Abstract
Background
Increasing age is associated with poor outcome after stroke. The Safety and Efficacy of NeuroFlo Technology in Ischemic Stroke (SENTIS) trial explored the augmentation of collateral circulation to the ischemic penumbra as a novel approach to stroke treatment. The aim of this post hoc analysis was to examine the effect of age on outcomes in the SENTIS trial.
Methods
Using data from the randomized controlled SENTIS trial, we explored outcomes of cerebral blood flow augmentation using the NeuroFlo TM device in patients categorized by age strata at 70 and 80 years. We evaluated outcomes of overall serious adverse event (SAE) and intracerebral hemorrhage (ICH) rates, freedom from all-cause and stroke-related mortality, and independent functional outcome as defined by the modified Rankin Scale score (mRS ≤ 2).
Results
The SENTIS as-treated cohort included 251 patients ≥ 70 years and 107 patients ≥ 80 years. Elderly SENTIS patients included a higher percentage of women and Caucasians than the younger group. Patients in the older group more frequently had vascular risk factors including hypertension, previous stroke, transient ischemic attacks and atrial fibrillation. However, baseline risk-factor profile, stroke severity, and time to randomization did not differ between the treated and nontreated elderly patients. The older patients treated with NeuroFlo had significantly higher chances for survival and for obtaining an independent functional state (mRS ≥ 2) compared with those who were not treated. Rates of SAEs and ICHs did not differ between the treatment groups.
Conclusions
NeuroFlo treatment is safe and results in better outcomes for elderly patients. This may be the result of recruitment and support of already existing collateral systems in these patients.
Keywords: Brain perfusion augmentation, Clinical trials, Elderly, Ischemic stroke, SENTIS
Introduction
Partial temporary occlusion of the abdominal aorta results in a prompt increase in blood volume above the occlusion and has been shown in animal experiments to specifically and persistently increase cerebral blood flow (CBF) even after the occlusion is removed [1] . The NeuroFlo TM catheter (CoAxia, Inc., Maple Grove, Minn., USA) is a novel device with dual balloons that are used to obstruct the abdominal aorta above and below the origin of the renal arteries during a 45-min procedure. Neuro-Flo has been previously studied in patients with symptomatic vasospasm after subarachnoid hemorrhage [2] , in a small number of patients with an acute ischemic stroke treated with tissue plasminogen activator [3] , and in patients with MRI mismatch who were treated up to 24 h following stroke onset [4] . The Safety and Efficacy of NeuroFlo Technology in Ischemic Stroke (SENTIS) trial was a prospective, randomized, multicenter trial that evaluated the safety and efficacy of CBF augmentation in patients with acute ischemic stroke randomized within 14 h of symptom onset [5] . It is likely that CBF augmentation opens existing collaterals in the brain, leading to an increase in penumbral perfusion that ultimately minimizes infarct growth [6] .
Increasing age has been found to be a marker for poor outcome following stroke [7, 8] . Older age has also been associated with increased risk of bleeding following thrombolysis in acute stroke patients [7, 8] . These findings resulted in the exclusion of elderly patients from many stroke studies as well as from treatment with thrombolytic drugs in clinical practice [8] . In this article, we report the post hoc findings of the effects of age on outcomes in the SENTIS trial.
Methods
The SENTIS trial methods and primary results have been previously reported [5]. In brief, the trial enrolled patients who were 18 years and older, presented with acute cerebral ischemia with hemispheric cortical dysfunction, had a presenting NIHSS score ≥ 5 and ≤ 18, and could be randomized within 14 h of symptom onset. In the current analysis of the SENTIS data we focused on the effect of age on patient outcomes. The SENTIS trial was registered on www.ClinicalTrials.gov (NCT 00119717).
Patient Population
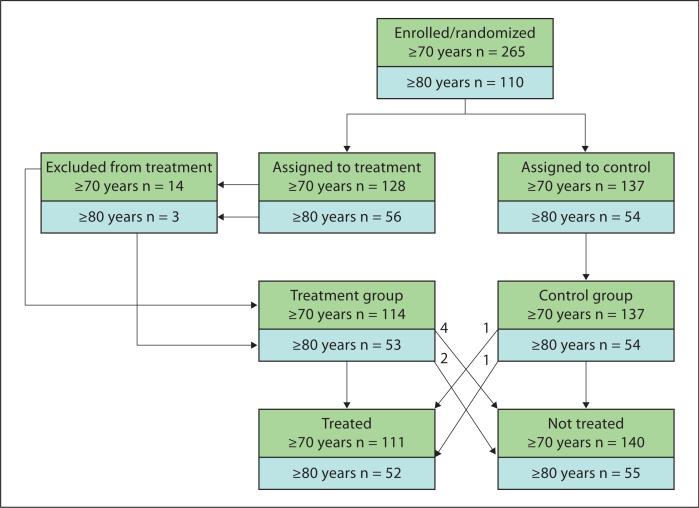
A total of 515 patients were enrolled in the SENTIS trial. Of these, 28 patients were excluded due to prespecified anatomical exclusions to NeuroFlo insertion and treatment, 5 patients assigned to the treatment arm did not receive NeuroFlo treatment, and 1 patient assigned to the control arm received NeuroFlo treatment (protocol deviations). This resulted in a modified-as-treated population comprised of 487 patients (226 treated and 261 not treated). There were 251 enrolled patients ≥ 70 years (111 treated and 140 not treated) of which 246 (108 treated and 138 not treated) had evaluable data at 90-day follow-up. Moreover, there were 107 enrolled patients ≥ 80 years (52 treated and 55 not treated) of which 102 (40 treated and 53 not treated) had evaluable data at 90-day follow-up. Safety outcomes were based on all enrolled patients; efficacy outcomes were based on all patients with 90-day (or 30-day carried forward) evaluable data. Figure 1 shows the randomization and treatment cohorts for the SENTIS patients in both age groups.
Fig. 1.
Randomization of SENTIS patients by age strata (≥ 70 years and ≥ 80 years).
Outcome Measures
Safety outcomes evaluated included the incidence of serious adverse events (SAEs) from the time of enrollment through 90-day follow-up (including intracranial hemorrhage), freedom from all-cause mortality, and freedom from stroke-related mortality. An independent Data and Safety Monitoring Board adjudicated all adverse events.
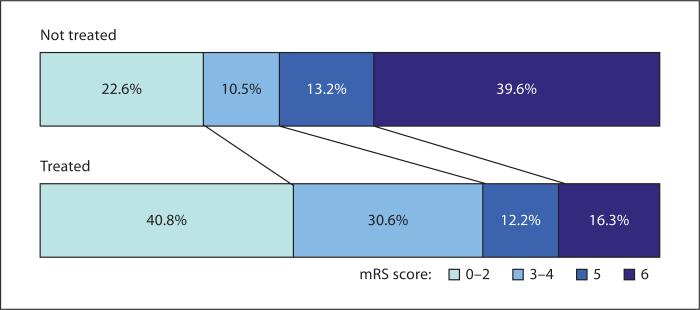
The efficacy outcome evaluated in the current analysis was the percent of patients achieving an independent functional outcome defined as a modified Rankin score (mRS) ≤2 at 90-day follow-up [9] . The 90-day mRS assessments were conducted by certified assessors blinded to the patients’ treatment allocations. We also examined mRS outcomes using a tetrachotomized shift analysis (mRS 0–2, 3–4, 5, 6) to assess good outcomes, fair-to-moderate outcomes, severe disability, and mortality between the treated and nontreated groups in the ≥ 80-year-old cohort.
Statistical Analyses
All analyses presented were based on the modified-as-treated population [5] . The age categories were based on the age of 80 having been the age by which the Cochran-Mantel-Haenszel test was stratified in the primary trial analysis and 70 being the median age of the SENTIS trial population.
For continuous variables, summary statistics included means, standard deviations and medians. Categorical variables were summarized using counts and percentages. Statistical comparisons between groups in baseline demographics were made using 2-sample Wilcoxon tests (continuous variables) and Fisher's exact tests (categorical variables). Kaplan-Meier curves for freedom from all-cause mortality were created for treated and nontreated patients based on the 80-year stratum. The outcomes of mRS ≥ 2, all-cause mortality, and stroke-related mortality were analyzed using logistic regression and were adjusted by treatment group, age, and baseline stroke severity (NIHSS score). Models were fit within each age strata. Odds ratios (OR) of survival are reported for all-cause and stroke-related mortality.
A Cochran-Mantel-Haenszel test of proportions stratified by stroke severity was used to compare the proportions of patients experiencing SAEs and intracerebral hemorrhage (ICH) in the treated versus nontreated groups within age strata. Adjusted OR, 95% CI, and p values were obtained from these statistical models.
Two-sided statistical tests were used and no adjustments for multiple comparisons were made. Statistical analyses were conducted in SAS version 9.1 or higher (SAS Institute).
Results
Demographics and Baseline Characteristics
The baseline characteristics of the entire SENTIS cohort were presented previously [5]. In this analysis, we focused on the effects of age on outcome. We first com pared baseline variables between the entire cohort of patients who were < 70 and those ≥ 70 years and between patients < 80 and those ≤ 80 years (treated and not treated). The results (table 1) show that in both age strata the percentage of women and Caucasians was higher among the elderly patients. They also suffered more frequently from comorbidities including hypertension, prior stroke, transient ischemic attacks, and atrial fibrillation, but were less frequently smokers. Although the initial stroke severity did not differ between age groups, the elderly patients were randomized somewhat earlier from symptom onset. Other variables including the frequencies of diabetes, peripheral vascular disease, stable ischemic heart disease, the affected hemisphere, and admission glucose levels did not differ between the groups.
Table 1.
Baseline characteristics of patients in the SENTIS cohort segregated by age
| Characteristic | Age <70 (n = 236) | Age ≥70 (n = 251) | p value | Age <80 (n = 380) | Age ≥80 (n = 107) | p value |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, years | ||||||
| Mean ± SD | 55.9 ± 10.2 | 79.1 ± 5.6 | <0.001 | 63.2 ± 12.5 | 84.4 ± 3.6 | <0.001 |
| Median | 58.3 | 78.8 | 65.3 | 83.4 | ||
| Gender, male | 59.3 (140) | 46.6 (117) | 0.006 | 56.1 (213) | 41.1 (44) | 0.008 |
| Race/ethnicity, white | 77.1 (182) | 90.8 (228) | <0.001 | 81.1 (308) | 95.3 (102) | <0.001 |
| Medical history | ||||||
| Diabetes mellitus | 33.5 (79) | 36.7 (92) | 0.506 | 35.3 (134) | 34.6 (37) | 1.000 |
| Hypertension | 72.9 (172) | 88.8 (223) | <0.001 | 78.7 (299) | 89.7 (96) | 0.011 |
| Hyperlipidemia | 43.6 (103) | 57.8 (145) | 0.002 | 48.9 (186) | 57.9 (62) | 0.102 |
| Current smoker | 41.5 (98) | 9.6 (24) | <0.001 | 31.8 (121) | 0.9 (1) | <0.001 |
| Cerebral ischemic infarct | 11.4 (27) | 18.3 (46) | 0.042 | 12.6 (48) | 23.4 (25) | 0.009 |
| Transient ischemic attack | 7.2 (17) | 15.1 (38) | 0.006 | 9.2 (35) | 18.7 (20) | 0.009 |
| Seizure | 3.8 (9) | 2.4 (6) | 0.436 | 3.2 (12) | 2.8 (3) | 1.000 |
| Atrial fibrillation | 12.7 (30) | 45.0 (113) | <0.001 | 22.1 (84) | 55.1 (59) | <0.001 |
| Peripheral vascular disease | 6.4 (15) | 5.6 (14) | 0.849 | 6.3 (24) | 4.7 (5) | 0.648 |
| Percutaneous transluminal coronary angioplasty | 6.4 (15) | 10.0 (25) | 0.186 | 8.2 (31) | 8.4 (9) | 1.000 |
| Coronary artery bypass graft | 8.1 (19) | 10.4 (26) | 0.435 | 9.5 (36) | 8.4 (9) | 0.851 |
| Myocardial infarction | 9.7 (23) | 13.1 (33) | 0.258 | 10.0 (38) | 16.8 (18) | 0.059 |
| Angina | 6.8 (16) | 6.4 (16) | 0.857 | 6.8 (26) | 5.6 (6) | 0.826 |
| Stroke characteristics | ||||||
| Time from symptom onset to randomization, h | ||||||
| Mean ± SD | 8.4 ± 2.8 | 7.8 ± 2.9 | 0.027 | 8.2 ± 2.8 | 7.6 ± 3.0 | 0.030 |
| Median | 7.9 | 7.5 | 7.8 | 7.0 | ||
| Baseline NIHSS score | ||||||
| Mean ± SD | 10.6 ± 4.1 | 11.0 ± 4.5 | 0.521 | 10.7 ± 4.3 | 11.2 ± 4.4 | 0.291 |
| Median | 10.0 | 10.0 | 10.0 | 10.0 | ||
| Admission glucose level, mg/dl | ||||||
| Mean ± SD | 133.8 ± 53.0 | 132.5 ± 44.8 | 0.292 | 133.5 ± 51.0 | 132.0 ± 40.9 | 0.437 |
| Median | 118.0 | 122.0 | 119.0 | 120.0 | ||
| Side of infarct, left, % | 55.1 (124) | 52.0 (127) | 0.518 | 54.9 (201) | 48.5 (50) | 0.265 |
Continuous variables are presented as means ± SD, with medians; categorical variables are presented as percentages, with numbers in parentheses.
Next, we compared treated versus nontreated patients in the ≥ 70-year and ≥ 80-year age strata. The results (table 2) show that there were no significant differences in baseline variables between the two groups ≥ 70 years. The nontreated patients ≥ 80 years were more frequently Caucasian and more frequently had a history of transient ischemic attacks. They also had a tendency towards having more peripheral vascular disease and myocardial infarction; although the presence of these comorbidities did not reach statistical significance. Importantly, other parameters including baseline stroke severity, time from stroke onset to randomization, and other comorbidities did not differ significantly between the treated and non-treated elderly patients.
Table 2.
Baseline characteristics of treated and nontreated patients in the SENTIS cohort
| Characteristic | ≥70 years |
≥80 years |
||||
|---|---|---|---|---|---|---|
| treated (n = 111) | not treated (n = 140) | p value | treated (n = 52) | not treated (n = 55) | p value | |
| Demographics | ||||||
| Age, years | ||||||
| Mean 8 SD | 79.3 ± 5.5 | 79.0 ± 5.8 | 0.474 | 84.0 ± 3.2 | 84.8 ± 3.9 | 0.454 |
| Median | 79.5 | 78.3 | 83.3 | 83.5 | ||
| Gender, male | 45.9 (51) | 47.1 (66) | 0.899 | 36.5 (19) | 45.5 (25) | 0.432 |
| Race/ethnicity, white | 88.3 (98) | 92.9 (130) | 0.271 | 90.4 (47) | 100.0 (55) | 0.024 |
| Medical history | ||||||
| Diabetes mellitus | 35.1 (39) | 37.9 (53) | 0.694 | 30.8 (16) | 38.2 (21) | 0.542 |
| Hypertension | 86.5 (96) | 90.7 (127) | 0.318 | 86.5 (45) | 92.7 (51) | 0.351 |
| Hyperlipidemia | 63.1 (70) | 53.6 (75) | 0.157 | 57.7 (30) | 58.2 (32) | 1.000 |
| Current smoker | 9.0 (10) | 10.0 (14) | 0.832 | 0 (0) | 1.8 (1) | 1.000 |
| Cerebral ischemic infarct | 13.5 (15) | 22.1 (31) | 0.100 | 17.3 (9) | 29.1 (16) | 0.175 |
| Transient ischemic attack | 12.6 (14) | 17.1 (24) | 0.377 | 9.6 (5) | 27.3 (15) | 0.025 |
| Seizure | 2.7 (3) | 2.1 (3) | 1.000 | 5.8 (3) | 0 (0) | 0.111 |
| Atrial fibrillation | 43.2 (48) | 46.4 (65) | 0.702 | 53.8 (28) | 56.4 (31) | 0.847 |
| Peripheral vascular disease | 4.5 (5) | 6.4 (9) | 0.588 | 0 (0) | 9.1 (5) | 0.057 |
| Percutaneous transluminal coronary angioplasty | 11.7 (13) | 8.6 (12) | 0.525 | 7.7 (4) | 9.1 (5) | 1.000 |
| Coronary artery bypass graft | 13.5 (15) | 7.9 (11) | 0.151 | 11.5 (6) | 5.5 (3) | 0.311 |
| Myocardial infarction | 14.4 (16) | 12.1 (17) | 0.707 | 15.4 (8) | 18.2 (10) | 0.059 |
| Angina | 4.5 (5) | 7.9 (11) | 0.312 | 6.8 (26) | 5.6 (6) | 0.798 |
| Stroke characteristics | ||||||
| Time from symptom onset to randomization, h | ||||||
| Mean ± SD | 7.7 ± 2.9 | 7.9 ± 2.9 | 0.612 | 7.6 ± 3.0 | 7.5 ± 3.0 | 0.881 |
| Median | 7.5 | 7.4 | 7.2 | 7.0 | ||
| Baseline NIHSS score | ||||||
| Mean ± SD | 11.1 ± 4.2 | 10.8 ± 4.6 | 0.565 | 11.5 ± 4.3 | 10.9 ± 4.5 | 0.390 |
| Median | 11.0 | 9.5 | 12.5 | 9.0 | ||
| Admission glucose level, mg/dl | ||||||
| Mean ± SD | 137.9 ± 52.1 | 128.0 ± 38.1 | 0.295 | 132.6 ± 33.9 | 131.5 ± 46.7 | 0.364 |
| Median | 122.3 | 122.0 | 121.3 | 120.0 | ||
| Side of infarct, left, % | 51.4 (56) | 52.6 (71) | 0.898 | 47.1 (24) | 50.0 (26) | 0.844 |
Continuous variables are presented as means ± SD, with medians; categorical variables are presented as percentages, with numbers in parentheses.
Safety Outcomes
The results demonstrate that NeuroFlo treatment is safe. SAE rates did not differ between the treated and nontreated patients in either of the age strata (table 3). Although there was a higher rate of SAEs in the older age strata, the rates were not different from those seen in the nontreated patients of comparable age. Importantly for older patients, the rates of ICH were not different between the treated and nontreated patients in either age strata whether looking at symptomatic ICH [10] or ICH within 24 h or 90 days.
Table 3.
SAE and ICH rates in SENTIS patients by age
| Event | Treated % (n) | Not treated % (n) | pvalue1 |
|---|---|---|---|
| Age <70 | n = 115 | n = 121 | |
| SAE | 39.1 (45) | 35.5 (43) | 0.749 |
| All ICH | 23.5 (27) | 24.0 (29) | 0.832 |
| ICH within 24 h | 17.4 (20) | 14.9 (18) | 0.672 |
| Symptomatic ICH2 | 0.0 (0) | 0.8 (1) | 1.000 |
| Age ≥70 | n = 111 | n = 140 | |
| SAE | 49.5 (55) | 48.6 (68) | 0.878 |
| All ICH | 29.7 (33) | 30.0 (42) | 0.739 |
| ICH within 24 h | 22.5 (25) | 24.3 (34) | 0.903 |
| Symptomatic ICH2 | 2.7 (3) | 0.7 (1) | 0.324 |
| Age <80 | n = 174 | n = 206 | |
| SAE | 41.4 (72) | 37.4 (77) | 0.432 |
| All ICH | 28.7 (50) | 27.7 (57) | 0.900 |
| ICH within 24 h | 20.7 (36) | 20.4 (42) | 0.992 |
| Symptomatic ICH2 | 1.1 (2) | 1.0 (2) | 1.000 |
| Age ≥80 | n = 52 | n = 55 | |
| SAE | 53.8 (28) | 61.8 (34) | 0.174 |
| All ICH | 19.2 (10) | 25.5 (14) | 0.413 |
| ICH within 24 h | 17.3 (9) | 18.2 (10) | 0.936 |
| Symptomatic ICH2 | 1.9 (1) | 0.0 (0) | 0.486 |
The Cochran-Mantel-Haenszel test was stratified by stroke severity. For symptomatic ICH, Fisher's exact test was used in place of the Cochran-Mantel-Haenszel test due to the small number of events.
The definition from the SITS-MOST trial was used to define symptomatic ICH in the SENTIS trial.
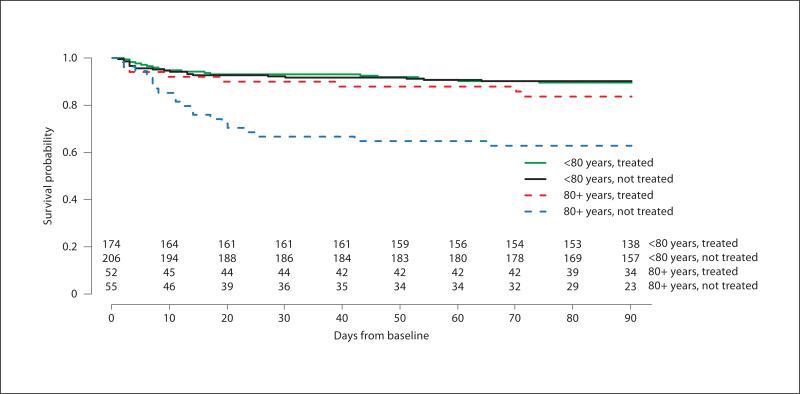
Multivariate logistic regression analysis for mortality showed that elderly treated patients had significantly lower all-cause mortality rates compared with elderly patients who were not treated [≥ 70 years: 15.3 vs. 24.3%, OR = 2.02 (1.01–4.05), p = 0.047; ≥ 80 years: 15.4 vs. 38.2%, OR = 5.35 (1.77–16.15), p = 0.003]. Furthermore, the stroke-related mortality rate was also significantly lower in the elderly treated patients compared to non-treated patients [≥ 70 years: 9.9 vs. 21.4%, OR = 3.10 (1.36–7.04), p = 0.007; ≥ 80 years: 11.5 vs. 32.7%, OR = 6.62 (1.92–22.79), p = 0.003]. Table 4 shows the causes of death in treated and nontreated patients in both groups (≥ 70 and ≥ 80 years). Figure 2 shows the Kaplan-Meier curves for freedom from all-cause mortality in the 80-year stratum (stratified by treatment group and age stratum).
Table 4.
Causes of death of treated and nontreated SENTIS patients
| Event type | ≥70 years, % (n) |
≥80 years, % (n) |
||
|---|---|---|---|---|
| treated (n = 111) | not treated (n = 140) | treated (n = 52) | not treated (n = 55) | |
| All deaths1 | 15.3 (17) | 24.3 (34) | 15.3 (8) | 38.2 (21) |
| Stroke-related deaths | 5.4 (6) | 13.5 (19) | 5.8 (3) | 20.0 (11) |
| Cerebral bleeding (HT, ICH) | 1.8 (2) | 3.6 (5) | 1.9 (1) | 3.6 (2) |
| Cerebral edema, neurological worsening, progression | 3.6 (4) | 8.6 (12) | 3.8 (2) | 14.5 (8) |
| New stroke | 0 (0) | 1.4 (2) | 0 (0) | 1.8 (1) |
| Other index stroke related events | 5.4 (6) | 10.0 (14) | 5.8 (3) | 14.5 (8) |
| Continuous epileptic activity | 0 (0) | 0.7 (1) | 0 (0) | 1.8 (1) |
| Cardiovascular | 0 (0) | 0.7 (1) | 0 (0) | 0 (0) |
| Sepsis, multiorgan failure | 0.9 (1) | 2.8 (4) | 0 (0) | 3.6 (2) |
| Respiratory dysfunction/failure, pneumonia | 4.5 (5) | 5.0 (7) | 5.8 (3) | 10.9 (6) |
| Unspecified | 0 (0) | 0.7 (1) | 0 (0) | 0 (0) |
| Deaths not stroke-related | 5.4 (6) | 2.8 (4) | 3.8 (2) | 5.4 (3) |
| Cancer | 2.7 (3) | 0.7 (1) | 1.9 (1) | 0 (0) |
| Cardiac tamponade | 0.9 (1) | 0 (0) | 1.9 (1) | 0 (0) |
| Respiratory failure, pneumonia | 0 (0) | 1.4 (2) | 0 (0) | 3.6 (2) |
| Diabetes | 0 (0) | 0.7 (1) | 0 (0) | 1.8 (1) |
| Cardiopulmonary collapse secondary to ruptured viscus and sepsis | 0.9 (1) | 0 (0) | 0 (0) | 0 (0) |
| Multiorgan failure | 0.9 (1) | 0 (0) | 0 (0) | 0 (0) |
HT = Hemorrhagic transformation.
A patient may have had more than 1 adverse event associated with the cause of death. All deaths were adjudicated by the Data and Safety Monitoring Board as stroke related or not stroke related based on the origin of the event and the timing of the event onset.
Fig. 2.
Kaplan-Meier curves for freedom from all-cause mortality in SENTIS patients by age.
Efficacy Outcome
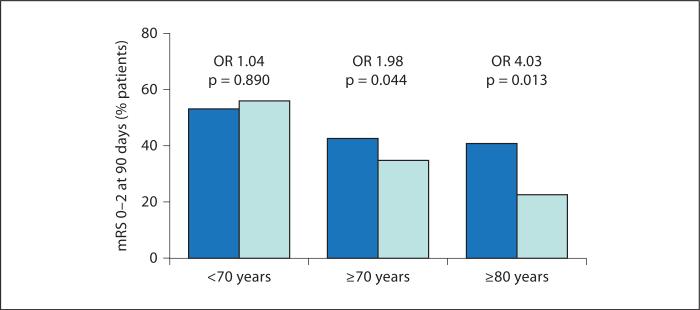
We then used a multivariate logistic regression model controlling for age and stroke severity to evaluate functional outcomes. As shown in table 5 , the treated patients ≥ 70 years had an OR of 1.98 (95% CI = 1.02, 3.87) for good outcome (mRS 0–2) compared with the nontreated patients in the same age strata. The treated patients ≥ 80 years had even greater treatment benefit with an OR of 4.03 (95% CI = 1.35, 12.09) compared with the nontreated patients in the same age strata. A good outcome (mRS ≤ 2) at 90 days was 2–4 times more likely in the elderly treated patients compared with the elderly nontreated patients. Figure 3 shows that elderly patients are less likely to attain independent functional outcomes (mRS 0–2), but NeuroFlo treatment can mitigate poorer outcomes. The frequency of moderate-to-poor outcome (mRS 3–5) was comparable between the groups (fig. 4).
Table 5.
Logistic regression analysis for obtaining good outcome (mRS 0-2) in the SENTIS trial by age
| Age subgroup | OR (95% CI)1 | p value | Interaction model p value2 |
|---|---|---|---|
| <70 years | 1.04 (0.57, 1.92) | 0.890 | 0.198 |
| ≥70 years | 1.98 (1.02, 3.87) | 0.044 | |
| <80 years | 1.08 (0.66, 1.78) | 0.750 | 0.029 |
| ≥80 years | 4.03 (1.35, 12.09) | 0.01 | |
OR are for treated vs. not treated within the age subgroup; models are adjusted by stroke severity.
Interaction p value is for treatment by age subgroup, adjusted by stroke severity.
Fig. 3.
Rates of independent functional outcome (mRS 0–2) at 90 days by age strata. The dark blue (dark gray in the printed version) column represents the treated group and the light blue (light gray in the printed version) column represents the nontreated group. Although there is no difference in independent functional outcome in the < 70-year age stratum, the difference reaches statistical significance for the ≥ 70-year age stratum and is even more substantial at the ≥ 80-year age stratum.
Fig. 4.
mRS shift analysis – 90-day outcomes in SENTIS patients ≥ 80 years. Values for the shift analysis are based on the number of patients with evaluable data at 90 days.
Discussion
Because the average age of populations in Western civilizations is constantly increasing, it is estimated that many more octogenarians and nonagenarians will suffer from stroke in the ensuing years [11]. Yet, despite having evident benefits from therapy, these patients are frequently excluded from the intravenous [7, 8] or endovascular reperfusion treatments [12, 13] that are the mainstay of current stroke therapy because of higher risks for complications [14, 15] . Many of these patients are left untreated and have a high risk for mortality or significant residual disability. Therefore, novel therapeutic options for these patients are desperately needed.
The findings of the current analysis suggest that the strategy of CBF augmentation with the NeuroFlo device may be especially effective in elderly patients. Similar to prevalent data on stroke-related comorbidities, we found an increased rate of major comorbidities among our elderly patients. Therefore, one could have expected outcomes to be less favorable in the elderly patients in our trial as well. However, in contrast to previous studies exploring outcome following systemic thrombolysis [8, 15] or endovascular vessel recanalization techniques [12, 13] , our results specifically show that elderly patients have better chances for survival and for obtaining functional independence after severe stroke when treated with NeuroFlo.
There are a number of potential explanations for our findings. In brief, few data are available on the association of age with collaterals in the brain. It has been hypothesized that there is a higher level of collateral failure with advancing age; hence, the relative benefit gained from augmentation may be greater in the elderly than in younger patients. Another possibility is that older patients who have survived beyond 70 years of age may have developed more robust collaterals than those who died at earlier time points. This survival effect may result in the selection of elderly patients with preferentially more robust collaterals. Once these anastomotic collateral routes have been developed, it remains quite logical that collateral augmentation with NeuroFlo may confer greater benefit. In other words, the substrate for collateral therapeutics may be superior in the elderly population who present with stroke. Alternatively, collaterals may require higher perfusion pressures to become patent in elderly individuals and, therefore, may become available only after CBF augmentation. As is the case with patients with chronic ischemic heart disease, stroke patients tend to form collaterals over the years, potentially resulting in better outcomes [16] . Nevertheless, without CBF augmentation that takes advantage of the presence of these collaterals, these patients generally do poorly due to the presence of comorbidities [8, 15] such as heart failure that may prevent the opening of these collateral channels.
The data demonstrate that CBF augmentation using NeuroFlo is safe in elderly patients. Reassuringly, despite an expected increase in complication rates typically observed in these patients [15] , there was no difference in overall SAE rates or in the rates of symptomatic or symptomatic intracranial hemorrhages between treated and nontreated patients even when treatment was given as late as 14 h after stroke onset. Importantly, these safety results suggest that NeuroFlo treatment can be applied in elderly patients even late after stroke onset, thereby potentially increasing the number of stroke patients that could be offered a potential treatment for the reduction of chronic disability.
The strength of our findings is that they are the result of a blinded, randomized trial with a large sample size. Limitations of the current analysis include: (1) the post hoc nature of the analysis; (2) possible type-I error inflation due to multiple comparisons; (3) the SENTIS trial was not originally powered to assess the effects of age on outcome, and (4) the collateral mechanism cannot be confirmed by this analysis. Furthermore, this analysis is based on the as-treated population, not the intent-to-treat population; however, supporting analyses demonstrated similar results between outcomes in the as-treated and intent-to-treat populations. Finally, we cannot rule out the possibility that differences in the populations other than age may have contributed to differences in outcome. For example, the nontreated patients who were older than 80 were more likely to have a history of transient ischemic attacks and tended toward higher rates of vascular disorders that may have contributed to their poorer outcomes.
In conclusion, our findings suggest that CBF augmentation with the NeuroFlo intra-aortic device is safe and may be especially beneficial in elderly patients with stroke. NeuroFlo may represent a viable treatment option for patients who are at increased risk for complications with conventional stroke therapies and, therefore, are otherwise left without specific treatment.
Acknowledgments
The authors would like to thank Lisa M. Thackeray, MS, of The Integra Group for statistical support, and Kay Zander, MA, and Ellen O'Malley, MS, of CoAxia, Inc. for their valuable input, review and editing of the manuscript.
Footnotes
Disclosure Statement
The SENTIS trial was funded by CoAxia, Inc. All authors who participated as investigators for the SENTIS Trial and their institutions received study payments based on the number of patients enrolled in the trial. The following authors indicated no additional disclosures: R.L., C.M., K.C., M.C., P.P.D. and W.S.B. D.S.L. serves as a consultant to Concentric Medical, CoAxia, and Reverse Medical and was also supported by grants NIH/NINDS K23NS054084, P50NS044378 and K24NS072272. A.S. received honorarium and consulting fees from CoAxia for consulting and clinical trials design. R.G. serves as a Consultant/Scientific Advisory Board member for CoAxia, Concentric Medical, and Rapid Medical, and on the Data and Safety Monitoring Board for Reverse Medical and Rapid Medical. W.D. received funding from CoAxia for the imaging core laboratory and has received honorarium for consulting with CoAxia. H.-C.D. received honoraria for participation in clinical trials, contribution to advisory boards or oral presentations from the following: Abbott, Allergan, Astra-Zeneca, Bayer Vital, BMS, Boehringer Ingelheim, CoAxia, Corimmun, Covidien, Daichii-Sankyo, D-Pharm, EV3, Fresenius, GlaxoSmithKline, Janssen Cilag, Knoll, MSD, Medtronic, Mind-Frame, Neurobiological Technologies, Novartis, Novo-Nordisk, Paion, Parke-Davis, Pfizer, Sanofi-Aventis, Schering-Plough, Ser-vier, Solvay, Thrombogenics, Wyeth and Yamanouchi. Financial support for research projects was provided by Astra/Zeneca, GSK, Boehringer Ingelheim, Lundbeck, Novartis, Janssen-Cilag, Sanofi-Aventis, Syngis and Talecris. The Department of Neurology at the University Duisburg-Essen received research grants from the German Research Council (DFG), German Ministry of Education and Research (BMBF), European Union, NIH, Bertelsmann Foundation and Heinz-Nixdorf Foundation. H.-C.D. has no ownership interest and does not own stocks in any pharmaceutical company.
References
- 1.Hammer M, Jovin T, Wahr JA, Heiss WD. Partial occlusion of the descending aorta increases cerebral blood flow in a nonstroke porcine model. Cerebrovasc Dis. 2009;28:406–410. doi: 10.1159/000235628. [DOI] [PubMed] [Google Scholar]
- 2.Lylyk P, Vila JF, Miranda C, Ferrario A, Romero R, Cohen JE. Partial aortic obstruction improves cerebral perfusion and clinical symptoms in patients with symptomatic vasospasm. Neurol Res. 2005;27(suppl 1):S129–135. doi: 10.1179/016164105X35512. [DOI] [PubMed] [Google Scholar]
- 3.Emery DJ, Schellinger PD, Selchen D, Douen AG, Chan R, Shuaib A, Butcher KS. Safety and feasibility of collateral blood flow augmentation after intravenous thrombolysis. Stroke. 2011;42:1135–1137. doi: 10.1161/STROKEAHA.110.607846. [DOI] [PubMed] [Google Scholar]
- 4.Hammer MD, Schwamm L, Starkman S, Schellinger PD, Jovin T, Nogueira R, Burgin WS, Sen S, Diener HC, Watson T, Michel P, Shuaib A, Dillon W, Liebeskind DS. Safety and feasibility of NeuroFlo use in eight- to 24 h ischemic stroke patients. Int J Stroke. doi: 10.1111/j.1747-4949.2011.00719.x. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shuaib A, Bornstein NM, Diener HC, Dillon W, Fisher M, Hammer MD, Molina CA, Rutledge JN, Saver JL, Schellinger PD, Shown-keen H. SENTIS Trial Investigators: Partial aortic occlusion for cerebral perfusion augmentation: Safety and Efficacy of NeuroFlo in Acute Ischemic Stroke Trial. Stroke. 2011;42:1680–1690. doi: 10.1161/STROKEAHA.110.609933. [DOI] [PubMed] [Google Scholar]
- 6.Liebeskind DS. Aortic occlusion for cerebral ischemia: from theory to practice. Curr Cardiol Rep. 2008;10:31–36. doi: 10.1007/s11886-008-0007-3. [DOI] [PubMed] [Google Scholar]
- 7.Bhatnagar P, Sinha D, Parker RA, Guyler P, O'Brien A. Intravenous thrombolysis in acute ischaemic stroke: a systematic review and meta-analysis to aid decision making in patients over 80 years of age. J Neurol Neurosurg Psychiatry. 2011;82:712–717. doi: 10.1136/jnnp.2010.223149. [DOI] [PubMed] [Google Scholar]
- 8.Engelter ST, Reichhart M, Sekoranja L, Georgiadis D, Baumann A, Weder B, Müller F, Lüthy R, Arnold M, Michel P, Mattle HP, Tettenborn B, Hungerbühler HJ, Baumgartner RW, Sztajzel R, Bogousslavsky J, Lyrer PA. Thrombolysis in stroke patients aged 80 years and older: Swiss survey of IV thrombolysis. Neurology. 2005;65:1795–1798. doi: 10.1212/01.wnl.0000183702.04080.27. [DOI] [PubMed] [Google Scholar]
- 9.N Engl J Med. Vol. 333. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group; 1995. Tissue plasminogen activator for acute ischemic stroke. pp. 1581–1587. [DOI] [PubMed] [Google Scholar]
- 10.Wahlgren N, Ahmed N, Eriksson N, Aichner F, Bluhmki E, Dávalos A, Erilä T, Ford GA, Grond M, Hacke W, Hennerici MG, Kaste M, Köhrmann M, Larrue V, Lees KR, Machnig T, Roine RO, Toni D, Vanhooren G. Safe Implementation of Thrombolysis in Stroke-MOnitoring STudy Investigators: Multivariable analysis of outcome predictors and adjustment of main outcome results to baseline data profile in randomized controlled trials: Safe Implementation of Thrombolysis in Stroke-MOnitoring STudy (SITS-MOST). Stroke. 2008;39:3316–3322. doi: 10.1161/STROKEAHA.107.510768. [DOI] [PubMed] [Google Scholar]
- 11.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee: Executive summary: heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation 2012. 125:188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 12.Arkadir D, Eichel R, Gomori JM, Ben Hur T, Cohen JE, Leker RR. Multimodal reperfusion therapy for large hemispheric infarcts in octogenarians: is good outcome a realistic goal? AJNR Am J Neuroradiol. 2012;33:1167–1169. doi: 10.3174/ajnr.A2916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qureshi AI, Suri MF, Georgiadis AL, Vazquez G, Janjua NA. Intra-arterial recanalization techniques for patients 80 years or older with acute ischemic stroke: pooled analysis from 4 prospective studies. AJNR Am J Neuroradiol. 2009;30:1184–1189. doi: 10.3174/ajnr.A1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berrouschot J, Rother J, Glahn J, Kucinski T, Fiehler J, Thomalla G. Outcome and severe hemorrhagic complications of intravenous thrombolysis with tissue plasminogen activator in very old (< or = 80 years) stroke patients. Stroke. 2005;36:2421–2425. doi: 10.1161/01.STR.0000185696.73938.e0. [DOI] [PubMed] [Google Scholar]
- 15.Mishra NK, Diener HC, Lyden PD, Bluhmki E, Lees KR. Influence of age on outcome from thrombolysis in acute stroke: a controlled comparison in patients from the Virtual International Stroke Trials Archive (VISTA). Stroke. 2011;41:2840–2848. doi: 10.1161/STROKEAHA.110.586206. [DOI] [PubMed] [Google Scholar]
- 16.Nathoe HM, Koerselman J, Buskens E, van Dijk D, Stella PR, Plokker TH, Doevendans PA, Grobbee DE, de Jaegere PP, Octopus Study Group Determinants and prognostic significance of collaterals in patients undergoing coronary revascularization. Am J Cardiol. 2006;98:31–35. doi: 10.1016/j.amjcard.2006.01.050. [DOI] [PubMed] [Google Scholar]