Abstract
We investigate whether physicians' financial incentives influence health care supply, technology diffusion, and resulting patient outcomes. In 1997, Medicare consolidated the geographic regions across which it adjusts physician payments, generating area-specific price shocks. Areas with higher payment shocks experience significant increases in health care supply. On average, a 2 percent increase in payment rates leads to a 3 percent increase in care provision. Elective procedures such as cataract surgery respond much more strongly than less discretionary services. Non-radiologists expand their provision of MRIs, suggesting effects on technology adoption. We estimate economically small health impacts, albeit with limited precision.
Critics contend that fee-for-service medicine leads to high medical expenditures without improving patient health.1 Alternatively, the incentives embedded in volume-based compensation may facilitate access to valuable treatments (Ellis and McGuire 1986).2 Determining the fiscal consequences of volume-based payment policies and the health benefits of incremental care are thus pressing empirical tasks (Baicker and Chandra 2011).
We study how changes in physicians' financial incentives influence the quantity, composition, and value of health care they provide. Since payment policies may influence medical innovation through their effect on technology adoption (Weisbrod 1991; Chandra and Skinner 2012), we examine their impact on physicians' use of high margin technologies.3 Finally, we investigate the consequences of incremental treatments and technologies for patient health, the crucial outcome for any intervention in health care financing and delivery.
We estimate the effects of payment rates using an overhaul of geographic adjustments to provider reimbursements in the Medicare program. In 1997, Medicare consolidated the areas across which it adjusts physician payments, reducing the number of payment regions nationally from 210 to 89. This consolidation, which is similar to that studied by Rice (1983) in Colorado, led to area-specific price shocks that are plausibly exogenous with respect to other changes in local health care demand and supply.4 We use these payment changes to estimate the effect of prices on care provision, the utilization of advanced technologies, and patient health.
We find that physician and outpatient care follows a traditional positively-sloped supply curve. Care supplied to Medicare patients exhibits a relatively large long-run elasticity of around 1.5 with respect to reimbursement rates. We are unable to determine with precision whether private patient care also responds, either through patient substitution or treatment spillovers. The implications for overall health care spending thus remain ambiguous.
Reimbursement changes lead physicians to adjust treatment patterns along several margins. Responses are strongest amongst relatively elective services. The intensity of the average service also rises substantially while the total number of services changes little. The responses unfold over several years, suggesting that changes in profitability induce dynamic changes in physician practice.
To understand the timing and size of these supply responses, we develop a model of physicians' joint supply and investment decisions. In our framework, doctors have heterogeneous productivity and can pay to invest in a productivity-enhancing technology. They value their own income as well as patient health. This framework predicts relatively large supply responses when many providers are near the margin of adopting new practice styles and when large numbers of patients would benefit moderately from incremental care.5 We then test these predictions empirically in a range of settings.
We first observe that the aggregate supply response is concentrated primarily among relatively elective procedures, including cataract removal and colonoscopy. There is little response among less discretionary services, such as oncological procedures and dialysis. Our model of physician behavior predicts exactly this pattern; when physicians value patient health, services with a clear benefit for some patients, and potential harm for others, should respond less to payment rates.
We next examine a mechanism that may drive the size and dynamics of the supply response, namely the spread of advanced technologies. While financial incentives strongly affect the development and production of pharmaceuticals (Acemoglu and Linn 2004; Finkelstein 2004; Yin 2008; Yurukoglu 2012), as well as the diffusion of technologies across hospitals (Finkelstein 2007; Acemoglu and Finkelstein 2008), less is known about the adoption of the technologies used in outpatient settings.6 We investigate the vertical integration of office visits and imaging services that occurs when non-radiologists acquire magnetic resonance scanners. While further study is needed, we find modest evidence that reimbursement rates influence these investment decisions and hence the diffusion of medical technology. Such responses, which mirror findings of Finkelstein (2007) and Acemoglu and Finkelstein (2008) in the context of hospitals, will tend to magnify the direct effect of reimbursement-rate changes on physicians' profit margins.
In our context, the wedge between cost and consumer payments raises classic moral hazard concerns. Evaluating the welfare consequences of treatment expansions requires direct estimation of incremental care's health benefits. For this we focus on patients with cardiovascular disease, who face significant potential gains from medical treatments thanks to technologies like cardiac catheterization. They also have much at risk since heart disease is the leading cause of mortality in the United States (Cutler 2004; Murphy and Topel 2006). Consistent with our aggregate results, we find that payment increases significantly expand the supply of services to these patients, with an overall price elasticity of 0.9. This incremental care has insignificant effects, though estimated with limited precision, on mortality, hospitalizations, and heart attacks. If anything, additional outpatient care is positively associated with hospital expenditures.
These results resonate with the RAND Health Insurance Experiment's demand-side finding that care induced by reductions in patient cost-sharing has little impact on health (Manning et al. 1987). In contrast with the RAND study, Chandra, Gruber, and McKnight (2010) find that incremental preventive care reduces subsequent hospital expenditures. We find that reimbursement-induced increases in the provision of broader packages of outpatient care do not similarly substitute for inpatient care.
Our results suggest that, together with medical technology (Newhouse 1992), changes in patient cost sharing (Finkelstein 2007), and increases in the demand for health (Hall and Jones 2007), providers' financial incentives may play an important role in driving the health sector's size. Payment policy has significant implications for Medicare's costs. In contrast with the federal budgeting process, which assumes that backward-bending labor supply drives a 30 to 50 percent “volume offset,” or negative supply response (Congressional Budget Office 2007; Codespote, London, and Shatto 1998), we find that aggregate Medicare spending reacts positively to reimbursement rates.
I. Price Shock From 1997 Payment Area Consolidation
We estimate the influence of price shocks on health care provision, technological diffusion, and health outcomes in the context of Medicare Part B, which finances physician and outpatient care for most elderly Americans.7 Since 1992, Medicare has paid physicians and other outpatient providers through a system of centrally administered prices, based on a national fee schedule. While the fee schedule assigns a fixed “relative value” (a quantity metric) to each health care service,8 it recognizes that goods and services have different production costs in different parts of the country. For service j, supplied by a provider in payment area a, the provider's fee is approximately9
| (1) |
The Conversion Factor is a national adjustment factor, updated annually and generally identical across all services; it was equal to $37.8975 in 2005.10 The Relative Value Units (RVUs) associated with service j are intended to measure the resources required to provide that service. RVUs are constant across areas while varying across services. Finally, the Geographic Adjustment Factor (GAF) is the federal government's adjustment for differences in input costs across payment regions. The adjustments are derived from census and other data on area-level rents, wages, and malpractice insurance premiums. Reimbursements for physicians in county i depend on the beneficiary-weighted average of input costs across all counties in payment area a(i).11
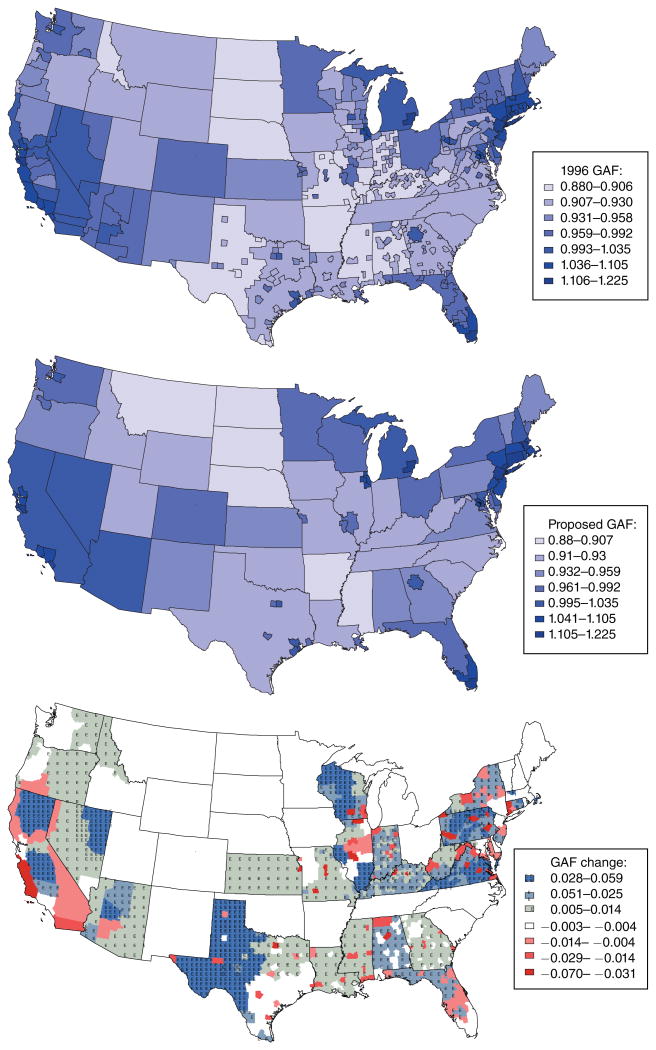
We estimate the influence of prices on health care supply using changes induced by an administrative shift in the system of geographic adjustments. In 1997, the Health Care Financing Administration consolidated the payment regions in many states, leading to reimbursement rate shocks that vary across the pre-consolidation regions. The 210 payment areas that existed as of 1996 were consolidated to 89 distinct regions, as shown in Figure 1. The top panel of Figure 1 presents the regions as of 1996, with darker colors indicating higher GAFs; the middle panel shows the post-consolidation payment regions. As the maps indicate, the consolidation of payment regions dramatically changed the county groupings in many states, leading to differential price shocks, which we denote ΔRR. We estimate the responses of medical care supply, technology adoption, and patient welfare to these shocks.12
Figure 1. Medicare Payment Areas.
Notes: The first panel shows the 206 Medicare fee schedule areas in the continental United States as of 1996 and the second shows the 85 such localities after the consolidation in 1997. (These totals exclude Alaska, Hawaii, Puerto Rico, and the US Virgin Islands, each of which was its own unique locality throughout this period.) The colors indicate the Geographic Adjustment Factors (GAF) associated with each Payment Locality, with darker colors indicating higher reimbursement rates. The third panel shows the change in -GAF for each county due to the payment region consolidation that took place in 1997.
Source: Federal Register, various issues.
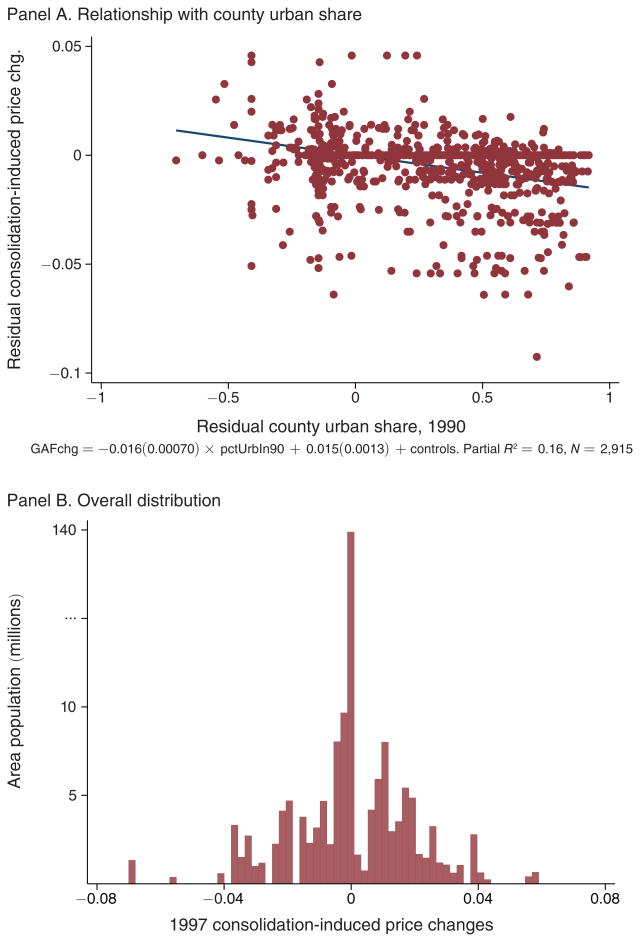
A comparison of these two maps, summarized in the third panel, reveals key features of the payment area consolidation. First, substantial variation in reimbursement rates was eliminated in many states. Wisconsin, Kentucky, Alabama, and several others were collapsed from multiple regions to a single statewide payment area. The number of regions was also reduced substantially in large states like Texas and California. Second, increases in reimbursement rates generally took place in rural areas while decreases took place in urban areas, as Figure 2 shows. We address the possibility of differential trends across these areas by flexibly controlling for time-varying rural-urban differences, by restricting our sample to those counties that pass a matching criterion, and by checking for pre-existing trends that are correlated with ΔRR.
Figure 2. Distribution of Consolidation-Induced Price Shocks.
Notes: Panel A shows the relationship between the county-level changes in the Geographic Adjustment Factor (GAF) from Figure 1 and each county's urban population share in 1990, after controlling for state fixed effects. Letting i denote counties, s(i) each county's state, and ΔRRi the reimbursement rate change from Figure 1, we estimate:
across a cross section of counties. Panel A plots the residuals resulting from these regressions. Panel B shows the distribution of the county-level changes in the GAF, weighted by county population. Note that the y-axis scale has been adjusted at the high end to accommodate the large number of counties in states with no price change.
Sources: Price change: Federal Register, various issues; county population: US Census.
A. County-Level Analysis
Letting ΔRRi denote the price shocks discussed above, we estimate the effect of reimbursements on care provision using the following equation:
| (2) |
Our most comprehensive measure of health care supply is the log of total RVUs provided per patient seen in county i in state s(i) during year t. We later decompose care across service and provider types as well as by service quantity and intensity.
We present two forms of evidence, which involve variations on specification (2). Our reimbursement rate changes ΔRRi are a fixed characteristic for each county, defined using the one-time consolidation. We interact ΔRRi with an indicator Ip(t) for observations in period p(t). The forms of evidence, which can be characterized as full parametric event studies and parametric difference-in-differences estimators, are differentiated by the manner in which we specify the p(t).
In full parametric event studies, which we present graphically, each period corresponds to a year. We omit t = 1996 so that each βp(t) is estimated relative to the year immediately preceding the price shocks. Estimates of βp(t) for periods prior to 1996 provide a sense for the importance of pre-existing trends that are correlated with ΔRRi, while estimates of βp(t) for years following 1996 measure the effect of the reimbursement rate changes on care provision. For parametric difference-in-differences estimates we group years, typically into short-, medium-, and long-run post-consolidation periods, and estimate each βp(t) relative to a base period extending from 1993 to 1996.13 Since the quantity of RVUs per beneficiary is expressed in logs and the GAF is an index normalized to a have mean of 1, these βp(t) coefficients can be interpreted as short-, medium-, and long-run elasticities. In both cases we denote county fixed effects by γi, year fixed effects by δt, and state-by-year effects by ηs(i), t. These fixed effects capture the effects of other changes to payment policies and the structure of medical care that took place during this time period, which we discuss in online Appendix A.2.
We control for county characteristics Xi,s(i),t that are correlated with the consolidation-induced GAF changes or may be important determinants of care per Medicare beneficiary. Since price increases occurred primarily in rural areas while decreases occurred in urban areas, we allow for differential urban-rural trends by controlling for interactions between year indicators and proxies for an area's urban status.14 We measure urban status with two variables: the share of an area's population classified as urban by the Census Bureau, and whether the county is in a metropolitan statistical area.15 We confirm that the baseline estimates are robust to controlling similarly for base year quantities of care, county population, and/or county population density. To reduce noise resulting from changes in the underlying health of the beneficiaries sampled from small counties, we use standard controls for the fraction of each county's sample that meets particular health and demographic criteria.
Our baseline estimate of equation (2) uses a sample of counties that pass the following matching procedure. We first regress ΔRR on baseline county characteristics using the sample of states in which payment locality consolidations occurred (the “affected” sample).16 Using the results from this regression, we generate predicted price shocks for the full sample of counties, including those that are not in states that were affected by consolidations. The sample used in our baseline estimates includes all nearest-neighbor matches (matched on the predicted price shocks) between a county from the “affected” set of states and a county from the unaffected set.17 We calculate standard errors under the assumption that the error term εi,s(i),t is clustered at the level of pre-1997 payment areas.
B. Payment Area Level Analysis
In nearly all cases, the consolidation affected payments identically throughout each pre-consolidation payment area.18 This makes the pre-consolidation payment regions the natural unit of analysis for purposes of statistical inference. However, direct aggregation to the payment regions would largely eliminate our ability to control for differential urban-rural trends in the supply of health care. To see why, consider the regions in neighboring Wisconsin and Minnesota as shown in Figure 1. In 1997, Wisconsin was consolidated from eight payment regions into one while Minnesota consisted of a single region throughout our sample. Rural Minnesota thus implicitly provides a counterfactual for rural Wisconsin in the absence of its consolidation, and similarly for the states' urban areas. But Minnesota becomes a less useful average of its urban and rural regions when aggregated directly to the payment area level.
To ensure appropriate statistical inference, we conduct our baseline analysis at the payment area level. But to fully utilize the desirable properties of our natural experiment we do this after partialing out county-by-year characteristics. Letting p̃a,t denote the payment area's adjusted log RVUs and its adjusted reimbursement rate interaction for period p in year t, we estimate the following regression:19
| (3) |
where the θp(t) coefficients are our estimated supply response in period p(t) and ua,t is the error term. As discussed above, the analysis includes both full parametric event studies, in which each period corresponds to a year, and parametric difference-in-differences estimates, in which the event study results are more concisely summarized. This estimation is described in greater detail in online Appendix B.1. To adjust for unobserved shocks correlated within a payment area, as well as potential measurement error in our residualizing procedure, we estimate standard errors using the nonparametric bootstrap described in online Appendix B.1. The procedure allows us to (i) make meaningful use of controls at the county level; (ii) conduct inference at the appropriate level; and (iii) account for unobserved correlated shocks within payment areas over time.
C. Medicare Data
Our data on health care provision come from claims submitted by providers to Medicare for reimbursement. The data document all claims associated with a 5 percent random sample of the Medicare Part B beneficiary population for each year from 1993 through 2005.20 The same individuals are sampled each year, and the data contain itemized reports of the services purchased for them by Medicare. We obtain demographic information about our beneficiary sample from the Denominator files. Summary statistics for the baseline sample are reported in Table 1.
Table 1. Summary Statistics.
| N | Mean | SD | Range | |
|---|---|---|---|---|
| Consolidation-induced shock to Medicare Part B reimbursement rates | ||||
| Counties with price decline | 258 | −0.015 | (0.012) | (−0.070, 0) |
| Counties with no change | 720 | 0.000 | (0.000) | (0, 0) |
| Counties with price gain | 1,202 | 0.018 | (0.011) | (0.0001, 0.059) |
| County population (thousands) | ||||
| Counties with price decline | 258 | 192 | (305) | (3, 2, 498) |
| Counties with no change | 720 | 67 | (160) | (1, 1, 853) |
| Counties with price gain | 1,202 | 40 | (73) | (2, 969) |
| County urban share (percent) | ||||
| Counties with price decline | 258 | 41.2 | (40.0) | (0, 100) |
| Counties with no change | 720 | 11.7 | (27.7) | (0, 100) |
| Counties with price gain | 1,202 | 6.7 | (20.3) | (0, 100) |
| Health care provided to Medicare beneficiaries, county-by-year | ||||
| RVUs per patient | 28,340 | 18.41 | 17.65 | (1.78, 94.65)* |
| Charges per patient | 28,340 | $508.61 | $332.85 | ($86.03, $1, 638.63)* |
Note:
Ranges shown from the first to the ninety-ninth pecentile of the distribution because confidentiality requirements prevent the release of data points generated from ten or fewer beneficiaries.
Sources: Price change: Federal Register, various issues; county characteristics: Ruggles et al. (2010); Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC.
We compute the aggregate quantity of health care supplied to this sample of beneficiaries using the scaling of individual services used by the Centers for Medicare and Medicaid Services (CMS) to reimburse providers (Relative Value Units). Since the GAF is associated with the location of the service provider, we assign services to counties using providers' zip codes. We provide further details in online Appendix B.2.
II. The Impact of Price Changes on Aggregate Care
A. Overall Supply Response
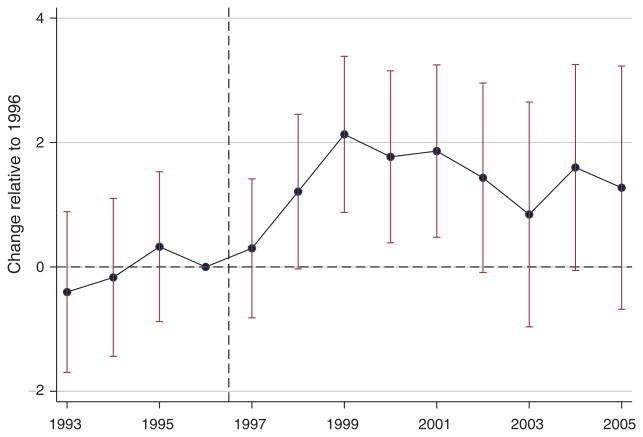
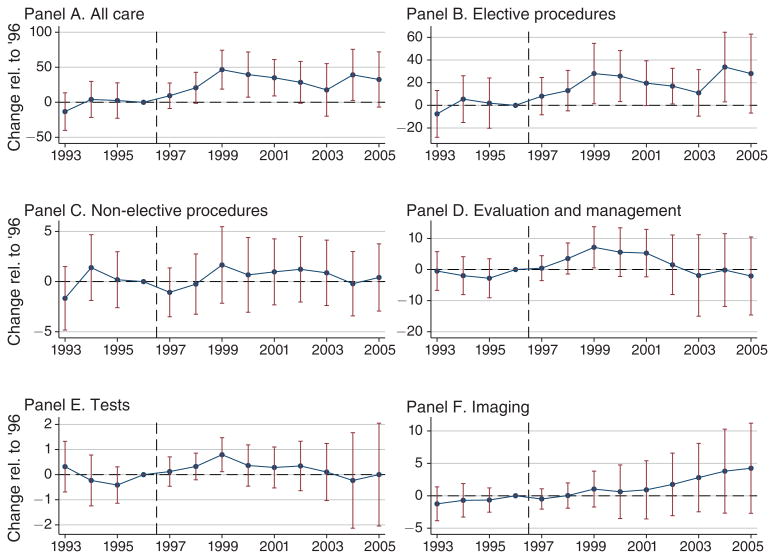
Our baseline estimates of the effect of changes in reimbursement rates on aggregate quantities of care are shown in Figure 3. This graph reports the θt coefficients from estimating equation (3) as a parametric event study, with standard errors estimated using the bootstrap described in online Appendix B.1. We find that Medicare services respond significantly to prices, building toward a long-run elasticity around 1.5 over the years following the price shock. Estimates for years prior to 1996 show that Δ RR was not correlated with a pre-existing trend in service supply, giving us confidence in our methods of controlling for relevant county characteristics.
Figure 3. Impact of Price Change on Aggregate Quantity Supplied.
Notes: This figure shows coefficients and associated bootstrap standard errors from an ordinary least squares regression in which log health care quantity supplied per Medicare patient is the dependent variable. This quantity is regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, as interacted with indicator variables for each year. This regression is run at the payment area level after partialing out the controls listed below, as described in Section IB, and coefficients correspond to θp parameters in equation (3). The controls include county fixed effects, state-by-year effects, a set of year dummy variables interacted with each county's 1990 urban population share and an indicator for metropolitan status, as well as the fraction of beneficiaries aged 65–59, 70–74, 75–79, and 80–84, black, Hispanic, female, eligible for Medicare due to end-stage renal disease or due to disability, with 2 or more, 3 or more, 4 or more, and 6 or more comorbidities as defined by Elixhauser et al. (1998). Standard errors are calculated using the bootstrap method described in online Appendix B.1.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; county population: Census Bureau.
Table 2 shows these results as parametric difference-in-differences estimates. The first column shows the βp(t) coefficients from estimating equation (2) at the county level. Column 2, which reports our baseline estimates, is estimated at the payment area level and uses the bootstrap described in online Appendix B.1 to estimate standard errors. Both columns report supply elasticities of 0.8 in the short run, nearly 2 in the medium run, and roughly 1.45 in the long run. Bootstrapping at the payment area level increases the standard errors estimated in column 1 by roughly 10 percent.
Table 2. Effect of Reimbursement Rates on log Health Care per Patient.
| Aggregate health care supply: ln(relative value units per patient) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| County level (1) | Baseline (2) | Weighted (3) | Unmatched counties (4) | w/ HMO control (5) | No demog. Controls (6) | No comorb. Controls (7) | Population controls (8) | |
| Price change × short run | 0.801 (0.531) | 0.817 (0.596) | 1.010 (0.721) | 0.454 (0.554) | 0.741 (0.598) | 0.763 (0.596) | 0.776 (0.579) | 1.223** (0.653) |
| Price change × medium run | 1.966*** (0.650) | 2.012*** (0.770) | 1.952** (0.825) | 1.676** (0.701) | 1.876** (0.762) | 1.956** (0.770) | 1.996*** (0.750) | 2.583*** (0.827) |
| Price change × long run | 1.423* (0.735) | 1.464* (0.884) | 2.686** (1.211) | 1.391* (0.790) | 1.405 (0.888) | 1.405 (0.880) | 1.423 (0.889) | 2.268** (0.938) |
| Old MPLs | 177 | 177 | 177 | 200 | 177 | 177 | 177 | 177 |
| Estimation | OLS | OLS | OLS | OLS | OLS | OLS | OLS | OLS |
| Standard errors | Clustered | Bootstrap | Bootstrap | Bootstrap | Bootstrap | Bootstrap | Bootstrap | Bootstrap |
| Observations | 28,340 | 2,301 | 2,301 | 2,600 | 2,301 | 2,301 | 2,301 | 2,301 |
Notes: This table reports coefficients from ordinary least squares regressions in which log health care quantity supplied per Medicare patient is the dependent variable. This quantity is regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, as interacted with indicators for time relative to the payment area consolidation. “Short Run” following the consolidation refers to 1997 and 1998, “Medium Run” refers to 1999 and 2000, while “Long Run” refers to 2001 through 2005. In column 1, this regression is run at the county level, as described in Section IA. In columns 2 through 8, it is run at the payment area level after partialing out the following controls, as described in Section IB: county fixed effects, state-by-year effects, and a set of year dummy variables interacted with the county's 1990 urban population share and an indicator for metropolitan status. For all regressions except column 4, we restrict the sample to counties satisfying the matching criterion described in Section IA. Column 5 adds as a control the share of Medicare beneficiaries enrolled in an HMO. The demographic controls used in all regressions except column 6 are the fraction of the county's sample beneficiary pool aged 65–59, 70–74, 75–79, and 80–84, the fraction black, Hispanic, female, eligible for Medicare due to end-stage renal disease or due to disability. All regressions except column 7 control for the share of beneficiaries with 2 or more, 3 or more, 4 or more, and 6 or more comorbidities as defined by Elixhauser et al. (1998). Column 8 controls for year interacted with county population instead of urban share. Standard errors are calculated with the bootstrap from online Appendix B.1.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; county characteristics: Ruggles et al. (2010).
The remaining columns of Table 2, supplemented by online Appendix Figure D.1, show the robustness of the baseline results to a variety of specification changes. The specification changes include weighting counties according to the average pre- consolidation number of patients, augmenting the sample by including counties that failed our matching procedure, controlling for the fraction of each county's sample of beneficiaries receiving coverage through a Medicare Advantage HMO, dropping the demographic controls, dropping the comorbidity controls, and controlling for differential rural-urban trends on the basis of county population rather than the urban population share. With one exception, the coefficients in columns 3 through 8 are within one standard error of the corresponding baseline coefficient. The exception involves the alternative weighting of counties in column 3, where the long-run elasticity is estimated to be 2.7 rather than 1.5. We illustrate the parametric event studies corresponding to each column of Table 2 in online Appendix Figure D.1. The patterns of coefficients are similar to those observed in Figure 3. Finally, online Appendix Table D.1 combines the short-, medium-, and long-run coefficients into a single post-consolidation time period.
We characterize these initial results as fairly robust evidence for a traditional, positively sloped supply curve. The medium- and long-run elasticities, of 2 and 1.5 respectively, suggest that the supply of services to Medicare beneficiaries is quite responsive to across-the-board changes in Medicare's payment rates.
B. Interpreting Reimbursement-Rate Elasticities
The elasticity just estimated is an elasticity of care for Medicare beneficiaries with respect to Medicare's reimbursement rates. Properly interpreting this elasticity requires first observing how it differs from more traditional labor supply elasticities. An initial difference, emphasized in the subsequent section's conceptual framework, is that many avenues for expanding a physician's practice require little of the physician's own labor. The concept of a labor supply elasticity is thus not particularly well suited to this context. A related point is that the reimbursement rate is not equivalent to the physician's wage; variable costs associated with providing incremental services imply that net wages are smaller than reimbursement rates. Medicare's accounting of resource intensity implies that a physician's “own work” accounts for 40 percent of the cost of providing a typical service.21 A 1 percent change in reimbursement rates thus translates, on average, into a 2.5 percent change in the physician's net wage. Hence a reimbursement-rate elasticity of 1.5 translates into a wage elasticity of around 0.6.22
A final point, emphasized by McGuire and Pauly (1991), is that one potentially important response to reimbursement rates involves physicians' decisions over whom to treat. Providers can substitute between treating more profitable and less profitable patients due to either income or price effects, and changes in the incentives associated with one set of patients can influence the treatment of others (Glied and Graff Zivin 2002). We investigate such effects in online Appendix Tables D.2 and D.3 using private insurance data from large employers, but the estimates suffer from substantial imprecision.23 The confidence intervals encompass a wide range of possible effects, including both substitution away from private patients and spillovers associated with uniform application of a particular “practice style.”24
Theories of a target income predict that physicians may react differently to a negative payment shock than to a positive one. In online Appendix Tables D.2 and D.3 we also test for differences between the supply elasticity in these two cases. We are unable to distinguish between responses to positive and negative shocks with any precision.
While the aggregate national effects are ambiguous, the effect of Medicare's reimbursements on the treatment of Medicare beneficiaries is large and positive. We next present a model of physician behavior that motivates our further exploration both of the welfare implications of this response and of the economic forces behind it.
III. Reimbursement Rates, Physician Practice Styles, and the Supply of Health Services
The magnitude and timing of supply responses raise two further sets of questions. First, why are supply responses large and not instantaneous? Second, what are the welfare implications of physicians' changing treatment decisions? To explore these issues, we present a model of the incentives and choices physicians face. The model highlights three distinctive characteristics of the supply of health-care services and the welfare implications of reimbursement rates. These include physician altruism, insurance-induced limits on consumer cost exposure, and differences in physician practice styles. We focus on the adoption of medical technologies as an example of practice style differences.
A. Medical Care Supply
In our framework, physicians can practice medicine using a standard practice style (S) that has a variable cost of c̅ per unit of care, or an intense practice style (I) that reduces unit costs to but costs k > 0 to adopt. Orthopedists can acquire advanced imaging equipment, for example, while urologists can invest in radiation therapy units and cardiologists can integrate nuclear stress testing into their practices.25 The crucial property of these technologies is not quality or sophistication, but rather that they lower the marginal cost of producing medical services. Such investments involve up-front costs, subsequently allowing practices to generate revenue with low marginal costs and minimal use of its physicians' valuable time.
Because insurance diminishes or eliminates price sensitivity (Feldstein 1973) and consumers lack information about treatment options, physicians make many health care decisions on their patients' behalf (Arrow 1963). We assume that demand is unsatiated, so that physicians' supply decisions drive the quantity of health care their patients receive.26 Since physicians act, at least in part, as agents on each patient's behalf, the patient's benefit curve influences supply decisions.27 Using Q to denote the market's aggregate supply, we let b(Q) capture the health benefit of marginal care. This benefit enters directly into the physician's utility function. Marginal benefits are decreasing in Q and individual physicians take b(Q) as given.
A continuum of physicians has productivity γi distributed over (0, ∞) according to F(·), already known when they make investment decisions. Doctor i takes 1/γi units of time to produce one unit of care. Each must choose a technology, S or I, and quantity of care, q. Medicare compensates providers for this care according to administratively set payments at reimbursement rate r per unit of care (Newhouse 2003). With quasilinear utility in income, utility in the standard and intense practice regimes is28
| (4) |
where e is an increasing and convex function of physician time that captures decreasing returns to leisure. 29 The last term captures physicians' desire to provide beneficial care. This agency benefit is linear in the value of care, the amount supplied, and the weight placed on patient benefits. Proposition 1 defines physicians' utility maximizing investment and service-supply decisions.
PROPOSITION 1: There exists a threshold productivity γ* such that physicians invest if and only if γ > γ*. The threshold decreases in the reimbursement rate r and in the weight placed on patient benefits α. Aggregate supply increases in the reimbursement rate, with a slope given by
| (5) |
where
| (6) |
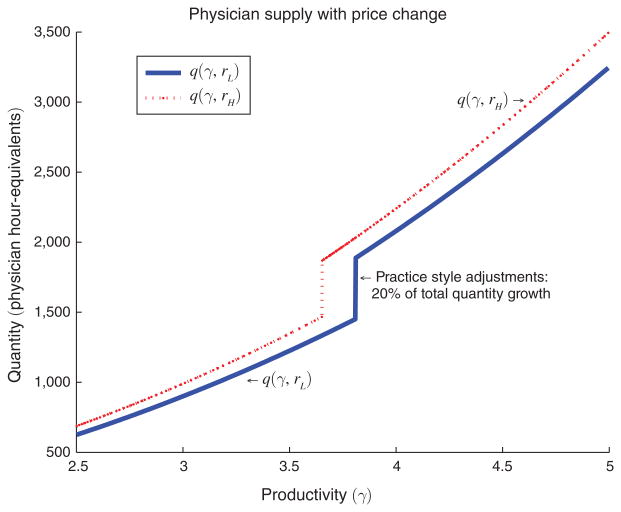
The equilibrium described in Proposition 1, which is proven in online Appendix C, involves two classes of physicians. At a given reimbursement rate, firms above the productivity threshold γ* invest and have higher optimal production levels than firms with γ < γ*, who do not invest. The more productive firms are shown on the right in Figure 4, and the vertical part of the solid line depicts the investment threshold γ*.
Figure 4. Physicians' Production at Two Reimbursement Rates.
Notes: This figure illustrates the effect of reimbursement rates change on physicians' threshold γ* for investing in intensive practice style. At a given reimbursement rate, whether rL or rH, more productive physicians (γ > γ*) invest in the intensive practice style, and quantity supplied is increasing with productivity γ. As shown in Proposition 1, an increase in reimbursement rates from rL to rH increases the quantity supplied for a physician with any fixed productivity γ, and also reduces the investment threshold γ*, meaning that more physicians invest. The increase in supply due to the threshold shift is labeled “Practice Style Adjustments.” The parameters underlying this calibration are given in online Appendix C.2.
The supply response described by equation (5) is composed of three parts, corresponding to the three regions of the figure. The first term, which integrates over the lower part of the effort cost distribution, captures the supply shift from firms that do not invest at either reimbursement rate. The second term captures a similar continuous shift from firms that invest at either price. Below we say more about these first two terms, which are further characterized by equation (6). The “practice style effect” drives some firms to invest only after the reimbursement rate rises, illustrated by the shift in the vertical line. These firms expand quantity supplied dramatically after the return to investing increases. The magnitude of this effect depends on the density of firms near the investment threshold (Caballero and Engel 1999), and is likely to be larger following a period of high uncertainty (Bloom, Bond, and Van Reenen 2007).
B. Health Care Supply and Patient Welfare
Welfare in this market is tightly linked to patient health benefits. Physicians supply care up to the point where their profit margins equal effort cost less their agency benefit from improved patient health. When physicians value health gains (α > 0), supply responds less strongly to prices than it would on the basis of financial motives alone. As can be seen from equation (6), supply responses are particularly small when health benefits diminish rapidly as the market moves down the marginal benefit curve (b′(Q) is very negative). This is likely true with emergency care, which has high benefits for a small fraction of the population and no benefit for the remainder, and treatments such as chemotherapy, which has significant side effects and is only worthwhile for cancer patients. In contrast, elective procedures like cataract surgery offer modest or moderate benefits for large swaths of the population, implying fatter marginal benefit curves (b′(Q) is small) and hence relatively large supply elasticities (Chandra and Skinner 2012).
The quantity is only optimal when the social benefits of marginal care equal its cost. Physicians' optimization ensures that marginal costs equal the reimbursement rate. The equilibrium is thus socially efficient when r = b(Q*), which only holds if payments are set optimally. A sufficient statistic for the welfare impact of price changes is
| (7) |
Higher reimbursements reduce welfare when prices r exceed marginal health benefits b(Q). While we can directly measure r using Medicare's reimbursement rates, health impacts must be estimated directly.
The remainder of this paper explores three issues raised by this section's theoretical framework. We first investigate which types of treatment respond most strongly to prices, generating evidence on the relevance of the marginal benefit curve to physician decision making. We then study the relevance of practice styles by examining a budgetarily important case of physician investments that can be identified in the Medicare claims data, namely the use of MRI machines by non-radiologists. Finally, we explore the effect of incremental care on observable outcomes for a large and important class of patients, namely those with cardiovascular disease.
IV. What Service Types and Supply Margins Respond?
One implication of the previous section's model is that physician concern for patient benefits translates into supply responses that differ based on the marginal benefit of care. We investigate which types of services respond to reimbursements by dividing them according to a standard classification system known as Betos categories.30 The broad Betos categories include Evaluation and Management (e.g., office visits), Testing, Imaging, and Procedures. We examine the role of physician agency by using the medical literature to further divide the Procedures category into more and less discretionary services. The former category includes a variety of non-essential procedures for which the timing of the treatment is highly discretionary (e.g., major joint replacement, cataract removal, and a variety of musculoskeletal procedures), intensive diagnostic services (e.g., catheterization and endoscopy) and procedures related to cardiac care, the intensity of which varies widely around the country. Less discretionary procedures include cancer and dialysis treatments and explicit repair procedures, such as hip fracture repair.31
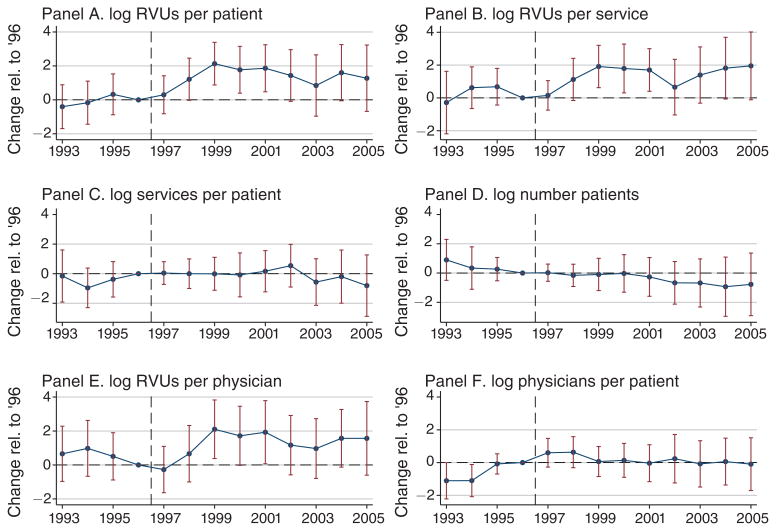
Figure 5 presents the results. Consistent with an important role for physician agency, roughly two-thirds of the supply response loads onto relatively elective services, which are shown in panel B and account for one-third of all care. Online Appendix Tables D.4 and D.5 show that these results imply medium- and long-run elasticities on the order of 4. Estimates for other categories often lack precision, but tend to imply elasticities on the order of 1. The results are consistent with a role for agency because physician concern for patient benefits implies small elasticities when benefits drop off sharply for marginal patients. This is precisely how one might describe benefits from the category of less discretionary services. Once all hip fractures are repaired, for example, the marginal health benefit of an additional hip fracture repair is zero.32 The observed responses imply that the overall composition of services shifts toward more elective procedures as reimbursement rates increase.
Figure 5. Supply Response by Service Category.
Notes: These graphs show coefficients and associated bootstrap standard errors from ordinary least squares regressions in which the quantities of health care supplied in different categories (as measured in Relative Value Units) are the dependent variables. These quantities are regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, as interacted with indicator variables for each year. These regressions are run at the payment area level after partialing out the following controls, as described in Section IB, and coefficients correspond to θp parameters in equation (3): county fixed effects, state-by-year effects, a set of year dummy variables interacted with each county's 1990 urban population share and an indicator for metropolitan status, the fraction of beneficiaries aged 65–59, 70–74, 75–79, and 80–84, black, Hispanic, female, eligible for Medicare due to end-stage renal disease or due to disability, with 2 or more, 3 or more, 4 or more, and 6 or more comorbidities as defined by Elixhauser et al. (1998). Standard errors are calculated with the bootstrap from online Appendix B.1.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; demographics: Ruggles et al. (2010).
We further investigate the composition of health care responses along dimensions including service intensity and physician entry, with results reported in Figure 6 and online Appendix Tables D.8 and D.9. Panels B and C of Figure 6 divide the baseline dependent variable (shown in panel A) into the sum of log RVUs per service and log services per beneficiary. RVUs per service approximates the intensity of the average service patients receive. The results suggest that the total response comes almost exclusively through an increase in the average intensity of each service provided; intensive services thus exhibit larger elasticities than minor services.
Figure 6. Potential Margins of Response.
Notes: These graphs show coefficients and associated bootstrap standard errors from ordinary least squares regressions in which different aspects of health care supply are the dependent variable. These quantities are regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, as interacted with indicator variables for each year. These regressions are run at the payment area level after partialing out the following controls, as described in Section IB, and coefficients correspond to θp parameters in equation (3): county fixed effects, state-by-year effects, a set of year dummy variables interacted with each county's 1990 urban population share and an indicator for metropolitan status, the fraction of beneficiaries aged 65–59, 70–74, 75–79, and 80–84, black, Hispanic, female, eligible for Medicare due to end-stage renal disease or due to disability, with 2 or more, 3 or more, 4 or more, and 6 or more comorbidities as defined by Elixhauser et al. (1998). Standard errors are calculated with the bootstrap from online Appendix B.1.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; demographics: Ruggles et al. (2010).
The remaining panels of Figure 6 consider margins such as the number of patients, RVUs per physician, and physicians per patient. The number of patients is unaffected by the price changes, suggesting that reimbursement rates have little impact on the extensive margin governing whether or not a beneficiary obtains care over the course of the year. The evidence in panels E and F suggests that, with respect to the suppliers of care, the response occurs primarily along the intensive margin of RVUs per physician rather than the extensive margin of physicians per patient.
V. The Impact of Prices on MRI Technology Diffusion
The model in Section III points to the potentially important effects of reimbursement rates on physician investment decisions, which can be broadly construed to include effort to establish referral networks, the development of new skills, and investments in new technology. Here we study the diffusion of advanced imaging technology, specifically magnetic resonance imaging (MRI) machines. While MRI is only one of many high-technology services, its diffusion across provider types has the benefit of being readily tracked in Medicare claims data (Baker 2010). In 2010, Medicare Part B paid roughly $1.6 billion for MRI services (MEDPAC 2012).
A. Physician Ownership of MRI Equipment
In recent years, physicians have increasingly acquired financial interests in the provision of auxiliary services, many of which require substantial capital investments and subsequently have large margins. Specifically, non-radiologists have increasingly installed MR and computed tomography (CT) scanners in their offices (Levin et al. 2008).33 Such investments amplify the direct incentive effects of changes in reimbursement rates as illustrated below.
When a patient complains of back pain, a traditional physician's office might take a detailed patient history, prescribe a painkiller, and schedule follow-up appointments. Suppose that variable costs, such as the staff time allocated to this patient, average 50 percent of a practice's typical service. For this practice, a 2 percent increase in reimbursement rates would imply a 4 percent increase in the profit margin. Now suppose the practice installs a magnetic resonance (MR) scanner. Capital-intensive MRI services come with negligible marginal costs. The profitability of incremental services, specifically of scheduling back pain patients for an immediate MRI appointment, thus rises beyond the initial 4 percent. If the adjustment reduces variable costs by just 10 percent (averaged across the practice's full range of services), from 50 percent to 45 percent in our example, the reimbursement change's dynamic effect on the profit margin will be more than twice its static effect.
B. How Do Prices Influence MRI Provision?
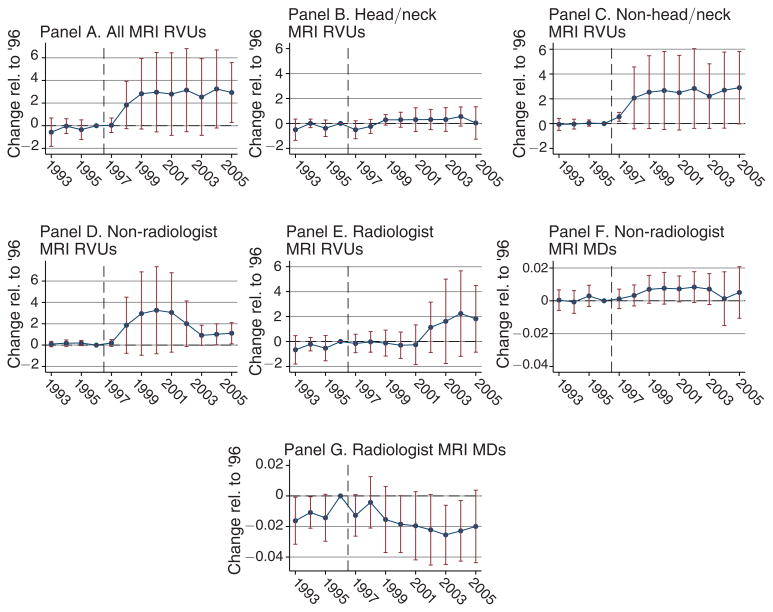
We present our analysis of the effect of payment rates on MRI provision in Figure 7. As in Figures 5 and 6, the regressions are run at the payment area-level, following equation (3) and the procedure outlined in Section IB. In panels A through E, the dependent variables are numbers of RVUs per patient falling into the Betos categories that represent MRIs. In panels F and G, the dependent variables are the numbers of physicians associated with these services.34
Figure 7. Impact of Price Change on MRI Provision and Ownership.
Notes: These graphs show coefficients from ordinary least squares regressions in which the dependent variables are related to the provision of magnetic resonance imaging (MRI) services to Medicare beneficiaries. In columns 1 through 5 provision is measured in terms of Relative Value Units per patient. In panel A this represents total MRI-related RVUs. In panels B and C the total is divided into those associated with MRIs to the head/neck region and all other MRIs. In panels D and E the total is divided into those provided by non-radiologists and those provided by radiologists. Non-radiologist physician ownership of MRI imaging is defined in Section VB, following the method outlined in Baker (2010). In panels F and G the dependent variables are measures of the numbers of non-radiologist and radiologist MDs associated with these services. These variables are regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, as interacted with indicators for time relative to the payment area consolidation. These regressions are run at the payment area level after partialing out the following controls, as described in Section IB: county fixed effects, state-by-year effects, a set of year dummy variables interacted with the county's 1990 urban population share and an indicator for metropolitan status, the fraction of the county's sample beneficiary pool aged 65–59, 70–74, 75–79, and 80–84, the fraction black, Hispanic, female, eligible for Medicare due to end-stage renal disease or due to disability, and the share of beneficiaries with 2 or more, 3 or more, 4 or more, and 6 or more comorbidities as defined by Elixhauser et al. (1998). Standard errors are calculated with the bootstrap from online Appendix B.1.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; demographics: Ruggles et al. (2010).
Panel A shows a positive response of MRI supply to reimbursement rates over the short, medium, and long run. Although economically substantial, the longer-run coefficients are estimated with sufficient imprecision their statistical significance is marginal. Panels B and C split the dependent variable into MRIs in the head/neck region (column 2) and other MRIs, including those of the back (column 3).35 Since the former category tends to be less elective, this decomposition provides another test of the prediction that more elective care is more responsive to price changes on the margin. This prediction is borne out in the data, as the bulk of the response occurs in the category including MRIs of the back. However, the exercise's limited statistical precision should be kept in mind.
We next measure the effect of prices on the organization of MRI provision. We do this by splitting MRIs into those provided by radiologists and independent imaging centers, on the one hand, and those provided by non-radiologists. Panel D shows the result for non-radiological practices, which have high-powered incentives due to their ability to integrate evaluative and imaging services through self-referral; panel E shows the results for radiologists. Although non-radiologists provide 13 percent of all MRIs, they account for the majority of the response we observe.
Panels F and G show a similar pattern for the number of physicians billing for MRIs. The number of non-radiologists is increasing in the price shocks, although the effect is only marginally significant (with p < 0.1) in the medium run and statistically insignificant otherwise. Taken together, the results suggest that MRI provision shifted toward non-radiologists, who played a small role in this market at the beginning of our sample. The responses of these non-radiologists, whose incentives for provision are strong once they have invested in MRI technology, appear to have occurred on both the intensive utilization margin and the extensive adoption margin. The imprecision of these estimates points to a need for further study of the effects of incentives on the diffusion of technology across physicians' practices.
C. Back Pain Patients
To describe how changes in the provision of MRIs relate to changes in a broader package of care, we focus on 475,834 individuals with lower back pain. Back pain is common and often presents with no apparent cause. Deyo and Weinstein (2001) document wide cross-sectional variations in patterns of treatment, and the national time series shows a secular increase in back pain treatment intensity (Friedly, Chan, and Deyo 2007). By definition, back pain is diagnosed on the basis of symptoms, but physicians can use advanced imaging techniques to pinpoint the source of the pain. While these techniques suffer a high rate of false positives (Jensen et al. 1994), they are nonetheless employed frequently. In our sample, 9 percent of back pain patients receive a lumbar spine MRI within the year after diagnosis.
We analyze the impact of our price shocks on treatments received by patients diagnosed with back pain using linear probability models of the form
| (8) |
This patient-level regression uses either (i) an indicator for whether patient k received a given service, or (ii) a count of the number of services received as the outcome variable. Treatment is modeled as a function of the price change (ΔRRi(k)) linked to the county i(k) where patient k was diagnosed. We omit those diagnosed in 1996 since their one-year follow-up would include episodes of exposure to both pre-consolidation and post-consolidation reimbursement rates. We therefore use 1995 as the base year in regressions of treatment outcomes on reimbursement rate shocks. Summary statistics on these patients' demographics and subsequent medical care are presented in online Appendix Table D.16.
Among the treatments we study, the least intensive is physical therapy, which twenty percent of our sample receives despite minimal evidence of effectiveness (Cherkin et al. 1998). We also study spinal injection of corticosteroids, which may generate moderate short-term benefits (Weiner et al. 2006) but which have not been shown to reduce pain over the long term. Back pain patients can also receive spinal surgery (e.g., arthrodesis, diskectomy, laminectomy, or laminotomy) in an effort to resolve problems with vertebrae or intervertebral disks. These surgeries are major operations with serious risks and limited benefits. They are performed on only two percent of our cohort members.
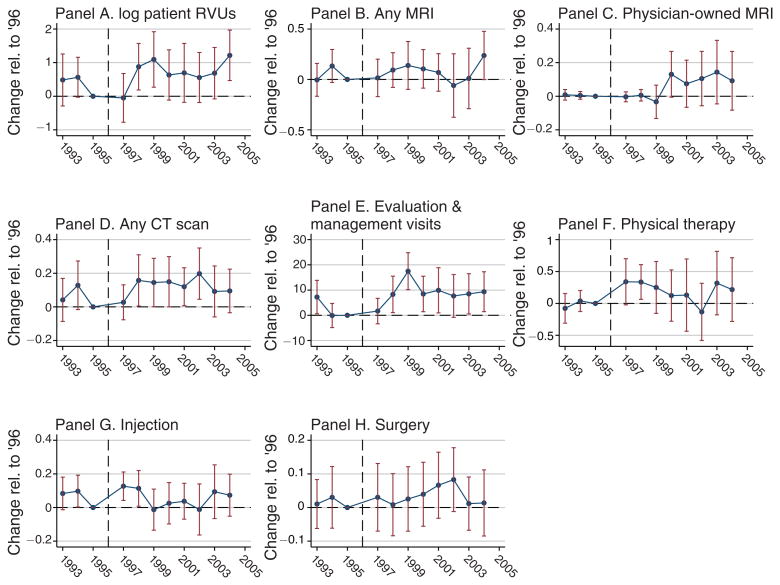
Figure 8 presents our estimates of the effect of reimbursement rates on courses of treatment for back pain. We detect little to no response in the overall provision of MRIs to individuals with back pain (panel B). Consistent with the results in Figure 7, however, we find that the MRIs provided shift away from provision by radiologists and independent imaging facilities (panel C). Online Appendix Table D.12 shows that, conditional on the receipt of an MRI, a 1 percent increase in the reimbursement rate predicts a 1 percentage point increase in the probability that it is administered by a non-radiologist.36
Figure 8. Impact of Price Change on Back Pain Treatment.
Notes: These graphs show coefficients from regressions in which the treatment received by each Medicare patient in the back pain cohorts defined in online Appendix D.1 are the dependent variables. The sample is restricted to patients living in counties that satisfy our matching criterion, as described in the text (the results are essentially unchanged when we include the complete cohort defined in online Appendix D.1). The dependent variables are expressed as indicators for having received a given treatment at least once in the year after diagnosis, with the exception of panel E, which is a count of office visits. Panel C is conditional on having some MRI taken during the year following diagnosis; all other columns include the entire cohort. These variables are regressed on reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, in the county where the patient was first diagnosed, as interacted with indicators for time relative to the payment area consolidation. All specifications control for county fixed effects, state-by-year effects, a set of year dummy variables interacted with an indicator whether the patient resides in a metropolitan area, and indicators for the patient's age, race, gender, and whether or not the individual was eligible for Medicare due to end-stage renal disease. The results are robust to controlling additionally for each patient's health as proxied for by a set of indicators for having the individual comorbidities defined by Elixhauser et al. (1998), as well as having 2 or more, 3 or more, 4 or more, and 6 or more comorbidities. Standard errors are clustered by pre-consolidation payment area.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; county demographics: Ruggles et al. (2010).
Among the treatments available to individuals with back pain, we find moderately strong evidence that office visits and physical therapy respond to prices, while estimates of the effect of prices on injections and surgeries are statistically indistinguishable from zero. The latter results suggest that moderate changes in financial incentives generally do not sway physicians to expose patients to treatments with real risks and minimal expected benefits. At the same time, the results for office visits and physical therapy suggest that these incentives are sufficient to influence the provision of services with modest diagnostic benefits and a low likelihood of causing harm. The estimates for surgery and injection are sufficiently imprecise, however, that the implied elasticities are not statistically distinguishable from the implied elasticities for imaging services, office visits, and physical therapy.
VI. The Impact of Price Changes on Cardiac Patients
In this section we further analyze the effect of reimbursement rates on care provision in the context of patients with cardiovascular disease. Heart disease is the leading cause of mortality in the United States and its treatment has made a large contribution to aggregate increases in life expectancy (Cutler, Rosen, and Vijan 2006). Here we also take up the question of incremental care's impact on patient health. While the model in Section III demonstrated the need for direct estimation of marginal benefits for purposes of welfare analysis, the results presented below highlight the difficulty of this endeavor.
A. Treating Cardiovascular Disease
We study the effect of reimbursement rates on three imaging, testing, and evaluative services that are non-invasive, low intensity, and low risk. The first, echocardiography, is a technique for visualizing a patient's heart, which allows the cardiologist to evaluate its function and anatomy. The second, a stress test, monitors a patient's blood flow and symptoms during exercise (usually, walking on a treadmill). Third, we record the number of distinct office visits experienced by each patient.
We also study the effect of reimbursement rates on the frequency of three relatively intensive procedures involving cardiac catheterization. Catheterization, which requires threading a catheter up an artery into the heart, can be both diagnostic and interventional. In addition to diagnostic catheterization, we study two related interventions: angioplasty and the insertion of stents. Angioplasty reverses arterial occlusion by expanding a balloon catheter within a blood vessel to push plaque out of the bloodstream. A stent is a metal sheath that can be installed in a coronary artery to prevent future occlusion. The medical literature contains extensive debate regarding the risks associated with angioplasty and stent insertion. We study the treatment of individuals with cardiovascular disease using the linear probability model of equation (8).37
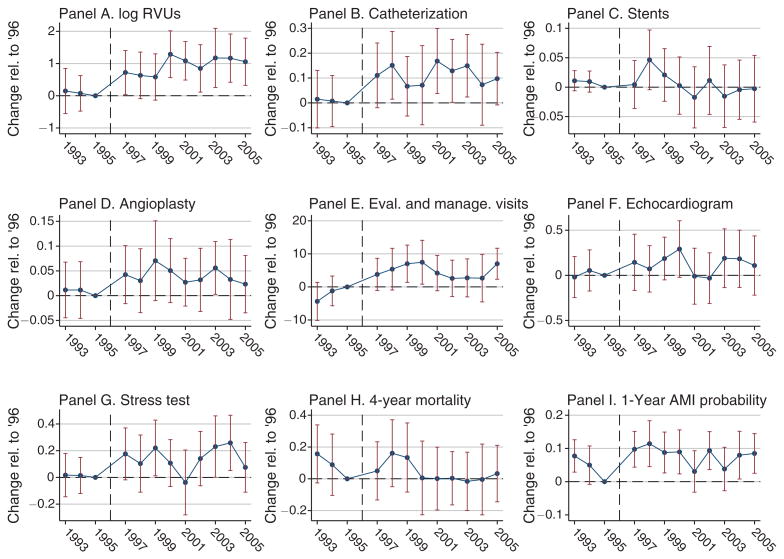
B. The Impact of Price Changes on Patient Care
We begin our analysis of patients with cardiovascular disease by examining the effect of reimbursement rates on the care they receive. Results are presented in Figure 9. The first panel of Figure 9 shows the impact of the 1997 price changes on the log RVUs received within one year of diagnosis. Short run estimates of the elasticity of supply are on the order of 0.6, while the long-run elasticity is in the neighborhood of 1. Panels B through D report the effect of reimbursement rates on the probability that a patient receives relatively intensive procedures, specifically catheterization (whether purely diagnostic or interventional), catheterization coupled with angioplasty, and catheterization coupled with stent insertion. Panel E reports the effect on the number of patients' evaluation and management visits, panel F on the probability of receiving an echocardiogram, and panel G on the probability of receiving a stress test. Consistent with prior results describing the responsiveness of relatively elective, but intensive, procedures, the elasticities associated with catheterization and angioplasty (shown in online Appendix Tables D.14 and D.15) are particularly large (on the order of 2 and 3 respectively).38 Office visits exhibit an elasticity of around 0.75, while the elasticities are intermediate and relatively imprecisely estimated for imaging and testing, on the order of 1.39
Figure 9. Impact of Price Change on Cardiac Patient Treatment.
Notes: These graphs show coefficients from ordinary least squares regressions in which the treatments received by patients with cardiovascular disease are the dependent variables. The sample is restricted to patients living in counties that satisfy our matching criterion, as described in the text (the results are essentially unchanged when we include the complete cohort defined in online Appendix D.1). The dependent variable in panel A is total quantity of care, expressed in logs, and in panels B through F they are indicators for receiving the relevant treatment in the year after diagnosis (excepting physician visits, reported in panel E, which are expressed as counts). The outcomes in panels G and H are health outcomes, with panel G corresponding to 4-year mortality and panel H corresponding to 1-year admission to the hospital with a heart attack diagnosis. These quantities, measured for each patient, are regressed on the reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, in the county where the patient was first diagnosed, as interacted with indicators for time relative to the payment area consolidation. All specifications control for county fixed effects, state-by-year effects, a set of year dummy variables interacted with an indicator whether the patient resides in a metropolitan area, and indicators for the patient's age, race, gender, and whether or not the individual was eligible for Medicare due to end-stage renal disease. The results are robust to controlling additionally for each patient's health as proxied for by a set of indicators for having the individual comorbidities defined by Elixhauser et al. (1998), as well as having 2 or more, 3 or more, 4 or more, and 6 or more comorbidities. Standard errors are clustered by pre-consolidation payment area.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; county demographics: Ruggles et al. (2010).
Transitioning to an analysis of health outcomes, we consider two splits of our sample, first by patient age and second by geographic practice intensity. To divide the sample by practice intensity, we divide the states into the top and bottom half of their distribution when ranked by the frequency with which the intensive services involving catheterization are used. Column 1 of Table 3 shows the results for total care elasticities. Although the differences in care elasticities are not statistically distinguishable across groups, they suggest in both instances that incremental care went disproportionately to populations already receiving relatively intensive treatment. The total care elasticity for those aged 75 and older is around 80 percent larger than the elasticity for those aged 65 to 74 (see panel B). The elasticity of total care in high intensity states is, similarly, around 60 percent larger than the elasticity of total care in low intensity states (see panel C).
Table 3. Effect of Reimbursement Rates on Cardiac Patients.
| Outcome | log care (1) | Mortality within 4 years (2) | MI hosp. within 1 year (3) |
|---|---|---|---|
| Panel A. Full sample | |||
| Price change × post-consolidation | 0.861*** (0.265) |
−0.057 (0.041) |
0.029** (0.014) |
| Panel B. Treatment effect heterogeneity by patient age | |||
| Price change × post-consolidation | 0.723*** (0.243) |
−0.131*** (0.045) |
0.031 (0.018) |
| Price change × post-consolidation × age ≥ 75 | 0.645 (0.424) |
0.236** (0.106) |
0.019 (0.040) |
| Panel C. Treatment effect heterogeneity by state-level cath intensity | |||
| Price change × post-consolidation | 0.733** (0.344) |
−0.074* (0.044) |
0.031** (0.014) |
| Price change × post-consolidation × high cath. intensity | 0.482 (0.579) |
0.067 (0.100) |
−0.004 (0.040) |
| Observations | 801,150 | 810,330 | 810,330 |
Notes: This table reports coefficients from ordinary least squares regressions for the following patient care and health-related outcomes: total care (column 1), an indicator for whether the patient dies within 4 years (column 2), and an indicator for whether the patient is hospitalized for MI (heart attack) during the first year following the initial diagnosis of cardiovascular disease (column 3). The sample is restricted to patients living in counties that satisfy our matching requirements, as described in the text (the results are essentially unchanged when we include the complete cohort defined in online Appendix D.1). In panel C, states are classified based on whether the entire state has an above-median share of patients with cardiovascular disease who receive this treatment. The outcomes are regressed on the reimbursement rate shocks resulting from the consolidation of Medicare's fee schedule areas in 1997, in the county where the patient was first diagnosed, interacted with an indicator for years after the consolidation. All specifications control for county fixed effects, state-by-year effects, a set of year dummy variables interacted with an indicator whether the patient resides in a metropolitan area, and indicators for the patient's age, race, gender, and whether or not the individual was eligible for Medicare due to end-stage renal disease. The results are robust to controlling additionally for each patient's health as proxied for by a set of indicators for having the individual comorbidities defined by Elixhauser et al. (1998), as well as having 2 or more, 3 or more, 4 or more, and 6 or more comorbidities. Standard errors are clustered by pre-consolidation payment area.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Sources: Price change: Federal Register, various issues; Medicare claims data: Medicare Research Identifiable Files, 5 percent sample, described in Section IC; county characteristics: Ruggles et al. (2010).
C. The Impact of Price Changes on Patient Outcomes
Column 2 of Table 3 reports effects on the probability that beneficiaries die within 4 years of their initial diagnosis. The mortality result for the full cardiac cohort suggests that a 1 percent increase in reimbursement rates reduces the probability that a patient dies within 4 years by 0.06 percent. The standard error of 0.04 is sufficiently large that this value cannot be statistically distinguished from either zero or from substantially larger values.
A comparison of mortality impacts across patient sub-groups yields a somewhat surprising result. The observed mortality reductions load entirely onto the younger and less intensively treated (at baseline) populations. Older beneficiaries appear, if anything, to experience increased mortality as a result of receiving more intensive care. While this positive point estimate is not statistically distinguishable from 0, it is statistically distinguishable from the mortality gains for younger beneficiaries. The mortality results are consistent with the view that care for these intensively-treated populations has approached “the fat of the curve.” Coupled with the estimated elasticities associated with care for these groups, our results suggest that incremental care may have been inefficiently allocated across the patient population.40
Column 3 reports results for the probability that cohort members are admitted to the hospital for treatment associated with an MI in the year following diagnosis. This constitutes an outcome of immediate concern for this particular cohort, as heart attacks are one of the principal outcomes that cardiac care is intended to prevent. The results provide no evidence that incremental care reduces the likelihood that a patient receives hospital care associated with an MI. Patients appear, if anything, to become more likely to be hospitalized as the intensity of their outpatient care regime increases.41 The evidence appears to be inconsistent with the hypothesis that incremental outpatient care generates significant offsetting reductions in spending on inpatient care. The offsets found by Chandra, Gruber, and McKnight (2010), who isolate changes in the utilization of office visits and prescription drugs, do not materialize for the broader packages of outpatient care that we analyze.42
An important shortcoming of this analysis is that we are restricted to health outcomes that can be detected in claims data. While mortality and hospitalizations are important outcomes, they are far from being a complete characterization of a patient's quality of life. Incremental care could very well improve or worsen a variety of outcomes that cannot be detected in the data.
VII. Conclusion
This paper finds that financial incentives significantly influence physicians' supply of health care. We estimate that a two percent increase in reimbursement rates across the board leads to a three percent increase in care. Physicians disproportionately adjust their provision of relatively intensive and elective treatments as reimbursements rise, and they appear to invest in new technologies in order to do so.
Our results highlight the importance of payment policy as a determinant of patient access to care, of the composition of care delivered, and of Medicare's aggregate spending on outpatient services. When patients are well insured, so that demand-side constraints are unlikely to bind, physician discretion becomes an important driver of these outcomes. While our estimates speak directly to the effects of across-the-board changes in reimbursements, they also point to the potential importance of payment reforms.
Our results speak most directly to so-called value based payments, which would be adjusted, among other things, for estimates of the relative cost effectiveness of substitutable services. If targeted payment changes have service-specific effects similar to those we find in the aggregate, then such adjustments hold the promise of curbing costs without jeopardizing quality. Bundled payments, which move away from fee-for-service medicine by making a single payment for a broader package of care or course of treatment, would also significantly alter the incentives physicians face. Our results speak less directly to such reforms. We thus close by noting that analysis of such payment models, in the context of both private and public insurance arrangements, is a natural direction for future research.
Supplementary Material
Acknowledgments
We are deeply indebted to Amitabh Chandra, David Cutler, Edward Glaeser, Lawrence Katz, and Andrei Shleifer for invaluable advice and guidance, and to four thoughtful referees and numerous others for extremely helpful comments and suggestions. We gratefully acknowledge support from the Taubman Center for State and Local Government and the Institute for Humane Studies, as well as support and data provided by the National Institute on Aging under grant P01AG031098 to the National Bureau of Economic Research. Gottlieb further thanks the NIA for a training fellowship provided under grant T32-AG000186-23 to the NBER.
Footnotes
Go to http://dx.doi.org/10.1257/aer.104.4.1320 to visit the article page for additional materials and author disclosure statement(s).
For instance, see Arrow et al. (2009), Ginsburg (2011), and Hackbarth, Reischauer, and Mutti (2008).
The care physicians provide has personal financial consequences, as 60 percent are self-employed (Wassenaar and Thran 2003, Table 2) and 85 percent of those in group practices have compensation linked to patient care revenues (Medical Group Management Association 1998, Table 12).
Past studies, including Acemoglu and Finkelstein (2008) and Finkelstein (2007), investigate the response of such decisions to incentives in the hospital context. The current study is, to the best of our knowledge, the first to do so in the environment of physicians' own practices.
We discuss Rice (1983) in greater detail in online Appendix A.
The investment response can also explain why aggregate results don't show the backward-bending labor supply found by Gruber and Owings (1996), Rice (1983), and others.
Clemens (2013) presents evidence that insurance arrangements significantly influence the development of the relevant medical equipment and devices, which is often spurred by physicians themselves.
Medicare covers nearly every American over age 65, and some additional beneficiaries eligible due to end-stage renal disease or disability. We study only those over 65. According to the Centers for Medicare and Medicaid Services, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MedicareMedicaidStatSupp/Downloads/05SS_CostShare_z.zip (Table 19a; accessed January 19, 2014), beneficiaries' cost sharing was 15.6 percent of total spending as of 2003, including that part paid by private supplemental insurance.
These values are determined according to the Resource-Based Relative Value Scale (RBRVS), initially developed by Hsiao et al. (1988).
This is a slight simplification; online Appendix A.1 details the payment structure.
The annual political wrangling over the “doc fix” results from the statutory formula, known as the Sustainable Growth Rate, that drives the evolution of the Conversion Factor.
By exploiting cross-sectional differences between costs in county i and broader area a(i), Hadley et al. (2009) estimate supply responses for ten services consistent with our results.
Geographic adjustments to hospital reimbursements under Medicare Part A are structured differently from the physician and outpatient reimbursements discussed here, so were not affected by this consolidation.
We define the short run post-consolidation period as the two years following the consolidation (1997 and 1998), the medium run as the next two years (1999 and 2000) and the long run as the remainder of the sample (2001 through 2005).
Importantly for these purposes, many urban and rural areas did not experience price shocks; no price shocks occurred in states, including those as large as Minnesota, that consisted of a single payment area prior to 1997.
Urban population share is from Ruggles et al. (2010) and metropolitan status is from http://www.census.gov/population/metro/data/pastmetro.html (accessed December 21, 2007).
These characteristics are log population in 1990, log density in 1990, and level of the GAF in 1993.
We show that our results are little affected by including the full sample of counties.
Two exceptions apply to this statement, and are detailed in online Appendix A.3.
That is, adjusted for all of the fixed effects and other controls in Xi,s(i), t defined in Section IA.
Part B, formally known as Supplementary Medical Insurance, is the part of Medicare that covers physician services and outpatient care, including all of the fee schedule care we study. By including only beneficiaries participating in Part B, we are ignoring those recipients of Part A hospital insurance who choose not to enroll in Part B, as well as those who choose a Medicare Advantage managed care plan instead of traditional Part B.
This 40 percent margin is consistent with data from the American Medical Association (Wassenaar and Thran 2003, Tables 32 and 35).
This elasticity is moderately larger than standard population-wide estimates. It is, however, quite comparable to estimates specific to the self-employed or to other individuals with flexible labor supply. Most directly relevant to our setting, Showalter and Thurston (1997) estimate a labor supply elasticity of 0.6 for self-employed physicians in sole proprietorships. Saez (2010) estimates elasticities around 1 for self-employed individuals with relatively low incomes.
For purposes of interpretation, it is important to note that the estimated response of private care provision to changes in Medicare's reimbursement rates has a very reduced form character. The estimates cannot be interpreted as pure cross-price elasticities because changes in Medicare's payments may result in changes in private sector payments.
Exploring linear combinations of the Medicare and private coefficients in online Appendix Table D.3, we estimate that there is a 12 percent chance that the sum of private and Medicare supply responses is zero or below. The high level of uncertainty is driven in part by the fact that the private market for these services is more than twice as large as the Medicare market. We thank an anonymous referee for suggesting this exercise as a way to gauge the uncertainty surrounding our results' implications for the effects of Medicare's reimbursement rates on quantities supplied across the entire health sector. Unexplored, and adding further uncertainty, are implications for care provided to Medicaid beneficiaries and the uninsured.
Afendulis and Kessler (2007) and Shah et al. (2011) show that vertically integrated cardiology practices influence patients' treatment courses, as does Baker (2010) for self-referral to magnetic resonance imaging.
While traditional Medicare does have co-payments, 90 percent of beneficiaries have either supplemental insurance or are eligible for a state-funded Medicaid supplemental that reduces or eliminates patient costs at the margin (MEDPAC 2011).
This contrasts with standard markets in which the benefit curve would simply describe demand.
This treatment of income, which implies high-powered financial incentives, applies quite directly to the three-fifths of American physicians that are self-employed (self-employment data are available in Wassenaar and Thran 2003, Table 2). It is also a reasonable approximation of the incentives faced by the 85 percent of physicians in group practices who, as of 1997, had their compensation directly linked to revenue (Table 12, Medical Group Management Association 1998). The quasilinear utility assumption simplifies the analysis and guarantees the positive supply responses that characterized Section II's empirical results. With a more general utility function in income, supply responses would depend on the relative magnitudes of substitution effects (Staiger, Auerbach, and Buerhaus 2010) and income effects (Gruber and Owings 1996; Congressional Budget Office 2007).
We assume that e(·) satisfies e(0) = 0, e′(0) = 0, e′(·) > 0, e′(·) > 0.
The Berenson-Eggers Type of Service (Betos) categories provide a mapping between each specific medical service and 106 aggregate categories of services. They are updated by CMS annually to incorporate new service codes, and are available online at http://www.cms.gov/HCPCSReleaseCodeSets/20_Betos.asp (accessed October 16, 2011).
A detailed classification of the Betos codes is available in online Appendix B.3.
We present results in online Appendix D.3 showing that, for patients diagnosed with hip fractures, the likelihood of receiving a hip fracture repair is unaffected by reimbursement shocks while the number of evaluative office visits (a relatively elective service) responds.
This has been increasingly common since the Stark law banned physician referrals to outside entities with which the doctor has a financial relationship (MEDPAC 2009, p. 86). This installation can involve a variety of financial arrangements that have the common and crucial feature of giving the physician a financial incentive to use the scanner more frequently (Mitchell 2007). Baker (2010) finds that physicians increase the use of MRIs following the acquisition of a machine.
Online Appendix Tables D.10 and D.11 report the relevant parametric difference-in-differences results.
Head and neck MRIs are those included in Betos category I2C, and the others are those in category I2D.
Online Appendix Table D.13 combines the three difference-in-differences coefficients into one post-1997 interaction term.
Online Appendix D describes our protocol for assembling cohorts of individuals with cardiovascular disease and measuring their treatments.
Interpreting these elasticities is somewhat problematic because the physician payments are only part of the compensation for hospital-based catheterization services. The hospital's facility charges are not adjusted using the same geographic adjustment as physician charges so are not directly affected by the consolidation. Hence the observed elasticities with respect to the overall payment are larger than those reported here, but the economically relevant response depends on who makes treatment decisions in this context.
The small office visit elasticity may reflect the fact that these patients are coming in for a large number of office visits at baseline.
We estimate the effect of reimbursement rates on life expectancy more directly using Cox proportional hazard models, which are not reported. The results of this analysis exhibit a pattern similar to those shown here; modest overall mortality gains appear to be concentrated among the relatively young and among those in states associated with less intensive care regimes. Results from these models can never be distinguished statistically from zero.
This result may reflect complementarities between incremental outpatient care and hospital care rather than a worsening of health outcomes.
This should not be taken to imply that this paper's results contradict those of Chandra, Gruber, and McKnight (2010). The packages of care affected by the relevant natural experiments differ in two important ways. First, as already noted, this paper's price shocks affected a broad package of outpatient care, as opposed to being targeted at office visits and prescription drugs. Second, changes in utilization are, in this paper's case, driven by physician incentives, while they are driven by changes in patient cost sharing in Chandra, Gruber, and McKnight's analysis.
Contributor Information
Jeffrey Clemens, Email: jeffclemens@ucsd.edu, Department of Economics, University of California, San Diego, 9500 Gilman Drive #0508, La Jolla, CA 92093, and NBER.
Joshua D. Gottlieb, Email: Joshua.Gottlieb@ubc.ca, Vancouver School of Economics, University of British Columbia, 997-1873 East Mall, Vancouver, BC V6T 1Z1, Canada.
References
- Acemoglu Daron, Finkelstein Amy. Input and Technology Choices in Regulated Industries: Evidence from the Health Care Sector. Journal of Political Economy. 2008;116(5):837–80. [Google Scholar]
- Acemoglu Daron, Linn Joshua. Market Size in Innovation: Theory and Evidence from the Pharmaceutical Industry. Quarterly Journal of Economics. 2004;119(3):1049–90. [Google Scholar]
- Afendulis ChristopherC, Kessler DanielP. Tradeoffs from Integrating Diagnosis and Treatment in Markets for Health Care. American Economic Review. 2007;97(3):1013–20. doi: 10.1257/aer.97.3.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrow Kenneth J. Uncertainty and the Welfare Economics of Medical Care. American Economic Review. 1963;53(5):941–73. [Google Scholar]
- Arrow KennethJ, Auerbach Alan, Bertko John, Shannon Brownlee, Casalino LawrenceP, Cooper Jim, Crosson FrancisJ, et al. Toward a 21st-Century Health Care System: Recommendations for Health Care Reform. Annals of Internal Medicine. 2009;150(7):493–95. doi: 10.7326/0003-4819-150-7-200904070-00115. [DOI] [PubMed] [Google Scholar]
- Baicker Katherine, Chandra Amitabh. Aspirin, Angioplasty, and Proton Beam Therapy: The Economics of Smarter Health Care Spending. 2011 Unpublished. [Google Scholar]
- Baker LaurenceC. Acquisition Of MRI Equipment By Doctors Drives Up Imaging Use And Spending. Health Affairs. 2010;29(12):2252–59. doi: 10.1377/hlthaff.2009.1099. [DOI] [PubMed] [Google Scholar]
- Bloom Nick, Bond Stephen, Reenen JohnVan. Uncertainty and Investment Dynamics. Review of Economic Studies. 2007;74(2):391–415. [Google Scholar]
- Caballero RicardoJ, Engel EduardoMRA. Explaining Investment Dynamics in U.S. Manufacturing: A Generalized (S, s) Approach. Econometrica. 1999;67(4):783–826. [Google Scholar]
- Chandra Amitabh, Gruber Jonathan, McKnight Robin. Patient Cost-Sharing and Hospitalization Offsets in the Elderly. American Economic Review. 2010;100(1):193–213. doi: 10.1257/aer.100.1.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra Amitabh, Skinner JonathanS. Technology Growth and Expenditure Growth in Health Care. Journal of Economic Literature. 2012;50(3):645–80. [Google Scholar]
- Cherkin DanielC, Deyo RichardA, Battié Michele, Street Janet, Barlow William. A Comparison of Physical Therapy, Chiropractic Manipulation, and Provision of an Educational Booklet for the Treatment of Patients with Low Back Pain. New England Journal of Medicine. 1998;339(15):1021–29. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- Clemens JeffreyP. The Effect of U.S. Health Insurance Expansions on Medical Innovation. National Bureau of Economic Research Working Paper 19761 2013 [Google Scholar]
- Clemens Jeffrey, Gottlieb JoshuaD. Do Physicians' Financial Incentives Affect Medical Treatment and Patient Health?: Dataset. American Economic Review. 2014 doi: 10.1257/aer.104.4.1320. http://dx.doi.org/10.1257/aer.104.4.1320. [DOI] [PMC free article] [PubMed]
- Codespote SuzanneM, London WilliamJ, Shatto JohnD. Physician Volume & Intensity Response. Memorandum to Richard S Foster Office of the Actuary, Health Care Financing Administration, August 13 1998 [Google Scholar]
- Congressional Budget Office. Factors Underlying the Growth in Medicare's Spending for Physicians' Service. The Congress of the United States, Background Paper. 2007:2597. [Google Scholar]
- Cutler DavidM. Your Money Or Your Life: Strong Medicine for America's Health Care System. Oxford: Oxford University Press; 2004. [Google Scholar]
- Cutler DavidM, Rosen AllisonB, Vijan Sandeep. The Value of Medical Spending in the United States, 1960–2000. New England Journal of Medicine. 2006;355(9):920–27. doi: 10.1056/NEJMsa054744. [DOI] [PubMed] [Google Scholar]
- Deyo RichardA, Weinstein JamesN. Low Back Pain. New England Journal of Medicine. 2001;344:363–70. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- Elixhauser Anne, Steiner Claudia, Harris DRobert, Coffey RosannaM. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Ellis RandallP, McGuire ThomasG. Provider Behavior under Prospective Reimbursement: Cost Sharing and Supply. Journal of Health Economics. 1986;5(2):129–51. doi: 10.1016/0167-6296(86)90002-0. [DOI] [PubMed] [Google Scholar]
- Feldstein MartinS. The Welfare Loss of Excess Health Insurance. Journal of Political Economy. 1973;81(2):251–80. [Google Scholar]
- Feldstein Amy. Static and Dynamic Effects of Health Policy: Evidence from the Vaccine Industry. Quarterly Journal of Economics. 2004;119(2):527–64. [Google Scholar]
- Feldstein Amy. The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare. Quarterly Journal of Economics. 2007;122(1):1–37. [Google Scholar]
- Friedly Janna, Chan Leighton, Deyo Richard. Increases in Lumbosacral Injections in the Medicare Population: 1994 to 2001. Spine. 2007;32(16):1754–60. doi: 10.1097/BRS.0b013e3180b9f96e. [DOI] [PubMed] [Google Scholar]
- Ginsburg PaulB. Reforming Provider Payment—The Price Side of the Equation. New England Journal of Medicine. 2011;365(14):1268–70. doi: 10.1056/NEJMp1107019. [DOI] [PubMed] [Google Scholar]
- Glied Sherry, Zivin JoshuaGraff. How Do Doctors Behave When Some (but Not All) of Their Patients Are in Managed Care? Journal of Health Economics. 2002;21(2):337–53. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Gruber Jonathan, Owings Maria. Physician Financial Incentives and Cesarean Section Delivery. RAND Journal of Economics. 1996;27(1):99–123. [PubMed] [Google Scholar]
- Hackbarth Glenn, Reischauer Robert, Mutti Anne. Collective Accountability for Medical Care—Toward Bundled Medicare Payments. New England Journal of Medicine. 2008;359(1):3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]
- Hadley Jack, Reschovsky James, Corey Catherine, Zuckerman Stephen. Medicare Fees and the Volume of Physicians' Services. Inquiry. 2009;46(4):372–90. doi: 10.5034/inquiryjrnl_46.4.372. [DOI] [PubMed] [Google Scholar]
- Hall RobertE, Jones CharlesI. The Value of Life and the Rise in Health Spending. Quarterly Journal of Economics. 2007;122(1):39–72. [Google Scholar]
- Hsiao WilliamC, Braun Peter, Yntema Douwe, Becker EdmundR. Estimating Physicians' Work for a Resource-based Relative-value Scale. New England Journal of Medicine. 1988;319(13):835–41. doi: 10.1056/NEJM198809293191305. [DOI] [PubMed] [Google Scholar]
- Jensen MaureenC, Brant-Zawadzki MichaelN, Obuchowski Nancy, Modic MichaelT, Malkasian Dennis, Ross JeffreyS. Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain. New England Journal of Medicine. 1994;331(2):69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- Levin DavidC, Rao VijayM, Parker Laurence, Frangos AndreaJ, Sunshine JonathanH. Ownership or Leasing of MRI Facilities by Nonradiologist Physicians Is a Rapidly Growing Trend. Journal of the American College of Radiology. 2008;5(2):105–9. doi: 10.1016/j.jacr.2007.09.017. [DOI] [PubMed] [Google Scholar]
- Manning WillardG, Newhouse JosephP, Duan Naihua, Keeler EmmettB, Leibowitz Arleen, Marquis MSusan. Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. American Economic Review. 1987;77(3):251–77. [PubMed] [Google Scholar]
- McGuire ThomasG, Pauly MarkV. Physician Response to Fee Changes with Multiple Payers. Journal of Health Economics. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- Medical Group Management Association (MGMA) Physician Compensation and Production Survey: 1998 Report Based on 1997 Data. Englewood, CO: MGMA; 1998. [Google Scholar]
- Medicare Payment Advisory Commission (MEDPAC) Report to the Congress; Improving Incentives in the Medicare Program. Washington, DC: MEDPAC; 2009. Impact of Physician Self-Referral on Use of Imaging Services within an Episode; pp. 81–100. [Google Scholar]
- Medicare Payment Advisory Commission (MEDPAC) A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: MEDPAC; 2011. [Google Scholar]
- Medicare Payment Advisory Commission (MEDPAC) A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: MEDPAC; 2012. [Google Scholar]
- Mitchell JeanM. The Prevalence Of Physician Self-Referral Arrangements After Stark II: Evidence From Advanced Diagnostic Imaging. Health Affairs. 2007;26(3):w415–w424. doi: 10.1377/hlthaff.26.3.w415. [DOI] [PubMed] [Google Scholar]
- Murphy KevinM, Topel RobertH. The Value of Health and Longevity. Journal of Political Economy. 2006;114(5):871–904. [Google Scholar]
- Newhouse JosephP. Medical Care Costs: How Much Welfare Loss? Journal of Economic Perspectives. 1992;6(3):3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- Newhouse JosephP. Pricing the Priceless: A Health Care Conundrum. Cambridge, MA: MIT Press; 2003. [Google Scholar]
- Rice ThomasH. The Impact of Changing Medicare Reimbursement Rates on Physician-Induced Demand. Medical Care. 1983;21(8):803–15. doi: 10.1097/00005650-198308000-00004. [DOI] [PubMed] [Google Scholar]
- Ruggles Steven, Alexander JTrent, Genadek Katie, Goeken Ronald, Schroeder MatthewB, Sobek Matthew. Integrated Public Use Microdata Series: Version 5.0. Minneapolis: University of Minnesota; 2010. [Google Scholar]
- Saez Emmanuel. Do Taxpayers Bunch at Kink Points? American Economic Journal: Economic Policy. 2010;2(3):180–212. [Google Scholar]
- Shah BimalR, Cowper PatriciaA, O'Brien SeanM, Jensen Neil, Patel ManeshR, Douglas PamelaS, Peterson EricD. Association Between Physician Billing and Cardiac Stress Testing Patterns Following Coronary Revascularization. Journal of the American Medical Association. 2011;306(18):1993–2000. doi: 10.1001/jama.2011.1604. [DOI] [PubMed] [Google Scholar]
- Showalter MarkH, Thurston NormanK. Taxes and Labor Supply of High-Income Physicians. Journal of Public Economics. 1997;66(1):73–97. [Google Scholar]
- Staiger DouglasO, Auerbach DavidI, Buerhaus PeterI. Trends in the Work Hours of Physicians in the United States. Journal of the American Medical Association. 2010;303(8):747–53. doi: 10.1001/jama.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassenaar JohnD, Thran SaraL., editors. Physician Socioeconomic Statistics 2003. Atlanta, GA: American Medical Association Press; 2003. [Google Scholar]
- Weiner DebraK, Kim YoungSin, Bonino Paula, Wang Tracy. Low Back Pain in Older Adults: Are We Utilizing Healthcare Resources Wisely? Pain Medicine. 2006;7(2):143–50. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- Weisbrod BurtonA. The Health Care Quadrilemma: An Essay on Technological Change, Insurance, Quality of Care, and Cost Containment. Journal of Economic Literature. 1991;29(2):523–52. [Google Scholar]
- Yin Wesley. Market Incentives and Pharmaceutical Innovation. Journal of Health Economics. 2008;27(4):1060–77. doi: 10.1016/j.jhealeco.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Yurukoglu Ali. Medicare Reimbursements and Shortages of Sterile Injectable Pharmaceuticals. National Bureau of Economic Research Working Paper 17987 2012 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.