic and hypolipidemic drugs were recruited from the outpatient Motahari Clinic at Shiraz University of Medical Sciences, Shiraz, Iran. To find our cases, we evaluated 1000 dossiers in the diabetes clinic and called the patients. Ten of these patients had died before the researchers’ call. A large number of them (n = 530) did not meet the inclusion and hence were excluded. Eligible patients were invited to participate in the trial, but 390 of them declined to participate. Finally, 70 patients participated in the trial.
No severe fluctuation was seen in their plasma glucose and hence there was no need to change their drugs dosage. Criteria for case inclusion were well-controlled fasting plasma glucose, serum calcium < 10.5 mg/dl, controlled low-density lipoprotein (LDL)-cholesterol, normal liver and kidney function and no history of kidney stone and hypercalcemia. The exclusion criteria included taking insulin for diabetes control, taking calcium and vitamin D supplements, history of diseases affecting vitamin D status, and intestinal malabsorptive disease.
At the beginning of the study, participants were given an oral and written explanation of the study, including its benefits and procedure, and were asked to read and sign an informed consent document.
The study protocol was reviewed and approved by the Human Ethics Committee of Research council of the Vice Chancellor for research affairs of Shiraz University of Medical Sciences. The code and date of ethical approval was 2009/8/3 and 88-4617. Iranian clinical trial registration number of this study is IRCT138806282480N1.
Background characteristics assessment
Demographic data were collected by interviews and anthropometric indices were determined for each subject. Anthropometric assessments included measurement of weight and height. Body weight was measured to the nearest 0.1 kg using the Seca 713 scale, while subjects were minimally clothed. Height was determined using non stretchable measuring tape, without shoes and subsequently body mass index was calculated by dividing weight (kg) by squared height (m2). All equipments were calibrated every morning.
Intervention design
This 12 weeks clinical trial was conducted between August and November month of 2009. Using balanced block randomization method, we allocated the patients randomly into one of the two study groups: treatment and placebo group. One group received two capsules of calcitriol (0.25 mcg 1,25-dihydroxycholecalciferol per each capsule) per day. The second group received identical-looking placebo tablets. All calcitriol tablets and their placebo had the same color and shape and were produced by Zahravi Pharmacy Company (Tehran, Iran). All the participants received their oral hypoglycemic drugs as well, as prescribed by the endocrinologist. The participants were asked not to take any vitamin or supplements during the trial. The researcher supervised the ingestion of supplements each week.
Biochemical assessment
At the beginning, after 6 weeks, and at the end of the 12 week supplementation trial, 10 ml fasting venous blood samples were drawn from the patients’ arms after 12 h fasting. Blood was collected for measurement of serum total-cholesterol, LDL, high-density lipoprotein (HDL), triglyceride (TG), and malondialdehyde (MDA). Total cholesterol, HDL, and TG were measured by spectrophotometric methods. Serum LDL-cholesterol was calculated using Friedwald formula.22 Serum concentrations of MDA were measured by the modified thiobarbituric acid method (spectrophotometric method).23
Statistical analysis
The normality of distributions was checked for all variables. Data processing and analysis were performed using SPSS for windows (version 15.5, SPSS Inc., Chicago, IL, USA). Normally distributed data were expressed as mean (± standard deviation). Baseline characteristics of treatment and placebo groups were compared using independent Samples t-test. General linear model repeated measures analysis was used for comparing triple measurements in each group. Significance level was set at P < 0.05.
Results
A total of 70 diabetic patients (35 males and 35 females) participated in our study. Background characteristics of the participants are displayed in table 1.
Table 1.
Comparison of the baseline characteristics between treatment and placebo group
| Variable | Treatment | Placebo | P* |
|---|---|---|---|
| Gender (%) | |||
| Male | 10 (28.5) | 10 (28.5) | > 0.999 |
| Female | 25 (71.5) | 25 (71.5) | |
| Age (year) | 53.8 ± 8.9** | 52.4 ± 7.8 | 0.462 |
| Weight (kg) | 72.9 ± 12.7 | 70.9 ± 12.5 | 0.514 |
| Height (cm) | 160.3 ± 8.9 | 161.1 ± 10.4 | 0.718 |
| BMI (kg/m2) | 28.3 ± 4.4 | 27.0 ± 3.4 | 0.164 |
| Education (year) | 7.2 ± 4.5 | 7.2 ± 4.8 | 0.980 |
| Diabetes duration (year) | 6.3 ± 5.3 | 6.6 ± 4.8 | 0.819 |
| Metformin (mg/day) | 1450.0 ± 700.0 | 1200.0 ± 600.0 | 0.110 |
| Glybenclamide (mg/day) | 16.0 ± 6.5 | 14.5 ± 8.5 | 0.437 |
| Atorvastatin (mg/day) | 20.2 ± 9.2 | 18.4 ± 6.8 | 0.605 |
Independent samples t-test;
Mean ± SD;
SD: Standard deviation; BMI: Body mass index
The mean dose of metformin prescribed to control their blood glucose was 1450 ± 700 and 1200 ± 600 mg/day in treatment and placebo groups, respectively. These values were 16 ± 6.5 and 14.5 ± 8.5 mg/dl, respectively for glybenclamide.
At the beginning of the study, there was no significant difference in the variables between placebo and control group. As shown in table 2, there was a significant reduction in total cholesterol, LDL-cholesterol and TG level in both treatment and placebo groups (P < 0.05). Serum HDL-cholesterol level decreased significantly in the placebo group (P < 0.05); while it remained unchanged in the treatment group. We also measured MDA as oxidative stress marker. It decreased in both groups significantly (P < 0.05). However, the P values related to the between group’s comparisons were not significant for any variables. Furthermore, time-treatment interactions were not statistically significant for any variables.
Table 2.
Between group and within group comparison of lipid profile and oxidative stress marker in diabetic patients*
| Variable | Placebo |
Treatment |
Placebo versus treatment | Time-treatment interaction | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (1) | 6 weeks (2) | 12 weeks (3) | P§ | Pair wise comparisons** | Baseline (1) | 6 weeks (2) | 12 weeks (3) | P§ | Pair wise comparisons** | p¥ | p€ | |
| FBS (mg/dl) | 141.8 ± 48.5 | 153.7 ± 57.2 | 157.7 ± 60.8 | 0.038 | 1,3 (P = 0.03) | 145.6 ± 52.1 | 148.1 ± 52.0 | 143.8 ± 51.8 | 0.712 | 0.66 | 0.12 | |
| Total cholesterol (mg/dl) | 199.7 ± 46.2 | 182.7 ± 44.7 | 158.2 ± 40.8 | <0.001 | 1,2; 1,3; 2,3 (P < 0.001) | 195.7 ± 36.0 | 170.8 ± 34.1 | 150.2 ± 37.9 | <0.001 | 1,2; 1,3 (P < 0.001) | 0.36 | 0.55 |
| 2,3 (P = 0.002) | ||||||||||||
| LDL-C (mg/dl) | 123.7 ± 41.9 | 109.1 ± 33.8 | 97.0 ± 33.8 | <0.001 | 1,2 (P = 0.010) | 120.8 ± 34.6 | 98.5 ± 27.7 | 89.7 ± 28.6 | <0.001 | 1,2 (P = 0.001) | 0.31 | 0.57 |
| 1,3 (P < 0.001) | 1,3 (P < 0.001) | |||||||||||
| HDL-C (mg/dl) | 35.6 ± 9.6 | 37.0 ± 11.2 | 33.0 ± 8.3 | 0.040 | 2,3 (P = 0.04) | 39.2 ± 12.5 | 38.0 ± 13.9 | 35.4 ± 10.7 | 0.100 | 0.30 | 0.58 | |
| TG (mg/dl) | 201.6 ± 116.2 | 190.4 ± 124.7 | 140.7 ± 102.9 | <0.001 | 1,3 (P < 0.001) | 178.0 ± 83.1 | 147.8 ± 67.3 | 124.8 ± 73.3 | <0.001 | 1,2 (P = 0.02) | 0.19 | 0.29 |
| 2,3 (P = 0.002) | 1,3 (P < 0.001) | |||||||||||
| MDA (μmol/l) | 4.2 ± 0.8 | 3.70 ± 0.8 | 3.5 ± 0.7 | 0.001 | 1,2 (P = 0.01) | 4.17 ± 0.7 | 3.68 ± 0.7 | 3.52 ± 0.7 | <0.001 | 1,2 (P < 0.001) | 0.93 | 0.89 |
| 1,3 (P < 0.001) | 1,3 (P < 0.001) | |||||||||||
General linear model repeated measures analysis;
Within groups;
Adjustment for multiple comparisons: Bonferroni;
Between groups;
Time-treatment interaction
FBS: Fasting blood sugar; LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TG: Triglyceride; MDA: Malondialdehyde
Table 3 shows the mean difference of variables between the beginning and end of the study. Although the reduction in total cholesterol and LDL was more pronounced in the treatment group, it was not statistically significant.
Table 3.
Comparison of the mean difference of variables at the beginning and end of the study (end-beginning) between the two groups
| Variable | Placebo | Treatment | P* |
|---|---|---|---|
| Total cholesterol (mg/dl) | −41.5 ± 5.90** | −45.5 ± 5.60 | 0.635 |
| LDL-C (mg/dl) | −26.7 ± 5.50 | −31.0 ± 4.40 | 0.544 |
| HDL-C (mg/dl) | −2.6 ± 1.40 | −3.8 ± 1.80 | 0.610 |
| TG (mg/dl) | −60.9 ± 12.40 | −53.2 ± 1107.00 | 0.657 |
| MDA (μmol/l) | −0.7 ± 0.10 | −0.6 ± 0.09 | 0.784 |
Independent t-test;
Mean ± standard error;
LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TG: Triglyceride; MDA: Malondialdehyde
Discussion
The present study showed that active vitamin D reduced lipid profile and oxidative stress markers in diabetic patients compared to the control group, but these alterations were not statistically significant.
Several studies demonstrated that 25(OH)D levels were inversely correlated with total cholesterol, LDL, TG, and low HLD level.8,16 Multiple interventional studies have investigated the effect of vitamin D supplementation on lipids and have produced conflicting results. An early small study evaluating the effect of short-term calcium (1000 mg daily) and vitamin D (800 IU daily) supplementation in healthy postmenopausal women showed no change in the levels of lipid parameters.18 Motiwala and Wang18 and Zittermann et al.24 randomized overweight participants to vitamin D supplementation versus placebo over 12 months and found a significant decrease in TGs, but not LDL level. Jorde and Figenschau25 found in their study that high dose vitamin D supplementation in diabetic patients did not have any effect on the lipid profile. Major et al.26 showed that in overweight or obese women with low calcium intakes, supplementation with calcium and vitamin D improved blood lipid and lipoprotein during a weight-loss intervention. In a study by Bonakdaran et al.,27 supplementation with 0.5 µg calcitriol versus placebo for 8 weeks in chronic renal failure patients on hemodialysis lowered the serum TG and total-cholesterol. Ultraviolet (UV) radiation for 12 months did not have any effect on the serum lipids, but in a subgroup of subjects with vitamin D insufficiency (25(OH)D < 30 ng/ml), UV radiation increased apo-AI and decreased apo-AII level.28
Several mechanisms are recommended for the impact of vitamin D on the serum lipids. In theory, vitamin D could affect the serum lipid levels directly, but also indirectly through its effect on serum parathyroid hormone (PTH) and/or on the calcium balance.10
Two mechanisms might be involved in vitamin D mediated reduction in serum TGs: (1) vitamin D increases intestinal calcium absorption. This calcium could then reduce the serum TGs by reducing hepatic TG formation and secretion; (2) via a suppressive effect of vitamin D on serum PTH concentrations. A reduction in serum PTH may reduce the serum TGs via increased peripheral removal.
Free radical production is up-regulated in hyperglycemia.29,30 Increased free radicals in oxidative stress cause DNA, lipid, carbohydrate and protein oxidation and hence tissue damage.31 There are limited data on antioxidant properties of vitamin D. It is shown in some studies that vitamin D acts as a membrane antioxidant.19 Antioxidant properties of vitamin D was proved in two animal studies,32,33 and it has been estimated to be even stronger than vitamin E and melatonin.20 Vitamin D supplementation in vitamin D deficient subjects decreased the level of the serum thiobarbituric acid reactive substances (TBARS) significantly.20 In our study, active vitamin D did not reduce serum TBATS significantly.
We saw a significant decrease in total cholesterol, LDL, and TG level in the placebo group. These changes could have two reasons. First, it can be related to the “regression to the mean” phenomenon. In statistics, regression toward the mean (also known as regression to the mean) is the phenomenon in which if a variable is extreme on its first measurement, it will tend to be closer to the average on a second measurement, and a fact that may superficially seem paradoxical-if it is extreme on a second measurement, it will tend to be closer to the average on the first measurement.34,35 To avoid making wrong inferences, the possibility of regression toward the mean must be considered when designing experiments and interpreting experimental, survey, and other empirical data in the physical, life, behavioral, and social sciences.34,35 Second, it can be attributed to the placebo effect and behavior modification in the placebo group during this follow-up.
Future studies on vitamin D deficient subjects, and within the subgroups of vitamin D receptor polymorphisms are worth to be done. The strength of our study included its randomized, placebo controlled design and a drawback to our study is that we assessed only one marker to evaluate oxidative stress.
Conclusion
Active vitamin D reduced lipid profile and oxidative stress markers in diabetic patients compared to the control group, but these alterations were not statistically significant.
Acknowledgments
This study was funded by the Grant Number 88-4617 from Shiraz University of Medical Sciences. We gratefully thank all 70 diabetic patients for their good cooperation.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Zittermann A, Gummert JF. Sun, vitamin D, and cardiovascular disease. J Photochem Photobiol B. 2010;101(2):124–9. doi: 10.1016/j.jphotobiol.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol . 2012;60(14):1207–16. doi: 10.1016/j.jacc.2012.03.074. [DOI] [PubMed] [Google Scholar]
- 3.Stocker R, Keaney JF. Role of oxidative modifications in atherosclerosis. Physiol Rev. 2004;84(4):1381–478. doi: 10.1152/physrev.00047.2003. [DOI] [PubMed] [Google Scholar]
- 4.Franz MJ. Medical Nutrition Therapy for Diabetes Mellitus and hypoglycemia of Nondiabetic Origin. In: Mahan LK, Escott-Stump S, Raymond JL, editors. Krause's Food & the Nutrition Care Process. Philadelphia, PA: Elsevier Health Sciences; 2012. pp. 675–706. [Google Scholar]
- 5.Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615–25. doi: 10.2337/diabetes.54.6.1615. [DOI] [PubMed] [Google Scholar]
- 6.Peterson CA, Heffernan ME. Serum tumor necrosis factor-alpha concentrations are negatively correlated with serum 25(OH)D concentrations in healthy women. J Inflamm (Lond) 2008;5:10. doi: 10.1186/1476-9255-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beilfuss J, Berg V, Sneve M, Jorde R, Kamycheva E. Effects of a 1-year supplementation with cholecalciferol on interleukin-6, tumor necrosis factor-alpha and insulin resistance in overweight and obese subjects. Cytokine. 2012;60(3):870–4. doi: 10.1016/j.cyto.2012.07.032. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez-Rodriguez E, Ortega RM, Gonzalez-Rodriguez LG, Lopez-Sobaler AM. Vitamin D deficiency is an independent predictor of elevated triglycerides in Spanish school children. Eur J Nutr. 2011;50(5):373–8. doi: 10.1007/s00394-010-0145-4. [DOI] [PubMed] [Google Scholar]
- 9.Kendrick J, Targher G, Smits G, Chonchol M. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis. 2009;205(1):255–60. doi: 10.1016/j.atherosclerosis.2008.10.033. [DOI] [PubMed] [Google Scholar]
- 10.Jorde R, Grimnes G. Vitamin D and metabolic health with special reference to the effect of vitamin D on serum lipids. Prog Lipid Res. 2011;50(4):303–12. doi: 10.1016/j.plipres.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Parker J, Hashmi O, Dutton D, Mavrodaris A, Stranges S, Kandala NB, et al. Levels of vitamin D and cardiometabolic disorders: systematic review and meta-analysis. Maturitas. 2010;65(3):225–36. doi: 10.1016/j.maturitas.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Martini LA, Wood RJ. Vitamin D and blood pressure connection: update on epidemiologic, clinical, and mechanistic evidence. Nutr Rev. 2008;66(5):291–7. doi: 10.1111/j.1753-4887.2008.00035.x. [DOI] [PubMed] [Google Scholar]
- 13.Judd SE, Tangpricha V. Vitamin D deficiency and risk for cardiovascular disease. Am J Med Sci. 2009;338(1):40–4. doi: 10.1097/MAJ.0b013e3181aaee91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe EL, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham Heart Study. Diabetes. 2010;59(1):242–8. doi: 10.2337/db09-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanham-New S, Lee P, Wong M, Sui C, Starkey S, Lovell D, et al. Association between dietary vitamin D intake and serum lipid profiles in Asian and Caucasian UK women: preliminary results from the Vitamin D, Food Intake, Nutrition and Exposure to Sunlight in Southern England (D-FINES) Study. Proc Nutr Soc. 2008;67:E320. [Google Scholar]
- 16.John WG, Noonan K, Mannan N, Boucher BJ. Hypovitaminosis D is associated with reductions in serum apolipoprotein A-I but not with fasting lipids in British Bangladeshis. Am J Clin Nutr. 2005;82(3):517–22. doi: 10.1093/ajcn.82.3.517. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Zalewski A, Liu Y, Mazurek T, Cowan S, Martin JL, et al. Diabetes-induced oxidative stress and low-grade inflammation in porcine coronary arteries. Circulation. 2003;108(4):472–8. doi: 10.1161/01.CIR.0000080378.96063.23. [DOI] [PubMed] [Google Scholar]
- 18.Motiwala SR, Wang TJ. Vitamin D and cardiovascular risk. Curr Hypertens Rep. 2012;14(3):209–18. doi: 10.1007/s11906-012-0262-y. [DOI] [PubMed] [Google Scholar]
- 19.Bao BY, Ting HJ, Hsu JW, Lee YF. Protective role of 1 alpha, 25-dihydroxyvitamin D3 against oxidative stress in nonmalignant human prostate epithelial cells. Int J Cancer. 2008;122(12):2699–706. doi: 10.1002/ijc.23460. [DOI] [PubMed] [Google Scholar]
- 20.Tarcin O, Yavuz DG, Ozben B, Telli A, Ogunc AV, Yuksel M, et al. Effect of vitamin D deficiency and replacement on endothelial function in asymptomatic subjects. J Clin Endocrinol Metab. 2009;94(10):4023–30. doi: 10.1210/jc.2008-1212. [DOI] [PubMed] [Google Scholar]
- 21.Eftekhari MH, Akbarzadeh M, Dabbaghmanesh MH, Hasanzadeh J. Impact of treatment with oral calcitriol on glucose indices in type 2 diabetes mellitus patients. Asia Pac J Clin Nutr. 2011;20(4):521–6. [PubMed] [Google Scholar]
- 22.Warnick GR, Knopp RH, Fitzpatrick V, Branson L. Estimating low-density lipoprotein cholesterol by the Friedewald equation is adequate for classifying patients on the basis of nationally recommended cutpoints. Clin Chem. 1990;36(1):15–9. [PubMed] [Google Scholar]
- 23.Zal F, Mostafavi-Pour Z, Vessal M. Comparison of the effects of vitamin E and/or quercetin in attenuating chronic cyclosporine A-induced nephrotoxicity in male rats. Clin Exp Pharmacol Physiol. 2007;34(8):720–4. doi: 10.1111/j.1440-1681.2007.04623.x. [DOI] [PubMed] [Google Scholar]
- 24.Zittermann A, Frisch S, Berthold HK, Gotting C, Kuhn J, Kleesiek K, et al. Vitamin D supplementation enhances the beneficial effects of weight loss on cardiovascular disease risk markers. Am J Clin Nutr. 2009;89(5):1321–7. doi: 10.3945/ajcn.2008.27004. [DOI] [PubMed] [Google Scholar]
- 25.Jorde R, Figenschau Y. Supplementation with cholecalciferol does not improve glycaemic control in diabetic subjects with normal serum 25-hydroxyvitamin D levels. Eur J Nutr. 2009;48(6):349–54. doi: 10.1007/s00394-009-0020-3. [DOI] [PubMed] [Google Scholar]
- 26.Major GC, Alarie F, Dore J, Phouttama S, Tremblay A. Supplementation with calcium + vitamin D enhances the beneficial effect of weight loss on plasma lipid and lipoprotein concentrations. Am J Clin Nutr. 2007;85(1):54–9. doi: 10.1093/ajcn/85.1.54. [DOI] [PubMed] [Google Scholar]
- 27.Bonakdaran S, Ayatollahi H, Mojahedi MJ, Sharifipoor F, Shakeri M. Impact of treatment with oral calcitriol on glucose intolerance and dyslipidemia(s) in hemodialysis patients. Saudi J Kidney Dis Transpl. 2008;19(6):942–7. [PubMed] [Google Scholar]
- 28.Carbone LD, Rosenberg EW, Tolley EA, Holick MF, Hughes TA, Watsky MA, et al. 25-Hydroxyvitamin D, cholesterol, and ultraviolet irradiation. Metabolism. 2008;57(6):741–8. doi: 10.1016/j.metabol.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Cetinkalp S, Delen Y, Karadeniz M, Yuce G, Yilmaz C. The effect of 1alpha,25(OH)2D3 vitamin over oxidative stress and biochemical parameters in rats where Type 1 diabetes is formed by streptozotocin. J Diabetes Complications. 2009;23(6):401–8. doi: 10.1016/j.jdiacomp.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 30.Noyan T, Balaharoglu R, Komuroglu U. The oxidant and antioxidant effects of 25-hydroxyvitamin D3 in liver, kidney and heart tissues of diabetic rats. Clin Exp Med. 2005;5(1):31–6. doi: 10.1007/s10238-005-0061-8. [DOI] [PubMed] [Google Scholar]
- 31.Kumaraguruparan R, Subapriya R, Kabalimoorthy J, Nagini S. Antioxidant profile in the circulation of patients with fibroadenoma and adenocarcinoma of the breast. Clin Biochem. 2002;35(4):275–9. doi: 10.1016/s0009-9120(02)00310-7. [DOI] [PubMed] [Google Scholar]
- 32.Kuzmenko AI, Morozova RP, Nikolenko IA, Korniets GV, Kholodova Y. Effects of vitamin D3 and ecdysterone on free-radical lipid peroxidation. Biochemistry (Mosc) 1997;62(6):609–12. [PubMed] [Google Scholar]
- 33.Sardar S, Chakraborty A, Chatterjee M. Comparative effectiveness of vitamin D3 and dietary vitamin E on peroxidation of lipids and enzymes of the hepatic antioxidant system in Sprague--Dawley rats. Int J Vitam Nutr Res. 1996;66(1):39–45. [PubMed] [Google Scholar]
- 34.Everitt BS. The Cambridge Dictionary of Statistics. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- 35.Upton GJ, Cook IG, Cook IT. Oxford Dictionary of Statistics. Oxford, UK: Oxford University Press, Incorporated; 2006. [Google Scholar]